Search
Search
Small box holds big promise in cardiac care
London, Ontario – For a non-descript box it wields a mighty name and even more impressive possibilities for people with heart disease. Called the AngioDefender, the machine – no bigger than a shoebox - holds much promise in the ability to personalize cardiac care, say researchers at Lawson Health Research Institute, the research arm of St. Joseph’s Health Care London.
St. Joseph’s Hospital in London is the only Canadian cardiac rehabilitation centre testing the AngioDefender, a non-invasive tool that can assess the health of blood vessels by using a simple blood pressure cuff. At the recent Canadian Cardiovascular Congress in Toronto, Lawson researchers presented findings of their study, which assessed the feasibility and reliability of the AngioDefender in patients undergoing cardiac rehabilitation.
“Right now everyone basically gets similar treatment in terms of maximizing therapy based on risk factor profiles,” says Dr. Neville Suskin, Lawson scientist and medical director of St. Joseph’s Cardiac Rehabilitation and Secondary Prevention Program. “With this machine, if it does what we hope it will do, it gives us insight into a person’s vascular health so that we can know if the treatment is working and adjust and individualize their care.”
Also key, says Dr. Suskin, is the machine can be used by any medical professional in any doctor’s office.
The AngioDefender system, manufactured by Everist Health, measures the health of the endothelium — the interior lining of blood vessels. Using a blood pressure cuff, the device runs through a series of inflations and deflations to analyze the endothelium’s response to changes in blood flow. When the blood pressure cuff is inflated, blood flow decreases and stops. When the blood pressure cuff deflates, blood flow increases and the main artery in the arm responds by getting bigger (dilating). How well it dilates is a sign of endothelial (vascular) health.
Using a specially designed data analysis algorithm, the AngioDefender system produces each patient’s “flow-mediated dilation” score. When the information is combined with the patient’s other risk factors, it calculates the patient’s vascular age. The whole process takes 15 to 20 minutes.
“The ability for a health professional to obtain a measure of vascular health in such a straightforward manner is very novel” says Dr. Suskin, whose team has found that the machine is feasible to use in a busy cardiac rehabilitation practice setting. “It doesn’t take long, patients tolerate it, and they are also very keen to know their vascular health as determined by this machine.”
If successful, the device may become part of the standard screening to assess early-stage cardiovascular disease and atherosclerosis, and an innovative way to monitor the effectiveness of treatment.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Renowned for compassionate care, St. Joseph’s Health Care London is a leading academic health care centre in Canada dedicated to helping people live to their fullest by minimizing the effects of injury, disease and disability through excellence in care, teaching and research. Through partnership with Lawson Health Research Institute and our collaborative engagement with other health care and academic partners, St. Joseph’s has become an international leader in the areas of: chronic disease management; medical imaging; specialized mental health care; rehabilitation and specialized geriatrics; and surgery. St. Joseph’s operates through a wide range of hospital, clinic and long-term and community-based settings, including: St. Joseph’s Hospital; Parkwood Institute; Mount Hope Centre for Long Term Care; and the Southwest Centre for Forensic Mental Health Care. www.sjhc.london.on.ca
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Smart Homes for community living
A first-of-its-kind research study by Lawson Health Research Institute is moving into the community and evaluating the use of smart technologies in the home for people with severe mental illness.
After prototyping this approach within a hospital setting through St. Joseph’s Health Care London, the research team will be outfitting eight affordable housing units at Canadian Mental Health Association Middlesex and London and Middlesex Community Housing with smart home technology.

In-hospital prototype for using smart technologies in the home
The Smart Home Community Model
“This solution is for people who are having difficulty managing their everyday life and need a high level of care to maintain community living,” says Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and project lead for the Smart Home Community Model. “Technology and applications are being embedded in the lived environment and then tested to ensure they are safe, secure and appropriate for use in health care.”
Dr. Cheryl Forchuk announcing this phase of the project, from within one of the apartment buildings.
Study participants will select from a wide range of tools that will best meet their individual needs. Devices such as smartphones and touch-screen monitors connect with applications to provide video-conferencing, questionnaires, and prompts and reminders based on the person’s care plan.
As an example, participants have regular access to mood scales with questions about how they are feeling. These are used extensively in mental health care settings to help address issues and start conversations with clients. The care team receives notification of the answers, giving regular insight into how the person is doing and if they need additional follow-up.

Depending on their needs, participants have access to automated medication dispensers and smart health monitoring devices, such as weigh scales, blood pressure monitors, glucometers, and tracking monitors for heart rate, activity and sleep.
This patient population often faces health challenges on multiple fronts, with higher rates of diabetes and cardiac issues. They can struggle keeping balance when it comes to activity, weight and sleep. Fluctuations in any of these can be early indicators that a crisis is looming.

“By integrating and testing these smart tools for health care, we are not simply looking at the technology but how it can be used as a tool for communication,” says Dr. Forchuk. “We see smart technology supporting more seamless communication between health care providers and the client – all from their own homes. This helps them better manage their care and overall wellbeing, flag issues earlier on and avoid trips to the clinic when appropriate.”
Paula's Perspective
Paula Rawlinson is chair of the family council and sits on the patient council for St. Joseph’s Parkwood Institute Mental Health Care. She personally has lived experience with mental health and as also acted as a caregiver for a family member.
“Both myself and my family member could have benefitted from these tools, very much so,” says Paula. “When I was really suffering, I isolated myself from people a lot. Even when I lived in a group home because I needed a higher level of care. Having some sort of helpful device right there, encouraging me to keep up with things and connecting me to someone I trusted, would have made a huge difference. Especially after the first discharge.”

She adds that for someone who is really struggling, this could be a life-saving strategy that makes a vital difference.
For her family member, Paula sees many uses for these tools and knows that they would actually use them. “I’ve been able to see the tools and they are even simpler than using email. It makes them accessible to a lot of people in the community who would make good use of them to improve their situation.”
Results and Impact
Some of the tools as part of this project have previously been tested formally as part of a research study and shown positive results.
The health team has access to the data to more easily stay in touch with the person. They can work together to track trends and pinpoint triggers, creating more personalized and effective strategies. With less focus on the daily aspects of care, providers reported that in-person meetings offered more meaningful and important discussions.
“All of the data is also viewable by the client who continues to work with a health care provider,” explains Dr. Forchuk. Clients can reach out sooner and get support more quickly. Potential issues and crisis are addressed earlier on, and in previous studies they reduced psychiatric readmissions, emergency room visits and arrests. Clients reported more satisfaction with their care and feeling better overall.

“When we have more people successfully achieving community living and managing their care with fewer outpatient visits and other service utilization, we can open up capacity in the system and deliver quality care at a lower cost.”
The team anticipates that participants will experience greater levels of independence and autonomy in maintaining housing and self-care for mental health and chronic illnesses.
Paul points out that one of the key outcomes is to avoid re-admission. “One of the main, recurring struggles is loneliness. With tools to keep people in more regular contact with their care team and assistance with their everyday life, they can shift more to having a fun life. You can build up those crucial relationships with family and friends – and those people feel less burnout as caregivers. It adds a lot of support and resiliency.”

Dr. Forchuk adds that “our approach is to care for the whole person – mind, body and soul. It goes beyond managing the mental illness and is about supporting people in managing their life.”
The team already has four people enrolled in the study. In addition to people living alone, they will have participants with roommates and families to test the strategy under various real-life situations. The initial study will take place over one year.
This phase of project has received generous funding from the Canada Mortgage and Housing Corporation. The Canadian Institutes for Health Research contributed to the initial pilot phase.
Smart technology in the home effective for supporting mental health care, study finds
A research team from Lawson Health Research Institute has announced promising results from a one-of-a-kind demonstration study that evaluated the use of smart technologies in the home for people with severe mental illness.
“Our Smart Homes solution is for people who are having difficulty managing their everyday life and need a high level of care to maintain community living,” says Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and project lead for Smart Home Community Model Phase.
“We have strong initial evidence showing that technology and applications embedded in the lived environment are safe, secure and appropriate for use in health care.”
After prototyping this approach within a hospital setting through St. Joseph’s Health Care London, the research team outfitted affordable housing units at Canadian Mental Health Association (CMHA) Elgin-Middlesex and London and Middlesex Community Housing (LMCH) with smart home technology.
The team presented the full study results during a virtual event.
There were 13 participants as part of this project phase who had different living situations such as individual apartments, group homes or family homes. Anxiety, mood and psychotic disorders were the most common mental health diagnoses, with many also suffering from chronic pain that make the activities of daily life difficult.

Each study participant selected from a wide range of tools that would best meet their individual needs, with all but one participant selecting more than one tool. Devices such as smartphones and touch-screen monitors connect with applications to provide video-conferencing, questionnaires, and prompts and reminders based on the person’s care plan. They also had access to automated medication dispensers and smart health monitoring devices for tracking heart rate, activity and sleep.
“All of the data is viewable by both the client and health care provider, allowing for more seamless care and identification of issues earlier on,” adds Dr. Forchuk.
The study found that visits to a health or social service provider and the emergency department decreased, as did home visits from a provider. Telephone appointments increased and communication between the client and provider were enhanced. Almost 80 per cent of the participants felt that the technologies improved their health care overall.
Higher levels of community integration and a greater sense of independence were also reported, including a better ability to remain connected with friends and family during the pandemic. When medication dispensers were used, no medication doses were missed. Participants felt they were better able to track their own health and more motivated to lead healthier lives.
“The compliment of smart technology in our Supportive Independent Living Program has proven to improve the quality of life of participants by reducing use of emergency services and fostering learning opportunities for independent living skills to create a good quality of life,” says Nedrita Shemshedini, Manager of Supportive Independent Living at CMHA Elgin-Middlesex. “In a large-scale rollout, this model could improve wellbeing and empower persons to better manage their care.”
The research team hopes this work will help inform the integration of smart technology more fully into mental health care delivery. Laura Pearson, Executive Director at Ontario Peer Development Initiative, urges that “there is a need for key policies to be addressed and changed in order to support funding and access for technology at a system level for the purpose of mental health care.”
The community model phase of the Smart Homes project was generously funded by the Canada Mortgage and Housing Corporation (CMHC).
Smart technology in the home effective for supporting mental health care, study finds
LONDON, ON – A research team from Lawson Health Research Institute has announced promising results from a one-of-a-kind demonstration study that evaluated the use of smart technologies in the home for people with severe mental illness.
“Our Smart Homes solution is for people who are having difficulty managing their everyday life and need a high level of care to maintain community living,” says Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and project lead for Smart Home Community Model Phase. “We have strong initial evidence showing that technology and applications embedded in the lived environment are safe, secure and appropriate for use in health care.”
After prototyping this approach within a hospital setting through St. Joseph’s Health Care London, the research team outfitted affordable housing units at Canadian Mental Health Association (CMHA) Elgin-Middlesex and London and Middlesex Community Housing (LMCH) with smart home technology.
There were 13 participants as part of this project phase who had different living situations such as individual apartments, group homes or family homes. Anxiety, mood and psychotic disorders were the most common mental health diagnoses, with many also suffering from chronic pain that make the activities of daily life difficult.
“More and more, smart technologies like phone applications or virtual care are being used for mental health care. A smart home solution like the one we have tested could be considered a higher dose of technology, offered to clients with higher needs. The right dose for one may not work for another – the technological solutions used should vary depending on the individual,” explains Dr. Forchuk.
Each study participant selected from a wide range of tools that would best meet their individual needs, with all but one participant selecting more than one tool. Devices such as smartphones and touch-screen monitors connect with applications to provide video-conferencing, questionnaires, and prompts and reminders based on the person’s care plan. They also had access to automated medication dispensers and smart health monitoring devices for tracking heart rate, activity and sleep.
“All of the data is viewable by both the client and health care provider, allowing for more seamless care and identification of issues earlier on,” adds Dr. Forchuk.
The study found that visits to a health or social service provider and the emergency department decreased, as did home visits from a provider. Telephone appointments increased and communication between the client and provider were enhanced. Almost 80 per cent of the participants felt that the technologies improved their health care overall.
Higher levels of community integration and a greater sense of independence were also reported, including a better ability to remain connected with friends and family during the pandemic. When medication dispensers were used, no medication doses were missed. Participants felt they were better able to track their own health and more motivated to lead healthier lives.
“The compliment of smart technology in our Supportive Independent Living Program has proven to improve the quality of life of participants by reducing use of emergency services and fostering learning opportunities for independent living skills to create a good quality of life,” says Nedrita Shemshedini, Manager of Supportive Independent Living at CMHA Elgin-Middlesex. “In a large-scale rollout, this model could improve wellbeing and empower persons to better manage their care.”
The research team hopes this work will help inform the integration of smart technology more fully into mental health care delivery. Laura Pearson, Executive Director at Ontario Peer Development Initiative, urges that “there is a need for key policies to be addressed and changed in order to support funding and access for technology at a system level for the purpose of mental health care.”
The community model phase of the Smart Homes project was generously funded by the Canada Mortgage and Housing Corporation (CMHC).
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Specialized diabetes care may help prevent recurrent emergency department visits
One in three Canadians is living with diabetes or prediabetes. When they experience complications like severe hyperglycemia (high blood sugar), they require emergency care. For many, one emergency department (ED) visit leads to multiple others.
“There’s an increasing prevalence of diabetes in our population. It’s imperative that we support patients in managing the disease to prevent adverse outcomes and optimize health,” says Dr. Justin Yan, Associate Scientist at Lawson Health Research Institute and Emergency Department Physician at London Health Sciences Centre (LHSC). “In our research, we wanted to see whether specialized diabetes care was associated with a reduction in recurrent ED visits and hospitalizations.”
Dr. Yan and his colleagues studied de-identified data from patients who presented with hyperglycemia to the EDs at LHSC’s Victoria and University Hospitals over a one-year period. They compared those patients who had been followed by specialized diabetes care at St. Joseph’s Health Care London (250 patients) to those who had not (206 patients).
At St. Joseph’s Centre for Diabetes, Endocrinology and Metabolism, patients with diabetes are supported by a dedicated team of endocrinologists, family physician diabetologists, certified diabetes educators (registered nurses and dietitians), nurse practitioners, pharmacists, social workers and social service workers. The multidisciplinary team provides specialized care and comprehensive teaching which includes diet and lifestyle management advice, exercise programs, help with medications and more.
“Our team provides patient-centered multidisciplinary support to patients with diabetes” says Dr. Selina Liu, Associate Scientist at Lawson, Endocrinologist at St. Joseph’s and co-investigator on the study. “We work with patients to empower them to manage their diabetes with a goal of preventing serious complications, both acute and chronic, including those that can lead to ambulance calls, ED visits and hospitalizations.”
The research team found that patients who had received specialized diabetes care were less likely to revisit the ED due to hyperglycemia (9.6 per cent versus 32.5 per cent) and to be hospitalized due to hyperglycemia (5.2 per cent versus 14.1 per cent) within 30 days of their initial ED visit.
“While further research is needed, our findings are important for a number of reasons,” notes Dr. Yan. “They suggest that follow-up with specialized diabetes care may prevent recurrent ED visits and hospitalizations. In addition to improving patient outcomes, this could equate to significant cost savings for the health care system.”
The team hopes this knowledge can be used to develop targeted interventions for patients who are at higher risk of returning to hospital for hyperglycemia. They are planning future studies to look at what factors contribute to a patient being at higher risk of adverse outcomes and what interventions are most effective in preventing them.
The study, “Do adult patients with type 1 or 2 diabetes who present to the emergency department with hyperglycemia have improved outcomes if they have access to specialized diabetes care?,” is published in the Canadian Journal of Diabetes. It was funded by Lawson Health Research Institute’s Internal Research Fund.
Specific type of inflammation may be linked to risk of colorectal cancer
LONDON, ON – In a new preclinical study published in the journal Gastroenterology, researchers at Lawson Health Research Institute and Western University have found that a specific type of inflammation may be associated with an increased risk of colorectal cancer.
Colorectal cancer is the second most common cancer in Canada and one of the leading causes of cancer death. One of the major risk factors is inflammation caused by illnesses like colitis, Crohn’s disease or other forms of inflammatory bowel disease (IBD).
Previous studies have shown that the degree of inflammation caused by colitis is an important indicator of the risk of a patient developing colorectal cancer. In this study, researchers from Lawson and Western’s Schulich School of Medicine & Dentistry studied six different types of colitis – which result in different forms of inflammation – to assess whether certain types were associated with a higher risk of cancer.
“We found it wasn't necessarily the severity and duration of the inflammation that was most important, but rather the type of inflammation,” says Dr. Samuel Asfaha, a Lawson Scientist, Gastroenterologist at London Health Sciences Centre (LHSC) and Associate Professor at Schulich.
The team found that only one type of colitis led to cancer in preclinical models. They identified a new subset of immune cells called macrophages that were critical to the development of cancer. They also found that if they blocked these specific immune cells, they could prevent colitis-associated cancer.
“To our knowledge this is the first published study that extensively compares the different models of colitis or inflammation in the colon,” says Dr. Alice Shin, lead author on the study, which she worked on as PhD student at Schulich. “We are also the first to show that this specialized subset of macrophages that we identified are important for the initiation phase of inflammation-associated cancer.”
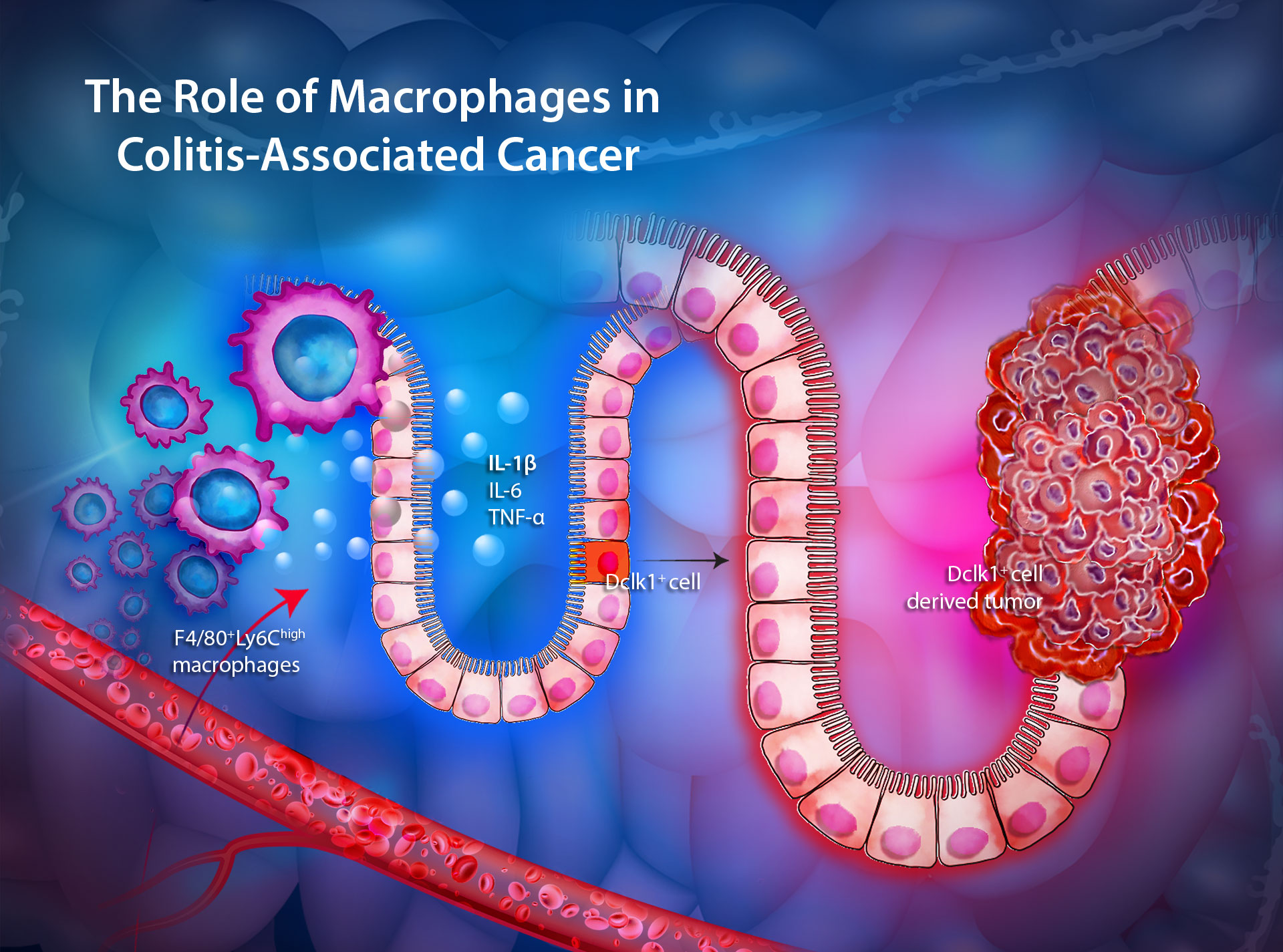
The next steps are to understand what the macrophages are doing to initiate cancer and whether a biomarker could be found that would identify which patients with chronic inflammation are at higher risk of developing cancer.
“Patients who have chronic inflammation often must undergo annual cancer surveillance,” Dr. Asfaha says. “By being able to differentiate those who are most at risk for developing cancer versus those who are who are at lower risk, we can focus our attention on those who are at increased risk.”
There is hope that further study could also lead to an understanding of whether certain treatments are more effective for colitis-associated cancer as opposed to other non-hereditary (sporadic) colorectal cancers.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
St. Joseph’s in partnership with Lawson to become Canada’s first centre of excellence in molecular imaging and theranostics
In a Canadian first, Lawson Health Research Institute (Lawson) and St. Joseph’s Health Care London (St. Joseph’s), in partnership with GE HealthCare, will become a centre of excellence in personalized treatment of cancer and other diseases by advancing the powerful blend of precision diagnostic imaging and targeted therapy.
This rapidly emerging field of medicine is called molecular imaging and theranostics (MIT). Molecular imaging provides detailed imaging at the molecular level and theranostics is a term that combines the words therapeutics and diagnostics. Together, MIT is a two-pronged approach to diagnosing and treating cancers and other diseases that merges imaging with the use of radiotracers that can not only identify the location and extent of diseased tissues but also selectively destroy the abnormal cells while leaving surrounding healthy cells undamaged.

“The centre will confirm St. Joseph’s and the wider London medical and scientific community as national and international leaders in advancing MIT in the diagnosis of disease, for instance in the identification of cancer and its sub-types, to allow more treatment options for patients,” says Dr. Narinder Paul, Lawson Scientist, Chief, Medical Imaging at St. Joseph’s and Physician Executive, Medical Imaging at London Health Sciences Centre (LHSC). “It will also allow for an expansion of scientific collaborations, increased numbers of scientific and medical learners, and access to the latest software to acquire and integrate imaging science with other patient information.”
The partnership with GE HealthCare will see St. Joseph’s become the first hospital in Canada to install the latest generation, state-of-the-art PET-CT from GE, which will be delivered to St. Joseph’s Hospital by September 2023. The new PET-CT will mean faster exams, better patient experience, more detailed images and increased accuracy in diagnosing disease at a lower dose of radiation for patients. It will also expand clinical care at St. Joseph’s by significantly enhancing research through the Imaging Research Group at Lawson, working together with researchers at LHSC, the London Regional Cancer Program, and Western University.

“We will leverage the combined scientific expertise and innovation of scientists from GE HealthCare and Lawson to maximize the future opportunities of molecular imaging theranostics made possible through PET- CT imaging and be leaders in Canada in this area of medical science,” says Dr. David Hill (D.Phil), Lawson’s Scientific Director.
As a dedicated MIT centre of excellence, St. Joseph’s will…
• Advance innovation and expand the science in precision imaging of disease through Lawson, and broaden the potential of PET-CT imaging
• Develop new treatment options for patients with cancer and other diseases
• Examine how to maximize the opportunities of digital health technologies to improve access for patients across Canada and optimize their treatment journeys
• Create a knowledge dissemination hub for Canada to educate and train others in the use of advanced imaging technologies, including how to organize hospital services to maximize access to patients and improve the health care system for all Canadians.
“St. Joseph’s is proud to be in partnership with GE HealthCare on this exciting opportunity to transform the care journey and outcomes for patients with cancer and other diseases, not only locally and regionally, but also nationally,” says Roy Butler (PhD), President and CEO of St. Joseph’s.
For patients seen in London, the benefits will include expanded use of PET-CT, the ability to extract more information from their diagnostic images more rapidly and with less radiation exposure compared to current procedures, greater diagnostic and treatment accuracy, and new options for treatment, particularly for cancers that are more difficult to treat.
“A personalized approach to medical care requires a very detailed understanding of the localization of disease and potential response to different treatment options,” says Dr. Paul who is also the Chair of Medical Imaging at Schulich School of Medicine & Dentistry at Western University. “We will be able to offer patients across our region access to the latest therapeutic options based on a deeper understanding of the nature of their individual disease conditions gained through next generation medical imaging.”
At its core, theranostics is about treating each patient as an individual, “recognizing that the same treatment plan doesn’t work for everyone – with the goal of providing more efficient and effective medical care,” adds says Mike Hamilton, President, GE HealthCare Canada. “This collaboration aims to advance this practice for the benefit of clinicians and patients around the world.”
St. Joseph’s and Lawson have invested in critical MIT infrastructure for more than two decades with an on-site cyclotron at St. Joseph’s Hospital, a radiochemistry laboratory, scientists to make the clinical grade reagents, Canada’s first PET-CT (2002), Canada’s first whole body PET-MRI (2012), and now Canada’s first next-generation PET-CT from GE HealthCare, says Dr. Ting-Yim Lee (PhD), Lawson’s Director of PET/CT Research and medical physicist at St. Joseph’s Hospital. There are also clinical trials research teams and state-of-the-art PET-CT cameras across London’s hospitals and Western, dedicated facilities at Western to develop new probes used to detect and diagnose disease, and the London Regional Cancer Program at LHSC.
In addition, there has been investment in research leadership roles through St. Joseph’s Health Care Foundation. Three donor-funded research chairs will be contributing to this important work.
“This makes the city the obvious location to maximize the development of this exciting new science for the benefit of patients,” says Dr. Lee. “London has an established record of working in partnership with global companies in the field of medical imaging and have together generated many discoveries that are now made available as best patient care.”
The new PET-CT at St. Joseph’s will replace an aging machine and has been made possible in part through the generosity of donors to St. Joseph’s Health Care Foundation, which is contributing $1 million to state-of-the-art machine.
St. Joseph’s in partnership with Lawson will become Canada’s first centre of excellence in molecular imaging and theranostics
London, Ontario – In a Canadian first, St. Joseph’s Health Care London (St. Joseph’s) and Lawson Health Research Institute (Lawson), in partnership with GE HealthCare, will become a centre of excellence in personalized treatment of cancer and other diseases by advancing the powerful blend of precision diagnostic imaging and targeted therapy.
This rapidly emerging field of medicine is called molecular imaging and theranostics (MIT). Molecular imaging provides detailed imaging at the molecular level and theranostics is a term that combines the words therapeutics and diagnostics. Together, MIT is a two-pronged approach to diagnosing and treating cancers and other diseases that merges imaging with the use of radiotracers that can not only identify the location and extent of diseased tissues but also selectively destroy the abnormal cells while leaving surrounding healthy cells undamaged.
“The centre will confirm St. Joseph’s and the wider London medical and scientific community as national and international leaders in advancing MIT in the diagnosis of disease, for instance in the identification of cancer and its sub-types, to allow more treatment options for patients,” says Dr. Narinder Paul, Lawson Scientist, Chief, Medical Imaging at St. Joseph’s and Physician Executive, Medical Imaging at London Health Sciences Centre (LHSC). “It will also allow for an expansion of scientific collaborations, increased numbers of scientific and medical learners, and access to the latest software to acquire and integrate imaging science with other patient information.”
The partnership with GE HealthCare will see St. Joseph’s become the first hospital in Canada to install the latest generation, state-of-the-art PET-CT from GE, which will be delivered to St. Joseph’s Hospital by September 2023. The new PET-CT will mean faster exams, better patient experience, more detailed images and increased accuracy in diagnosing disease at a lower dose of radiation for patients. It will also expand clinical care at St. Joseph’s by significantly enhancing research through the Imaging Research Group at Lawson, working together with researchers at LHSC, the London Regional Cancer Program, and Western University.
“We will leverage the combined scientific expertise and innovation of scientists from GE HealthCare and Lawson to maximize the future opportunities of molecular imaging theranostics made possible through PET- CT imaging and be leaders in Canada in this area of medical science,” says Dr. David Hill (D.Phil), Lawson’s Scientific Director.
As a dedicated MIT centre of excellence, St. Joseph’s will…
• Advance innovation and expand the science in precision imaging of disease through Lawson, and broaden the potential of PET-CT imaging
• Develop new treatment options for patients with cancer and other diseases
• Examine how to maximize the opportunities of digital health technologies to improve access for patients across Canada and optimize their treatment journeys
• Create a knowledge dissemination hub for Canada to educate and train others in the use of advanced imaging technologies, including how to organize hospital services to maximize access to patients and improve the health care system for all Canadians.
“St. Joseph’s is proud to be in partnership with GE HealthCare on this exciting opportunity to transform the care journey and outcomes for patients with cancer and other diseases, not only locally and regionally, but also nationally,” says Roy Butler (PhD), President and CEO of St. Joseph’s.
For patients seen in London, the benefits will include expanded use of PET-CT, the ability to extract more information from their diagnostic images more rapidly and with less radiation exposure compared to current procedures, greater diagnostic and treatment accuracy, and new options for treatment, particularly for cancers that are more difficult to treat.
“A personalized approach to medical care requires a very detailed understanding of the localization of disease and potential response to different treatment options,” says Dr. Paul who is also the Chair of Medical Imaging at Schulich School of Medicine & Dentistry at Western University. “We will be able to offer patients across our region access to the latest therapeutic options based on a deeper understanding of the nature of their individual disease conditions gained through next generation medical imaging.”
At its core, theranostics is about treating each patient as an individual, “recognizing that the same treatment plan doesn’t work for everyone – with the goal of providing more efficient and effective medical care,” adds says Mike Hamilton, President, GE HealthCare Canada. “This collaboration aims to advance this practice for the benefit of clinicians and patients around the world.”
The new PET-CT at St. Joseph’s will replace an aging machine and has been made possible in part through the generosity of donors to St. Joseph’s Health Care Foundation, which is contributing $1 million to state-of-the-art machine.
Additional details on this exciting partnership are available on St. Joseph’s website
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Renowned for compassionate care, St. Joseph’s Health Care London is a leading academic health care centre in Canada dedicated to helping people live to their fullest by minimizing the effects of injury, disease and disability through excellence in care, teaching and research. Through partnership with Lawson Health Research Institute and our collaborative engagement with other health care and academic partners, St. Joseph’s has become an international leader in the areas of: chronic disease management; medical imaging; specialized mental health care; rehabilitation and specialized geriatrics; and surgery. St. Joseph’s operates through a wide range of hospital, clinic and long-term and community-based settings, including: St. Joseph’s Hospital; Parkwood Institute; Mount Hope Centre for Long Term Care; and the Southwest Centre for Forensic Mental Health Care. www.sjhc.london.on.ca
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
St. Joseph’s launches Health Crisis Fund to support local COVID-19 research
LONDON, ON – St. Joseph’s Health Care London and Lawson Health Research Institute have announced plans to move forward with clinical trials testing a drug that could potentially be used to prevent and treat COVID-19. St. Joseph’s Health Care Foundation will accelerate the creation of the studies by providing seed funding to get the research started through donor support. Based on the immediate need, The St. Joseph’s Health Crisis Fund has been created by St. Joseph’s Health Care Foundation to enable these and other research studies currently in development through Lawson, the research arm of St. Joseph’s.
While supporting urgent COVID-19 clinical trials will be an immediate focus, The St. Joseph’s Health Crisis Fund will also support critical patient care equipment and care and comfort items for healthcare staff and volunteers working on the frontlines of the pandemic across St. Joseph’s.
The initial clinical trials aim to study the use of hydroxychloroquine as a preventative medication and treatment for COVID-19. Led locally by Dr. Michael Silverman, Medical Director of St. Joseph’s Infectious Diseases Care Program, one trial will assess the safety and efficacy of using the drug to prevent COVID-19 in health care workers recently exposed to the virus. This trial will also assess the drug as a treatment for non-hospitalized patients with mild cases of the illness. St. Joseph’s will be one of many participating sites in the trial, which is being led by the Research Institute of the McGill University Health Centre.
“There is much debate surrounding the drug hydroxychloroquine. We do not yet know whether it’s safe or effective, and it should not be routinely recommended until we do,” says Dr. Silverman, also a Lawson Associate Scientist and city-wide Chair/Chief of Infectious Diseases. “We plan to carefully study the drug through a randomized controlled trial and assess whether it can help combat COVID-19.”
Dr. Silverman is also partnering with Dr. Michael Borrie, Geriatrician at St. Joseph’s and Lawson Scientist, on a prevention trial to test the safety and efficacy of the drug for patients and residents at Parkwood Institute who have been exposed to COVID-19. They are at a higher risk of infection, as well as serious complications and potential admission to acute care.
“Lawson researchers like Drs. Silverman and Borrie excel in rapid response research,” says Dr. David Hill, Lawson Scientific Director. “Hospital-based research is uniquely positioned to handle these types of studies, as close proximity to patients and sample collection is essential.”
St. Joseph’s Infectious Diseases Program is the only program of its kind in the region. Dr. Silverman, head of St. Joseph’s Infectious Disease program, has worked with communities in crisis in Zambia, Zimbabwe, Uganda and the rainforests of Guyana. He is working closely with other health care partners in the London and surrounding area to coordinate the region’s response to the COVID-19 pandemic.
“The Sisters of St. Joseph, who founded our organization, faced contagious diseases and other pandemics at different times in our 150+ year history,” says Michelle Campbell. “Today, it’s a different time, and a new disease. Now, more than ever, we ask our community to help us address the crisis facing us all.”
Those interested in donating to St. Joseph’s Health Crisis Fund are asked to visit St. Joseph’s Health Care Foundation’s website to learn more at sjhcfoundation.org. Donations can be made online, through direct mail submissions or by calling the Foundation directly at 519-646-6085.
-30-
Renowned for compassionate care, St. Joseph’s Health Care London is a leading academic health care centre in Canada dedicated to helping people live to their fullest by minimizing the effects of injury, disease and disability through excellence in care, teaching and research. Through partnership with Lawson Health Research Institute and our collaborative engagement with other health care and academic partners, St. Joseph’s has become an international leader in the areas of: chronic disease management; medical imaging; specialized mental health care; rehabilitation and specialized geriatrics; and surgery. St. Joseph’s operates through a wide range of hospital, clinic and long-term and community-based settings, including: St. Joseph’s Hospital; Parkwood Institute; Mount Hope Centre for Long Term Care; and the Southwest Centre for Forensic Mental Health Care. www.sjhc.london.on.ca
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
St. Joseph’s Health Care Foundation gathers, grows and grants philanthropic funds to enable St. Joseph’s Health Care London to pursue excellence in care, teaching and research. Through donor support, the foundation contributes to advances in the delivery of patient care, specialized equipment, research initiatives and capital funds at St. Joseph’s Hospital, Parkwood Hospital, Mount Hope Centre for Long Term Care, Regional Mental Health Care London and Southwest Centre for Forensic Mental Health Care and Lawson Health Research Institute. As one of the largest charitable organizations in Southwestern Ontario, St. Joseph’s Health Care Foundation is an accredited member of Imagine Canada’s Ethical Trustmark Program, which recognizes the foundation’s commitment to ethical fundraising and donor accountability. www.sjhcfoundation.org
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca