Search
Search
Sharing the gift of hope through research
Community members and those in the field of health research attended a special open house and interactive tour by research groups at Lawson Health Research Institute – celebrating the holiday spirit and the gift of hope that is made possible through hospital-based research.
A part of St. Joseph’s Health Care London, Parkwood Institute represents the next era in care, recovery and rehabilitation. Across the site, clinical and research teams in different disciplines and specialties are collaborating in new ways.
The teams that make up Parkwood Institute Research, a Lawson program, are conducting clinical studies with the goal of understanding disease and improving care for a wide range of patients.
“Many people in the community know the high-quality and compassionate care that is supported by the various clinical teams at Parkwood Institute,” says Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery, and Assistant Scientific Director at Lawson. “What most don’t know is that we have research teams working across these sites, with each other and research patients.
Researchers tackle the most important challenges and provide access to highly innovative and meaningful solutions that improve the lives of patients and their families, added Dr. Forchuk.

At the open house on November 30, there were 11 interactive displays in the areas of cognitive vitality and brain health, mobility and activity and mental health. This included the Gait and Brain Laboratory, the Operational Stress Injury Clinic, wound care, the Mental Health Nursing Research Alliance and more:
- The Mental Health INcubator for Disruptive Solutions (MINDS) of London Middlesex is a social innovation lab focused on developing, testing, implementing and evaluating disruptive solutions that promote the mental and emotional wellbeing of Transition-Aged Youth in our London-Middlesex community.
- The Canadian Consortium on Neurodegeneration in Aging (CCNA), supported by CIHR and many partners, is the premier research hub for all aspects of research involving neurodegenerative diseases that affect cognition in aging – including Alzheimer's disease.
- A dynamic lab with the top neurorehabilitation evidence-based reviews in stroke, brain injury, spinal cord injury and multiple sclerosis, or insight into clinical trials of stroke rehabilitation using exoskeletons, exercise paradigms, pharmaceuticals, and clinical studies of psychosocial factors that influence chronic pain in brain injury and spinal cord injury populations.
The open house had a festive theme and each of the exhibits involved a problem solving element to encourage learning and foster teamwork.

Peggy Sattler, Member of Provincial Parliament for London West, and Terence Kernaghan, Member of Provincial Parliament for London North Centre, were among the over 300 people in attendance.
“This special open house opportunity is meant to be a fun experience where you were also learning about research,” explains Dr. Forchuk. “During this holiday season, we wanted to share our own gift of hope in the form of collaborative research that is making a real difference.”
See photos from the open house on Facebook.
Shocking number of heart attack patients suffer dangerous hemorrhage following heart attack
LONDON - A heart attack can be deadly, but there are effective lifesaving procedures if treated in time. The most common procedure is called reperfusion therapy, which is when the blocked coronary artery causing the heart attack is opened up and a stent is placed inside to let blood flow freely again.
In a recent published study by a multi-center research team at Lawson Health Research Institute, St. Joseph’s Health Care London and a number of other institutions across the globe, scientists examine a condition called reperfusion injury, a problem that can take place following reperfusion therapy.
“When you open up the coronary artery in someone experiencing a heart attack the blood starts to flow. However, we found there are a number of factors that lead to other injuries due to opening up the vessel,” explains Dr. Rohan Dharmakumar, Executive Director of the Krannert Cardiovascular Research Center at Indiana University. “Opening up the coronary artery, although lifesaving and necessary, can at times cause significant reperfusion injury which is a concept that had yet to be scientifically proven until now.”
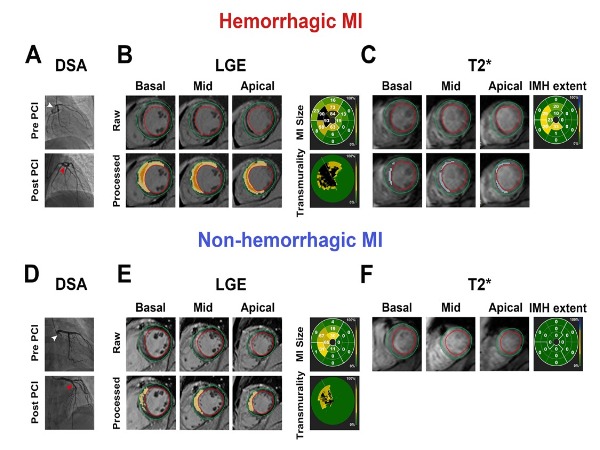
For example, when the blocked coronary artery is opened up with reperfusion therapy the blood flowing into narrower vessels can cause the smaller vessels to burst and cause internal bleeding within the heart muscle, which is called myocardial hemorrhage.
“Those who experience a myocardial hemorrhage have a much larger piece of their heart muscle die than those who don’t have hemorrhage,” says Dr. Frank Prato, Program Lead of Lawson’s Imaging Research Program and Assistant Scientific Director at Lawson. “We have been able to show that if there is hemorrhage due to reperfusion injury, the size of the dead tissue within the heart grows, which then can ultimately lead to heart failure.”
After studying 70 patients with heart attacks, the research team was able to show reperfusion injury led to hemorrhage in excess of 50 per cent of patients who were being treated for a heart attack.
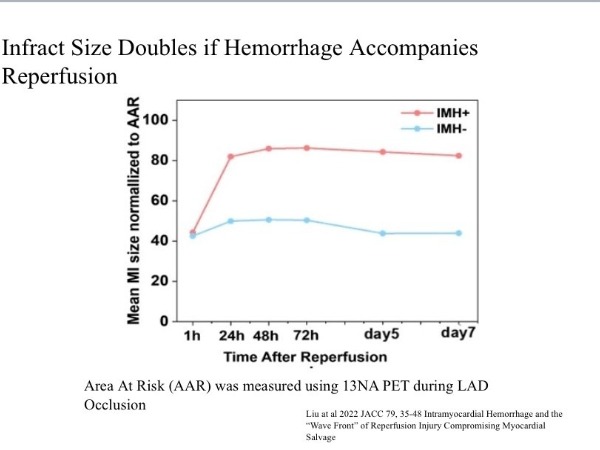
“The outcome isn’t immediate death, but heart failure that can start a few years after the heart attack,” says Dr. Dharmakumar. “So even though we are saving people initially from a heart attack, we are still losing a lot of people to heart failure within the first five years.”
This discovery was made possible through the use of Lawson’s cyclotron, a machine used to make isotopes for advanced PET/MRI scans at St. Joseph’s Health Care London.
“To validate the study with a PET/MRI we needed a specific radioactive isotope called nitrogen 13 ammonia,” explains Dr. Mike Kovacs, Scientist and Director of Lawson’s Cyclotron Facility. “We were able to create this isotope and went through Health Canada approval, so now we can use this not only in preclinical models but with human patients as well.”
The study has been published in the Journal of American College of Cardiology. The findings will now allow the research team to examine different forms of therapies that can be used in combination with reperfusion therapy to improve patient outcomes.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Shocking number of heart attack patients suffer dangerous hemorrhage following lifesaving treatment, study shows
MEDIA RELEASE
For immediate release
February 10th, 2022
LONDON- A heart attack can be deadly, but there are effective lifesaving procedures if treated in time. The most common procedure is called reperfusion therapy, which is when the blocked coronary artery causing the heart attack is opened up and a stent is placed inside to let blood flow freely again.
In a recent published study by a multi-center research team at Lawson Health Research Institute, St. Joseph’s Health Care London and a number of other institutions across the globe, scientists examine a condition called reperfusion injury, a problem that can take place following reperfusion therapy.
“When you open up the coronary artery in someone experiencing a heart attack the blood starts to flow. However, we found there are a number of factors that lead to other injuries due to opening up the vessel,” explains Dr. Rohan Dharmakumar, Executive Director of the Krannert Cardiovascular Research Center at Indiana University. “Opening up the coronary artery, although lifesaving and necessary, can at times cause significant reperfusion injury which is a concept that had yet to be scientifically proven until now.”
For example, when the blocked coronary artery is opened up with reperfusion therapy the blood flowing into narrower vessels can cause the smaller vessels to burst and cause internal bleeding within the heart muscle, which is called myocardial hemorrhage.
“Those who experience a myocardial hemorrhage have a much larger piece of their heart muscle die than those who don’t have hemorrhage,” says Dr. Frank Prato, Program Lead of Lawson’s Imaging Research Program and Assistant Scientific Director at Lawson. “We have been able to show that if there is hemorrhage due to reperfusion injury, the size of the dead tissue within the heart grows, which then can ultimately lead to heart failure.”
After studying 70 patients with heart attacks, the research team was able to show reperfusion injury led to hemorrhage in excess of 50 per cent of patients who were being treated for a heart attack.
“The outcome isn’t immediate death, but heart failure that can start a few years after the heart attack,” says Dr. Dharmakumar. “So even though we are saving people initially from a heart attack, we are still losing a lot of people to heart failure within the first five years.”
This discovery was made possible through the use of Lawson’s cyclotron, a machine used to make isotopes for advanced PET/MRI scans at St. Joseph’s Health Care London.
“To validate the study with a PET/MRI we needed a specific radioactive isotope called nitrogen 13 ammonia,” explains Dr. Mike Kovacs, Scientist and Director of Lawson’s Cyclotron Facility. “We were able to create this isotope and went through Health Canada approval, so now we can use this not only in preclinical models but with human patients as well.”
The study has been published in the Journal of American College of Cardiology. The findings will now allow the research team to examine different forms of therapies that can be used in combination with reperfusion therapy to improve patient outcomes.
-30-
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
For more information, please contact:
Celine Zadorsky
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C. 519-619-3872
@email
www.lawsonresearch.ca/news-events
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Showing the invisible: New research to help us see bacteria in the body
In recent years, research has increasingly shown us the importance of bacteria and other microbes in the human microbiome for maintaining health. Now, researchers at Lawson Health Research Institute are pioneering new imaging methods to see these microbes in the human body and open new avenues for health research. Early results of preclinical studies at Lawson have found positron emission tomography-magnetic resonance (PET/MR) imaging could allow the tracking and identification of bacteria inside the body and lead to more targeted use of antibiotic treatments.
Accurate targeting of antibiotic treatments can prevent antimicrobial resistance – when bacteria, viruses, fungi and parasites no longer respond to medication. According to a United Nations report, it is estimated that by 2050, antimicrobial resistance could result in 10 million deaths each year – more than cancer. New imaging research could be a gamechanger for treating bacterial infections by allowing us to see bacteria in the body using medical imaging equipment and then targeting the bacteria with specific therapies.
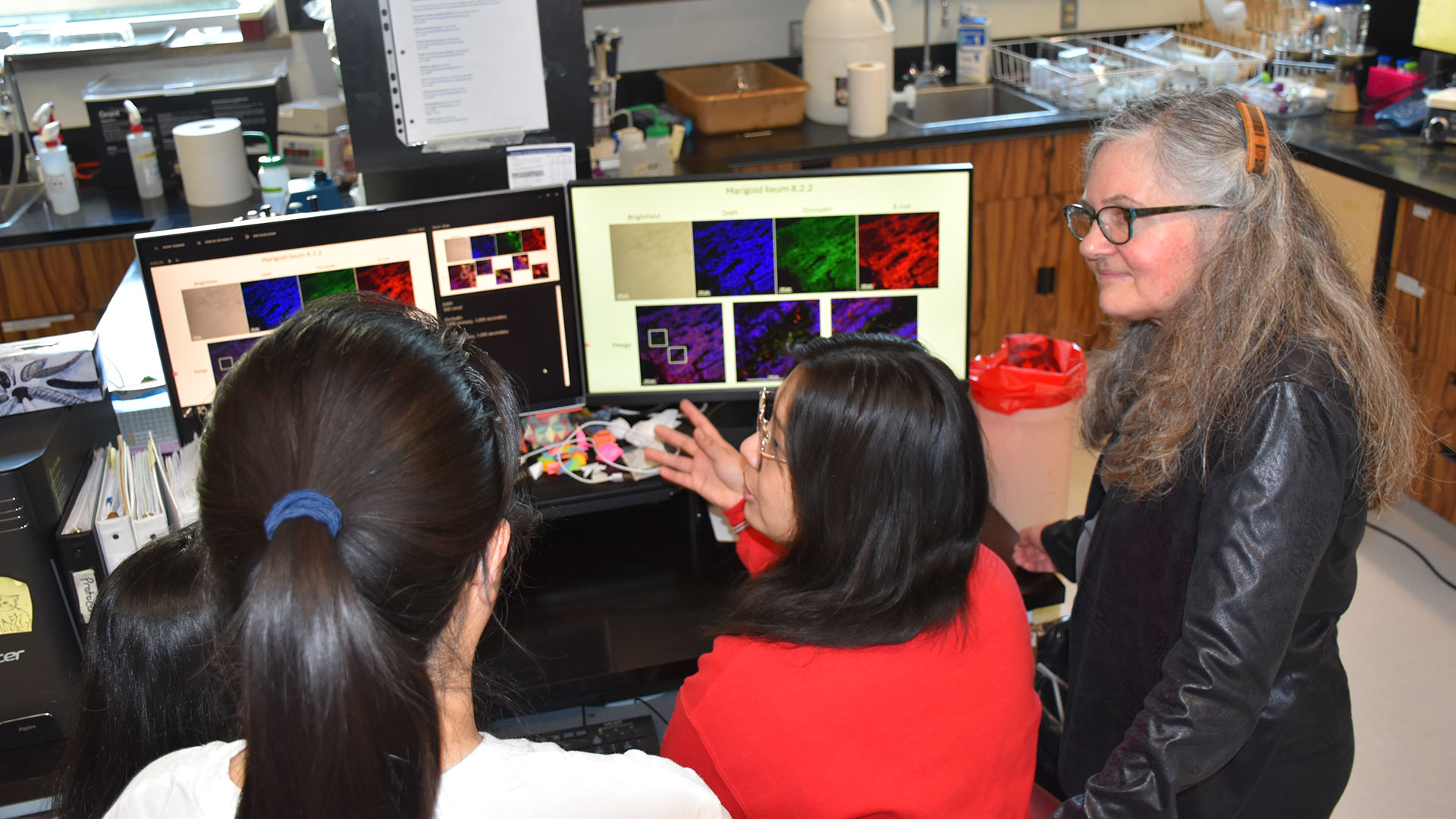
“Traditional imaging of infection means that you're looking at tissue damage; the bacteria have already started the process of inflammation and are wreaking havoc,” explains Dr. Donna Goldhawk, Lawson Scientist at St. Joseph’s Health Care London (St. Joseph’s). “Imaging bacteria catches the infection at an earlier stage. When you can image a particular species of bacteria, you can narrow the type of antibiotic that you might want to treat it with – reducing the need for broad-spectrum antibiotics that can lead to antimicrobial resistance.”
Imaging bacteria using PET/MR technology begins with attaching tracer molecules – also called isotopes – to specific bacteria in order to follow the movement of the microbes. A recent study from Lawson used PET/MR imaging to track bacteria labelled with an isotope called Zirconium-89 (89Zr) in a preclinical model. The researchers were able to demonstrate that PET/MR imaging could track ingested bacteria through the gut.
“Imaging of bacteria is a very new application of how PET/MR technology can be used. Using isotopes like 89Zr to label bacteria would allow you to image the same individual repeatedly and follow the ingestion of specific bacteria from the stomach through the digestive system since those isotopes last a long time,” adds Dr. Frank Prato, Scientist at Lawson and Lead of the Lawson Imaging research program.

This also has the potential to allow imaging of bacteria that migrate to other areas of the body like the brain, bladder, kidneys, and reproductive system. In the future, this technology could allow researchers to identify specific bacteria present and target those bacteria.
Similar research is underway to examine whether bacteria without tracers can also be tracked using MR imaging based on differences in their characteristics, like associations with specific metals. This could allow imaging of specific bacteria in the gut and how they respond when gut infections are treated with antibiotics, probiotics or microbial therapies like fecal microbiota transplantation (FMT).
With or without tracer molecules, both imaging methods could eventually become important for improving the efficacy and wider implementation of FMT, which introduces healthy microbes from donors into a patient’s gut with the goal of having the healthy bacteria reinstate a balanced microbiome. FMT is currently used to treat recurrent infections of C. diff. (Clostridium difficile), but new applications are expanding with clinical trials looking at its use to treat a variety of diseases, including certain forms of cancer. The ability to see how the balance of bacteria is changing could accelerate the development of effective new therapies.
While more research is needed, these studies are moving the monitoring of bacteria using PET/MR imaging closer to clinical implementation. The research has been made possible in part thanks to collaborations with Siemens Healthineers, Cubresa Inc. and London X-Ray Associates.
Simple CT scanning procedure can predict effectiveness of ovarian cancer treatment
Technology developed at Western University and Lawson Health Research Institute can provide a new window into whether or not patients are responding to treatment for advanced ovarian cancer. A multi-centre clinical trial has demonstrated that CT Perfusion, which measures blood flow and blood volume to tumours associated with ovarian cancer, can provide an accurate prediction of how well a treatment is working, allowing physicians the opportunity to better plan treatment. Funding for the trial was provided by the US National Cancer Institute through the National Clinical Trials Network including NRG Oncology and ECOG-ACRIN.
“CT perfusion is homing into the change in blood flow to the tumour before and after treatment,” said Ting-Yim Lee, professor at Western University’s Schulich School of Medicine & Dentistry, scientist at Lawson Health Research Institute, and a Medical Physicist at St. Joseph’s Health Care London. “In this particular case we can see that blood flow tends to decrease in those who will survive longer without symptoms, whereas for those whose symptoms will recur within six months, we saw blood flow to the tumour increase after their treatment.”
The study was published in the journal, Clinical Cancer Research. Its authors point out that in 60 to 85 per cent of ovarian cancer patients, relapse will occur after initial treatment. By using CT perfusion to identify which patients are more likely to benefit from a specific therapy enables better patient selection and treatment planning, and also provides a biomarker for future clinical trials assessing new treatment options. The authors also point out that although the trial is promising, further studies are required to corroborate the current findings.
“Using this method we are able to see a change in the blood flow as early as four weeks after treatment. This means we don’t have to wait months to determine whether symptoms will recur, we are able to tell whether the treatment is effective much sooner,” said Lee.
Developed by Lee and his team at Western University’s Robarts Research Institute, CT perfusion uses X-ray dye in combination with existing CT scanners to measure blood flow. The technology is already used globally to assess blood flow to the brain after stroke. This clinical trial for use in ovarian cancer took place across 19 U.S. centres, and also demonstrated that the technology is easily implemented onto any existing CT scanner, and requires minimal training to be successful.
Simple device improves care after kidney transplantation
LONDON, ON – In a published study, a team from Lawson Health Research Institute has found that a simple device can reduce swelling after kidney transplantation. The geko™ device, manufactured by Sky Medical Technology Ltd and distributed in Canada by Trudell Healthcare Solutions Inc., is a muscle pump activator which significantly improves blood flow by stimulating the body’s ‘muscle pumps.’ Patients using the device following kidney transplantation experienced shorter hospital stays and reduced surgical site infections by nearly 60 per cent.
Kidney and simultaneous pancreas-kidney transplantations can significantly reduce mortality and improve the quality of life for patients with end stage renal disease. “After surgery, many of these organ recipients require a longer hospital stay due to delayed kidney function, infection, lack of mobility or edema,” says Dr. Alp Sener, Lawson Scientist and Transplant Surgeon in the Multi-Organ Transplant Program at London Health Sciences Centre (LHSC).
Edema is swelling caused by excess fluid trapped in the body’s tissues which can impact wound healing. The current standard of care for managing lower-limb edema and improving blood flow is thrombo-embolic-deterrent (“TED”) stockings used with compression devices. Sleeves pumped with air squeeze the lower legs to boost circulation. They can be uncomfortable to wear, and the large pump can inhibit early mobility and disrupt sleep after surgery.
In a randomized controlled clinical trial spanning two years, 221 transplant recipients at LHSC either wore the standard TED stocking and pump or the geko™ device for six days after surgery. Dr. Sener’s research team found that wearing the device increased urine output by 27 per cent and lowered weight gain by over a kilogram. With more urine produced and less fluid retention, patients experienced 31 per cent less swelling. The duration of costly hospitalization was shortened by over one day after kidney transplantation compared to the standard of care.
A 60 per cent reduction in wound infection rates was a striking observation. “Transplant patients are at a higher risk of infection due to the immunosuppressant medications needed after surgery,” explains Dr. Sener, who is also the President of the Urologic Society for Transplantation and Renal Surgery, a global organization affiliated with the American Urological Association. “Reducing infection means a much better outcome for the patient and considering that recent data shows wound infections can cost the health care system thousands of dollars per person, it’s a win-win situation.”
Some of the study participants wore pedometers to track their steps, and those using the geko™ device had improved mobility after surgery. The team suspects this may be due to reduced swelling which could improve ease and comfort when moving.
“The study results have been both surprising and exciting. Not only have we cut down wound infection rates but we have also seen a considerable improvement in the new organ’s function following transplantation. Patients report feeling more satisfied with the transplant process and are more mobile,” says Dr. Sener. The geko™ device is now being offered to patients at LHSC in recovery after receiving a new kidney.
Ruben Garcia, 68 years old, recently received a new kidney from his daughter, Ruby, who was a match as a living kidney donor. Following his surgery, Garcia found it difficult to get out of bed due to the pain and swelling, and the function of his new kidney was very low. “My surgeon explained in very simple terms that it was as if my new kidney wasn’t awake yet,” describes Garcia.
Dr. Sener recommended that Garcia use the geko™ device to help stimulate blood flow in a way that is similar to walking. Garcia was soon able to sit up on a chair and by the next day he was walking. “My kidney woke up and starting working again! I could feel the device working and it was comfortable to wear, almost like a massage for my legs. I’m very grateful for the care that I received.”
Dr. Sener adds that “using a muscle pump activator could be a game changer for other procedures like orthopedic implants where wound infection can have disastrous consequences or in surgeries where wound infections are more common such as in cancer and intestinal surgery.”
The geko™ device is non-invasive, self-adhering, battery-powered and recyclable. It generates neuromuscular electro-stimulation and unparalleled systemic blood flow that equates to 60 per cent of that achieved by walking. Pain-free muscle contraction compresses deep veins in the lower legs to create better blood flow in these vessels and return blood to the heart. It is particularly well suited to hospital settings as it portable and requires minimal training. For the indications for the use of the geko™ device, go to www.gekodevices.com.
“The results of the study provide further evidence that the geko™ device is an effective treatment option that can improve outcomes for patients and help them return home sooner, while reducing costs for the health-care system,” says George Baran, Executive Chairman of the Trudell Medical Group and a Director of Sky Medical.
-30-
DOWNLOADABLE MEDIA

Dr. Alp Sener, Lawson Scientist and Transplant Surgeon in the Multi-Organ Transplant Program at London Health Sciences Centre

The geko™ device being applied on the leg

The geko™ device
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca