Search
Search
Diagnosing COVID-19 using artificial intelligence
LONDON, ON – A team of researchers at Lawson Health Research Institute is investigating whether an artificial neural network could be used to diagnose COVID-19. The AI system is being trained to learn and recognize patterns in ultrasound lung scans of patients with confirmed COVID-19 at London Health Sciences Centre (LHSC) by comparing them to ultrasound scans of patients with other types of lung infections.
“Machines are able to find patterns that humans cannot see or even imagine. Lung ultrasound scans of patients with COVID-19 pneumonia produce a highly abnormal imaging pattern. This pattern isn’t unique to COVID-19, and can be seen in other causes of pneumonia. It is plausible, however, that there are details that distinguish COVID-19 at the pixel level that cannot be perceived by the human eye,” explains Dr. Robert Arntfield, Lawson Researcher and Medical Director of the Critical Care Trauma Centre at LHSC. “If we can train a neural network to learn and identify these unique characteristics among different scans, we can apply this AI to enhance the diagnostic power of portable ultrasound.”
Point-of-care ultrasound has become increasingly important for the care of critically ill patients and LHSC is a global leader in the use of this technology at the bedside. Lung ultrasound has proven to be effective in diagnosing different types of lung infections and illnesses, such as pneumonia, with a high degree of accuracy. The convenience, portability and low cost of using these machines has helped them become a standard bedside tool in emergency departments and intensive care units worldwide.
This research project is part of a grassroots effort by a small group of local clinicians to innovate and create technology to solve sophisticated problems with AI. With many of Dr. Arntfield’s team having a background in computer programming, they were able to code the neural network being tested. Minimal funding was required, with the project being driven largely by the urgency of COVID-19 coinciding with the recent creation of this clinical AI working group.
“Our research team has used AI to help improve diagnostics related to other parts of the body. This project is a great example of the unique ability we have here in London to be agile: that is, to identify a gap and move quickly towards finding a solution,” says Dr. Arntfield. “I am thrilled that we were able to move through the approval process quickly, and get our ideas working in such a short amount of time.”
-30-
Downloadable Media

Dr. Robert Arntfield

COVID-19 pneumonia ultrasound
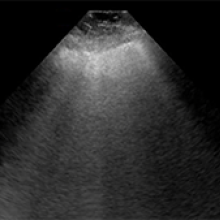
NON COVID-19 pneumonia ultrasound
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
DocTalks - Combating Food Allergies Using the Body’s Immune System

Combating Food Allergies Using the Body’s Immune System
Where: Shuttleworth Auditorium (Cheapside entrance)
Dr. Harold Kim is the Medical Director of St. Joseph’s Allergy and Immunology Program. He will explain how certain food allergies can gradually be reduced or eliminated through the process of immunotherapy.
Registration opens Open 11.
DocTalks is a series of community health discussions featuring leading physicians and researchers at St. Joseph’s Health Care London. Learn from the experts how St. Joseph’s is tackling the pressing health issues of our time and why it matters to you and your family.
DocTalks is a joint initiative presented by St. Joseph’s Health Care London and St. Joseph’s Health Care Foundation.
DocTalks - Recovery After Stroke: Retraining the Injured Brain Through Rehabilitation

Recovery After Stroke: Retraining the Injured Brain Through Rehabilitation
Where: Shuttleworth Auditorium (Cheapside entrance)
Dr. Robert Teasell is the Medical Director of St. Joseph’s Stroke Rehabilitation Program, Professor of Physical Medicine and Rehabilitation at Western University and a clinical scientist at Lawson Health Research Institute. He will discuss various rehabilitation therapies and technologies that can help an individual recover after a stroke.
Registration opens April 16.
DocTalks is a series of community health discussions featuring leading physicians and researchers at St. Joseph’s Health Care London. Learn from the experts how St. Joseph’s is tackling the pressing health issues of our time and why it matters to you and your family.
DocTalks is a joint initiative presented by St. Joseph’s Health Care London and St. Joseph’s Health Care Foundation.
Dr. Lisa Hoffman

PhD
I have capitalized on the breadth of research being conducted in the fields of stem cell research and imaging within this center, and now possesses an extremely unique skill-set in stem cell biology, classic cell/molecular biology, and multi-modality non-invasive imaging technologies (positron emission tomography [PET], dynamic contrast-enhanced computed tomography [DCE-CT], high frequency 3D ultrasound [HFU], and optical [bioluminescence]). Excitingly, I am currently one of few Canadian researchers poised to take full advantage of the recent opening of the PETtracer Cyclotron and PET-radiochemistry facility in London.
My future research goal is to develop a collaborative research program in Molecular and Functional Imaging, in which I will play a lead role in cutting-edge research that focuses on the development of therapeutics for neuromuscular diseases, and on the non-invasive assessment of such therapies.
Dr. Hoffman obtained her Ph.D. from the University of Saskatchewan in 2000. She went on to complete several postdoctoral positions that culminated in a unique skill set in stem cell biology, classic cell/molecular biology, and non-invasive multi-modality imaging.
Imaging modalities include positron emission tomography [PET], dynamic contrast-enhanced computed tomography [DCE-CT], high frequency 3D ultrasound [HFU]/echocardiography, and optical/bioluminescense imaging. She is currently one of few Canadian researchers poised to take advantage of the recent opening of the PETtracer Cyclotron and PET-radiochemistry facility in London.
Dr. Hoffman was appointed as a Lawson Imaging Scientist in the Fall of 2009, and as Assistant Professor in the Departments of Medical Biophysics, Western University (Fall 2009) and Anatomy & Cell Biology, Western University (Spring 2010). Capitalizing on the breadth of her multidisciplinary experience, Dr. Hoffman's current research interests lie in Molecular Imaging and Cell Therapeutics for the treatment of both the skeletal and cardiac manifestations of Duchenne muscular dystrophy (DMD). Specifically, her group aims to develop objective and quantitative non-invasive imaging technologies to track stem/progenitor cell fate following transplantation into mouse models of DMD.
Dr. Anurag Bhalla
BHSc (Honours), McMaster University
MD, Western University
FRCPC Internal Medicine and Respirology
MSc, Physiology and Phamacology, McMaster University
Contact Information
Asthma, sputum cell counts, eosinophils.
Anurag Bhalla is an Assisstant Professor of Medicine in Department of Medicine, Division of Respirology at Western University and Staff Respirologist at St. Joseph's Healthcare and London Health Sciences Centre.
He completed his medical school and internal medicine residency at Western University followed by respirology residency at McMaster University. Subsequently, he completed airway disease clinical fellowship and MSc in physiology and pharmacology with Dr. Parameswaran Nair at McMaster University.
His clinical interest includes complex airway diseases, including asthma, COPD and bronchiectasis. His research interest includes severe asthma, eosinophil biology, asthma biologics and airway inflammometery.
Dr. Cheryl Forchuk recognized for health care innovation
Dr. Cheryl Forchuk is the recipient of the 2020 Innovation Award for her work to prevent discharges from hospital to homelessness. Throughout her career, Dr. Forchuk has been investigating potential best practice approaches to prevent homelessness in our community for a wide range of people, including those with severe mental illness, veterans, families, and youth.
Her recent project, ‘Preventing Hospital Discharge into Homelessness: No Fixed Address Version 2 (NFAv2)’ streamlines housing and income services by bringing them into the hospital, and integrating them into a coordinated system of care.
Research shows that when someone is housed, their use of medical and social services decreases. Safe and adequate housing is required for individuals to recover from illness.
Version one of this program was a great success, providing direct access to a housing advocate and Ontario Works from inpatient hospital psychiatric units in London. The No Fixed Address v2 program provides individual inpatients, at risk of becoming homeless, with housing and financial assistance while in hospital. A collaborative approach which includes the local Canadian Mental Health Association, the Salvation Army Rent Stability Bank, Ontario Works, and the City of London brings community supports to the hospital. This enables patients to recover from their illness and reduces the number who may return to the hospital. Dr. Forchuk’s use of in-depth, individual, quantitative interviews, and qualitative focus groups, allows stakeholders to voice their experiences with the program as well as capture traditional outcomes.
“This innovative program has been so successful in London’s hospitals that the City of London has integrated the NFAv2 service within its municipal housing support programs,” explains Dr. Arlene MacDougall, Lawson Scientist and Dr. Forchuk’s nominator. “It also has the potential to be integrated across the province as the best practice in reducing homelessness in communities. Her efforts have been recognized by multiple funding agencies, and it will soon be the model for the rest of the nation to follow. Dr. Forchuk’s commitment to improve the lives and of those in our community makes her truly deserving of this award.”
“The No Fixed Address research project is the first evaluation anywhere of a strategy that aims to reduce the number of hospital patients being discharged into homelessness,” says Dr. Forchuk. “I’m really proud of our collective efforts. We have been able to help a lot of people, and have also learned a lot throughout the course of this study.”