Search
Search
New research on reducing harm for people who use methamphetamine
At a virtual event, a research team led by Lawson Health Research Institute announced details of the Methamphetamine Harm Reduction Project that will study the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose.
“Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk.
“We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
New research on reducing harm for people who use methamphetamine in hospital
LONDON, ON – At a virtual event today, a research team from Lawson Health Research Institute is announcing details of the Methamphetamine Harm Reduction Project that will test the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose. “Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk. “We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New research showcased at third annual Parkwood Institute Research Spring Update Half Day
More than 100 researchers, staff and trainees attended the third annual Parkwood Institute Research (PIR) Spring Update Half Day on April 27, 2018 to share their innovative research and learn about work from across PIR through interactive workshops and poster presentations.
A program of Lawson Health Research Institute and located at St. Joseph’s Health Care London’s Parkwood Institute, PIR represents three major research programs: cognitive vitality and brain health, mobility and activity, and mental health. The event allowed guests to hear about new studies and recent research developments from across these three themes.
“Parkwood Institute Research covers different research areas but what we want to emphasize with this event is the overlap and collaboration between our programs. Having an inter-disciplinary approach that encourages partnerships ultimately helps us to incorporate new knowledge into patient care at Parkwood Institute,” says Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery, and Assistant Director, Lawson.
Five interactive workshops were held on a variety of different topics, such as clinical trials, systematic reviews, innovation in health care, practice-based research methods and evaluating SMART technology. The workshops were led by some of Parkwood Institute’s research leaders, including Drs. Cheryl Forchuk, Robert Teasell, Michael Borrie, Dalton Wolfe, and Arlene MacDougall.
Attendees also had the opportunity to visit poster presentations on recent PIR projects.

Ashrafunissa Janmohammad (above), Lawson research coordinator at Parkwood Institute’s Chronic Wound Management Clinic, was one of the poster presenters at the event. She presented on a study led by Lawson associate scientist Dr. David Keast, which assessed whether chitosan gelling fibre dressing could be effective in controlling bleeding after minor wound surgery. Chitosan is derived from chitin, the structural component of the cell walls of fungi and the shells of arthropods such as crabs, lobsters, shrimps and insects.

Juweiriya Ahmed (above), a MSc candidate at Lawson and Western University’s Schulich School of Medicine & Dentistry, was another presenter. Her poster outlined a study investigating the interaction between neuroanatomical and genetic risk factors that may contribute to the development of psychotic symptoms (delusions and hallucinations) in patients with Alzheimer’s disease. Supervised by Lawson scientist Dr. Elizabeth Finger, the study could help inform the development of therapeutic targets and treatment plans.
New robotic 3D ultrasound may improve accuracy of liver cancer ablation therapy
LONDON, ON – A new system that turns ultrasounds into a 3D image could make treatment of liver cancer using thermal ablation more accurate, a new simulated study from Lawson Health Research Institute and Western University has found.
Liver cancer is the fourth leading cause of cancer death globally. While surgery is one treatment option, thermal ablation, using heat to destroy the cancerous tumour, can have fewer complications and a shorter recovery time. It can also be used for patients who are not surgical candidates.
Thermal ablation requires precise needle placement to treat the cancer without damaging the vital organs and blood vessels around it.
“It's very important that we get the needle right in the centre of the tumour,” says Dr. Derek Cool, Associate Scientist at Lawson, Assistant Professor at Western University’s Schulich School of Medicine & Dentistry and Interventional Radiologist at London Health Sciences Centre (LHSC). “If the treatment area doesn't fully cover the tumour, patients are left with a small amount of residual cancer, risking recurrence and the need for additional treatment.”
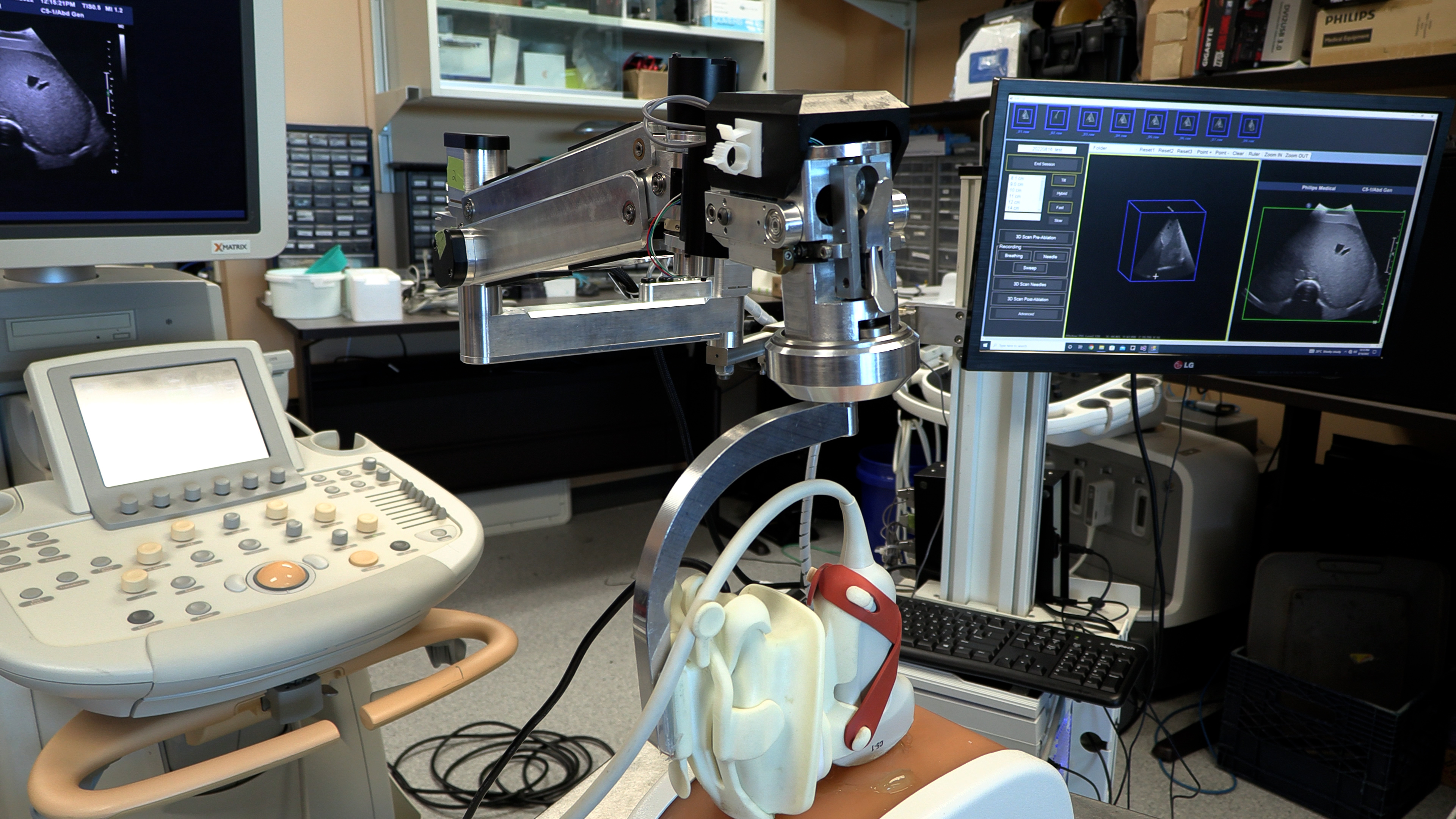
Ultrasound or CT (computerized tomography) imaging is normally used to guide needle placement, but both are limited. Ultrasound is widely available and can be done in real-time, but only delivers a 2D image. While a CT scan provides a 3D image, it isn’t in real-time and can be a lengthy process.
“We developed a new 3D ultrasound method that shows promise in analyzing whether the complete liver tumour will be ablated by the procedure,” explains Dr. Aaron Fenster, a Professor at Schulich and Scientist at Robarts Research Institute. “And we're now using the same system to guide the needle directly into the centre of the tumor.”
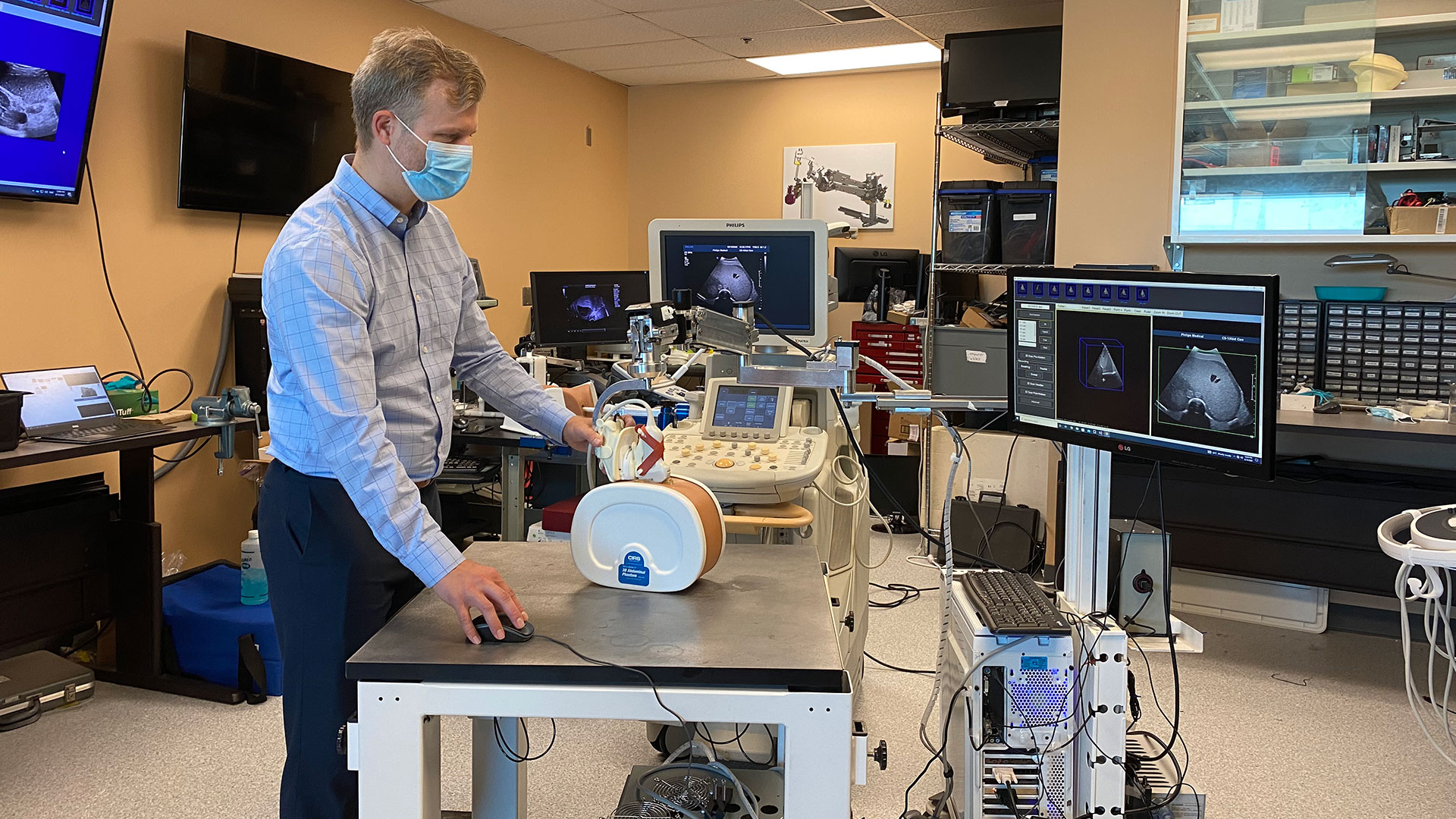
To create the 3D ultrasound images, a robotic cradle moves a standard ultrasound probe, collecting images and stacking them like puzzle pieces.
The simulated study, published in IEEE Transactions on Medical Imaging, used data from 14 patient cases at LHSC to analyze accuracy of the technology. It found that while 64.3 per cent of cases showed complete tumour coverage with standard imaging methods, the new system could result in complete coverage for 92.9 per cent of cases (13 of 14 cases). The researchers found that the remaining case could benefit from increasing the ablation time or intensity.
“Our next step is to move from simulation studies to a clinical trial,” says Dr. Cool.
If proven effective, the robotic ultrasound system’s portability could potentially allow for more widespread use of 3D ultrasound imaging, including in smaller health care centres. By eliminating the need for CT scans, it could also help to reduce imaging wait times.
“If a clinical trial shows the approach is more accurate and more precise than conventional techniques, there would be a direct impact on patient care,” says Dr. Fenster. “We hope to explore commercialization to license the technology and distribute it worldwide.”

Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study aims to improve mental health treatments for stroke patients
LONDON, ON- A team at Lawson Health Research Institute are looking to improve mental health treatments and resources for patients who have experienced a stroke. The team will recruit 100 stroke patients to assess whether the completion of a guided therapy program can improve mental health and quality of life.
Strokes affect approximately 400,000 Canadians each year and can be debilitating. They can negatively affect a person’s cognition and mobility, and severely impact mental health and wellbeing.
“More than sixty per cent of patients experience depression after stroke,” says Dr. Robert Teasell, Lawson Scientist and Physiatrist at St. Joseph’s Health Care London’s Parkwood Institute. “Having a stroke itself makes people more vulnerable and makes people feel their lives have changed negatively.”
During stroke rehabilitation, patients are typically offered mental health treatments, but the research team say it is post rehabilitation that stroke patients tend to experience worsening depression.
“Publicly funded allied health care services are available at inpatient and outpatient care; however, psychology is often limited across the rehabilitation continuum from acute to community care,” says Dr. Swati Mehta, Lawson Scientist. “We are looking at how we can provide a program that is cost effective to help those who have these barriers to access mental health services.”
The study will examine the use of cognitive behavioral therapy (CBT), which is an evidence based psychological intervention that aims to provide people with increased coping ability and self-efficacy. Participants will complete a 10-week guided program with specific targeted lessons, tailored to the needs of those post stroke, delivered virtually through a trained clinician. They will then complete a questionnaire to see if there have been any improvements to self-efficacy and emotional wellbeing.
“We have found this form of therapy (CBT) has been very effective and feasible for spinal cord injury patients with mild traumatic brain injury and we want to see how a modified version could potentially help those with stroke and depression,” says Randy Upper, Clinical Research Associate at Lawson.
If CBT is proven effective through this study, Dr. Mehta hopes it will encourage similar programming that would be available to stroke patients after rehab.
“We are hoping we can connect with community organizations and work with them to implement this program in a service delivery model that would be easily accessible for stroke patients living in the community.”
Recruitment for this study is currently underway, those interested in taking part can email Dr. Swati Mehta at: @email
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study aims to improve treatment for rheumatoid arthritis
A research team led by Lawson scientist Dr. Mamadou Diop has been awarded a Lawson Internal Research Fund to investigate whether a previously developed optical technique that can detect arthritis within one week of onset could also be used to provide early assessment of treatment response for rheumatoid arthritis (RA).
RA is a disease that causes chronic inflammation of the joints, which results in pain, reduced quality of life and loss of productivity. There is no cure for RA but a new category of drugs – biologic agents that can reduce pain and slow down or even halt disease progression – has revolutionized treatment.
However, these new drugs are expensive and only work in 30 per cent of patients, which means many RA sufferers are treated with no benefit for up to six months – the time it takes for current monitoring methods to reliably determine whether a treatment is working or not. “This is a direct consequence of the lack of sensitivity of current monitoring methods,” says Dr. Diop, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
Since their recently developed optical technique has a high sensitivity to arthritis, Dr. Diop and his team believes it could also be used as a safe and convenient method of assessing treatment efficacy in RA patients. Additionally, there are striking similarities between RA and cancer, and it has been shown that optical techniques can predict cancer in as early as one day after therapy starts.
At St. Joseph’s Health Care London, they will test this theory in a rat model of RA and compare the results of the optical technique to histology and CT imaging, other established methods of determining whether a treatment is effective.
“If successful, this project will generate a safe, low-cost technique that can detect treatment response in RA within days of starting treatment. This would reduce the risk of further joint damage experienced by many patients for whom the drugs are ineffective,” says Dr. Diop. “We hope this will enable early redirection of patients with non-responding RA to alternative treatments, such as a combination of multiple drugs and more frequent monitoring.”
Dr. Diop adds, “The Lawson IRF grant will enable us to test the validity of our hypothesis and subsequently generate valuable preliminary results to support grant proposals for larger external funding.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
New study aims to reduce recurrence of strokes by determining cause of Post-Stroke Atrial Fibrillation (PSAF)
The most frequent cause of stroke is Atrial fibrillation (AF), a cardiac arrhythmia consisting of irregular heartbeats. These strokes are the most devastating ones. Recent observations in stroke patients suggest that stroke can also cause AF. This Post-Stroke Atrial Fibrillation (PSAF), in turn, can produce more strokes.
Victoria Thorburn, a Master’s student at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry in the department of Anatomy and Cell Biology, has been awarded with a Lawson Internal Research Fund (IRF) Studentship to develop the first rodent model of PSAF. The goal of the study is to gain more understanding of the relationship between stroke and PSAF.
The cause of PSAF is currently unknown but it is believed that strokes occurring in the insular cortex, a brain region responsible for monitoring heart rhythm, may trigger PSAF. When this brain region is damaged by stroke, the heart is left without regulation, resulting in chaotic heart rhythms. Previous studies have not been able to confidently diagnose PSAF, since approximately one third of AF cases are silent or asymptomatic.
“Without continuous monitoring of heart rhythm prior to stroke, it is difficult to determine if PSAF is in fact a newly developed arrhythmia occurring after stroke or whether it was actually a silent form of AF that already existed before stroke,” Thorburn says.
Thorburn will experimentally induce stroke in the rat insular cortex to determine whether PSAF or other types of irregular heartbeats occur as a result. The project will be supervised by Dr. Luciano Sposato, Lawson scientist, physician at London Health Sciences Centre and associate professor in the Department of Clinical Neurological Sciences at Schulich, and Dr. Shawn Whitehead, assistant professor at Schulich. They will monitor heartbeat before and after insular stroke then assess potential biological factors or structural changes in the brain or heart that may be associated with PSAF. Animals that developed PSAF will be compared to those without the condition.
Since the proposed cause of PSAF, the involvement of insular cortex damage, differs greatly from the traditional cause of AF, which is often a structural abnormality in the heart, there could also be a difference in treatment. The hope is that the knowledge of PSAF formation gained from the first rodent model will lead to the development of prevention and therapeutic strategies, minimizing the number of stroke patients affected by PSAF and ultimately reducing the recurrence of stroke.
“I wanted to become involved with research that was currently relevant and had the translational potential to improve public health. With the current aging population, the number of individuals directly affected by stroke and AF will continue to rise,” says Thorburn. “Thanks to funding opportunities like Lawson’s IRF, students like myself are able to train alongside accomplished researchers and participate in research that uniquely integrates both basic science and clinical perspectives.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
New study aims to understand team-based care for chronic disease management
Chronic diseases, such as chronic obstructive pulmonary disease (COPD), are complex and require thorough care to help manage the condition. Patients often need support from an integrated team of health care professionals who work in different settings.
Dr. Shannon Sibbald, associate scientist at Lawson Health Research Institute, is leading a study to better understand integrated health care teams for chronic disease management and factors that help successful implementation.
Integrated team-based models of care include multiple health care providers working together to support patients with complex needs, such as those with chronic disease. There are many benefits to integrated team-based models of care. Patient outcomes are improved, health care providers feel more supported in their work and services are less likely to be duplicated.
Dr. Sibbald’s research focuses on chronic obstructive pulmonary disease (COPD), a devastating chronic disease affecting normal lung function in over 1.5 million Canadians. COPD is one example of a chronic disease where patients can benefit from team-based care. COPD is often underdiagnosed, and patients with COPD and other chronic diseases may not be receiving the ideal care for their condition.
While integrated team-based care is important, there are currently few studies to guide implementation. In this study, Dr. Sibbald’s research team will engage health care providers and patients to gain a rich understanding of successful integrated approaches to chronic disease management, including how team-based models of care are implemented. The team will also work to better understand how patients with chronic diseases view such models, and what their hopes and expectations are for their care.
“We want to explore innovative and successful approaches to implementing team-based models of care,” explains Dr. Sibbald. “We’re looking to learn how these methods can support practice, improve patient outcomes and spread innovation.”
The team will look at high performing integrated care teams that support current best practices at a family health team in London, Ontario.
When models are applied to practice, context is an important part to consider. For chronic diseases, context is often broad and elaborate. They hope to gain insight into what works well and what does not in dynamic contexts, and gain a better understanding of implementation facilitators and barriers.
The ultimate goal is to build knowledge that will support implementation and sustainability of high-performing integrated health teams across our health system.
“While motivation and momentum to use integrated teams is high, there is little guidance on how to do this well,” says Dr. Sibbald. “This research will provide insight into what works and what does not, reducing our gap in knowledge.”
Dr. Sibbald received a Lawson Internal Research Fund (IRF) grant to conduct this pilot study. Once complete, Dr. Sibbald’s team hopes to expand the study to look at integrated care models at other sites across the province.
"The IRF grant enables our team to validate our methods of evaluating the implementation of interprofessional team-based care in complex settings," adds Dr. Sibbald. "By examining the impact team-based care for patients with COPD, we hope to demonstrate the relevance of our findings, to support grant proposals."
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
New study examining if probiotics can improve outcomes in knee replacement surgeries
Researchers at Lawson Health Research Institute are examining whether the use of a daily probiotic can improve outcomes in patients who undergo a total knee replacement surgery.
There are more than 70,000 knee replacement surgeries in Canada each year, and up to 10 per cent of patients experience complications following the procedure.
“One in five patients are dissatisfied after surgery due to pain and discomfort, and some patients need a repeat surgery because there is complication, infection or loosening of the joint,” says Dr. Matthew Teeter, Lawson Scientist at London Health Sciences Centre (LHSC).

Dr. Teeter and the research team are focused on improving patient outcomes. Recognizing that knee replacement patients who are considered healthy tend to have better outcomes, they are interested in how they can better support patients’ overall health as one way to optimize their outcomes.
“The knee replacement patients I see in clinic are very diverse - from young healthy active patients to medically complex to socioeconomically disadvantaged,” says Dr. Brent Lanting, Lawson Scientist and Orthopaedic Surgeon at LHSC. “We know those with poor health do not do as well as those with good health, good diet, and good supports. This study is profound in that it investigates a core aspect of our health – the gut microbiome.”

The research team will recruit 30 participants who are scheduled for a knee replacement surgery. Half of the participants will receive a daily probiotic for six-weeks ahead of the surgery, and the other half will act as a control group.
“Our microbiome is a large part of why we are healthy. A healthy person has a microbiome that produces vitamins and other things which cross over to our system and helps promote healing,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London. “We are hoping it will improve more deep healing and prevention of the rejection of the joint by improving the microbiota by giving probiotics.”
The team will assess outcomes using CT imaging, looking at the bone and implant and how it is fixing into place. They will also use PET/MRI to look at the cellular activity around the joint and inflammation.
“This should give us a sharp focus of what is going on with the joint and help us determine if there was a positive effect by using probiotics,” explains Dr. Teeter.
If the pilot study proves to be promising, the team will then work towards a larger clinical trial, combining probiotics into pre-surgical care.
“Ultimately, we want better patient outcomes with a simple treatment,” adds Dr. Burton. “If we can help improve outcomes with the use of a daily probiotic, that is a great win.”
The research team received a New Frontiers in Research Fund (NFRF) of $250,000 over three years to conduct this study.
New study finds exercise, cognitive training combo boosts mental sharpness in seniors
In a ground-breaking discovery that could reshape the approach to elderly cognitive care, Western University and Lawson Health Research Institute researchers have found that a combination of computerized cognitive training and aerobic-resistance exercises (such as walking and cycling along with weight training) can significantly improve cognitive functions, such as memory, attention, recognition and orientation, in older adults with Mild Cognitive Impairment (MCI).
The researchers found the effect of the combined intervention was larger than the individual effects of exercise or cognitive training alone, suggesting a synergism in the sequential combination. They also found Vitamin D supplements, on the other hand, did not appear to contribute to improvement.
According to the latest data published by the Alzheimer’s Association, the global prevalence of dementia is on the rise, impacting over 50 million individuals and costing more than $800 billion. These alarming statistics underscore the imperative to identify new and effective strategies to address neurodegenerative diseases.
The study, led by Western Professor and Lawson Scientist Dr. Manuel Montero-Odasso, offers a new pathway to address declining mental sharpness in the aging population by incorporating aerobic-resistance exercises along with computer-based cognitive training.
“This trial opens new doors in the realm of nonpharmacological interventions for MCI,” said Dr. Montero-Odasso, professor in the departments of medicine, and epidemiology and biostatistics at Schulich School of Medicine & Dentistry and director of Lawson’s Gait & Brain Lab.
“We found through a multidomain approach that pairs aerobic and resistance exercises with computerized cognitive training, there may be hope in delaying the progression from MCI to dementia.” Dr. Montero-Odasso is also a Geriatrician at St. Joseph’s Health Care London and co-lead of the Canadian Therapeutic Platform Trial for Multidomain Interventions to Prevent Dementia (CAN-THUMBS UP) at the Canadian Consortium on Neurodegeneration in Aging (CCNA).
The multi-city clinical trial, published in JAMA Network Open, included 175 participants aged between 60 and 85 with MCI – an intermediate state between normal cognitive aging and early dementia – which is also considered a critical period for early treatments and preventive strategies to address cognitive decline. The 20-week study was structured into five arms, focusing on the combination of different interventions.
The findings show that aerobic-resistance exercises did contribute to improvements in cognition, but it was the addition of cognitive training that truly made a difference. Notably, the addition of vitamin D supplementation did not show any significant benefit. Though previously argued to enhance cognition due to its neuroprotective attributes, the vitamin did not contribute to the overall success of the interventions.
The study, known as the SYNERGIC Trial (Synchronizing Exercises, Remedies in Gait and Cognition), was conducted across five Canadian academic institutions with core of the interventions at the London site – exercise and cognitive training – completed at Western’s Laboratory for Brain and Heart Health.

“The SYNERGIC Trial goes beyond mere numbers and statistics; it’s about understanding the many sides of cognitive health,” said Dr. Kevin Shoemaker, co-author of the study. Dr. Shoemaker is a professor in the School of Kinesiology at Western and Canada Research Chair in the Integrative Physiology of Exercise and Health.
“By bringing together various interventions, we are creating a comprehensive view of well-being that reaches beyond pills and conventional treatments. These findings could lead to real, significant improvements in the lives of people with mild cognitive impairment, changes that could genuinely enhance their quality of life,” said Dr. Shoemaker.
“This is an important advance from a national CCNA team led by Dr. Montero-Odasso. The study shows clearly that intense exercise and cognitive training is an effective and feasible lifestyle intervention that clearly slows the decline in brain function in people with Mild Cognitive Impairment. We are proud that Canadian scientists have shown this to the world,” said Dr. Howard Chertkow, Scientific Director, CCNA, and Chair in Cognitive Neurology and Innovation and Senior Scientist, Baycrest Health Sciences and Rotman Research Institute.
The next phase of the trials
The researchers are now conducting the next phase of the trial. The SYNERGIC-2 trial will provide virtual, at-home interventions to 550 study participants with MCI, including personalized one-on-one coaching, to help make lifestyle and behavioural changes. This trial is being conducted by the Mobility, Exercise and Cognition (MEC) Team which is part of the CCNA.
The SYNERGIC Trial is part of the Canadian Therapeutic Platform Trial for Multidomain Interventions to Prevent Dementia (CAN-THUMBS UP) CCNA’s platform dedicated to dementia prevention and risk reduction research. This work was supported by CCNA, which receives funding from the Canadian Institutes of Health Research (CIHR) and other partner organizations.
The team of researchers involved in the study led by Dr. Montero-Odasso also included Western professors Guangyong Zou and Mark Speechley, Lawson researcher and adjunct professor Frederico Pieruccini-Faria and London Health Sciences Centre statistician Surim Son.
The trial was conducted at five Canadian academic institutions: Western (sponsor site), University of Waterloo, Wilfrid Laurier University, University of Montreal and University of British Columbia.
New study looking at advanced imaging to optimize treatments for prostate cancer patients
Advanced imaging will help better guide radiation treatments
MEDIA RELEASE
For Immediate Release
January 12th, 2022
London, Ontario- Prostate cancer is the most common cancer among Canadian men, and it is estimated that one in eight men will be diagnosed with prostate cancer within their lifetime. Researchers at both Lawson Health Research Institute and Sunnybrook Research Institute, are teaming up on a study which is pairing advanced imaging technology with high precision short course radiotherapy, that could lead to better outcomes for patients.
“We have started to look at ways to integrate advanced imaging to help better understand the amount of cancer in the prostate and the location of cancer in the prostate to help guide radiation treatments,” says Lawson Scientist, and Radiation Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Dr. Glenn Bauman.
Currently when radiation is done, a computer tomography scan (CT) gives radiologists the location and boundary of the prostate, but it doesn’t give details about the location of the cancer within the prostate.
“What we are doing in the study is integrating two other forms of imaging; magnetic resonance imaging (MRI) and prostate specific membrane antigen (PSMA) PET scans, both of which can give information on the exact location of the cancer,” explains Dr. Bauman. “This will allow us to refine the radiation treatment and to target the cancer with more intensified radiation.”
Scientist at Sunnybrook Research Institute, Dr. Andrew Loblaw says using advanced imaging will also pinpoint if the cancer has moved into other areas of the pelvic region, which helps target all possibilities and lessens the chance of the cancer coming back. The type of radiation being used for this study is called stereotactic body radiotherapy (SBRT) which is more accurate, and reduces both radiation side effects to adjacent organs, while also reducing treatment visits.
“The combination of PSMA and SBRT gives us the ability to save some normal tissue and dramatically reduce treatment times,” explains Dr. Loblaw. “If we know the cancer is in one place and not another, we can spare radiation from areas not needing it which spares side effects.”
The team plans to recruit 50 men for the study that have advanced prostate cancer and need more intense treatments. Participants will undergo the advanced PSMA PET imaging at St. Joseph’s Health Care London. The same imaging techniques will be used to determine and track if the cancer is responding well to treatments.
“This is a smarter tool that will help us more accurately know what patients have,” says Dr. Loblaw. “We will know if they have more of a metastatic disease and who has localized disease. Cure rates are better when you know exactly what you are trying to cure.”
Study participants will be closely monitored for five years, to determine the success of the more targeted and intense radiation treatments. Dr. Bauman says this will also help quickly identify the potential need for more advanced therapies.
“Our treatments are good, but If there is a man we haven’t cured we want to know as soon as possible.”
The study has received funding by the Ontario Institute for Cancer Research (OICR) as part of the Institute’s new initiative that supports pre-clinical research and new clinical trials that focus on early stage, and recurrent cancers.
-30-
About Lawson Health Research Institute: Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
About Sunnybrook Research Institute: Sunnybrook Research Institute (SRI) is the research arm of Sunnybrook Health Sciences Centre, an internationally recognized academic health sciences centre fully affiliated with the University of Toronto. SRI is one of the fastest growing hospital-based research enterprises in Canada with well-established programs in basic and applied sciences which span across three scientific platforms and ten clinical programs, developing innovations in care for the more than 1.3 million patients the hospital cares for annually. Recognized as a Centre of Excellence in focused ultrasound, SRI has one of the most comprehensive and successful focused ultrasound research programs in the world, with technical, scientific and clinical experts accelerating progress in the field.
FOR MORE INFORMATION, PLEASE CONTACT:
Celine Zadorsky
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C. 519-619-3872
@email
www.lawsonresearch.ca/news-events
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study sheds light on the connection between the microbiome and kidney stones
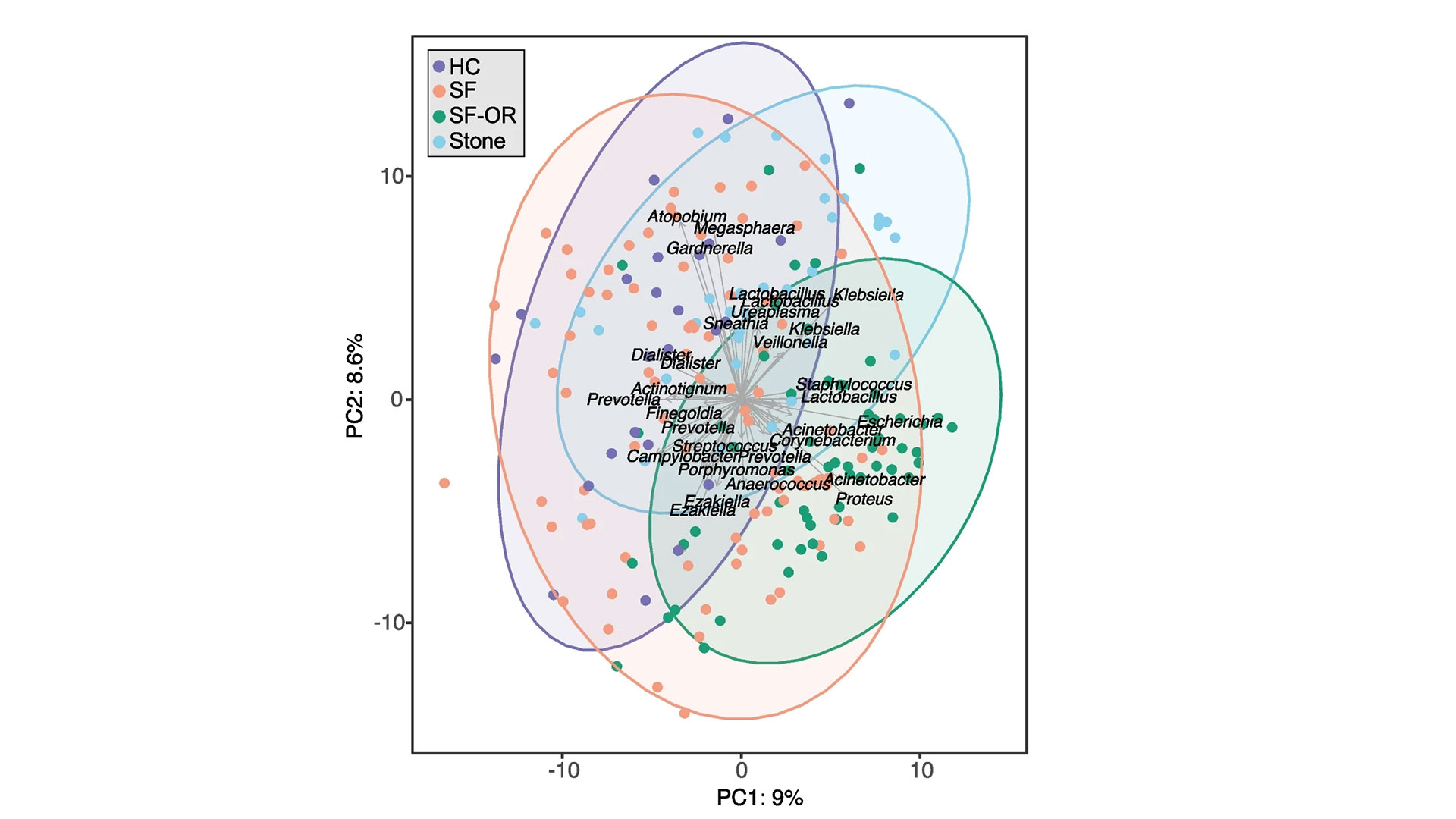
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study sheds light on the connection between the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
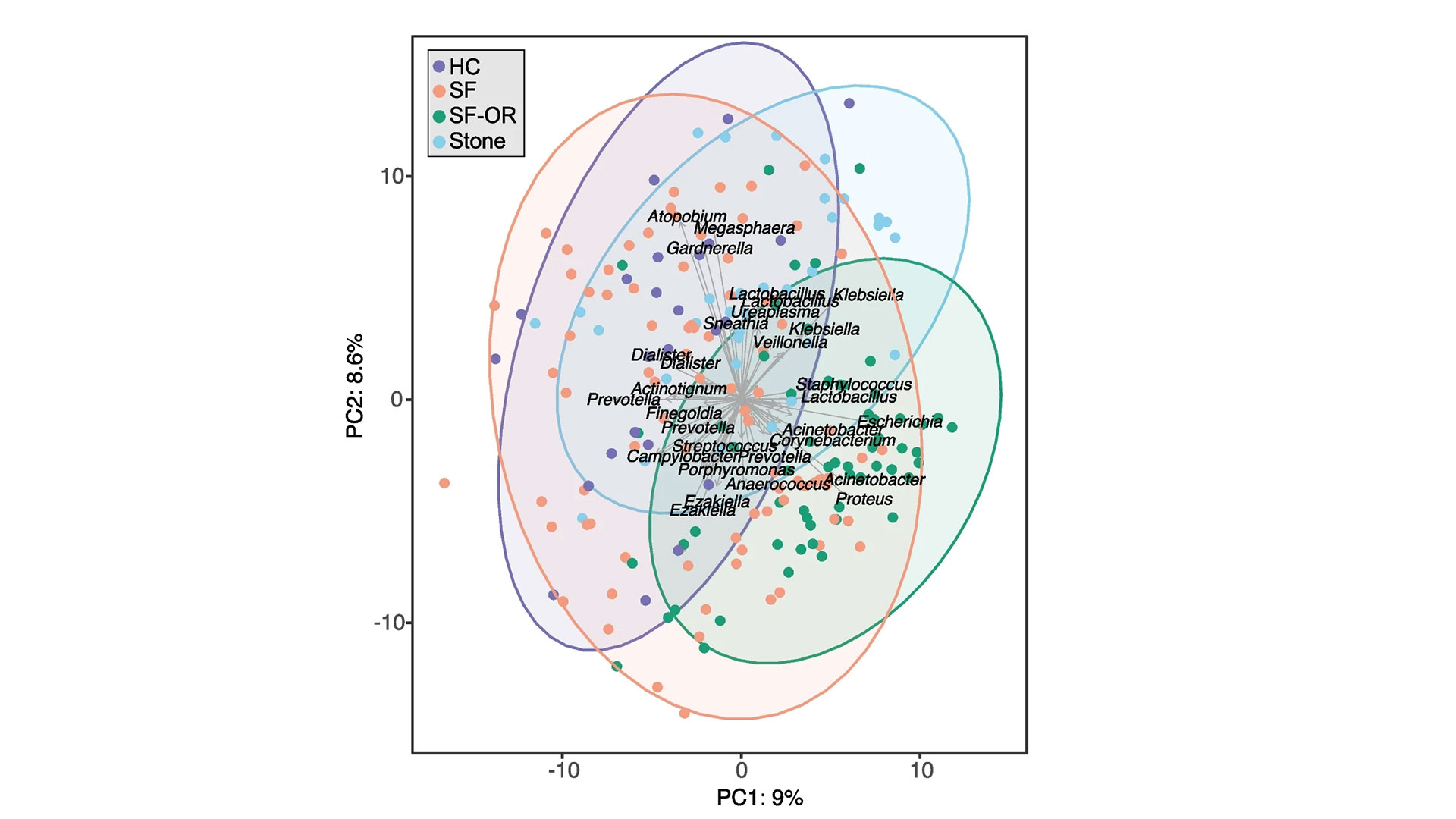
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study shows technology could play an important role in mental health support
LONDON - In a study published in MDPI Journal, a team of researchers at Lawson Health Research Institute have shown that the use of technology may assist in better outcomes for those living with both mental health and physical disorders.
Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson, and her team embarked on a pilot study that used smart home monitoring solutions to assist those living with both a mental health disorder and other health challenges. The purpose of this pilot study was to see if technology could improve overall lifestyle and wellbeing.
“We began our research by using hospital prototype apartments – apartment style care spaces within hospital settings – that were equipped with smart home technology solutions such as a screen device, activity trackers, weigh scales and medication dispensers,” says Dr. Forchuk who is also the Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery at St. Joseph’s Health care London. “Once we tested it in a hospital setting, we wanted to find a way to take this idea out into the community in different kinds of housing and living situations to see if it would be beneficial.”
The research team partnered with the Canadian Mental Health Association (CMHA) and the London and Middlesex Community Housing (LMCH) to work together to retrofit the homes of the 13 study participants.
“We worked together with the participants and their care providers to choose what combination of technology they felt would be best for them,” says Dr. Forchuk. “No matter their health condition each participant wanted to be more active and independent, with the goal of staying out of hospital.”
All smart devices were connected to the Lawson Integrated Database, which is a database that can securely collect data from multiple sources such as health devices. This allowed care providers to send reminders to participants, while also tracking usage and results.
“The key benefits we noted was that study participants started to live healthier lives,” says Jonathan Serrato, Lawson Research Associate. “Participants logged going for walks and exercising more often, as well as making healthier food choices. Those who used the medication dispensers did not miss a single dose. The touch screen devices also allowed participants to easily communicate with care providers and support networks, and access more resources.”
Following the pilot study, the research team also published a subsequent paper, as a ‘how-to guide’ for utilizing smart home technology interventions as a health care tool.
“This paper is a helpful resource that outlines implications and considerations when it comes to smart home technologies,” adds Serrato. “There are many areas we touch upon such as security, privacy and feasibility as well as hardware and software information for those who would like to take on their own similar type of smart home technology project.”
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study suggests blood plasma proteins hold answers to better understanding long COVID
LONDON - Recently published in The Journal of Translational Medicine, a team at Lawson Health Research Institute has discovered unique patterns of blood plasma proteins in patients with suspected long COVID that could act as a potential drug target to improve patient outcomes.
Currently, approximately 10-20 per cent of people with a confirmed case of COVID-19 will get long COVID.
“Those patients experience a wide variety of symptoms, which may include fatigue, brain fog and difficulty breathing,” says Dr. Douglas Fraser, Lawson Scientist and Critical Care Physician at London Health Sciences Centre (LHSC). “Their quality of life can be significantly altered, so anything that we can do to learn about this disorder and identify potential treatment targets is very important.”
Called “the plasma proteome,” the proteins being studied are found in blood plasma and are released by cells that often play an important role in the body’s immune response to viruses. The research team is studying how those proteins adapt and change in long COVID.
“Trying to understand this mechanism is quite important because it provides further insight into how patients are affected,” says Dr. Michael Nicholson, Associate Scientist at Lawson and Respirologist at St. Joseph’s Health Care London (St. Joseph’s). “This paper sheds further light onto a possible mechanism which may provide insight into why some patients have certain symptoms.”
As part of the study, blood plasma samples were collected from long COVID outpatients through the Post-Acute COVID-19 Program at St. Joseph’s and analyzed in comparison to acutely ill COVID-19 inpatients at London Health Sciences Centre (LHSC), as well as compared to a group of healthy volunteers.
“We used novel technologies for this study, allowing us to analyze more than 3,000 proteins in blood plasma at the same time with multiple patients,” explains Cristiana Iosef, Research Analyst at Children’s Health Research Institute (CHRI), a program of Lawson. “We used novel bioinformatic pipelines, a form of artificial intelligence (AI), to then analyze the proteins to determine the specific changes that occur in long COVID.”
By using advanced technology the researchers were able to determine unique patterns in the blood proteins. The team discovered that people with suspected long COVID have prolonged inflammation associated with changes in their immune cells and blood vessels. These changes may lead to problems in specific organs, like the brain and the heart.
Dr. Fraser, who is also a Professor at Western University, adds that the proteins discovered could act as a potential drug target. The team is now examining potential new drug therapies with the hopes of improving outcomes for these patients.
“When we identify these signaling patterns within the blood plasma, we can then take the information and screen drug databases to better understand which drugs would be best to target the changes we identified in long COVID patients,” says Dr. Fraser. “With this understanding, the identified drugs may be used in future long COVID clinical trials.”
This research, which used multiple state-of the-art technologies, was enabled by existing expertise and infrastructure through CHRI.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study suggests blood plasma proteins hold answers to better understanding long COVID
Recently published in The Journal of Translational Medicine, a team at Lawson Health Research Institute has discovered unique patterns of blood plasma proteins in patients with suspected long COVID that could act as a potential drug target to improve patient outcomes.
Currently, approximately 10-20 per cent of people with a confirmed case of COVID-19 will get long COVID.
“Those patients experience a wide variety of symptoms, which may include fatigue, brain fog and difficulty breathing,” says Dr. Douglas Fraser, Lawson Scientist and Critical Care Physician at London Health Sciences Centre (LHSC). “Their quality of life can be significantly altered, so anything that we can do to learn about this disorder and identify potential treatment targets is very important.”
Called “the plasma proteome,” the proteins being studied are found in blood plasma and are released by cells that often play an important role in the body’s immune response to viruses. The research team is studying how those proteins adapt and change in long COVID.
“Trying to understand this mechanism is quite important because it provides further insight into how patients are affected,” says Dr. Michael Nicholson, Associate Scientist at Lawson and Respirologist at St. Joseph’s Health Care London (St. Joseph’s). “This paper sheds further light onto a possible mechanism which may provide insight into why some patients have certain symptoms.”
As part of the study, blood plasma samples were collected from long COVID outpatients through the Post-Acute COVID-19 Program at St. Joseph’s and analyzed in comparison to acutely ill COVID-19 inpatients at London Health Sciences Centre (LHSC), as well as compared to a group of healthy volunteers.

“We used novel technologies for this study, allowing us to analyze more than 3,000 proteins in blood plasma at the same time with multiple patients,” explains Cristiana Iosef, Research Analyst at Children’s Health Research Institute (CHRI), a program of Lawson. “We used a novel bioinformatic pipeline, a form of artificial intelligence (AI), to then analyze the proteins to determine the specific changes that occur in long COVID.”
By using advanced technology the researchers were able to determine unique patterns in the blood proteins. The team discovered that people with suspected long COVID have prolonged inflammation associated with changes in their immune cells and blood vessels. These changes may lead to problems in specific organs, like the brain and the heart.
“The saved blood plasma samples that we are using helped us determine the long-term responses to COVID-19; serial blood plasma samples from individuals that had a COVID-19 infection and now presumed long COVID will help us determine how proteins are changing over time,” says Dr. Michael Knauer, Associate Scientist at Lawson.
Dr. Fraser, who is also a Professor at Western University, adds that the proteins discovered could act as a potential drug target. The team is now examining potential new drug therapies with the hopes of improving outcomes for these patients.
“When we identify these signaling patterns within the blood plasma, we can then take the information and screen drug databases to better understand which drugs would be best to target the changes we identified in long COVID patients,” says Dr. Fraser. “With this understanding, the identified drugs may be used in future long COVID clinical trials.”
This research, which used multiple state-of the-art technologies, was enabled by existing expertise and infrastructure through CHRI.
New study to assess pandemic's impact on Canadian Veterans and their spouses
LONDON, ONTARIO - Lawson Health Research Institute and the Centre of Excellence on Post-Traumatic Stress Disorder (PTSD) are partnering with a population at high risk of mental illness – Canadian Veterans and spouses of Canadian Veterans – to study how they have been impacted by the COVID-19 pandemic. Through online surveys, the project will hear directly from Veterans and their spouses to assess the pandemic’s effects on their wellbeing over time. The team hopes results can be used by health care workers and policymakers to support Veterans and their families during both the current pandemic and future public health emergencies.
“With concerns about COVID-19 infection and drastic changes to everyday life, the pandemic is taking a toll on the health of Canadians,” explains Dr. Don Richardson, Lawson Associate Scientist and Director of the MacDonald Franklin Operational Stress Injury (OSI) Research Centre. “And it may be particularly distressing for those vulnerable to mental illness.”
Population studies show that Canadian Veterans are at double the risk of mental illness when compared to the rest of the population. They experience higher rates of depression, anxiety and loneliness. Spouses of Canadian Veterans are also at higher risk of distress, sometimes undertaking significant caregiving responsibilities that lead to less independence.
“It’s currently unknown how the pandemic will impact Veterans and their spouses, but it could result in particularly serious outcomes,” says Dr. Anthony Nazarov, Associate Scientist at Lawson and the MacDonald Franklin OSI Research Centre. “We want to hear from all Canadian Veterans and their spouses, whether they’re doing well or not and whether they’re seeking care or not.”
The study aims to recruit 1,000 Canadian Veterans and 250 spouses of Canadian Veterans. Participants will complete online surveys, available in both English and French, once every three months for a total of 18 months. They will be asked questions about their psychological, social, family-related and physical wellbeing, and any relevant changes to their lifestyle and health care treatment.
“Veterans who regularly access health care services could encounter significant changes, including a move to virtual care appointments. This could lead to increased caregiving responsibilities for spouses,” says Dr. Nazarov. “Given the uncertainty surrounding the pandemic, these changes may persist well into the future, mandating a thorough assessment of patient satisfaction and treatment outcomes.”
The team hopes results can be used to support the wellness of Veterans and their families during public health emergencies. This includes providing health care professionals and policymakers with information to guide emergency preparedness policies and health care delivery models. They hope results can also be used to recognize early signs of distress in order to target with early interventions.
“We are seeking to understand the impact of COVID-19 on Veterans and their families to identify if this global pandemic is leading to psychological distress or triggering historical traumas,” says Dr. Patrick Smith, CEO of the Centre of Excellence on Post-Traumatic Stress Disorder. “The Centre’s primary goal is to increase Canadian expertise related to military and Veteran mental health, suicide prevention and substance use disorders. This study can help us understand if the pandemic is having debilitating and life-altering effects, and help us address a potential mental health crisis.”
Interested Canadian Veterans and spouses of Canadian Veterans can learn more about the study at www.veteransurvey.ca.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Centre of Excellence on Post-Traumatic Stress Disorder and Related Mental Health Conditions is located at the Royal Ottawa Hospital and is funded by Veterans Affairs Canada. Its goal is to build strong community networks to create the best possible supports and services for Veterans, first responders, service providers, and their families. It does this through knowledge and practice activities:
- conducts and facilitates applied research in PTSD and related mental health conditions
- widely shares information and knowledge about PTSD and mental health conditions and how to treat them
- transforms knowledge into training and resources to ensure veterans, first responders, and service providers, and their families are receiving the best possible supports and services
- shares standards for emerging and best practices with policy makers, mental health professionals, the Veteran Affairs Canada network of Operational Stress Injury Clinics, and Canadian Forces Health Services
The Centre’s primary goal is to increase Canadian expertise related to military and veteran mental health, suicide prevention, and substance use disorders, ultimately making this knowledge available to any first responders, family members, service providers, and researchers across Canada.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study using nuclear medicine and rare isotopes in the fight against cancer
London - In a national multicentre study, scientists at Lawson Health Research Institute and Western University are working to create rare isotopes that will be used as an important tool to help treat cancer.
Currently, radiation therapy is a staple in cancer treatment, with approximately 50 per cent of cancer patients receiving radiation at some point in their cancer journey. Although a very effective tool, traditional radiation therapies rely on intense beams of energy. These beams can kill cancer cells, but their use is limited to select locations, making them less suited for difficult-to-treat metastatic cancers that have spread to multiple sites.
“Cancer treatment has evolved over the years with targeted drugs that go straight to the cancer and advanced radiation therapy. However, radiation comes from an external source that can damage other areas in the body,” says Dr. Len Luyt, Lawson Scientist and Professor at Western. “We are now working to advance treatment further by combining radiation and targeted drug therapy.”
The therapies work like a homing device — using specially designed molecules to seek out and deliver radioactive isotopes directly to cancer cells, wherever they might be in the body.
The multidisciplinary research team involves researchers at Lawson, Western University, University of British Columbia, BC Cancer, TRIUMF, Simon Fraser University, Université Laval, Université de Sherbrooke, University of Toronto and University of Alberta.
“This is the holy grail of cancer treatment. These disease-targeting molecules circulate throughout the body, binding tightly to cancer cells in order to eliminate them with a highly localized blast of energy,” explains principal investigator Dr. François Bénard, Professor of Radiology and Associate Dean at UBC’s Faculty of Medicine, and Senior Executive Director of the BC Cancer Research Institute.
The London, Ontario team will focus on developing the radio pharmaceuticals at labs in the London Regional Cancer Program at LHSC, the Cyclotron located at St. Joseph’s Health Care London, and at Western.
“The radio pharmaceuticals we are designing will be very specific to certain receptor proteins that are on cancer cells and not elsewhere on the body. This allows us to bring the isotopes to the cancer cells and clear it from the body so you have less side effects in other areas,” says Dr. Luyt. “This approach is showing promise in prostate cancer and now this team-based approach is looking at targeting any metastatic cancer.”
This collaborative research project has received $23.7 million in federal funding through the New Frontiers Research Fund (NFRF) over six years.
“We will establish Canada as a world leader in the field of nuclear medicine and ensure Canadian patients are the ones who benefit,” adds Dr. Bénard. “By developing these medicines in Canada and bringing them into local clinical trials, we will ensure Canadians have access to innovative cancer treatments sooner.”
The team hopes to bring multiple drug candidates into clinical trials in the coming years with the ultimate goal of developing an effective treatment for metastatic cancer patients.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study using nuclear medicine and rare isotopes in the fight against cancer
In a national multicentre study, scientists at Lawson Health Research Institute and Western University are working to create rare isotopes that will be used as an important tool to help treat cancer.
Currently, radiation therapy is a staple in cancer treatment, with approximately 50 per cent of cancer patients receiving radiation at some point in their cancer journey. Although a very effective tool, traditional radiation therapies rely on intense beams of energy. These beams can kill cancer cells, but their use is limited to select locations, making them less suited for difficult-to-treat metastatic cancers that have spread to multiple sites.
“Cancer treatment has evolved over the years with targeted drugs that go straight to the cancer and advanced radiation therapy. However, radiation comes from an external source that can damage other areas in the body,” says Dr. Len Luyt, Lawson Scientist and Professor at Western. “We are now working to advance treatment further by combining radiation and targeted drug therapy.”

The therapies work like a homing device — using specially designed molecules to seek out and deliver radioactive isotopes directly to cancer cells, wherever they might be in the body.
The multidisciplinary research team involves researchers at Lawson, Western University, University of British Columbia, BC Cancer, TRIUMF, Simon Fraser University, Université Laval, Université de Sherbrooke, University of Toronto and University of Alberta.
“This is the holy grail of cancer treatment. These disease-targeting molecules circulate throughout the body, binding tightly to cancer cells in order to eliminate them with a highly localized blast of energy,” explains principal investigator Dr. François Bénard, Professor of Radiology and Associate Dean at UBC’s Faculty of Medicine, and Senior Executive Director of the BC Cancer Research Institute.
The London, Ontario team will focus on developing the radio pharmaceuticals at labs in the London Regional Cancer Program at LHSC, the Cyclotron located at St. Joseph’s Health Care London, and at Western.
“The radio pharmaceuticals we are designing will be very specific to certain receptor proteins that are on cancer cells and not elsewhere on the body. This allows us to bring the isotopes to the cancer cells and clear it from the body so you have less side effects in other areas,” says Dr. Luyt. “This approach is showing promise in prostate cancer and now this team-based approach is looking at targeting any metastatic cancer.”
This collaborative research project has received $23.7 million in federal funding through the New Frontiers Research Fund (NFRF) over six years.
“We will establish Canada as a world leader in the field of nuclear medicine and ensure Canadian patients are the ones who benefit,” adds Dr. Bénard. “By developing these medicines in Canada and bringing them into local clinical trials, we will ensure Canadians have access to innovative cancer treatments sooner.”
The team hopes to bring multiple drug candidates into clinical trials in the coming years with the ultimate goal of developing an effective treatment for metastatic cancer patients.
New study will assess fecal transplants in treatment of pancreatic cancer
Scientists examining microbiome to improve cancer therapies
MEDIA RELEASE
For Immediate Release
LONDON, ON- Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes.
“Pancreatic cancer is very hard to treat, partially because when it’s detected, the cancer is usually in a later stage and spreads very quickly,” explains Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s London Regional Cancer Program (LRCP) and Associate Scientist at Lawson. “Our best chemotherapy treatments for the average patient, will give them a little less than a year to live.”
With the goal of improving treatments for these patients the research team led by Dr. Saman Maleki, Scientist at Lawson, is studying whether changing the gut microbiome can result in better response to cancer treatments.
“We know that the microbiome plays an important role in patients’ response to various forms of systemic treatments such as immunotherapy and chemotherapy for different cancers,” says Dr. Maleki.
This unique study will happen in three stages. The first stage is an observational study to examine fecal samples of 52 patients at LRCP with advanced pancreatic cancer. The second stage will focus on using the samples from these patients in preclinical models to test new combinations of treatments. The final stage of the study will focus on intervention through human clinical trials by modifying a patient’s microbiome with something called a fecal transplant prior to treatment.
“The microbiome is involved in many aspects of cancer development and these organisms aren’t just living in the gut but also within the tumor,” says Dr. Michael Silverman, Lawson Scientist and Chair/Chief of Infectious Diseases at LHSC and St. Joseph’s Health Care London. “We believe that by giving people a fecal transplant, we can change the bacteria that live within the tumor and gut and then optimize the immune response to both the tumour and to treatment, with the goal of improving patient outcomes.”
Fecal transplants involve collecting stool from a healthy donor, preparing it in a lab and safely transplanting it to the patient, in this case with a capsule. The goal is to transplant the donor’s microbiome so that healthy bacteria will colonize in the patient’s gut.
“If you think of microbiome, each bacterium is like a little factory and all together they are a giant factory within us producing things we need,” explains Dr. Jeremy Burton, Lawson Scientist who specializes in human microbiome research. “Over time, a person’s diet, medications, and lifestyle can change the microbiome and it can have a big impact to the rest of our body.”
The research team was recently awarded a $450,000 Catalyst 2021 grant from the Weston Family Foundation to conduct this study, which is the first in the world focusing on prospectively modifying the microbiome in pancreatic cancer patients for treatments and outcomes.
“We normally don’t see this in one study where we go through the full spectrum of learning from patients, to looking at treatments, and then moving to a final intervention stage,” explains Dr. Maleki. “This has not been tried in pancreatic cancer before, but we think leveraging the microbiome and improving the immune response can potentially move the needle in this patient population.”
The team is recruiting both pancreatic cancer patients, as well as healthy volunteers for fecal transplant samples. Those interested in helping with fecal transplant donations can contact Dr. Seema Parvathy at 519-646-6100 ext. 61726 or email seemanair@@email
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca