Search
Search
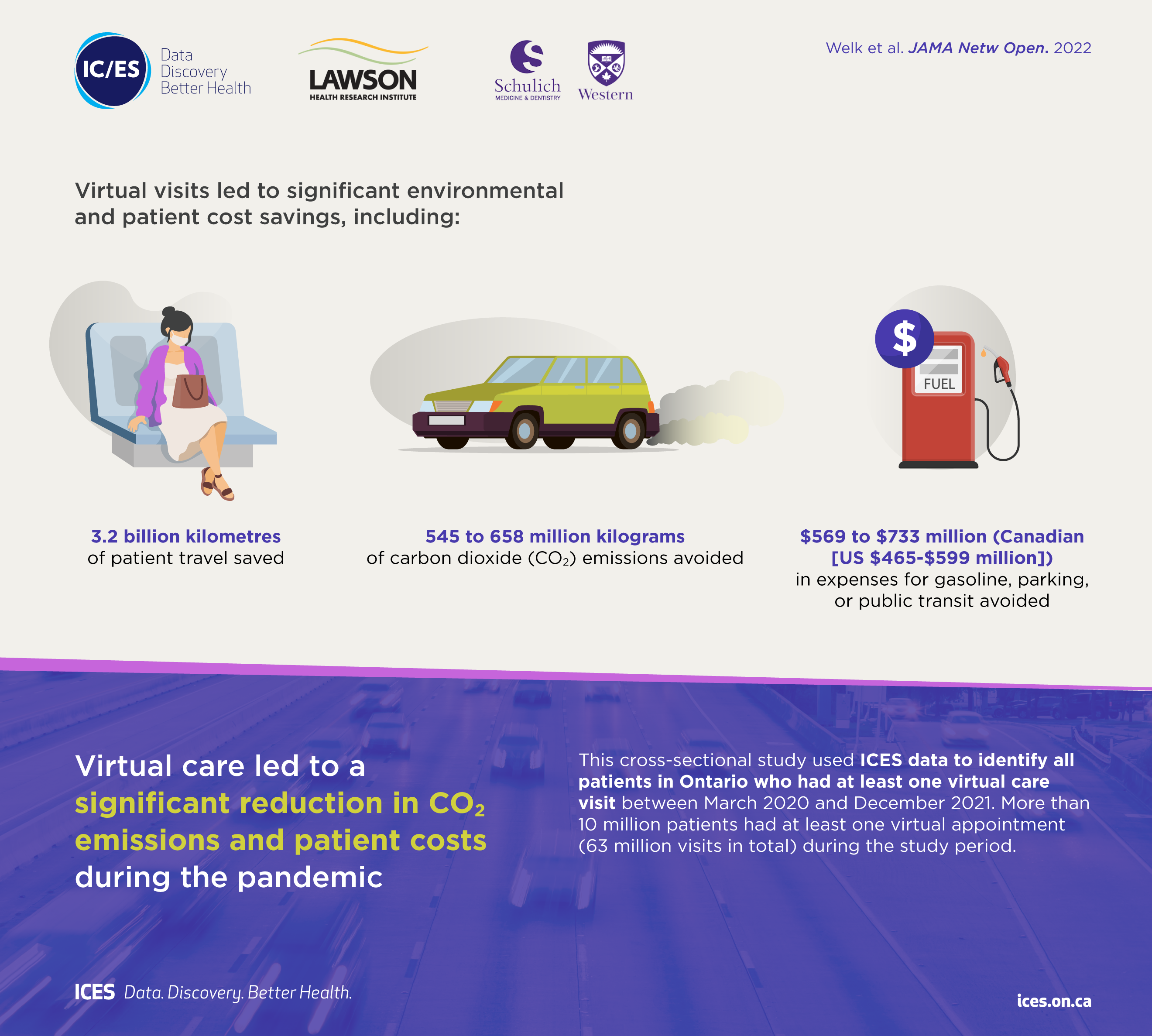
Virtual care associated with significant environmental and patient cost savings
London, ON - A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can
be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Virtual care associated with significant environmental and patient cost savings
A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Walking the labyrinth: A path for meaning, insight and reflection
At Southwest Centre for Forensic Mental Health Care (Southwest Centre) in Elgin County, the unique story of every individual is honoured as care practitioners assist in the journey toward recovery. Part of the St. Joseph’s Health Care London family, Southwest Centre is devoted to caring for people with a mental illness who have also come into contact with the criminal justice system.
A new study by Lawson Health Research Institute shows that the use of labyrinths contributes to recovery by promoting spiritual self-care, insight development and personal meaning-making reflection. The research was co-authored by Lawson Allied Scientist and Certified Spiritual Care Practitioner at Southwest Centre, Stephen Yeo, along with his colleagues Dr. Clark Patrick Heard and Jared Scott, both Lawson Associate Scientists and Occupational Therapists.
“Research has demonstrated that labyrinth-walking can result in increased focus and calm, along with a reduction in blood pressure and stress,” explains Yeo. “Additionally, labyrinth-walking is narrative-driven and highly constructivist in nature, which promotes the opportunity for one to critically reflect on his or her unfolding story.”
This can be done in solitude or a trained facilitator can support important narrative reflection and invite opportunities for integration.
The process of reflecting and making meaning helps individuals to think about what they observed or did, why it mattered and how they might think or act differently based on new knowledge. This allows them to set goals and use what they’ve learned from the past to inform future action, and to consider the real-life implications.
Participation supports patients as they cope with mental illness, and the impact is magnified for individuals who have come into contact with the criminal justice system. Their experience can increase existential questions along with spiritual pain and distress.
Even in the most complex and difficult circumstances, walking the labyrinth facilitates a variety of coping approaches including:
- stress reduction and mindfulness;
- understanding one’s awareness of relationship with that which is sacred to them (transcendence) and the environment;
- development of ongoing personal narrative and meaning-making; and,
- kinesthetic prayer and meditation.
Unlike mazes that are like puzzles with many choices of path and direction, labyrinths are created using continuous lines and are easier to navigate with one route to and from the centre. There are two permanent labyrinths at Southwest Centre – one indoors and one outdoors. For the most part, the labyrinths are accessible for self-guided walking and, throughout the year, various group opportunities are scheduled for invited participation. This activity can be continued in the community, as there are labyrinths in various places across the province such as parks, faith communities and other health-care settings.
“Labyrinth participation supports themes related to hope, coping, resiliency, autonomy – all of which are significant contributors to recovery and the maintenance of well-being. Future research in this area could examine the benefits for different patient populations and also for those who reside in the community.”
Labyrinths are trans-religious and their application can be beneficial to religious and non-religious participants. They are also easy to maintain and can be installed in a variety of locations.
Along with his study co-authors, Yeo was honoured with the CASC Group Research Award from the Canadian Association for Spiritual Care. The award recognizes a CASC member who collaborates with other professionals in the research field of spirituality, religion and wellbeing. The recipient supports the core values of professional connection and interdependence, promoting positive relationship with colleagues of various professionals as well as clients.
“Given that this was my first foray into research at this level, I was very humbled to have been nominated for, and to have received, this award,” says Yeo. “I remain especially grateful to the professional guidance and support of my research colleagues.”
“Walking the Labyrinth: Considering mental health consumer experience, meaning making, and the illumination of the sacred in forensic mental health setting” was published in the December 2015 issue of the Journal of Pastoral Care and Counseling. This study is believed to be a first of its kind in a forensic mental health care facility.
Image

|
Left: Photo of the indoor labyrinth at the Southwest Centre for Forensic Mental Health Care. |
What happens to our bodies when we feel social emotions?
Feeling emotions based on the interactions we have with other people is a common part of daily life, yet we know very little about how these emotions are experienced in the body.
Chloe Stewart, a PhD candidate at Lawson Health Research Institute (Lawson) and Western University’s Schulich School of Medicine & Dentistry, has been awarded a Lawson Internal Research Fund (IRF) Studentship to conduct the first study to comprehensively explore the physical experience of social emotions. The study will be supervised by Dr. Elizabeth Finger, a Lawson scientist, neurologist at St. Joseph’s Health Care London’s Parkwood Institute, and associate professor at Schulich Medicine & Dentistry.
“We feel social emotions based on our awareness, interpretation or anticipation of the thoughts and feelings of others. For example, we feel embarrassment not only because we have done something potentially embarrassing, but also because we know that another person is aware of it, or could become aware of it. Other social emotions include pride, empathy and guilt,” explains Stewart.
“These are distinct from basic emotions, such as anger and happiness, which only require us to be aware of how we ourselves are feeling and can occur completely independently of other people. Whether it’s your heart beating faster when you’re angry or the lump in your throat when you’re sad, the ways that our bodies experience basic emotions are very well understood. However, we do not have a good understanding of what happens to our bodies when we feel social emotions,” she adds.
Unhealthy levels of certain social emotions are associated with many conditions, including certain kinds of dementia, obsessive compulsive disorder and psychopathy. The results of the study, which will be conducted at Parkwood Institute, could help in developing potential interventions or treatment approaches to restore these emotions to healthy levels.
The first phase of the study will look at the physical experience of social emotion in healthy adults. Noninvasive electrodes will be attached to participants’ torso, hands and throat. The electrodes are connected by wires to receivers, which in turn send signals to a computer. The researchers can assess how the signals change based on the stimulus the participant is looking at. Stewart expects the emotions will influence several different physical responses, including heart rate, swallowing rate and movement of the stomach muscles.
The research team will then extend the study to patients with frontotemporal dementia, which can impair social functioning. They will compare the physical experience of social emotions in these participants to participants with Alzheimer’s disease and dementia with Lewy bodies. Patients with Alzheimer’s disease or dementia with Lewy bodies usually have healthy levels of social emotions, but those who have dementia with Lewy bodies often have impaired physiological functioning while those with Alzheimer’s do not.
Their goal is to compare how social emotions look in healthy adults to what happens in the body when social functioning is impaired.
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
What is ICES Western? Q&A with Dr. Amit Garg
As ICES Western recruits a new Site Director, Dr. Amit Garg, who currently holds the position, sat down to talk about the importance of the work being done. Dr. Garg is also a Scientist at Lawson Health Research Institute, Nephrologist at London Health Sciences Centre (LHSC) and Professor at Western University’s Schulich School of Medicine & Dentistry.
What is your role with ICES Western?
Starting in 2009, I supervised the team responsible for the ICES Western build over an approximately three-year period. Since then, I have spent the last decade serving as the inaugural Site Director for ICES Western.
Can you briefly describe the work that ICES Western does?
For those people who don't know, ICES is a province-wide non-profit research institute, founded in 1992, that is focused on translating data into trusted evidence. Our community is comprised of world-class research, data and clinical experts who evaluate health care delivery and population outcomes.
ICES scientists and staff (currently about 570 in Ontario) and trainees (currently about 700) access a vast and secure array of Ontario’s demographic and administrative health-related data. ICES currently has 108 linked data holdings (with over one trillion data points), and the amount of data that ICES has available for use in research grows each year. The linked data include vital statistics, hospital services, physician claims, drug benefits, laboratory results, biosamples and immigration records. Our research, including 1,200 active investigator-initiated projects, is focused on making health policy and health care better, and people healthier.
ICES Western is physically located at LHSC’s Victoria Hospital and is one of seven ICES satellite sites across Ontario. The site’s development is an ongoing partnership between LHSC, St. Joseph’s Health Care London, Lawson, the Academic Medical Organization of Southwestern Ontario (AMOSO) and Western.
How does ICES’ work impact research being done in Ontario and across Canada?
ICES Western is a core facility that researchers use for research, training and decision support. Organizations such as our local hospitals and public health agencies make requests for decision support through a procedural mechanism called Applied Health Research Questions.
Over the last two years, our researchers have conducted a great deal of COVID-19 research. Several projects at ICES Western have examined vaccine effectiveness and spread of the virus. Investigators have used a data-driven approach to help protect people experiencing homelessness in Ontario. Another study quantified the impact of COVID infections on physicians, including how many of them became ill, were hospitalized and received care in the intensive care unit.
Research done through ICES Western has led to important changes in health care. For example, Health Canada instituted labeling requirement changes based on drug safety studies done through ICES.
Why is this work so important?
We all want better health outcomes for citizens, both in Ontario and throughout the world. Ideally, we want people to live longer, healthier lives without needing many health care resources, and we want that to be done in an equitable fashion. There is a substantial amount of research needed in multiple areas to achieve this goal. ICES provides a cutting edge infrastructure to enable this work.
What kind of researchers are involved with ICES?
At ICES Western we support a whole host of individuals and entities as they conduct research. Health care delivery organizations and health agencies including LHSC, the Ontario Renal Network and Trillium Gift of Life Network use knowledge received through reports completed at ICES. Our typical individual investigators include both basic science and clinical investigators. We also support trainees in the areas of epidemiology and statistics, as well as many other fields of study, such as computer science and geography. These are all students who have an interest in working with ‘big’ data. Finally, we have personnel that work with privacy, data, analysis, epidemiology and more.
What do you see in the future for the organization?
We've made a lot of progress in the last 10 years and I can't wait to see what's going to happen in the future. We're still just scratching the surface in terms of what's possible. While what we have done in building this site and supporting important research is impressive, in terms of the possibilities – the sky's the limit. There is so much opportunity around new research and trial methodologies, new insights and new evaluation techniques. I expect ICES Western will continue to develop, enabling a growing number of people to make a large impact. I see ICES continuing to contribute to a world where people live longer, healthier lives.
What is the most important thing people should know about ICES?
How enabling it is. It's time well spent to really understand what is and is not possible with ICES data and research expertise. Once you invest in it – really spend your time and energy to understand the potential– you start realizing all of these opportunities that would not be possible otherwise. With more than a thousand research studies underway across all ICES sites, we have great discoveries ahead to shape the future of health care in Ontario.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
When connections break down
In Ontario alone, an estimated 285,000 individuals currently live with some form of neurodegenerative disorder. This includes Alzheimer’s Disease, Parkinson’s Disease, mild cognitive impairment, dementia and movement disorders.
The experiences and symptoms for each person vary, but they share a progressive decline in their cognitive and motor function. It can affect their ability to work, socialize and live independently.
As our population ages, there is an urgent need to understand markers that will predict decline and identify targets for therapy that might improve long-term function and outcomes.
This is where hospital-based research can make a real difference.
On June 21, 2018, Lawson Health Research Institute hosted Café Scientifique, a community event highlighting the groundbreaking and specialized research on neurodegenerative diseases happening right here in London.
Moderated by Lawson researcher Dr. Arlene MacDougall, a panel of three expert Lawson scientists shared their unique perspectives as both clinicians and researchers, and how the knowledge we are gaining is being applied to improve health and health care for people here and around the world.
Watch the video from the event featuring the three talks from our experts.
Café Talks
Back to the beginning: Targeting early markers for Alzheimer’s Disease
By Dr. Jennie Wells
Time stamp: 5 minutes
Dr. Wells is the Medical Care Coordinator for Geriatric Rehabilitation at St. Joseph's Health Care London's Parkwood Institute, and Chair of the Division of Geriatric Medicine and associate professor in the Department of Medicine at Western Univeristy’s Schulich School of Medicine. Her clinical and research interests are Alzheimer’s Disease and Geriatric Rehabilitation. She has particular interest in Mild Cognitive Impairment (MCI) and the potential for non-drug interventions, such as exercise and nutrition to slow progression of dementia. She is a principal site investigator in randomized controlled trials of new drugs to treat dementia, MCI, and Subjective Cognitive Impairment (SCI).
Highlights:
- What causes dementia?
- How early do changes happen in the brain before symptoms even appear?
- What is the single best diet approach for a healthy body and mind?
- How does exercise keep your brain healthy?

Neuroinflammation and dementia: The old and the new
By Dr. Elizabeth Finger
Time stamp: 24 minutes
Dr. Finger, a neurologist at St. Joseph's Parkwood Institute, received her MD from Cornell University. She completed an internship in Internal Medicine at Massachusetts General Hospital, followed by residency in Neurology at Massachusetts General Hospital and Brigham and Women's Hospital in Boston. Her research focuses on understanding the cognitive, neural, and genetic substrates of abnormal decision-making, emotion and social behavior. Using a variety of different diagnostic techniques and modalities, the research program investigates the cognitive and neural systems affected in patients with Frontotemporal Dementia, related disorders and their at-risk family members.
Highlights:
- Do anti-inflammatory medications reduce the risk of dementia or slow the rate of decline?
- How do genes related to the immune system increase the risk of developing dementia and Alzheimer’s Disease?
- What about the effects from dysfunction of the brain’s own immune system?
- Do conditions or events causing systematic inflammation (surgery, infection, auto-immune diseases) also increase neuroinflammation which can lead to dementia?

New Frontiers in the Treatment of Parkinson’s Disease: Addressing the unmet needs
By Dr. Mandar Jog
Time stamp: 45 minutes
Dr. Jog is a Lawson researcher, Director of the National Parkinson Foundation Centre of Excellence at LHSC, Director of the Movement Disorders Centre in London and Professor of Neurology at Western University. His research interests include topics such as motor control, neurophysiology and computational modeling, multichannel recording and web-based teaching of movement disorders. Dr. Jog has a passion for clinical and scientific innovation and holds numerous patents that are reaching commercialization with strong collaboration with university technology transfer and industry partners.
Highlights:
- How do clinician researchers take questions from the bedside and solve them at the bench using technology in order to treat movement disorders?
- How can wearable technology be used to detect movement disorders and monitor for optimized treatment – remotely from anywhere in the world?
- How can we use machine-guided sensors for personal diagnostics and therapy for essential tremors and Parkinson’s Disease?
- How can spinal cord stimulators improve movement and gait for patients, including those previously using wheelchairs and scooters?

Did you miss the event? Add your email address to our Café Scientifique invite list so that you’ll be the first to know when the next event takes place.
Sign up here.
Go to Lawson’s Facebook page to see photos from the event.
When connections break down
Lawson's Café Scientifique presents:
WHEN CONNECTIONS BREAK DOWN:
Slowing the decline to neurodegenerative diseases
In Ontario alone, an estimated 285,000 individuals currently live with some form of neurodegenerative disorder - Alzheimer’s Disease, Parkinson’s Disease, mild cognitive impairment, dementia and many others.
The experiences and symptoms for each person vary, but they share a progressive decline in their cognitive and motor function. It can affect their ability to work, socialize and live independently.
As our population ages, there is an urgent need to understand markers that will predict decline and identify targets for therapy that might improve long-term function and outcomes. This is where hospital-based research can make a real difference.
Join us on June 21 to hear an expert panel of scientists discuss groundbreaking and specialized research in this field, happening right here in London.
Scientist Panel
- Dr. Jennie Wells
- Dr. Mandar Jog
- Dr. Elizabeth Finger
- MODERATOR: Dr. Arlene MacDougall
Café Scientifique is a FREE community event hosted by Lawson Health Research Institute.
DATE: Thursday, June 21, 2018
TIME: 7 - 9 p.m. Doors open at 6:30 p.m.
LOCATION: Windermere Manor, 200 Collip Circle, N6G 4X8
PARKING: Free for event guests
*****Registration for this event is now FULL. *****
You can register to be placed on the waitlist and you will be contacted by email if a space opens up . Thank you for your interest in this event and Lawson research!
REGISTER NOW - To be placed on WAITLIST
Wide range of research showcased at Parkwood Institute Research's 2017 Spring Update
Lawson researchers at Parkwood Institute, part of the St. Joseph’s Health Care London family, work to improve both physical and mental health care based on the understanding that conditions of the body and mind are integrally linked. From studies on mobility after brain and spinal cord injury to treatment-resistant depression, a range of different research areas were highlighted on April 21, 2017 at Parkwood Institute Research’s 2017 Spring Update Half-Day event.
Parkwood Institute Research is a Lawson program that represents inter-disciplinary clinical research. At the second annual Spring Update event celebrating this work, attendees learned about research from across Parkwood Institute’s three core research themes: Cognitive Vitality & Brain Health, Mobility & Activity, and Mental Health Care. New this year was the addition of poster presentations, which provided another opportunity for researchers and trainees to promote and share their work.
Learn more about the work Lawson scientists at Parkwood Institute presented at the event:
Cognitive Vitality & Brain Health
Dr. Stephen Pasternak was one of the presenters in the Cognitive Vitality & Brain Health theme. Dr. Pasternak and his team are conducting a phase 2 randomized controlled trial looking at whether a European over-the-counter cough medicine, Ambroxol, could also treat Parkinson’s Disease Dementia (PDD).
“There are currently no effective treatments for cognitive impairment experienced by PDD patients. Existing treatments only treat the symptoms of Parkinson’s disease, but do not stop the disease process itself,” says Dr. Pasternak.
Parkinson’s disease is believed to be caused by the buildup of a protein called alpha-synuclein in the brain. Ambroxol increases the levels of an enzyme called β-Glucocerebrosidase (GCase), which has been shown to reduce the buildup of alpha-synuclein in animal and cell cultures models, suggesting that this could be used as a treatment for PDD.
This trial is well underway and the first participants have completed the first year of treatment. If successful, this trial will be the first to demonstrate that it is possible to change the underlying cause of PDD.
Mobility & Activity
As part of the Mobility & Activity themed presentations, Dr. Dalton Wolfe discussed an initiative supported by the St. Joseph’s Health Care Foundation and Ontario Neurotrauma Foundation to help improve mobility in patients with acquired brain and spinal cord injuries.
Called the Parkwood Program for Rehabilitation Innovations in Movement Enhancement (PRIME), a key goal of this initiative is to develop and implement a clinical decision support system that integrates approaches to activity-based therapy. Clinicians, researchers, administrators and IT specialists have combined their efforts to initiate development on this system.
“PRIME will provide recommendations for treatment based on patients’ injury level and type, and clinical characteristics,” says Dr. Wolfe. “It will also have suggestions for what to monitor for each patient to challenge them to optimize recovery, as well as to reduce risk of injury or secondary complications.”
This system will also enable electronic tracking of practices and outcomes, moving away from the current paper-based model and creating a practice-based research platform.
Mental Health Care
Dr. Amer Burhan presented his research on Transcranial Magnetic Stimulation (TMS) in the Mental Health Care portion of the presentations. TMS is a non-invasive method that uses magnetic fields to stimulate nerve cells in the brain. An electromagnetic coil is held against the head and short magnetic pulses are administered, causing a change in activity level in specific targeted areas and allowing for a study of the function and interconnectivity of the brain. The method has been approved to treat depression resistant to medications and has potential to be used to treat other mental and neurological disorders.
Dr. Burhan’s talk focused on the effectiveness of a certain type of TMS, bilateral theta-burst stimulation, in treating patients with depression who are not responsive to medication. This is a new method of TMS that is designed to facilitate change in brain activity and connectivity more efficiently. He presented preliminary results on the first 60 patients treated with this method. So far the treatment has resulted in significant improvement in over half of the patients.
“More studies are planned to understand predictors of response and facilitate individualized selection of treatment for patients struggling with this very disabling illness,” says Dr. Burhan.
Women with complications after pelvic mesh implants at increased risk of depression and suicide
Dr. Blayne Welk, a urologist at St. Joseph’s Health Care London, noticed that some of his patients were experiencing depression and other issues following complications related to pelvic mesh-based slings.
“A lot of patients were very emotional telling their story,” notes Dr. Welk.
“They told me about a lot of frustrations related to treatment options for complications. A lot of patients manage for years with problems and didn’t know the source of the issue, or that there is something that can be done to address it. Unfortunately, there are some cases where we can’t fix all the complications, but there are things that we can do to improve the situation. I think a lot of women get frustrated along the journey of finding that solution.”

Dr. Welk is also an adjunct scientist with ICES, associate scientist at Lawson Health Research Institute and assistant professor at Western University’s Schulich School of Medicine & Dentistry. Following his observations in the clinic, he led a research project to study the impact of the complications some women were facing.
“There have been regulatory warnings and lawsuits related to significant transvaginal mesh complications. We wanted to quantify the serious psychological complications that can occur in women as a result of complications from transvaginal midurethral slings,” said Dr. Welk.
Complications are rare but when they happen they can be difficult and challenging to fix, as well as quite impactful for patient lives. They can experience chronic pain, new or changing urinary symptoms and erosions where some of the mesh becomes exposed in surrounding tissue.
To determine whether women who experience midurethral sling mesh complications requiring surgical intervention have an increased risk of depression or self-harm behaviour, Welk's team tracked the number of Ontario women who needed a follow-up surgery to remove or fix a mesh implant and if they received treatment for depression or self-harm. The study, published in the journal JAMA Surgery, included almost 60,000 women who had the procedure January 2004 through December 2015.
The researchers found that 2. 8 per cent (1586 women) underwent a surgical procedure for a mesh complication. Of those women, 11 per cent (175 women) were treated for depression compared to eight per cent of women (4,470) who didn’t have corrective surgery. Of the women who needed corrective surgery, 2.77 per cent of women suffered from self-harm behaviour compared to only 1.15 per cent of women who did not need corrective surgery. These risks were highest in younger women, in particular those 46 years old and younger.
“Younger women are the ones who are most at risk of these mental health complications. We suspect that’s because of a stronger negative association between the complications and intimacy among this age group. They are also more likely to still be working full-time and raising children.”
The study reinforces some of the consequences that can occur from slings, and that those can be quite serious.
“It is important to note that a lot of women are going into these operations to improve their quality of life. It’s not necessarily a dangerous condition when you have stress incontinence. There is a decision made to treat it. I think that in those rare cases when someone does experience severe complications, it can lead to decisional regret.”
There is often not an easy solution, with patients often requiring multiple different therapies to address the complications. This can include pain management, surgery, consultations with pain specialists and psychological support along the way. In some cases, removing the mesh does not resolve the pain and it can be very difficult to identify which individuals will benefit from what therapy, including surgery, notes Dr. Welk.
The researchers add that when women experience midurethral sling complications, both they and their surgeons should be aware of the potential serious psychological impact of these complications.
Author block: Blayne Welk, Jennifer Reid, Erin Kelly, You (Maria) Wu.
World first discoveries allow researchers to accurately diagnose prenatal exposure syndromes and birth disorders
Researchers at London Health Sciences Centre (LHSC) and Lawson Health Research Institute are using advanced technology and artificial intelligence (AI) to diagnose rare diseases and prenatal exposure-related birth abnormalities in two studies published today in American Journal of Human Genetics and Genetics in Medicine.
The research uses technology called EpiSign™, which was developed by Dr. Bekim Sadikovic, Lawson Scientist at LHSC. EpiSign leverages AI to measure a patient’s epigenome – a unique chemical fingerprint that every person has on top of their DNA that is responsible for turning genes on or off. EpiSign can currently be used to help diagnose more than 100 genetic diseases that were previously difficult to diagnose.
In one of two newly published studies, Dr. Sadikovic’s team has found that EpiSign can be used to accurately identify patients affected by birth disorders called recurrent constellation of embryonic malformations (RCEMs). Since their discovery more than 70 years ago, attempts to identify the cause and specific diagnostic markers for RCEMs have been unsuccessful, making it challenging to provide patients and families with accurate diagnoses. EpiSign can now be used to accurately identify RCEMs for the first time using a blood test.
“Reaching an early and accurate diagnosis can be lifechanging. This is a major breakthrough that allows physicians to provide earlier and more accurate diagnosis, resulting in improved disease management,” said Dr. Sadikovic, who is also Research Chair in Clinical Genomics and Epigenomics at the Archie and Irene Verspeeten Clinical Genome Centre at LHSC. “It also has the potential to lead to health system cost savings since many patients spend years and even decades being tested to rule out other potential diseases with similar symptoms.”
In a second study, Dr. Sadikovic’s team used EpiSign technology for the first time to develop an accurate biomarker for a group of disorders called fetal valproate syndrome, which is caused by prenatal exposure to toxic levels of medication that may be used to treat bipolar disorder and migraines, or to control seizures in the treatment of epilepsy. It can result in neurodevelopmental disorders in infants, including learning, communication and motor disorders, autism, and intellectual disabilities.
“This is a significant breakthrough as it’s the first time the technology has been used to aid in diagnosis of a disease caused by environmental factors rather than genetics,” explained Dr. Sadikovic. “It highlights how epigenetics can be influenced by environmental and lifestyle factors, including diet, exercise and exposure to toxins.”

The research is ongoing as Dr. Sadikovic and his team, in collaboration with the global EpiSign Discovery Research network, are currently studying and developing biomarkers for more than 700 rare disorders. He noted the potential of this research is endless, showing promise for use in the diagnosis, prognosis and treatment of many other diseases and disorders, including cancer.
“One in 20 people have a rare disease that could present at any point in their lives and can be caused by genes, environmental exposures, or their combined effects,” he noted. “We can help diagnose a growing number of genetic diseases and, now for the first time, we can look beyond the genome and accurately measure the impact of the environment.”
These studies are a collaborative effort involving multidisciplinary teams in Canada, the United States, the United Kingdom and Europe. The first study, titled “Identification of a DNA methylation episignature biomarker for recurrent constellations of embryonic malformations,” is published in American Journal of Human Genetics. The second study, titled “Discovery of DNA methylation signature of teratogenic exposure to valproic acid,” is published in Genetics in Medicine. Funding for the research was provided by Genome Canada and Ontario Genomics, as well as in-kind support from EpiSign Inc.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Youth expectations of mental health care differ significantly from reality of care, study finds
In a recent study, researchers at Lawson Health Research Institute and Western University examined the expectations of young adults entering psychiatric treatment at an early intervention program and how those expectations differ from the reality of care. The research team found that young adults hold incorrect assumptions about the mental health care environment, relationships with care providers and the trajectory of psychiatric care.
The study included 20 patients from the First Episode Mood and Anxiety Program (FEMAP) at London Health Sciences Centre (LHSC), a novel outpatient mental health program that combines medication management and talk therapy, generally delivered by the same clinician, to help older teens and young adults with emotional concerns that fall into the categories of mood and anxiety symptoms. The vast majority of patients in the study described feelings of apprehension before entering treatment.
“Expectations and assumptions impact the way youth engage in psychiatric treatment, and their success and satisfaction with treatment,” said Dr. Sarah Armstrong, the study’s first author, a clinician-researcher at Lawson, assistant professor at Western’s Schulich School of Medicine & Dentistry and psychiatrist at FEMAP. “It’s critical that we understand the myths around mental health care so we can work to dispel them.”
The study identified three major misconceptions of patients entering care at FEMAP. The first is that patients expected a cold and unwelcoming care environment. “I thought it was umm…like you go to a psych ward and they like tie you up because they think you’re crazy,” one participant noted. Many patients acknowledged that this myth, a caricature of psychiatric care, was strongly influenced by portrayals in popular culture. In reality, they found care providers, staff members and the physical environment at FEMAP to be warm and welcoming which helped to relieve the anxiety around psychiatric care.
Patients also expected an authoritarian approach to care where they would play a passive role. This differed from the reality of care at FEMAP where patients found treatment was a collaborative effort between themselves and their care providers. Patients felt like they had a voice, that their opinions were respected and even felt comfortable disagreeing. They realized they could work towards making effective change for themselves by learning different ways of coping with symptoms and achieving personal goals.
Finally, patients expected quick treatment with an immediate recovery. The reality of treatment was more complicated, more time consuming and required more work than patients originally anticipated. For example, there was often an element of trial and error by using different treatment methods or different medications. Patients found treatment was not straight forward and it took more time than anticipated to see changes in their mental health.
“Ultimately, youth found that treatment at FEMAP was much more complex than they anticipated. However, they experienced a positive change in mindset with a strengthening of personal agency,” said Dr. Armstrong. “Their treatment fears were relieved and they valued their active role in their own care.”
The team hopes this study will be a first step in identifying myths and better preparing youth for the work involved in effective psychiatric care.
“Belief in a positive outcome often leads to better outcomes,” said Dr. Elizabeth Osuch, a clinician-scientist at Lawson, associate professor at Schulich Medicine & Dentistry and medical director at FEMAP. “Young adults are often reluctant to seek mental health care. Expectations can influence whether youth seek help to begin with. These results could help inform educational outreach about psychiatric care, helping to better align expectations with reality. But just as important, this study helps identify what youth value in the treatment provided at FEMAP and what principals would be beneficial to guide health care delivery models for emerging adults.”
The study, “Expectations vs. Reality: The Expectations and Experiences of Psychiatric Treatment Reported by Young Adults at a Mood and Anxiety Outpatient Mental Health Program,” is published in Early Intervention in Psychiatry.
Youth report improved wellbeing as result of tailored mental health services, study finds
In a new study from Lawson Health Research Institute and Western University, researchers partnered with youth receiving care at the First Episode Mood and Anxiety Program (FEMAP) at London Health Sciences Centre (LHSC) to better understand personal perspectives on care and treatment outcomes. The study found that patients experienced lasting improvements in managing their symptoms and improvements in academics, work performance and relationships, and they reported that these benefits involved being empowered by feelings of self-acceptance.
The study included 22 patients from FEMAP, a novel outpatient mental health program at LHSC that provides treatment to ‘emerging adults,’ ages 16 to 25, with emotional concerns that fall into the categories of mood and anxiety symptoms. Treatment at FEMAP takes a patient-centred approach and the research involved looking at what is meaningful and valuable to patients during their care journey.
“The transition from adolescence to adulthood is challenging. FEMAP employs an innovative model of care tailored to the needs of this complex population,” said Dr. Elizabeth Osuch, a clinician-scientist at Lawson, associate professor at Western University’s Schulich School of Medicine & Dentistry and medical director at FEMAP. “By engaging patients in a reflection of their experience, we can learn how effective the program is from the patient perspective.”
Participants shared their experiences through open-ended interviews with Dr. Osuch’s research team. Interview transcripts were collected and analyzed to determine common themes around treatment and outcomes. These themes were then presented back to the research participants for validation.
The study found that treatment led to development of coping strategies to better manage symptoms. Research participants credited these strategies for better functioning in academics, careers and personal relationships. Challenges in these areas are common among emerging adults and are often stressors that lead to youth seeking mental health care.
Participants characterized their treatment at FEMAP as an important investment in their mental health and wellbeing, and credited a collaborative partnership with their care provider for keeping them engaged in treatment. They appreciated the ease of accessing treatment at FEMAP where they could receive care from a psychiatrist, social worker, addictions counsellor, family counsellor and a psychologist, depending on their needs.
The research found that the complexities of treatment were initially frustrating to patients as they were seeking an “easy fix” to their mental health concerns, but they ultimately appreciated that mental health recovery is a journey. They valued that care providers partnered with them to set long-term treatment goals, choose the best treatment options and provide support both during and between appointments.
“Patients may prefer FEMAP over other mental health services because the care is tailored to emerging adults,” said Justin Arcaro, first author on the study and a former MSc candidate at Schulich Medicine & Dentistry and research associate at FEMAP. “There’s an important balance between recognizing emerging adults’ personal autonomy and their need for comprehensive support.”
Study results demonstrated that through treatment at FEMAP, patients realized they are not alone in their mental health journey which led to improved self-acceptance and self-compassion. Participants reported feeling empowered to create meaningful changes in their lives.
Participants also discussed the decision to seek mental health care in the first place. Many struggled with the decision of whether or not treatment was needed. “This shows a need for targeted campaigns to help emerging adults distinguish between normative feelings and those that indicate a need for help,” said Dr. Osuch.
This study also aligns with other research projects at FEMAP that suggest a need for targeted education campaigns about mental health care as a process with solutions that are not necessarily quick or easy. The research team highlights the importance of these findings in informing future funding decisions and policy around mental health care for emerging adults. The findings emphasize the need for quick engagement with a trusted care provider and an integrated treatment team that can partner with patients to support them while enhancing independent growth and self-acceptance.
The study, “Emerging adults’ evaluation of their treatment in an outpatient mood and anxiety disorders program,” is published in Emerging Adulthood.

Above: Dr. Elizabeth Osuch and Justin Arcaro
