Search
Search
Study aiming to slow cognitive decline in older adults gets $1.5M
LONDON, ON - Led by Dr. Manuel Montero-Odasso and his team at Lawson Health Research Institute, the first large-scale Canadian clinical trial using personalized lifestyle intervention delivered at home to help older adults with mild cognitive impairment is getting underway with support from a Weston Foundation grant of $1.5 million.
Mild cognitive impairment (MCI) is an intermediate stage between the expected cognitive decline of normal aging and the more serious decline of dementia. There is growing evidence that enhancing physical activity, stimulating cognitive training and addressing cardiovascular factors could delay or prevent the decline to dementia.
Part of the Canadian Consortium on Neurodegeneration in Aging (CCNA), the SYNERGIC-2 trial will provide virtual at-home interventions to 550 study participants with MCI, including personalized one-on-one coaching, to help make lifestyle and behavioural changes. This trial builds upon the successful SYNERGIC-1 trial, which used face-to-face interventions, by delivering them remotely using digital technology.
These interventions will target five areas including physical exercise, cognitive training, diet recommendations, sleep interventions and vascular risk factor management, with the goal of enhancing health and maintaining independence for individuals at risk for developing dementia.

“There are important risk factors related to exercise, diet, sleep and socialization,” says Dr. Montero-Odasso, Lawson Scientist, Geriatrician at St. Joseph’s Health Care London’s Parkwood Institute and a Professor at Western University. “If we can make the brain a little healthier with multiple lifestyle interventions, we may be able to delay or even prevent dementia.”
The year-long study includes 35 researchers recruiting a diverse population of older adults with MCI across 10 Canadian cities. The research teams are currently looking for participants ages 60-85 with MCI and additional dementia risk factors.
Researchers have created a digital platform to deliver the interventions at home with effective coaching strategies that will help to overcome barriers to lifestyle interventions, like difficulty accessing intervention sites, lack of time to attend gym sessions or living in rural/remote areas.
“There are many Canadians who are at high risk of developing dementia, based on their family history and genetics,” explains Dr. Howard Chertkow, Chair of Cognitive Neurology and Innovation at Baycrest Health Sciences, Scientific Director at CCNA and a co-investigator on the study. “Other risk factors include having high blood pressure and diabetes. We have seen that we can reduce the risk of getting dementia if we can get people to improve their lifestyles in multiple ways.”
Those interested in taking part in the study can contact @email for additional details.
The study is part of a global initiative known as World-Wide FINGERS, an interdisciplinary network working on the prevention of cognitive impairment and dementia, and is supported by The Gray Centre for Mobility and Activity at St. Joseph’s.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Study aiming to slow cognitive decline in older adults gets $1.5M
Led by Dr. Manuel Montero-Odasso and his team at Lawson Health Research Institute, the first large-scale Canadian clinical trial using personalized lifestyle intervention delivered at home to help older adults with mild cognitive impairment is getting underway with support from a Weston Foundation grant of $1.5 million.
Mild cognitive impairment (MCI) is an intermediate stage between the expected cognitive decline of normal aging and the more serious decline of dementia. There is growing evidence that enhancing physical activity, stimulating cognitive training and addressing cardiovascular factors could delay or prevent the decline to dementia.
Part of the Canadian Consortium on Neurodegeneration in Aging (CCNA), the SYNERGIC-2 trial will provide virtual at-home interventions to 550 study participants with MCI, including personalized one-on-one coaching, to help make lifestyle and behavioural changes. This trial builds upon the successful SYNERGIC-1 trial, which used face-to-face interventions, by delivering them remotely using digital technology.
These interventions will target five areas including physical exercise, cognitive training, diet recommendations, sleep interventions and vascular risk factor management, with the goal of enhancing health and maintaining independence for individuals at risk for developing dementia.

“There are important risk factors related to exercise, diet, sleep and socialization,” says Dr. Montero-Odasso, Lawson Scientist, Geriatrician at St. Joseph’s Health Care London’s Parkwood Institute and a Professor at Western University. “If we can make the brain a little healthier with multiple lifestyle interventions, we may be able to delay or even prevent dementia.”
The year-long study includes 35 researchers recruiting a diverse population of older adults with MCI across 10 Canadian cities. The research teams are currently looking for participants ages 60-85 with MCI and additional dementia risk factors.
Researchers have created a digital platform to deliver the interventions at home with effective coaching strategies that will help to overcome barriers to lifestyle interventions, like difficulty accessing intervention sites, lack of time to attend gym sessions or living in rural/remote areas.
“There are many Canadians who are at high risk of developing dementia, based on their family history and genetics,” explains Dr. Howard Chertkow, Chair of Cognitive Neurology and Innovation at Baycrest Health Sciences, Scientific Director at CCNA and a co-investigator on the study. “Other risk factors include having high blood pressure and diabetes. We have seen that we can reduce the risk of getting dementia if we can get people to improve their lifestyles in multiple ways.”
Those interested in taking part in the study can contact @email for additional details.
The study is part of a global initiative known as World-Wide FINGERS, an interdisciplinary network working on the prevention of cognitive impairment and dementia, and is supported by The Gray Centre for Mobility and Activity at St. Joseph’s.
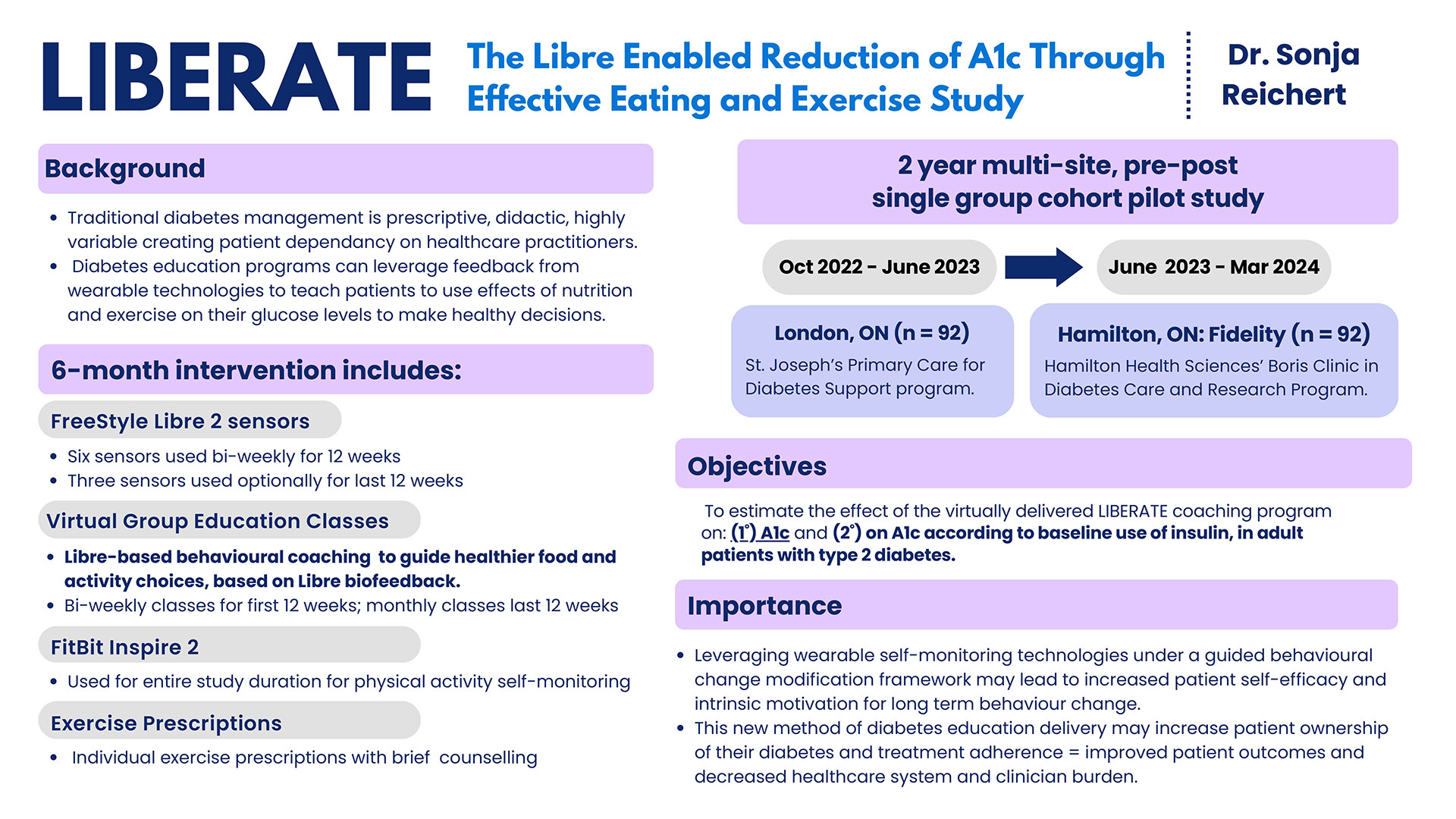
Study aims to empower patients with Type 2 diabetes to take control of their health
Through a novel, virtual coaching approach, researchers at Lawson Health Research Institute are aiming to improve the lives of patients with Type 2 diabetes by helping them learn to manage their blood glucose levels (A1c) through self-monitoring, healthy nutrition and exercise, with wearable technology providing real-time motivation.
The study, called LIBERATE (LIBre-Enabled Reduction of A1c Through Effective Eating and Exercise), will personalize diabetes management to each patient, recognizing there is no one-size-fits-all solution for people living with diabetes and the best food and activity strategy varies from person to person.

“The study uses a flash glucose device that's worn on the arm for two weeks and allows a user to scan their blood glucose as many times as they want. Participants also wear a fitness tracker that, together with the glucose monitor, provides real-time ‘biofeedback’ as to how food and activity are affecting glucose levels,” explains Dr. Sonja Reichert, Scientist at Lawson and Physician with the Primary Care Diabetes Support Program of St. Joseph’s Health Care London.
The research team is looking to recruit 92 people that have never before used Abbott's Freestyle LIBRE system, have an A1c above 8% in the last three months and have access to a computer or smartphone and the internet for the six-month study. After an initial in-person assessment, participants will be asked to join in biweekly virtual group education classes and offered brief exercise coaching as well, if interested.
The goal is to use the wearable technology to encourage patient-driven lifestyle changes based on monitoring how their own food and activity patterns impact their glucose levels – changes they choose themselves and that can be maintained in the long term versus the traditional more prescriptive approach to eating and exercise.
Researchers believe a combination of glucose monitoring, health coaching, behavior change support and technology could lead to the development of a toolkit that could be used by other diabetes management centres across Canada.
“We feel strongly that technology on its own is great,” says Dr. Reichert. “But the real magic happens when you have health care providers to motivate and teach, and provide a clear understanding of all this data and how it applies to each individual. That's what we're looking to do with LIBERATE.”
Anyone interested in participating can visit https://www.liberatediabetes.ca/ or reach out to the study team at 519-646-6000 ext. 67230 or email @email
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Study aims to empower patients with Type 2 diabetes to take control of their health
LONDON, ON – Through a novel, virtual coaching approach, researchers at Lawson Health Research Institute are aiming to improve the lives of patients with Type 2 diabetes by helping them learn to manage their blood glucose levels (A1c) through self-monitoring, healthy nutrition and exercise, with wearable technology providing real-time motivation.
The study, called LIBERATE (LIBre-Enabled Reduction of A1c Through Effective Eating and Exercise), will personalize diabetes management to each patient, recognizing there is no one-size-fits-all solution for people living with diabetes and the best food and activity strategy varies from person to person.
“The study uses a flash glucose device that's worn on the arm for two weeks and allows a user to scan their blood glucose as many times as they want. Participants also wear a fitness tracker that, together with the glucose monitor, provides real-time ‘biofeedback’ as to how food and activity are affecting glucose levels,” explains Dr. Sonja Reichert, Scientist at Lawson and Physician with the Primary Care Diabetes Support Program of St. Joseph’s Health Care London.

The research team is looking to recruit 92 people that have never before used Abbott's Freestyle LIBRE system, have an A1c above 8% in the last three months and have access to a computer or smartphone and the internet for the six-month study. After an initial in-person assessment, participants will be asked to join in biweekly virtual group education classes and offered brief exercise coaching as well, if interested.
The goal is to use the wearable technology to encourage patient-driven lifestyle changes based on monitoring how their own food and activity patterns impact their glucose levels – changes they choose themselves and that can be maintained in the long term versus the traditional more prescriptive approach to eating and exercise.
Researchers believe a combination of glucose monitoring, health coaching, behavior change support and technology could lead to the development of a toolkit that could be used by other diabetes management centres across Canada.
“We feel strongly that technology on its own is great,” says Dr. Reichert. “But the real magic happens when you have health care providers to motivate and teach, and provide a clear understanding of all this data and how it applies to each individual. That's what we're looking to do with LIBERATE.”
Anyone interested in participating can visit https://www.liberatediabetes.ca/ or reach out to the study team at 519-646-6000 ext. 67230 or email @email
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Study casts doubt on clinical significance of gadolinium brain deposits
A new study from Lawson Health Research Institute and the Institute for Clinical Evaluative Sciences (ICES) has cast doubt on the clinical significance of brain deposits of gadolinium (a chemical contrast agent commonly used to enhance MRI imaging).
In 2015, the US Food and Drug Administration raised safety concerns over reports of retained gadolinium in the brain for patients undergoing four or more gadolinium-enhanced MRIs. The FDA launched an inquiry at the time, stating that “it is unknown whether these gadolinium deposits are harmful.” Pending further investigation, the FDA suggested limiting the use of gadolinium-based contrast agents (GBCAs) to circumstances where contrast information is clinically necessary, and to evaluate the need for repetitive GBCA MRIs based on treatment protocols.
Studies since that time have shown deposits of gadolinium may be found long after they are administered. They tend to concentrate in the globus pallidi, a region of the brain that can cause parkinsonian symptoms if it is damaged. Parkinson’s disease is an example of a specific brain disorder that is commonly associated with parkinsonian symptoms.
“Given the concern around possible neurotoxicity of gadolinium, and because these deposits were found in the globus pallidi region of the brain, we wanted to see if people exposed to gadolinium MRIs have higher rates of subsequent parkinsonism,” says Dr. Blayne Welk, the lead author of the study who is an adjunct scientist with ICES Western and Lawson.
To test a possible link between GBCAs and parkinsonism, Welk and his team examined anonymized health care records for 246,557 patients in Ontario over the age of 66 who underwent an initial MRI in a 10-year period between 2003 and 2013. They excluded patients whose initial MRI was of the brain or spinal cord and those with prior parkinsonism or neurosurgery. Comparing patients who were exposed to gadolinium-enhanced MRIs with patients whose MRIs did not include gadolinium enhancement, they looked for differences in rates of future parkinsonism symptoms or treatment.
They found that the rates of parkinsonism for exposed vs non-exposed patients were virtually identical, at 1.2 per cent. These findings indicate that there is no increased risk for parkinsonism associated with the use of gadolinium in MRIs.
However, the researchers caution that this study does not clear up all the worries about gadolinium, since they investigated only its connection to parkinsonism.
“While these findings should be reassuring for patients and their care providers that gadolinium exposure does not appear to be associated with higher risk of developing parkinsonism symptoms, there have been other reports of nonspecific neurologic symptoms including pain and cognitive changes associated with prior gadolinium exposure which do require further study,” comments Dr. Welk.
The researchers also note that gadolinium may have different effects in younger patients (who were not included in this study), or in those with neurologic diseases (who may have been excluded based on the types of MRIs included in this study).
“Association between Gadolinium contrast exposure and the risk of parkinsonism” was published on July 5, 2016 in the journal JAMA.
Author block: Blayne Welk, Eric McArthur, Sarah A. Morrow, Penny MacDonald, Jade Hayward, Andrew Leung, Andrea Lum.
Study examines new forms of treatment for those suffering from post-traumatic stress disorder
Researchers looking to better personalize treatment for PTSD
MEDIA RELEASE
For immediate release
January 25th, 2022
LONDON, ON – Post-traumatic stress disorder (PTSD) is a condition that often develops in those who have experienced a traumatic event. PTSD affects close to 10 per cent of Canadians, and in some cases, can be difficult to treat.
In a new study through Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from PTSD.
“In our study we are looking at ways of trauma processing at the foundation of the stress response,” explains Dr. Ruth Lanius, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry. “When you are faced with a stressor the first thing you do is turn your attention to it, and when you do that you engage your head and neck muscles.”
DBR was developed by Scottish psychiatrist Dr. Frank Corrigan and focuses on the muscles of the shoulders, neck, head and face of patients when recalling a traumatic event. This form of trauma processing starts right at the moment the stressor is noticed by the individual, which is often quickly followed by a moment of shock. By addressing the stressor at this level, doctors can target the foundation of where the stress response begins.
“When patients bring up a trigger in their mind, we look at what happens in terms of the tension in their head and neck. We process that gently by asking the patient to notice and stay with that tension without trying to release it, and over time the tension usually decreases,” explains Dr. Lanius, who is also a Psychiatrist at London Health Sciences Centre. “The second part involves addressing the shock response. You turn your attention to the stressor and then notice any moments of shock that follows, which is often associated with tension behind the eyes and in the shoulders. Finally, you address the visceral sensations associated with feelings and emotions associated with the stressor.”
Dr. Lanius believes that by using DBR and focusing on muscle and visceral responses, it will help patients suffering from PTSD to process the visceral feelings associated with the trauma and its triggers.
“After this form of treatment, patients often say they feel safer and don’t see themselves negatively, like they did in the past,” says Dr. Lanius. “This is because we change those intense visceral feelings and it allows the person to reevaluate who they are and how they interact with the world.”
The research team is hoping to recruit approximately 60 people to take part in the DBR study. Participants will undergo a psychological interview and an MRI, then eight sessions of treatments. Following those sessions, participants will have another interview and MRI to assess if any positive changes were made within the neurological networks and/or in psychological systems.
“Our hopes are to really personalize treatment for those living with PTSD,” says Dr. Lanius. “Some people have difficulty tolerating some forms of trauma processing and in my experience this treatment is a gentler approach for those individuals.”
Interested participants who have been diagnosed with PTSD can contact Suzy Southwell, Research Coordinator, at 519-685-8500 ext. 35186 or @email.
MEDIA CONTACT
Celine Zadorsky, Communications & External Relations, Lawson Health Research Institute, T: 519-685-8500 ext. 75664, C: 519-619-3872
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world.
ABOUT WESTERN
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
ABOUT THE SCHULICH SCHOOL OF MEDICINE & DENTISTRY
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study examining moral injury in health care workers is focusing on functional brain changes
LONDON, ON – For many health care workers, the past year and a half of the COVID-19 pandemic has taken a toll on their mental health. Recognizing this is a growing concern, a London research team from Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry is examining moral injury amongst health care workers by imaging the effects on the brain.
“We are trying to look closely at what happens in the brain when a person recalls a moral injury event,” says Dr. Ruth Lanius, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry. “By understanding the changes happening in the brain, we may be better able to treat individuals suffering from moral injury.”
Moral injury refers to an injury to an individual’s moral conscious which can produce profound emotional guilt and shame. During this ongoing pandemic, some health care workers have experienced emotionally difficult situations that resulted in moral injury.
“Those suffering from moral injury have a cognitive or thinking component which may include repeated thoughts that they didn’t provide the best care for example, or that they let their family down do to their intense work schedule or need to self-isolated,” explains Dr. Lanius, who is also a psychiatrist at London Health Sciences Centre (LHSC). ‘These thoughts are coupled with intense visceral distress, a gnawing sensation in the stomach or the feeling like one is being eaten up inside. I think once we help resolve the visceral distress, we will also see the negative thinking patterns settle down.”
The new study will involve around 60 health care workers. These research participants will undergo a functional MRI scan at St. Joseph's Health Care London at the beginning of the study and have the option to receive eight weeks of treatment. Then, another MRI scan will be done to see if and how the moral injury changes and possibly resolves within the brain. “This can be very validating for the health care workers since brain scans can make the invisible wound of moral injury visible,” adds Dr. Lanius.
The research team’s goal is to better understand what networks of the brain are activated with moral injury. Dr. Lanius hopes this would help establish more neuroscientifically guided treatments. “We have to help our health care workers heal from the tremendous hardships they often endure.”
Health care workers are still being recruited for this study. Interested participants can contact Research Coordinator Suzy Southwell 519-685-8500 ext. 35186 or @email.
See all Lawson Media Releases
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study finds children in marginalized communities more likely to experience cardiac arrests
A new study shows children living in marginalized communities are at a higher risk of experiencing paediatric out-of-hospital cardiac arrest (POHCA) – a rare, life-threatening event occurring outside a hospital setting in which a child’s heart suddenly stops beating. It is estimated in other studies that the survival rate for POHCA is less than 10 per cent, and one-third of the children who survive POHCA will develop a significant neurological condition.
A province-wide case-control study from Western University, Lawson Health Research Institute and the Institute for Clinical Evaluative Sciences (ICES) addressed a gap in current literature related to how social determinants of health impact the risk of POHCA. The study was published in the Journal of the American Heart Association.
“We know the outcomes for children who experience POHCA are really poor. Most don’t survive, and those who do often develop new and severe neurological impairments,” said lead author Samina Idrees, an epidemiology and biostatistics Masters graduate, who completed the work while studying at Western. “Given the significance of this health outcome and its potential preventability, we wanted to investigate further and shed light on any potential disparities.”
The study established that the odds of POHCA were higher for children living in areas with the highest levels of material deprivation – which incorporates average income, education, the proportion of lone parent families and housing quality. The likelihood of experiencing POHCA was also greater for those living in urban centres in Northern Ontario (relative to those in urban centres in Southern Ontario) with a population greater than 10,000, rural areas in Southern Ontario, and in areas with highest levels of unpaid professions, unemployment or non-working age individuals, high levels of instability and lower levels of ethnic diversity.
“Racialized communities sometimes have higher risks for certain health conditions,” said Idrees, in reference to the finding that children living in areas with the lowest levels of ethnic diversity had a higher risk of POHCA. “However, these findings are in line with the finding that immigrants have a lower risk of experiencing POHCA relative to those born in the country, likely due to the healthy immigrant effect, where immigrants arriving in Canada are usually in good health.”
Most cases of POHCA are caused by respiratory failure, and cardiac arrests in children can be attributed to a wide range of preventable and unpreventable factors, including drowning, sudden infant death syndrome, accidental ingestion or existing medical conditions.
Dr. Janice Tijssen, senior author on the study, Associate Scientist at Lawson, Professor at Western and Adjunct Scientist at ICES, noted that while there is a variety of factors that may contribute to out-of-hospital cardiac arrests in children, a common theme was that kids living in these marginalized communities are at higher risk of experiencing cardiac arrest.

The case study group included 1,826 children, aged one day to 17 years, who were transported to an emergency department in Ontario after they suffered an out-of-hospital cardiac arrest between April 1, 2004 and March 31, 2020. The case study group was matched to a control group on a one-to-four ratio and researchers identified cases of POHCA using the National Ambulatory Care Reporting System – which contains data for hospital-based and community-based ambulatory care.
Solutions to reduce rates of POHCA in marginalized communities
The researchers emphasized that these findings underscore the need to address disparities through targeted prevention and intervention efforts to reduce the odds of POHCA. These include finding opportunities to increase public health education and awareness around POHCA, as well as implementing measures related to social determinants of health such as improving access to health care, health literacy and preventative healthcare.
The study also suggests other ways for communities to help reduce incidents of POHCA, such as improving emergency medical services, providing education to equip more people with cardiopulmonary resuscitation (CPR) skills and improving access to automated external defibrillators (AED).
“Information on how to provide CPR or how to apply an AED is very simple and anyone can learn,” said Tijssen, Associate Professor in the Departments of Paediatrics and Epidemiology & Biostatistics at the Schulich School of Medicine & Dentistry and Medical Director of the Paediatric Critical Care Unit at Children's Hospital at London Health Sciences Centre. “Children as young as six or eight can learn how to respond to a cardiac arrest so it’s crucial to get out to these communities with this information.”
The team also included Western researchers Kelly Anderson and Yun-Hee Choi.
Study finds high percentage of patients with a severe COVID-19 infection will end up with kidney injury, often fatal
Acute kidney injury associated with severe COVID-19 leads to high mortality rates
For Immediate Release
Severe cases of a COVID-19 infection can cause a host of serious complications, one of them being acute kidney injury. In a recent published study, scientists at Lawson Health Research Institute (Lawson) have found that acute kidney injury in patients with a severe COVID-19 infection is leading to a high mortality rate.
“These are patients who did not have kidney disease, or kidney injury prior to contracting COVID-19,” explains Dr. Peter Blake, Lawson researcher and Provincial Medical Director at the Ontario Renal Network. “This is what we call acute kidney injury, and in the case of these severe COVID-19 patients the kidney injury led to the need for acute dialysis.”
By accessing data collected through the Ontario Renal Network (ORN), Dr. Blake and his colleagues were able to examine 271 people at 27 renal programs across the province, including patients at London Health Sciences Centre (LHSC), who received acute dialysis for acute kidney injury due to a COVID-19 infection. The data examined was from the duration of the first two waves of the pandemic, up to January 31st, 2021.
“This is a complication that is occurs in 10 per cent of ICU COVID-19 cases,” says Dr. Blake, who is also a nephrologist at LHSC. “Men accounted for more than 75 per cent of this condition, half of the patients were diabetic and the majority of these patients were not seniors in the later stages of life, but rather middle-aged people.”
The provincially-collected data through the ORN also showed that patient populations living in postal codes with high ethnocultural deprivation were more likely to get this condition, at a rate of more than 60 per cent, and survival rates were not promising.
“The mortality rate was shockingly high with 64 per cent of these patients dying within 90 days,” adds Dr. Blake. “Many of those who survived remained in hospital for a long period of time and the one in five that did survive have remained on long-term dialysis.”
This study has been published in the Clinical Kidney Journal. Looking ahead, the research team plans to follow up with patients who have survived this severe complication to track what lasting health affects occur within a six-to twelve-month post-survival period.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study gives Ontario men access to advanced prostate cancer imaging
Prostate cancer can be elusive.
Wayne Smith’s journey with prostate cancer began 16 years ago when his family physician noticed increasing levels of prostate specific antigen (PSA) in his blood. PSA is a protein expressed by the prostate. A blood test is used to monitor levels of the protein as a screening tool for prostate cancer.
“My doctor referred me to Dr. Stephen Pautler, Urologist at St. Joseph’s Health Care London. Although we did a number of tests, we weren’t able to locate any spots of cancer,” says Wayne, a 71-year-old man from Ingersoll, Ontario. “We were able to manage my PSA levels for a number of years until they jumped up too high.”

Above: Wayne Smith
In 2012, Wayne was sent for a CT scan. This test finally revealed spots of cancer at the back of the prostate. “Dr. Pautler discussed my treatment options with me and I chose to have surgery to remove my prostate,” explains Wayne. “The team did a great job but we eventually realized some cancer remained. I asked about a PET scan to locate it but the technology was not available at that time.”
After consulting with Dr. Pautler and Dr. Glenn Bauman, Radiation Oncologist at London Health Sciences Centre, Wayne chose to postpone further treatment and monitor the cancer over time. It was undetectable for five years before his PSA levels started rising again. Earlier this year, the levels doubled.
“I was told a PET scan was available through research and that it could help locate the disease,” says Wayne. He went for the scan earlier this year at St. Joseph’s Hospital, part of St. Joseph’s Health Care London. “Nothing showed up on the scan, but that was good news; it meant the cancer was microscopically small.”
The PET scan helped Wayne and his care team in making decisions about his treatment. They decided on hormone therapy and radiation therapy to hopefully eradicate any cancerous cells. He was treated at London Health Sciences Centre’s (LHSC) London Regional Cancer Program.
“Early evidence suggests that a clear PET scan despite rising PSA levels is likely associated with persistent cancer at the original site,” explains Dr. Glenn Bauman, Lawson Scientist and Radiation Oncologist at LHSC. “Based on the scan, Wayne was able to do a much shorter round of hormone therapy – six months rather than being on hormone therapy indefinitely.”
“After the first hormone treatment, my PSA levels dropped significantly. With the added radiation, we’re confident this will be the end of my battle with prostate cancer,” says Wayne, who is currently enjoying retired life by spending time with his wife, two children and five grandkids. “Despite my diagnosis and treatments, I carried on with my life. I did what I had to do but still went places on weekends, did chores around the house and went golfing.”

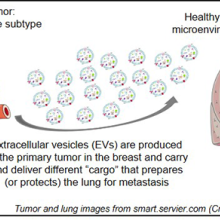
Above: Dr. Glenn Bauman (left) and Wayne Smith (right)
Wayne is one of 1,500 Ontario men who will participate in the PSMA-PET Registry Trial. Led by researchers at Lawson Health Research Institute, the multi-centre registry trial is testing the use of a new imaging tracer, called a PSMA tracer, for early detection of recurrent prostate cancer. The registry gives patients access to a new type of imaging and will assess the impact on patient care.
PSMA tracers are used in positron emission tomography (PET) scans to target a protein found in prostate cancer cells called prostate specific membrane antigen (PSMA). Supported by Cancer Care Ontario and McMaster University’s Centre for Probe Development and Commercialization (CPDC), the goal of the registry trial is to capture detailed PET images to guide treatment decisions made by patients and their care teams.
Eligible participants are those with suspected prostate cancer that cannot be detected in conventional bone and CT scans. Participants have a PET scan using a specific PSMA tracer called 18F-DCFPyL. The tracer is injected and spreads out in the body to find spots of cancer which are then visible on the scan.
“With this trial, men in Ontario can access a promising test that could impact their treatment outcomes,” says Dr. Bauman. “The PSMA tracer may be able to locate prostate cancer that was once undiscoverable.”
Led by Dr. Bauman along with Drs. Ur Metser and Tony Finelli at University Health Network (UHN), the trial is currently available across multiple sites in Ontario: London Health Sciences Centre; St. Joseph’s Health Care London; St. Joseph’s Health Care Hamilton; Sunnybrook Health Sciences Centre; Princess Margaret Cancer Centre (UHN); and Thunder Bay Regional Health Sciences Centre. The trial is also expected to open at The Ottawa Hospital this year.
The PSMA tracer is considered an investigational agent in Canada and is currently only available through clinical trials. After studying the accuracy of the tracer in detecting early cancer recurrence, the research team hopes to have enough data to recommend when it could be used in the clinic.
Patients from London, Ontario and region who are enrolled in the PSMA-PET Registry Trial have their scans performed at St. Joseph's Hospital. In 2016, Lawson researchers were the first in Canada to use the 18F-DCFPyL PSMA tracer to capture PET images with a patient at St. Joseph’s Hospital. The tracer is provided by CanProbe, a joint venture between CPDC and UHN located in Toronto, and was set up with funding from the Movember Foundation.
“We conducted an initial trial that included 20 men with prostate cancer who were having their prostate removed. The goal was to determine how effective the PSMA probe was in detecting disease at the time of initial treatment,” explains Dr. Bauman. “We found the PET scan was able to detect spots of cancer in almost all participants, which corresponded to spots of cancer identified in the prostate after it was removed and examined under the microscope.”
The initial trial was made possible with donor funding through London Health Sciences Foundation, which provided initial funding to hire Research Associate, Catherine Hildebrand, who set up citywide cancer imaging workshops and helped the team prepare successful grant applications to secure key funding from CIHR and OICR.
Dr. Bauman notes that conventional imaging tests like bone scans and computed tomography (CT) are not always effective for detecting prostate cancer. While other PET probes can be used to detect a number of different cancer types, they are unable to identify prostate cancer. The PSMA probe opens new avenues for prostate cancer diagnosis, prognosis and treatment guidance.
For patients like Wayne Smith, access to this advanced imaging is critically important.
“It’s fantastic we have access to this PET scan. It certainly gave me relief knowing nothing showed up on the scan and that, even if something did, it would light up to show us where to treat,” says Wayne. “I know PET scans are used for other cancers too and I think they’re imperative. They give you more of a chance through knowledge of where the disease is located.”

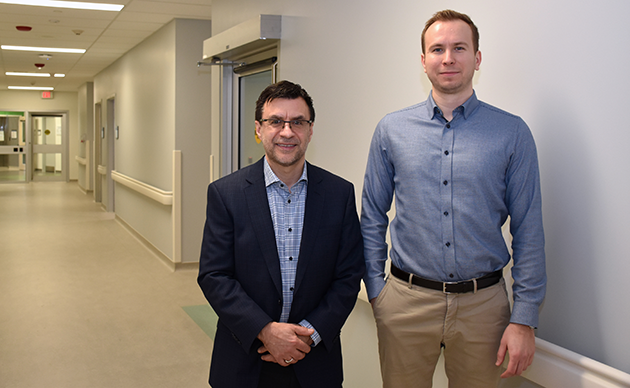
Study identifies biomarkers that could be used in a quick, inexpensive COVID-19 blood screening tool
LONDON, ONTARIO - A new study from Lawson Health Research Institute, Western University and University of Alberta suggests that COVID-19 affects the human body’s blood concentration levels of specific metabolites – small molecules broken down in the human body through the process of metabolism. Three specific metabolites identified in this study could act as biomarkers and one day be measured through an inexpensive blood test to quickly screen patients for the disease and predict which patients will become most critically ill. The team also suspects those metabolites depleted by the virus could be delivered to patients as dietary supplements, acting as a secondary therapy. Published in Critical Care Explorations, the early findings add to the research team’s growing body of evidence on the bodily changes caused by the SARS-CoV-2 virus.
“As the second wave progresses and COVID-19 cases rise, there is an overwhelming demand for testing,” says Dr. Douglas Fraser, lead researcher from Lawson and Western’s Schulich School of Medicine & Dentistry, and Critical Care Physician at London Health Sciences Centre (LHSC). “While our findings need to be confirmed in a larger group of patients, they could lead to a rapid, cost-effective screening tool as a first line of testing in the community and in-hospital.”
The study was conducted by performing metabolomics profiling on blood samples from 30 participants at LHSC: 10 COVID-19 patients and 10 patients with other infections admitted to LHSC’s ICU, as well as 10 healthy control participants. Samples were sent to The Metabolomics Innovation Centre (TMIC) at University of Alberta where a team measured plasma concentrations of 162 metabolites.
“Metabolites are the final breakdown products in the human body and play key roles in cellular activity and physiology. By studying them, we can understand chemical processes that are occurring at any given moment, including those that regulate biological functions related to health and disease,” explains Dr. David Wishart, Codirector of TMIC and Professor of Biological Sciences, Computing Science and Laboratory Medicine & Pathology with the University of Alberta. “Because the human metabolome responds very quickly to environmental factors like pathogens, metabolomics can play an important role in early-stage disease detection, including for COVID-19.”
The team discovered four metabolites of importance to COVID-19 disease detection. The concentration of one metabolite called kynurenine was elevated in COVID-19 patients while concentrations of the other three metabolites (arginine, sarcosine and lysophosphatidylcholines) were decreased. After further analysis, they discovered that by studying the concentrations of only two metabolites – kynurenine and arginine – they could distinguish COVID-19 patients from healthy participants and other critically ill patients with 98 per cent accuracy.
The team also discovered that concentrations of two metabolites (creatinine and arginine) could be used to predict which critically-ill COVID-19 patients were most at risk of dying. When measured on a patient’s first and third day in ICU, these metabolites predicted COVID-19-associated death with 100 per cent accuracy.
“It’s our hope these findings can be validated in larger patient populations and then used to develop a simple blood test that shows high likelihood of infection and disease severity, providing rapid results in as little as 20 minutes,” explains Dr. Fraser. “This could ease the demand for current testing methods, perhaps being used as a portable, first-line screening tool in the community and for when undiagnosed patients present to hospital.”
The team also notes the reduction of key metabolites reflects changes to biochemical pathways or functions in the body which are important to maintaining health and fighting disease. They suggest their findings warrant further study to determine whether certain metabolites could be boosted through dietary supplements. A precision health approach like this could lead to repaired biochemical pathways and improved disease outcomes.
“Providing dietary supplements could be a simple adjunctive or secondary therapy with meaningful outcomes,” says Dr. Fraser. “For example, the metabolite arginine is essential to tissue repair while the metabolite sarcosine activates a process to remove damaged cells. Knowing that COVID-19 causes hyperinflammation that can damage cells and tissue, particularly in the lungs, supporting these processes may prove critical.”
In an earlier study, the team was the first to profile the body’s immune response to the SARS-CoV-2 virus and discover six potential therapeutic targets to improve outcomes. In other studies, they have discovered additional biomarkers that could be used to predict how severely ill a COVID-19 patient will become and uncovered a mechanism causing blood clots in COVID-19 patients and potential ways to treat them.
“We’re working to uncover hard evidence about how the virus invades the body. Ultimately, we hope our combined findings can lead to faster diagnosis, ways to identify patients most at risk of poor outcomes and targets for novel treatments,” notes Dr. Fraser.
This study was made possible through generous donor support. London Health Sciences Foundation is the lead funder with an investment of $90,800 through a significant estate donation and existing funds. Additional funding came from Lawson, Western and the AMOSO Innovation Fund.
-30-
DOWNLOADABLE MEDIA


Dr. Douglas Fraser, Researcher from Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry

Dr. David Wishart, Codirector of TMIC and Professor of Biological Sciences, Computing Science and Laboratory Medicine & Pathology with the University of Alberta
TMIC is a nationally funded core facility which provides cutting edge metabolomics technologies, service and data resources to the research community. TMIC’s unique combination of infrastructure and scientific expertise allow for a wide range of tools for comprehensive and targeted metabolomics studies. For more information, visit www.metabolomicscentre.ca.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
The University of Alberta in Edmonton is one of Canada's top teaching and research universities, with an international reputation for excellence across the humanities, sciences, creative arts, business, engineering and health sciences. Great ideas change the world, but ideas need a push forward. At the University of Alberta, we know that push has never been more important as we do our part to keep doors of opportunity open to all. We're making research discoveries. We’re cultivating entrepreneurs. And we’re giving our students the knowledge and skills they need to turn today's ideas into tomorrow's innovations.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study is first to identify potential therapeutic targets for COVID-19
LONDON, ONTARIO - A team from Lawson Health Research Institute and Western University are the first in the world to profile the body’s immune response to COVID-19. By studying blood samples from critically ill patients at London Health Sciences Centre (LHSC), the research team identified a unique pattern of six molecules that could be used as therapeutic targets to treat the virus. The study is published this week in Critical Care Explorations.
Since the pandemic’s start there have been reports that the immune system can overreact to the virus and cause a cytokine storm – elevated levels of inflammatory molecules that damage healthy cells.
“Clinicians have been trying to address this hyperinflammation but without evidence of what to target,” explains Dr. Douglas Fraser, lead researcher from Lawson and Western’s Schulich School of Medicine & Dentistry and Critical Care Physician at LHSC. “Our study takes away the guessing by identifying potential therapeutic targets for the first time.”
The study included 30 participants: 10 COVID-19 patients and 10 patients with other infections admitted to LHSC’s intensive care unit (ICU), as well as 10 healthy control participants. Blood was drawn daily for the first seven days of ICU admission, processed in a lab and then analyzed using statistical methods and artificial intelligence (AI).
The research team studied 57 inflammatory molecules. They found that six molecules were uniquely elevated in COVID-19 ICU patients (tumor necrosis factor, granzyme B, heat shock protein 70, interleukin-18, interferon-gamma-inducible protein 10 and elastase 2).
The team also used AI to validate their results. They found that inflammation profiling was able to predict the presence of COVID-19 in critically ill patients with 98 per cent accuracy. They also found that one of the molecules (heat shock protein 70) was strongly associated with an increased risk of death when measured in the blood early during the illness.
“Understanding the immune response is paramount to finding the best treatments,” says Dr. Fraser “Our next step is to test drugs that block the harmful effects of several of these molecules while still allowing the immune system to fight the virus.”
The study was made possible with donor support to London Health Sciences Foundation. It also received additional funding from Lawson, Western and the AMOSO Innovation Fund.
-30-
DOWNLOADABLE MEDIA

Above: Blood samples from critically ill COVID-19 patients.

Above: A blood sample from a critically ill COVID-19 patient is collected at London Health Sciences Centre.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study may help explain why breast cancer often spreads to the lungs
A team from Lawson Health Research Institute has shown that triple-negative breast cancer cells can facilitate changes to the lung that both attract cancerous cells and allow them to grow, leading to lung metastasis.
Metastasis is the spread of cancer cells from a primary tumour to different organs. Lung metastasis is responsible for approximately 60 to 70 per cent of deaths related to breast cancer.
“The best way to explain lung metastasis is the seed and soil analogy,” says Dr. Alison Allan, Lawson Scientist. “The seeds are the breast cancer cells from a primary tumour and the soil is the lung’s microenvironment. Seeds can break away, but they only grow if the soil is fertile.”
The majority of studies on metastatic cancer have focused on the characteristics of tumour cells and not on the organs to which they spread. Dr. Allan’s team is studying how the lung microenvironment itself is contributing to lung metastasis.
In the new study, the team examined the lung microenvironment in preclinical models. They compared models with two different subtypes of breast cancer. The luminal A subtype is the least aggressive form of breast cancer and does not often metastasize to the lung. Triple-negative breast cancer, meanwhile, is the most aggressive form with a higher likelihood of metastasis and no targeted therapies available.
The team found that models with triple-negative breast cancer had a drastically different lung microenvironment that was much more hospitable to the growth of cancer. They also found that triple-negative breast cancer cells might be sending ‘signals’ to the lung to help it attract cancerous cells that enter the bloodstream.
“We suspect that triple-negative breast cancer cells release tiny particles called exosomes which are delivered to the lung,” explains Dr. Allan, who is also Chair of the Department of Anatomy and Cell Biology at Western University’s Schulich School of Medicine & Dentistry. “Once delivered, the exosomes signal the lung to start changing into a hospitable environment for tumour cells.”
With support from Lawson’s Internal Research Fund, the team is continuing to research this process. They are also studying ways to make the lungs less receptive to cancerous cells.
Their findings could help in the development of targeted therapies to prevent breast cancer from metastasizing. For example, in collaboration with investigators at the University of Alberta, they are developing an inhalable spray that is aimed at preventing cancer from spreading to and growing in healthy lungs.
“The ultimate goal is to eliminate the metastasis-promoting exosomes as a therapeutic strategy to prevent triple-negative breast cancer from spreading to the lungs,” says Dr. Allan.
The study “Triple-Negative Primary Breast Tumours Induce Supportive Premetastatic Changes in the Extracellular Matrix and Soluble Components of the Lung Microenvironment,” is published in Cancers. It was funded by the Cancer Research Society, the Canadian Cancer Society Research Institute, a London Regional Cancer Program Catalyst Grant, London Health Sciences Foundation, the Breast Cancer Society of Canada and an Ontario Graduate Scholarship awarded to Braeden Medeiros – the paper’s first author.
Above: Visual representation of the research findings
Study offers hope for hard-to-treat type 2 diabetes
A landmark international study involving patients and researchers at St. Joseph’s Health Care London shows automated insulin pump delivery can be ‘life-changing’ for people with type 2 diabetes
Lisa Mercer had tried just about everything to regulate the ups and downs of her blood sugars, from a strict diet to medication to four-a-day-day insulin shots.
But her busy life with type 2 diabetes finally started to feel better when she enrolled in a clinical trial at St. Joseph’s Health Care London to test the effectiveness of a system that combined glucose monitoring with an automated insulin pump.
“It was life-changing for me. I was diagnosed with type 2 diabetes 25 years ago and my blood sugars have always been all over the map. I felt sort of helpless. I said yes to this clinical trial because I hoped it would return some normalcy to my life,” she says. Now that study, with results newly published in the prestigious New England Journal of Medicine, is being heralded as a big step forward for patients with hard-to-treat type 2 diabetes.
“This is an exciting finding because it shows we can improve patients’ blood sugars and hopefully prevent long-term negative consequences of high sugars while at the same time making it easier for patients to manage the disease,” says Dr. Tamara Spaic, Medical Director of St. Joseph’s Diabetes Education Centre and the lead Canadian researcher for the multi-site international study based at the Jaeb Center for Health Research in Tampa, Fla.
Study participants were placed either in a group testing the effectiveness of a new system called Control IQ+ or a control group continuing their existing diabetes management regimen.
The intervention group wore glucose monitors that electronically talked with high-tech pumps that delivered insulin – automatically, in the right dose and at the right time – with minimal patient input.
While the device was approved about five years ago for people with type 1 diabetes, this is the first examination of its effectiveness managing the complexities of type 2 diabetes.
“The biggest burden in diabetes control is that it’s 24/7 vigilance: did I eat or not; what did I eat and how much; did I exercise; do I need to wake up for an insulin shot in the middle of the night? This system largely removes those variables to bring blood sugars to target levels,” says Spaic, who is also a Lawson Research Institute scientist and professor of endocrinology and metabolism at Western University’s Schulich School of Medicine & Dentistry.
“What surprised us was that this worked so well across all populations regardless of duration of the disease, amount of insulin needed, whether they used other medications or not, whether they were tech-savvy or not. It worked for everyone regardless of their ethnicity, socioeconomics, and whether they were male or female, old or young,” she adds.
Researchers even asked participants in the intervention group to skip insulin with meals on occasion – generally a no-no in the highly regimented life of someone with insulin-managed diabetes – and the automated system responded appropriately and quickly to adjust blood sugars.
Mercer found improvement within a couple of weeks: “Before the pump, I felt awful. When my sugars were too low, I got the shakes, I had trouble communicating and thinking clearly and I got extremely tired. When my sugars were too high, I was exhausted. It dominated every day and was tough on my job as a police officer. Now I feel better. I feel more in control.
“Is it perfect? No. But my sugars are stable and consistent more often than not.”
Not yet approved in Canada
In February, the US Food and Drug Administration cleared the use of the Control IQ+ system in adults with type 2 diabetes – approval that also meant the expense could be covered through health insurance.
However, it has not yet been brought to Health Canada regulators for approval, Spaic says.
Even so, several of her patients, including Foster, decided to continue using the system after the 13-week trial, paying out-of-pocket or through private insurance.
Spaic and St. Joseph’s colleagues, endocrinologist Dr. Selina Liu and nurse coordinator Marsha Driscoll, were extensively involved in the design of the study, recruiting and monitoring participants and reporting results.
Diabetes type 2 usually develops in adulthood and is a condition in which body cannot make enough insulin or does not properly use the insulin it makes to regulate the amount of glucose (sugar) in the blood.
While most people with type 2 diabetes can control their blood sugars through lifestyle changes or with new treatments such as non-insulin glucose-lowering medications, the sub-set of North Americans who require insulin still numbers in the millions.
THE STUDY:
What: 13-week, large-scale clinical trial to test the effectiveness of a system combining automated insulin delivery with continuous glucose monitoring for people with type 2 diabetes.
Who: 319 study participants – including 13 at Lawson Research Institute of St. Joseph’s Health Care London – all needing multiple daily insulin doses. Age range 19 to 87, from 21 centres across the U.S. and Canada. Study led by Jaeb Centre for Health Research in Tampa, Fla., and funded by Tandem Diabetes Care, which also provided the automated insulin-delivery systems
How: Two-thirds of patients received an automated insulin pump, continuous glucose monitor and transmitter to track and automatically administer insulin to regulate their blood sugars. A control group continued their existing insulin-delivery method and also received glucose monitors.
Results: The intervention group had more stable blood sugar levels – with 3.4 more hours per day in the target glucose range – than the control group. Use of automated insulin devices was successful and safe even for patients without previous experience with an insulin pump
Why it matters: Automated insulin delivery can help insulin-dependent patients manage their type 2 diabetes better than before. Better management means improved quality of life and may result in fewer diabetes complications such as heart disease and damage to the eyes, kidneys and nerves.
Study results prove success of project aimed at preventing family homelessness
Lawson Health Research Institute, Western University, City of London, and Mission Services of London, Ontario, partnered on the Prevention of Homelessness Among Families (PHAF) project to assess the effectiveness of a shelter diversion pilot-program at Rotholme Women’s and Family Shelter (Mission Services).
The results of the study illustrate that a low percentage of families ended up in shelter when accessing the program, and as many as 90 per cent of the families were known to still be housed 18-months later.
The project was supported by $134,000 in funding delivered through the Government of Ontario’s Local Poverty Reduction Fund (LPRF). The grant, funded by the Government of Ontario and administered by its agency, the Ontario Trillium Foundation, is helping groups disproportionately affected by poverty get into housing, develop skills and find employment in London, Ontario.
This project focuses on local community partnerships and includes a third-party evaluation component, which is important because better data will help communities develop better solutions to increasing food security, reducing child poverty and homelessness, and helping people find jobs and earn a stable income.
Rotholme’s shelter diversion program aims to divert family homelessness by working with families to maintain stable housing prior to eviction. Families at risk of homelessness who contact the shelter before leaving their home are immediately connected with a housing crisis worker. Together, parents and the crisis worker explore alternate housing arrangements, services, and supports.
“To keep families in their home we have a ‘whatever it takes approach.’ Once families have left their homes and belongings it is very difficult to escape homelessness,” says Gordon Russell, director of shelters, Mission Services, of London. A variety of tactics are used to divert families from shelter, such as negotiating with landlords to keep the family in their home or move them into an available unit.
To evaluate the success of the program, researchers assessed administrative shelter data, interviewed parents who participated in the program, and conducted focus groups with staff and families who did not access the program.

Researchers interviewed 20 families at four time points, approximately six months apart. Thirteen families were able to complete all four interviews. In total the information of 75 individuals, including 29 parents and 46 dependents, was collected, and included demographics, specific needs, utilization of health services, and quality of life metrics. A majority of the parents interviewed had never experienced homelessness before accessing Mission Services.
“We found that Rotholme’s pilot program was effective for preventing family homelessness,” explains Dr. Cheryl Forchuk, assistant scientific director at Lawson, and professor of Nursing at Western University. “Family homelessness is a serious problem, one that can be prevented with early intervention according to our results.”
Other themes that emerge from the study suggest:
- families at risk of homelessness may have life challenges such as mental health and addiction issues, language issues, or low level education levels;
- families at risk of homelessness may have a lack of understanding the system including shelter rules, social assistance and school supports and their own rights;
- and, families at risk of homelessness may experience difficulty with conflict, both within the family dynamic and in resolving conflicts with landlords.
“When we know the challenges that families face, we are better equipped to meet their needs and continue to help them live in stable housing,” continues Dr. Forchuk. “Understanding issues of service preference and outcomes from the context of the whole family are critical to planning appropriate services.”
This investment by the Government of Ontario is just one way the province is bolstering innovative local programs that support groups disproportionately affected by poverty. Through the Local Poverty Reduction Fund, Ontario is helping to break the cycle of poverty for children and youth, increase employment and income security, and end homelessness in Ontario.
Study reveals clinical factors linked to reduced mortality in injection drug users with heart valve infection
Cases of endocarditis – infection of the heart valves – have risen dramatically in recent years as a result of the opioid crisis. In London, Ontario 55 per cent of people who experience heart valve infections are injection drug users. They are particularly vulnerable to the disease and a third die as a result.
In an effort to improve outcomes, researchers at Lawson Health Research Institute and Western University are studying which clinical factors are associated with improved survival in this patient population. In a new study, they showed that both surgery and in-hospital addictions counselling are linked to significantly reduced mortality in injection drug users with first-episode endocarditis. Surgery was associated with a 56 per cent reduction in mortality, while in-hospital addictions counselling was associated with a 72 per cent reduction.
The project was a retrospective cohort study that examined anonymous patient data from 2007 to 2016 at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. Of 370 patients with first-episode endocarditis, 202 were persons who inject drugs. Of those 202 patients, 39 had cardiac surgery at LHSC and 40 were referred for addictions counselling to start in while they were still in-hospital.
The study found that patients who received surgery experienced a 56 per cent reduction in mortality. Patients who received surgery were normally the most severely ill and most in need. While additional studies are necessary, the researchers point to these findings as a reason for cardiac surgery to be considered as a viable treatment option in carefully selected patients.
“In the past, many centres have not performed cardiac surgery in patients who inject drugs due to concerns about poor outcomes. Continued injection drug use was viewed as a risk for reinfection,” says Dr. Michael Silverman, author of the study, Lawson scientist and Chair/Chief of Infectious Diseases for Western’s Schulich School of Medicine & Dentistry, LHSC and St. Joseph’s. “Our study challenges those beliefs. It shows that when we account for the severity of a patient’s illness, they’re more likely to survive with surgery.”
Patients who were referred for addictions counselling while in-hospital experienced a 72 per cent reduction in mortality. Addictions counselling was provided by a consultant who would meet with patients to provide education on risks for infection, harm reduction strategies and support towards addictions recovery, including referral to community supports.
The study’s authors point out that, in other centres, patients are not commonly referred for addictions counselling while still being treated for an acute infection. It is commonly believed they are too ill to undergo this type of therapy. The more common approach is to treat the infection and refer patients for addictions counselling after discharge.
“Education and support for these patients is critical. The majority of the patients I see don’t understand what they’re doing to cause an infection and may be highly motivated to undertake a lifestyle change,” says Dr. Sharon Koivu, author of the study, Lawson scientist, associate professor at Schulich Medicine & Dentistry and palliative-care physician at LHSC. “This study shows the importance of working with patients towards harm reduction and addiction recovery while they’re still being treated in-hospital.”
London’s rates of endocarditis in persons who inject drugs are significantly higher than other regions. While injection drug users account for 55 per cent of all heart valve infections in London, they account for only 8 to 12 per cent in large studies in the United States. To address this issue, the research team is conducting a number of additional studies. Current projects are exploring the reasons behind such high local rates and the best strategies for treatment, including antibiotic and surgical interventions.
“We don’t often get a chance to look at large numbers of this particular patient population but there is a plethora of local data available,” says Dr. Laura Rodger, author of the study and a resident physician at Schulich Medicine & Dentistry and LHSC. “Our team wants to bring meaning to that data by asking the right questions to ultimately improve patient outcomes.”
The study, “Clinical Characteristics and Factors Associated with Mortality in First-Episode Infective Endocarditis Among Persons Who Inject Drugs,” is published in JAMA Network OPEN.
Study shows a decline in Veterans’ mental health throughout the pandemic
MEDIA RELEASE
For immediate release
February 16th, 2022
LONDON, ON – In newly-published findings from Lawson Health Research Institute, more than half of Canadian Veterans report a decline in their mental health over the course of the COVID-19 pandemic.
When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population.
“We anticipated the ongoing pandemic would have impacts to multiple domains of life such as loneliness, isolation, depression and PTSD,” says Associate Scientist at Lawson and the MacDonald Franklin Operational Stress Injury (OSI) Research Centre, Dr. Anthony Nazarov.
To examine the potential impacts the research team launched a longitudinal study in early 2021, recruiting Canadian Veterans and spouses of Canadian Veterans. A total of 1,136 Veterans have participated in the study which spans over 18 months. Participants complete online questionnaires every three months, with questions focused on mental health and virtual health care services.
“We looked at use of care services, including virtual care services, which we know have been on the rise during the pandemic,” says Lawson Associate Scientist and Scientific Director of the Macdonald Franklin OSI Research Centre, Dr. Don Richardson.
The team recently published preliminary findings based on the Veterans portion of the study, which confirm a decline in mental health amongst the Veterans that took part.
“One of the important preliminary findings demonstrated a little more than 55 per cent of Veterans (55.9 per cent) have indicated that their mental health has worsened over the pandemic.” explains Dr. Richardson.
The findings also revealed that nearly one in five Veterans used virtual health care and telepsychiatry services and found them to be helpful.
“Veterans have been having positive experiences with virtual care for mental health support,” adds Dr. Nazarov. “Most found it helpful, and more importantly, many would like to continue to use this form of health care services even post pandemic.”
The preliminary study findings have been published in the European Journal of Psychotraumatology. The longitudinal study will wrap up this summer, and then the team hopes to use the information to improve and innovate different forms of mental health supports for Veterans and their spouses in the future.
-30-
About Lawson Health Research Institute: Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
For more information, please contact:
Celine Zadorsky
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C. 519-619-3872
@email
www.lawsonresearch.ca/news-events
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study shows a decline in Veterans’ mental health throughout the pandemic
LONDON, ON – In newly-published findings from Lawson Health Research Institute, more than half of Canadian Veterans report a decline in their mental health over the course of the COVID-19 pandemic.
When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population
“We anticipated the ongoing pandemic would have impacts to multiple domains of life such as loneliness, isolation, depression and PTSD,” says Associate Scientist at Lawson and the MacDonald Franklin Operational Stress Injury (OSI) Research Centre, Dr. Anthony Nazarov.
To examine the potential impacts the research team launched a longitudinal study in early 2021, recruiting Canadian Veterans and spouses of Canadian Veterans. A total of 1,136 Veterans have participated in the study which spans over 18 months. Participants complete online questionnaires every three months, with questions focused on mental health and virtual health care services.
“We looked at use of care services, including virtual care services, which we know have been on the rise during the pandemic,” says Lawson Associate Scientist and Scientific Director of the Macdonald Franklin OSI Research Centre, Dr. Don Richardson.
The team recently published preliminary findings based on the Veterans portion of the study, which confirm a decline in mental health amongst the Veterans that took part.
“One of the important preliminary findings demonstrated a little more than 55 per cent of Veterans (55.9 per cent) have indicated that their mental health has worsened over the pandemic.” explains Dr. Richardson.
The findings also revealed that nearly one in five Veterans used virtual health care and telepsychiatry services and found them to be helpful.
“Veterans have been having positive experiences with virtual care for mental health support,” adds Dr. Nazarov. “Most found it helpful, and more importantly, many would like to continue to use this form of health care services even post pandemic.”
The preliminary study findings have been published in the European Journal of Psychotraumatology. The longitudinal study will wrap up this summer, and then the team hopes to use the information to improve and innovate different forms of mental health supports for Veterans and their spouses in the future.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study shows fewer higher-dose radiation treatments safe and well tolerated by women with uterine cancer
MEDIA RELEASE
FOR IMMEDIATE RELEASE
Sunnybrook Health Sciences Centre and Lawson Health Research Institute
April 14, 2022
LONDON,ON - Five high-dose radiation treatments targeting uterine cancer rather than the current standard 25 treatments are safe and well-tolerated by patients, a new study published in JAMA Oncology has found.
SPARTACUS (Stereotactic Pelvic Adjuvant Radiation Therapy in Cancers of the Uterus) — a multi-institutional non-randomized controlled trial — looked to assess the feasibility and safety of using a specialized technique called stereotactic body radiation therapy (SBRT) for women with uterine cancer where instead of 25 treatments over five weeks, five treatments can be delivered over 1.5 weeks.
SBRT uses many precise beams of radiation to target tumours or cancerous cells. It uses a higher dose of radiation in a smaller number of treatments. It can be done on a standard linear accelerator, the machine that delivers radiation treatments.
Sixty-one women were enrolled in SPARTACUS at two centres — Sunnybrook Health Sciences Centre and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC).
“Uterine cancer is a common cancer in women, usually treated with surgical removal followed by radiation and/or chemotherapy to reduce the risk of recurrence,” said Dr. Eric Leung, radiation oncologist at Sunnybrook’s Odette Cancer Centre. “External beam radiation is usually given over five weeks, and that can place a heavy burden on women who have to travel to a radiation centre every day, spend time away from home and work, and incur the financial burden of these factors as well.”
With a median follow-up of nine months, the patients enrolled in SPARTACUS reported an acceptable level of side effects from the radiation that resolved, and also reported a reasonable quality of life during treatment, Dr. Leung said.
“We were interested in examining the toxicity of the higher dose – would it affect the nearby bowels or bladder and place a heavy symptom burden on patients? We were pleased to find that patients reported their symptoms as manageable.”
“This study represents a novel way of treating uterine cancer in a shorter time. It was conducted mainly through the COVID pandemic and gave women a chance to receive treatment in less time with fewer visits to our centres,” said Dr. David D’Souza, radiation oncologist at LHSC and the study co-lead through Lawson Health Research Institute.
Patients will continue to be followed on the study for late side effects and further research is planned to further compare this more convenient schedule to the standard five-week course of radiation.
“This novel treatment could lead to a practice change that places less burden on patients and on the healthcare system,” Dr. Leung said. “Delivering radiation over the course of a week and half rather than over five weeks for patients facing uterine cancer would open up healthcare resources by reducing visits and usage of the linear accelerators.”
-30-
ADDIONAL QUOTES – Dr. David D’Souza:
“Giving radiation in a shorter time can have several advantages for both the patient and the health care system."
“Our study assessed the safety of delivering a higher dose of radiation in fewer treatments for patients with uterine cancer by adapting what has successfully been done for other types of cancer in the pelvis like prostate and rectal cancer.”
“This study was made possible with advances in treatment planning, radiation machine capabilities, and an outstanding radiation therapy program at LRCP.”
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
ABOUT SUNNYBROOK HEALTH SCIENCES CENTRE
Sunnybrook Health Sciences Centre is inventing the future of health care for the 1.2 million patients the hospital cares for each year through the dedication of its more than 10,000 staff and volunteers. An internationally recognized leader in research and education and a full affiliation with the University of Toronto distinguishes Sunnybrook as one of Canada’s premier academic health sciences centres. Sunnybrook specializes in caring for high-risk pregnancies, critically-ill newborns and adults, offering specialized rehabilitation and treating and preventing cancer, cardiovascular disease, neurological and psychiatric disorders, orthopaedic and arthritic conditions and traumatic injuries. The Hospital also has a unique and national leading program for the care of Canada’s war veterans.
Media Contacts:
Celine Zadorsky
Communications & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C: 519-619-3872
@email
Sunnybrook Health Sciences Centre
Communications & Stakeholder Relations
416-480-4040
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca


