Search
Search
Celebrating the 2022 Lawson Impact Award winners
The Lawson Impact Awards are a pinnacle of celebration in the Lawson Health Research Institute community, celebrating innovation across London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. The Impact Awards recognize hospital-based research that makes a difference by advancing scientific knowledge and applying it directly to patient care.
With awards in eight categories, the annual awards honour Lawson scientists, staff, trainees and partners who demonstrate excellence.
“The Lawson Impact Awards are a celebration of the research mission of LHSC and St. Joseph’s,” says Dr. David Hill, Scientific Director at Lawson. “There is innovation happening every day here in London, Ontario. The environment and close proximity to patient care allow us to hire great scientists that flourish in our research space.”
Recognized for his high-impact work over the past several years, Dr. Douglas Fraser was named as Lawson’s Scientist of the Year – the Lawson Impact Awards’ highest honour. Dr. Fraser, who is a Scientist at Lawson and Critical Care Physician at Children’s Hospital at London Health Sciences Centre (LHSC), has led the way in a number of areas of research. Over the past few years, he has published numerous studies and signed multiple licensing agreements that show promise for improving the diagnosis and treatment of concussion, COVID-19 and long COVID.
“Research is exciting to me and I love showing up to work. We have great colleagues, wonderful resources which allows us to ask good questions and it is a pleasure coming to work each day,” says Dr. Fraser, who is also a Professor at Western University’s Schulich School of Medicine & Dentistry. “It I always an honor to be recognized and humbling as well, because most of the work we have done has always been a group effort.”
Dr. Fraser is one of eight 2022 Lawson Impact Award recipients.
A big congratulations to all of this year’s winners, as well as our 2022 Lawson Strategic Research Fund recipients:
Scientist of The Year Award: Dr. Douglas Fraser
Dr. Joseph Gilbert Research Contribution of The Year Award: Dr. Daniel Hardy
Innovation Award: Dr. Dalton Wolfe
London Health Sciences Foundation Community Partner Of The Year Award: Archie Verspeeten
St. Joseph's Health Care Foundation Community Partner Of The Year Award: Dr. Joseph Rea
Children's Health Foundation Community Partner Of The Year Award: Dr. Paul and Mrs. Mary Harding
Leadership Award for Fellows & Students: Karnig Kazazian
Staff Award Of Excellence: Dr. Jeff Weiler
Strategic Research Fund Recipients: Dr. Matthew Teeter & Dr. Jonathan Thiessen and Dr. Luciano Sposato & Dr. Frank Prato
You can visit the full Impact Awards site by clicking here
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Changing our MINDS
Local youth use art and storytelling to illustrate the personal and system challenges in mental health.
The words and images are both heartbreaking and hopeful.
“Nobody likes you if you are sad.”
you are enough. stay strong. let life surprise you.
“Please don’t leave like everyone else.”
1 year sober. 1 year of school. 1 year building a safe home. 1 year loving myself.
Zine-writing, a personal and introspective medium often used by people who have been marginalized, is an important part of local research that is finding solutions to complex mental health challenges among young adults. Its name derives from its magazine (“zine”) format.
“When we make the voices of people with lived experience central to our research, we can learn from each other and then change the system together,” says Dr. Arlene MacDougall, founder of MINDS of London-Middlesex.
The social innovation and research lab based at St. Joseph’s Health Care London (St. Joseph’s) is dedicated to designing, piloting and testing mental health innovations for teens and young adults. Its recent evolution into MINDS 2.0 adds insights by and for people up to age 35 who have complex, pervasive mental health and addiction issues.
Learning from experts
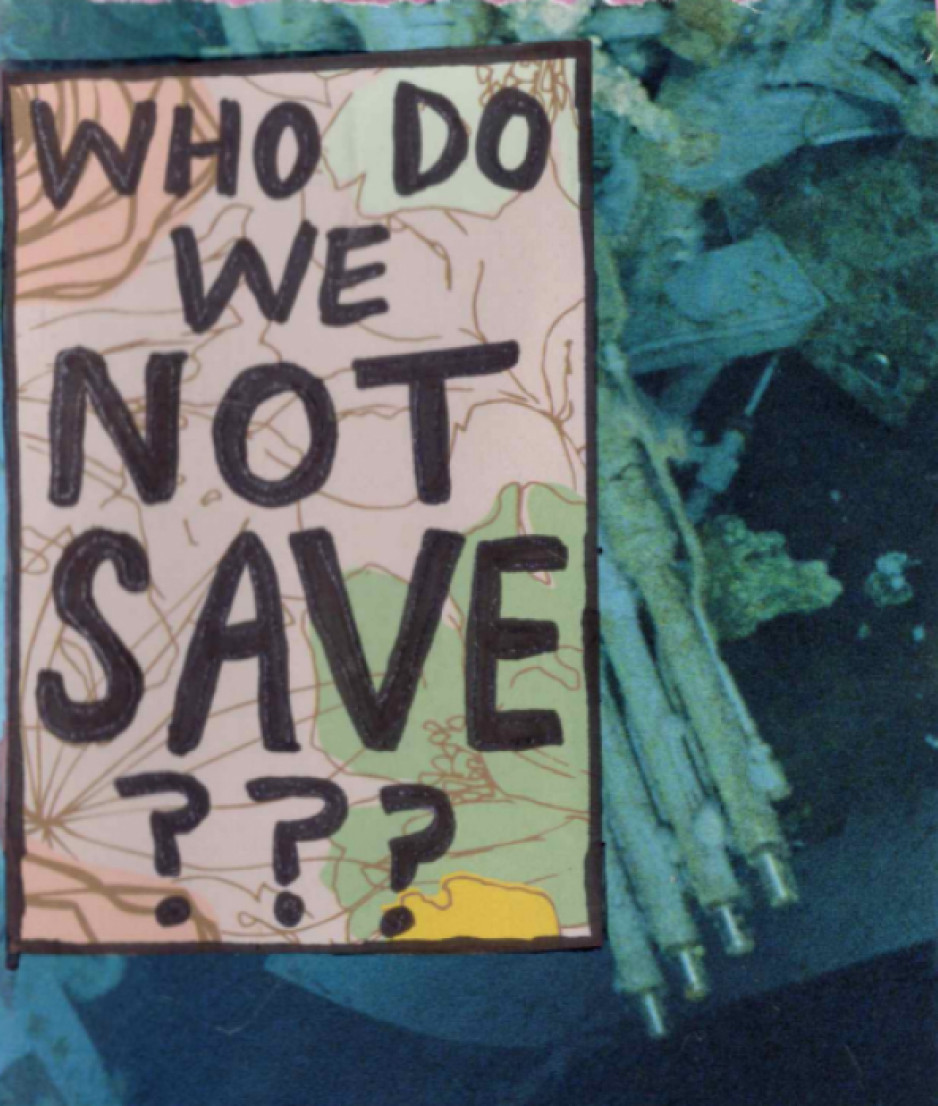
Rin, a London artist, who has published independent zines for a decade, created three for this project, including one that, with irony, asks the reader to ponder which vulnerable people aren’t worth saving.
“I believe making art can be very healing,” says Rin. “I wanted to share some of my story to help myself and help others. I want to play a part in shaping a mental health system that’s better than the one I encountered.”
The zines weave art, prose and poetry into story:
3 things I would change: affordability, stigma, waitlists.
“If I had a magic wand, I would use it to heal the waters, grow the trees, foster animal growth.”
Look in the mirror, see how far you’ve come.
They also raise and propose solutions to troubling issues among people with mental illness: housing and homelessness, sparse resources for people with addictions, lack of coordination among service providers, and dehumanizing attitudes in health and criminal justice systems.
“Participants experienced catharsis just in telling their stories,” says Renee Hunt PhD, Associate Director of Research and Operations at MINDS. “And because they’re the experts, they’re also playing an important part in changing systems that need an overhaul.”
Adds Rin, “It feels empowering knowing people are listening to us – people who care and are committed to making change to the system.”
MacDougall notes the pivotal role of St. Joseph’s Health Care Foundation – in particular, a groundbreaking $5-million donation towards mental health research from philanthropist Ryan Finch – in advancing mental health innovation through MINDS and MINDS 2.0.
“They’ve been our biggest supporters since day one. This wouldn’t have happened without support from Ryan and the foundation and all the many donors who believe in mental health research,” says MacDougall, who is also Director of Research and Innovation with St. Joseph’s Mental Health Care Program.
“MINDS has been a catalyst for system change,” MacDougall adds. “Research is always about finding answers and generating impact.”
Many findings from MINDS research have been put into practice, among them are the creation of guidebooks for peer support, free taxi service for rural youth needing urban mental health or addiction services, and educational resources to support 2SLGBTQI+ students.
MacDougall says MINDS 2.0 expands that work with new voices and the exploration of more in-depth solutions.
What’s next for MINDS 2.0
- Workshopping ideas and prototypes for mental health systems change. Sessions will be held where people with lived/living experience and service providers propose and develop potential solutions.
- Leadership-building. Twenty mental health practitioners will be trained to become “agents of change” who will collectively create, implement and evaluate mental health programs, technology, interventions and training.
- Imaginarium conference. In 2025, a first-of-its-kind national conference will take place to share system innovations in mental health and addiction.
Children born in Sarnia at higher risk of developing asthma, compared to London and Windsor
LONDON, ON – New findings from Ontario have shown that children born in Sarnia have a higher risk of developing asthma compared to neighbouring cities. A research team from Lawson Health Research Institute and Western University, using provincial data from ICES, found that higher air pollution exposure in the first year of life very likely contributed to this higher risk. Their results are published today in CMAJ Open.
Summary of study results:
- Children born in Sarnia in the 1990s and early 2000s were disproportionally at a higher risk of developing asthma in the first few years of life, compared to neighbouring cities.
- Air pollution exposure in the first year was found to be associated with the development of asthma in children.
- Overall rates of new childhood asthma diagnosis in Southwestern Ontario have been decreasing over time in parallel to decreases in air pollution levels.
“It’s known that cities in Southwestern Ontario have varied levels of air pollution because of differences in industry and traffic. For example, Sarnia is home to the ‘Chemical Valley’ where numerous chemical plants and oil refineries are clustered,” says Dr. Dhenuka Radhakrishnan, an Adjunct ICES Scientist, formerly working out of ICES Western in London, and Pediatric Respirologist at CHEO. “We wanted to see if children born in three cities – London, Windsor and Sarnia – had a different risk of developing asthma due to the differing air pollution levels in the three regions, even though the people living in these cities are otherwise comparable in many ways.”
The researchers followed 114,427 children born in these cities between 1993 and 2009 for 10 years, and found that those in Sarnia were at the highest risk of developing asthma. The researchers found that by the age of 10, nearly 24 per cent of children in Sarnia were diagnosed with asthma, compared to 21 per cent in Windsor and 17 per cent in London. The differences were also present after accounting for many risk factors associated with asthma, such as sex, socioeconomic status and urban versus rural setting. The findings were most apparent in the first two years of life, but persistent beyond the age of six.
“Reassuringly, we found the asthma risk for children has reduced in more recent years as pollution levels have also decreased,” adds Dr. Radhakrishnan.
Asthma is the most common chronic disease in Canadian children and has significant impact on quality of life. Asthma is the leading cause of emergency department visits and hospital admissions in this age group.
“It’s important to find strategies to prevent asthma development and this study suggests that reducing air pollution exposure, including environmental causes, might reduce the number of children who suffer from asthma,” explains Dr. Salimah Shariff, Associate Scientist at Lawson, Adjunct Professor at Western and Scientist at ICES Western.
There is also growing evidence that exposure during pregnancy can influence development of asthma in children. “We need to carefully examine how reducing air pollution exposures within a geographic area translates to reductions in asthma development. Understanding the amount of air pollution that a mother and infant are exposed to, and how this impacts their personal risk, could enable regions to target safer levels for their residents,” adds Dr. Shariff.
Wednesday, May 5 is World Asthma Day (WAD). Recognizing symptoms of asthma early is the best a parent can do to improve the health of their child, so they can be diagnosed quickly and start appropriate treatments. If a parent notices their child has wheezing, persistent cough or difficulty with exercise, they are encouraged to bring this to the attention of a health care provider.
-30-
DOWNLOADABLE MEDIA

Child using an age-appropriate valved spacer device with an asthma inhaler. They should be used together for children to ensure the medication is properly delivered to the lungs.

Child using an age-appropriate valved spacer device with an asthma inhaler. They should be used together for children to ensure the medication is properly delivered to the lungs.

Dr. Dhenuka Radhakrishnan, an Adjunct ICES Scientist, formerly working out of ICES Western in London, and Pediatric Respirologist at CHEO

Dr. Salimah Shariff, Associate Scientist at Lawson, Adjunct Professor at Western and Scientist at ICES Western

Proportion of children with an asthma diagnosis by studied region
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
CIHR funding for COVID-19 enables researchers to investigate virus transmission during surgery and pandemic planning
Researchers at Western University and Lawson Health Research Institute continue to make important contributions to help mitigate the spread of COVID-19 and its negative consequences. Two projects in London will address virus transmission during surgery and pandemic planning for COVID-19, thanks to new funding announced by the Government of Canada, through the Canadian Institutes of Health Research (CIHR), along with provincial partners.
Researchers in London received more than $400,000 in funding through this latest round.
“Accelerating high-quality research and real-time evidence is a priority for Canada in its fight against COVID-19. I congratulate the successful teams for their essential work aimed at better preventing, detecting and treating COVID-19 at the individual and population levels,” said Patty Hajdu, Minister of Health in a press release. “Our government believes that it’s through collaboration and data sharing that we will respond efficiently to this global health emergency.”
Virus transmission in surgical smoke
In an effort to perform surgery during the pandemic as effectively and safely as possible, Dr. Leigh Sowerby, Associate Professor at Schulich Medicine & Dentistry and Associate Scientist at Lawson, will be investigating whether or not the virus that causes COVID-19 can be transmitted in surgical smoke. Surgical smoke is the aerosol produced by an essential surgical tool called electrocautery.
“Electrocautery is a ubiquitous tool for surgery, and is known to generate aerosol and smoke. We do not know if the SARS-CoV-2 virus can be transmitted in this plume, and this is important to answer for all surgeons, but in particular, for surgeons working in the respiratory and aerodigestive tract,” said Dr. Sowerby, who is also a head and neck surgeon at London Health Sciences Centre and St. Joseph’s Health Care London. “CIHR funding will allow us to rapidly execute this project. Without this funding, the project would not be possible.”
Dr. Sowerby says the results from this study, whether positive or negative, will have important implications. If positive, it will have a critical and direct impact on ensuring the safety of health care workers performing procedures on patients. Procedures using cautery will continue to require high level protection if the COVID-19 status of the patient is unknown. If negative, it will allow these surgical procedures to continue safely and effectively while conserving critical protective equipment for cases that need it.
The family physician’s role in pandemic plans
Maria Mathews, PhD, Associate Professor at Schulich Medicine & Dentistry, is investigating how the role of family physicians can be better incorporated into pandemic plans. Family physicians play important roles during a pandemic, from detecting potential outbreaks and screening and testing patients to providing care to infected patients and contributing to surge capacity in hospitals.
“During the early stages of the COVID-19 pandemic, family physicians had concerns about roles they were asked to fill for a variety of reasons, including the lack of appropriate personal protective equipment, availability of tests, and concerns about infection risks to other patients and staff in a family practice clinic,” said Mathews.
Mathews will examine the experiences in four regions in Canada – Newfoundland and Labrador, Nova Scotia, Ontario and British Columbia – to identify key roles, supports and best practices. The results will provide government ministries, public health units, and other health organizations with evidence and tools in order to incorporate family physicians in the response to a potential second COVID-19 wave and plan for future pandemics.
Class of medication used for overactive bladder linked to new onset of dementia
A study from Western University, Lawson Health Research Institute and ICES provides further evidence of a link between a common class of medications called anticholinergics and the onset of dementia.
Anticholinergic medications are those that act on the body’s cholinergic receptors, and are used to treat a range of conditions from allergies and nausea to overactive bladder and psychiatric disorders.
Using ICES data for more than 60,000 Ontarians, Dr. Blayne Welk looked at a specific group of patients with a condition known as overactive bladder. This condition, which affects one in ten Canadians, can be treated with two different classes of medication – anticholinergic medication, and another medication class known as beta-3 agonists. Both medications are effective for treating overactive bladder.
The results of the study showed an increase in the number of new cases of dementia for patients being treated with an anticholinergic medication compared to those being treated with beta-3 agonists. While the overall risk for dementia was low, the rate was 20 per cent higher for patients treated with an anticholinergic medication. During the study, 2.3 per cent of people developed dementia if they used an anticholinergic, as compared to 1.6 per cent of people who used a beta-3 agonist medication.
“The unique thing about this study is that with overactive bladder there is a new medication that isn’t an anticholinergic, so it allowed us to do a very good comparison between two groups of patients that all have the same condition at the start of the study,” said Dr. Welk, an Associate Professor at the Schulich School of Medicine & Dentistry at Western and Scientist at Lawson Health Research Institute. “We were able to confirm with more certainty that there is an increased risk of dementia with the use of anticholinergic medication.”
Dr. Welk hopes this study will help to further emphasize the cognitive risks associated with this class of drugs, and to encourage physicians to consider alternative medications or appropriate deprescribing where possible.
“The hope is to draw attention from the medical community to consider the cognitive side-effects when prescribing anticholinergic medications,” Dr. Welk, who is also an Adjunct Scientist at ICES said. “With overactive bladder, we have an alternate medication choice now that works through a different pathway. If a patient has cognitive dysfunction, it may be appropriate to consider using a non-anticholinergic medication first for the treatment of overactive bladder symptoms.”
Clinical trial will evaluate new therapy for patients with treatment-resistant depression as a result of bipolar disorder
LONDON, ON – Researchers at Lawson Health Research Institute are offering new hope to patients with treatment-resistant depression through participation in a national clinical trial. The study is the first randomized controlled trial to examine the efficacy of a new treatment called magnetic seizure therapy (MST) for patients with treatment-resistant depression as a result of bipolar disorder.
Treatment-resistant depression is a severe form of depression that does not respond to traditional therapies like medication. It is particularly common in patients with depression from bipolar disorder who are left with limited treatment options.
For years electroconvulsive therapy (ECT) has been the gold standard for patients with treatment-resistant depression. ECT uses an electric field to induce a seizure that provides a therapeutic benefit. But while ECT is effective, many patients opt out of treatment due to stigma surrounding the therapy and the potential for cognitive side effects like disorientation and amnesia.
MST has emerged as a promising alternative. MST works in a similar way to ECT but uses a focused magnetic field as opposed to electricity. As a result, MST induces a more focused seizure to reduce the risk of cognitive side effects.
“Magnetic seizure therapy has already been shown as a promising treatment for major depressive disorder or unipolar depression,” explains Dr. Amer Burhan, local site lead, researcher at Lawson and neuropsychiatrist at St. Joseph’s Health Care London. “For the first time, we’re studying how effective the treatment is for depression as a result of bipolar disorder and whether it can reduce the risk of cognitive side effects associated with electroconvulsive therapy.”
The clinical trial is being led by the Centre for Addiction and Mental Health (CAMH) and will also be offered through Lawson and University of British Columbia (UBC) Hospital. Lawson researchers will invite eligible patients with treatment-resistant depression from bipolar disorder to participate in the trial at Parkwood Institute, a part of St. Joseph’s Health Care London.
Eligible patients will be randomized to receive either ECT or MST. Patients will be offered support throughout the study with the goal of improving patient outcomes in both groups. Patient outcomes will be compared to study the efficacy of MST and whether it is associated with reduced cognitive side effects.
MST will be delivered under anesthesia in 12 to 20 sessions. Sessions will last 10 to 15 minutes each with 60 to 90 minutes of recovery time.
“Magnetic seizure therapy holds promise of one day replacing electroconvulsive therapy as the gold standard for treatment-resistant depression,” says Dr. Burhan. If proven as a viable first-line treatment, MST would be very easy to implement in existing ECT clinics. MST would therefore be readily available to patients in need.
“We are on the leading edge of the field of brain stimulation for treatment-resistant depression in collaboration with CAMH and UBC,” says Dr. Burhan. “Our goal is to continue informing the care process through clinically-relevant research that serves patients, medical professionals and the public.”
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Clinical trial will evaluate new therapy for treatment-resistant depression as a result of bipolar disorder
Treatment-resistant depression is a severe form of illness that does not respond to traditional therapies like medication and counselling. It is particularly common in patients with depression from bipolar disorder who are left with limited treatment options.
“There are some mental illnesses that can become resistant to therapy, similar to how infections, for example, can become resistant to antibiotics,” explains Dr. Amer Burhan, researcher at Lawson Health Research Institute and neuropsychiatrist at St. Joseph’s Health Care London. “Patients with those illnesses need more options.”
Brain stimulation is a field that holds promise for this patient population.
“When people are in a state of depression, research shows their brain networks are not functioning properly,” says Dr. Burhan. “Brain stimulation aims to stimulate neurons in the brain to correct activity and improve patient outcomes.”
Through involvement in a national clinical trial, Dr. Burhan and his research team at Lawson are offering new hope with a treatment called magnetic seizure therapy (MST). The study is the first randomized controlled trial to examine the efficacy of MST for patients with treatment-resistant depression as a result of bipolar disorder.
For years electroconvulsive therapy (ECT), one form of brain stimulation, has been the gold standard for patients with treatment-resistant depression. ECT uses an electric field to induce a seizure that provides a therapeutic benefit by stimulating the brain. But while ECT is effective, many patients opt out of treatment due to stigma surrounding the therapy and its potential for cognitive side effects like disorientation and amnesia.
MST has emerged as a promising alternative. MST works in a similar way to ECT but uses a focused magnetic field as opposed to electricity. As a result, MST induces a more focused seizure to reduce the risk of cognitive side effects.

“Magnetic seizure therapy has already been shown as a promising treatment for major depressive disorder or unipolar depression,” explains Dr. Amer Burhan, local site lead for the clinical trial. “For the first time, we’re studying how effective the treatment is for depression as a result of bipolar disorder and whether it can reduce the risk of cognitive side effects associated with electroconvulsive therapy.”
The clinical trial is being led by the Centre for Addiction and Mental Health (CAMH) and will also be offered through Lawson and University of British Columbia (UBC) Hospital. Lawson researchers will invite approximately 30 eligible patients with treatment-resistant depression from bipolar disorder to participate in the trial at Parkwood Institute, a part of St. Joseph’s Health Care London.
Eligible patients will be randomized to receive either ECT or MST. Patients will be offered support throughout the study with the goal of improving patient outcomes in both groups. Patient outcomes will be compared to study the whether MST is effective and whether it is associated with reduced cognitive side effects.
MST will be delivered under anesthesia in 12 to 20 sessions. Sessions will last 10 to 15 minutes each with 60 to 90 minutes of recovery time.
“Magnetic seizure therapy holds promise of one day replacing electroconvulsive therapy as the gold standard for treatment-resistant depression, but we need to learn more about where it fits in our toolbox of potential treatments,” says Dr. Burhan.
If proven as a viable first-line treatment, MST would be very easy to implement in existing ECT clinics. MST would therefore be readily available to patients in need.
“We are on the leading edge of the field of brain stimulation for treatment-resistant depression in collaboration with CAMH and UBC,” says Dr. Burhan. “Our goal is to continue informing the care process through clinically-relevant research that serves patients, medical professionals and the public.”
Those who would like more information about the trial can email @email or @email.
Clinical use of EpiSign proven for diagnosing rare heritable disorders
LONDON, ON – A study led by researchers at Lawson Health Research Institute (Lawson) provides clinical validation of EpiSign, a molecular genomics test that diagnoses rare, heritable neurodevelopmental conditions.
Invented at Lawson by Dr. Bekim Sadikovic, the diagnostic test uses machine learning to analyze the EpiSign Knowledge Database. This database compiles information on rare genetic diseases using laboratory analyses of the epigenome from patients with suspected genetic abnormalities. The epigenome is a process that can change the expression of a gene without changing the gene sequence.
“Using 211 blood samples, we measured test performance and diagnostic yield in 207 subjects from two different cohorts,” explains Dr. Sadikovic, lead researcher at Lawson and Scientific and Clinical Director of the Verspeeten Clinical Genome Centre at London Health Sciences Centre (LHSC). The targeted cohort were subjects with previous genetic findings that were ambiguous or inconclusive. The screening cohort were those with clinical findings consistent with hereditary neurodevelopment syndromes but with no previous genetic findings.
“Of the 207 subjects tested, 57 were positive for a diagnostic episignature including 48 in the targeted cohort, and 8 in the screening cohort. Only four remained inconclusive after EpiSign analysis,” says Dr. Sadikovic. “This gives us strong evidence for the clinical use of EpiSign, as well as the ability to provide conclusive findings in the majority of subjects tested.”
While currently there are limited treatment options associated with many of these conditions,
providing a diagnosis can help physicians better predict the course of the disease, and allows for better planning and support for the patient. EpiSign is the only test in the world that has been clinically validated for testing these kinds of genetic disorders.
“Patients with rare diseases often wait years and undergo numerous exams and tests before receiving a correct diagnosis, if one is found at all,” says Matthew Tedder, PhD, staff scientist at the Greenwood Genetic Center, one of the EpiSign clinical testing laboratories. “EpiSign provides an additional high-yield diagnostic tool for clinicians to include in their evaluation of patients with undiagnosed diseases, providing better medical management for patients and hope for their families.”
The study, “Clinical epigenomics: genome-wide DNA methylation analysis for the diagnosis of Mendelian disorders", is published in February’s Genetics in Medicine and was completed in collaboration with the Greenwood Genetic Center and the University of Amsterdam.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca