Search
Search
A year in review: Lawson research highlights from 2018
New clinical protocol after general surgery cuts opioid prescribing in half
Recognizing the role that opioid prescribing plays in the national opioid crisis, a team of researchers at Lawson and Western University have developed a new clinical protocol called STOP Narcotics. The protocol includes a combination of patient and health care provider education and an emphasis on non-opioid pain control. The study found that they were able to reduce the overall amount of opioids being prescribed after general surgery by 50 per cent while still adequately treating a patient’s post-operative pain. Read more.

Probiotics for respiratory tract infections could save Canada nearly $100 million a year
A recent study suggests the use of probiotics to prevent respiratory tract infections in Canada could result in nearly $100 million per year in savings. There is growing evidence that probiotics can reduce the risk of respiratory tract infections and lower their frequency, as well as reduce the duration of an infection, antibiotic use and absences from work. Replicating a research model used in France, researchers examined the potential clinical and economic impacts in Canada. Read more.

Blood test can predict optimal treatment for advanced prostate cancer, study finds
An international collaborative study between Lawson, Memorial Sloan Kettering Cancer Center, the Royal Marsden and Epic Sciences is one of the first to demonstrate that a blood test can predict how patients with advanced prostate cancer will respond to specific treatments, leading to improved survival. The study used a liquid biopsy test that examines circulating tumour cells (CTCs) in blood samples from patients with advanced prostate cancer who are deciding whether to switch from hormone-targeting therapy to chemotherapy. Read more.
Machine learning could predict medication response in patients with complex mood disorders
Mood disorders like major depressive disorder (MDD) and bipolar disorder are often complex and hard to diagnose, especially among youth when the illness is just evolving. This can make decisions about medication difficult. In a collaborative study by Lawson, The Mind Research Network and Brainnetome Center, researchers have developed an artificial intelligence (AI) algorithm that analyzes brain scans to better classify illness in patients with a complex mood disorder and help predict their response to medication. Read more.
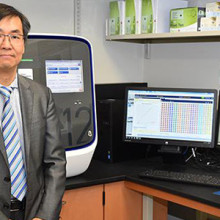
Lawson researchers receive $4.4 million to study personalized medicine at LHSC
Personalized medicine is the analysis of a patient’s DNA to predict how they will respond to medications. Led by Dr. Richard Kim, scientist at Lawson and clinical pharmacologist at London Health Sciences Centre (LHSC), researchers at Lawson have received $4.4 million to study an expanded personalized medicine program at LHSC that involves full integration of research into patient care. Read more.
Drinking more water does not slow decline of kidney function for patients with kidney disease clinical trial shows
A study published in JAMA (Journal of the American Medical Association) by researchers at Lawson and Western University found that coaching patients with Chronic Kidney Disease to drink more water does not slow down the decline of their kidney function. Read more.

Funding for unique strategy to prevent homelessness after hospital discharge
On September 10, the Ministry of Families, Children and Social Development, announced that Lawson will receive $223,572 from the Homelessness Partnering Strategy’s Innovative Solutions to Homelessness funding stream to support the project “No Fixed Address Version 2 Expansion” research project. This research will further refine the No Fixed Address strategy for reaching and supporting patients during the crucial transitional period when they are being discharged from the hospital and re-integrated into the community. Read more.

Synthetic surfactant could ease breathing for patients with lung disease and injury
Human lungs are coated with a substance called surfactant which allows us to breathe easily. When lung surfactant is missing or depleted, which can happen with premature birth or lung injury, breathing becomes difficult. In a collaborative study between Lawson and Stanford University, scientists have developed and tested a new synthetic surfactant that could lead to improved treatments for lung disease and injury. Read more.
Research team develops clinically-validated 3D printed stethoscope
A team of researchers have developed an open-source, clinically validated template for a 3D printed stethoscope for use in areas of the world with limited access to medical supplies – places where a stethoscope could mean the difference between life and death. Read more.

Family environment influences emotional well-being of children with epilepsy
Children with epilepsy have a higher risk of developing emotional and behavioural disorders, including depression, anxiety and poor self-esteem, yet it has been difficult for researchers to pinpoint why this occurs. Researchers at Children’s Health Research Institute, a Lawson program, have found that family environment influences the relationship between clinical characteristics of epilepsy at diagnosis and children’s emotional well-being two years later. Read more.

How the brain is folded provides researchers with an accurate marker to predict psychosis in high-risk patients
By using images of the brain to look at how its outer surface is folded on itself, researchers can predict which high-risk patients will develop psychosis with more than 80 per cent accuracy. Before now, there has been no way to examine young people before they become ill to reliably identify who will develop acute psychosis and who will not. Read more.
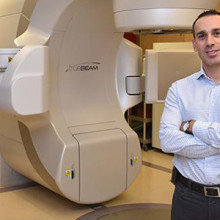
High-dose radiation can improve survival in cancer patients once thought incurable
Cancer that spreads from an original tumour to other parts of the body is generally considered incurable. In an international study led by Lawson, researchers challenged this idea by showing that high-dose radiation can improve survival in patients with cancer that has spread to five or less sites. The study called SABR-COMET was the first randomized phase II clinical trial of its kind. Read more.
Advocating for health research during “H on the Hill”
HealthCareCAN held its third annual Lobby Day “H on the Hill” event on Parliament Hill in Ottawa, on Tuesday, October 30, 2018.
Canada’s hospital CEOs and vice presidents of health research joined HealthCareCAN - the national voice of Canada’s healthcare organizations, community and research hospitals - to meet with MPs, Senators and senior government staff.
Collectively, they issued a call for federal action to unlock the tremendous economic potential of the health and life sciences sector to support better health for Canadians.
Dr. David Hill, Scientific Director for Lawson and Integrated Vice President of Research for London Health Sciences Centre and St. Joseph’s Health Care London, participated in the lobby day. Dr. Hill currently sits on the Board of Directors for HealthCareCAN.

Image

“Minister of Crown Indigenous Relations @Carolyn_Bennett, Parliamentary Secretary for Science, Sport, and Accessibility @KateYoungMP, and Dr. David Hill, catching up over lunch at #HontheHill #CDNpoli #CDNhealth”
Meeting participants stressed the need for action on HealthCareCAN’s recommendations for the 2019 federal budget, specifically:
- Setting a minimum 25% funding floor for the indirect costs of research under the Research Support Fund;
- Granting eligibility to federal infrastructure funding competitions to healthcare organizations, and;
- Investing in digital health platforms to support care, training, and research in healthcare organizations.
Diverse areas of the health and life sciences sector and key health issues were discussed, including:
- Health and science research, granting councils;
- Hospital infrastructure;
- Health innovation;
- Electronic health technology;
- Opioid crisis response;
- Mental health;
- Aboriginal health; and,
- Home care.
Read Dr. Hill’s recent column in Hospital News on bridging the gap from discovery to patient care.

HealthCareCAN provides high-quality policy research advocacy and leadership development services to our members while championing healthcare system transformation in Canada. Visit www.healthcarecan.ca to learn about our solutions to health and healthcare challenges. Follow us on Twitter: @HealthCareCAN
An image of the future: Innovations in imaging research
Lawson Health Research Institute (Lawson) has long been a leader in biomedical imaging. The first Canadian magnetic resonance imaging (MRI) of a human occurred at St. Joseph’s Health Care London (St. Joseph’s). The country’s first positron emission tomography/computed tomography (PET/CT) and positron emission tomography/magnetic resonance imaging (PET/MRI) scanners were also installed at St. Joseph’s. New developments in imaging research continue to enhance the diagnosis, prevention and treatment of a wide range of diseases, from cancer to post-traumatic stress disorder.
On May 23, Lawson hosted a Café Scientifique event where a panel of Lawson Imaging scientists discussed their cutting-edge work. Guests had the opportunity to ask questions as part of an open-forum discussion to gain insights from the speakers, and from one another.
In celebration of Canada’s 150th anniversary as a nation, this event is the first of a two-part series focusing on the future vision for health care in Canada and the legacy that research at Lawson will leave.
Imaging of the heart: Seeing the cause of chest pain more clearly
By Dr. Ting-Yim Lee, Lawson scientist, Medical Physicist at St. Joseph’s, professor at Western University’s Schulich School of Medicine & Dentistry, and scientist at Robarts Research Institute
When patients with chest pain arrive in the emergency department, they are given an electrocardiogram (ECG) and blood test. These diagnostic tests determine if the pain has a non-cardiac cause (such as heart burn), if it is caused by a heart attack, or if the patient has angina (plaque formation in the coronary arteries that either reduces or temporarily cuts off blood flow to the heart) but did not have a heart attack.
If a patient has angina, they are then given additional diagnostic testing to see whether a blood clot has formed and where it is located. This is determined by two different imaging techniques: x-ray imaging (angiogram) and nuclear imaging. This process is invasive and means that patients must be scheduled for two different exam days. Using two techniques also means that there can be image misalignment, and the images often provide poor detail.
Dr. Ting-Yim Lee’s lab has pioneered a Computed Tomography (CT) method for imaging blood flow to the heart muscle (CT Perfusion), which can help patients avoid unnecessary tests and treatment, as well as reduce health care costs.
“CT imaging is a non-invasive imaging technique that uses x-rays to create high-detail cross-sectional images of the body. Using this method, we can evaluate the degree of blockage in coronary arteries – with one diagnostic test instead of two,” says Dr. Lee.
Using light and sound to improve breast surgery
By Dr. Jeffrey Carson, Lawson scientist and associate professor at Western University’s Schulich School of Medicine & Dentistry
“Most women diagnosed with breast cancer undergo surgery, and months of chemotherapy and radiotherapy. They must deal with the discomfort, side-effects, emotional stress and financial burden of treatment. Almost one in four surgeries for breast cancer must be repeated, meaning many women have to go through this all over again,” says Dr. Jeffrey Carson.
In breast conserving surgery, there is a high chance of repeat surgery as the surgeon must see and remove 100 per cent of the tumour in order for it to be successful. They are not able to determine whether the entire tumour was removed until after the surgery has been completed.
Dr. Carson and his team at St. Joseph’s have developed a technology called Intraoperative Photoacoustic Tomography (iPAT), which has the potential to reduce the chance of repeat surgery for breast cancer. The technology is able to image surgery specimens in the operating room during surgery, allowing surgeons to determine whether the whole tumour has been removed before the surgery is complete.
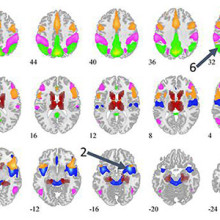
How imaging can improve the management of epilepsy
By Dr. Udunna Anazodo, postdoctoral fellow at Lawson
Most patients with epilepsy are effectively treated with antiepileptic drugs. However, 36 per cent will not respond to the drugs. For these patients, surgery on the area of the brain that is causing seizures is the standard of care – if patients are good surgical candidates.
“If patients with epilepsy are to undergo surgery there must be a good indication of where the seizure focus is and it must be possible to determine that removing this portion of the brain will not affect brain function,” says Dr. Udunna Anazodo.
To see whether they are good candidates for surgery, patients must undergo an invasive procedure called intracranial monitoring, where electrodes are placed on the brain.
Dr. Anazodo has been studying how PET/MRI can be used to map seizures with the goal of minimizing the need for invasive intracranial monitoring. This technique makes it possible to locate areas in the brain that cause seizures and to see if the seizures affect brain functions.
See photos from the event on Lawson’s Facebook page.

Above: Café Scientifique presenters (from left to right): Drs. Jeffrey Carson, Frank Prato (moderator), Ting-Yim Lee and Udunna Anazodo.
An online approach to care
With an aging population, neurological conditions like stroke, brain injury and multiple sclerosis (MS) are on the rise in Canada. Those living with neurological conditions face many long-term challenges that can affect both their physical and cognitive functioning. They are also at an increased risk for mental health challenges such as depression and anxiety.
“While mental health challenges are common for those with neurological conditions, they often go untreated for a number of reasons,” says Dr. Swati Mehta, Scientist at Lawson Health Research Institute. “For example, those living in remote areas often do not have access to specialized services and many patients are concerned about stigma.”
Yet seeking mental health care is critically important for patients with neurological conditions. “Research suggests that depression among these patients can impair recovery, leading to decreased quality of life and increased health care costs.”
To improve patient outcomes, Dr. Mehta and a collaborative research team are developing an internet-delivered cognitive behavioural therapy (ICBT) program.

Cognitive behavioural therapy (CBT) is a specialized type of therapy that involves patients learning strategies and skills to self-manage mental health symptoms. It’s one of the most widely used therapies for the treatment of depression and anxiety.
A panel of researchers, persons with lived experience of neurological conditions and community organizations are working collaboratively to develop an accessible ICBT program that meets the needs of persons with neurological conditions and mild cognitive impairment who are also experiencing symptoms of depression or anxiety. The program, called The Neuro Course, will be a modified version of an existing course developed in Australia by the eCentreClinic.
“Through co-development with patients and experts in the field, the ICBT program will meet the specific needs of persons with neurological conditions who are also experiencing mental health challenges,” explains Dr. Mehta. “With online delivery, it can provide personalized treatment while being flexible and easily accessible.”
The Neuro Course will be piloted with a small group of research participants, including patients from Parkwood Institute, a part of St. Joseph’s Health Care London. Eligible participants can sign up to be notified of the course’s availability at https://www.onlinetherapyuser.ca/neuro.
The free online course consists of six easy-to-understand CBT lessons and will take approximately 10 weeks to complete. In addition to the six lessons, participants will be encouraged to work through various activities during the week.
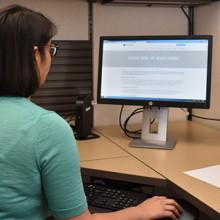
Participants will also receive regular support from a designated online guide. Guides will be health educators who are certified providers or graduate students working under the supervision of certified providers. All guides will have training in psychology or social work. The participant’s guide will review the participant’s progress and answer any questions or comments through a secure messaging system.
Participants in the study will be asked to complete brief questionnaires before they begin the course, on a weekly basis throughout the course and then again three months after treatment ends. The research team will use the questionnaires to assess patient outcomes and improve future versions of the course.
The goal of the program is to overcome barriers to face-to-face therapy, such as limited access to specialized care and concerns about stigma related to seeking care, by providing an effective online alternative. By reaching those in need, the research team hopes to improve patient outcomes and overall wellbeing.
“The long term goal would be to implement the ICBT program into clinical practice to provide increased access to mental health services among this population,” says Dr. Mehta. “The program could be used to provide care to those with mild to moderate mental health concerns or those waiting to access face-to-face programs.”
The team is being funded for this project through Lawson’s Internal Research Fund (IRF) competition. “As an early career researcher, receiving funding from Lawson’s IRF is a great honour. It’s a great opportunity to help researchers obtain funding for small feasibility studies to develop evidence for larger grants that can be used to translate knowledge across the community,” states Dr. Mehta.