Search
Search
Study to examine health impacts of the COVID-19 pandemic for mothers and their new babies
LONDON, ON - The COVID-19 pandemic has drastically altered many people’s lifestyles. Parents may be working from home, providing additional childcare or experiencing social isolation. Some are dealing with decreased work hours and loss of employment. With all these factors at hand, a team of researchers from Lawson Health Research Institute and Western University are investigating the possible health impacts on mothers and their babies who were born or will be born during the pandemic.
“This has been a stressful and pivotal time for everyone in the world, but we know the post-partum experience can greatly affect both the birthing person and their baby, in the short and long term,” says Dr. Genevieve Eastabrook, Associate Scientist at Lawson and Assistant Professor at Western’s Schulich School of Medicine & Dentistry. “We know perceived stress in the perinatal period may have a contribution to health later in life for the birthing person and their children in terms of overall cardiovascular and metabolic health, bonding experiences, and risk of mood disorders.” Dr. Eastabrook is also an obstetrician-gynecologist (OB-GYN) at London Health Sciences Centre (LHSC).
As part of the new study, the London research team is using an approach called ‘One Health’ which offers a holistic perspective to explore how various risk factors and social determinants of health interact to affect health. This is being studied through the Department of Pathology and Laboratory Medicine at Western. “It’s important for us to think of the environment as all of our surroundings, including the things around us like health care, grocery stores, education and employment,” says Mei Yuan, MSc research student at Schulich Medicine & Dentistry. “The purpose of this study is to look at the pandemic response rather than the pandemic itself. We know that even if women haven’t been infected with COVID-19, it doesn’t mean they haven’t been impacted.”
Study participants are asked to complete a 30-minute questionnaire at around 6-12 weeks after their delivery. The questionnaire focuses on perceived stress, postpartum depressive symptoms, perceived social support, the impact of COVID-19, health-care access and breastfeeding. Data from the questionnaire will be linked with participants’ medical records to look for associations between the various factors and pregnancy outcomes. “Even though the study is mainly focused on maternal health, studies have shown that once mental health is affected it really does impact the infant’s health, especially in the area of attachment between baby and caregivers,” explains Yuan.
Data from the study will be compared to the Maternity Experiences Survey, a national survey of Canadian women compiled in 2007 which looked at experience, perception, knowledge and practice during pregnancy, birth and the early months of parenthood. “The unique aspect here is that we have a comparative group using a historic cohort to see whether or not there are differences in markers that increase risk of depression, perceived stress and lack of social support,” adds Dr. Eastabrook. “We will also look at some unique things from the pandemic, such as how the use of virtual care for antenatal, postpartum and baby care impacted people’s experiences.”
The research team hopes to recruit 300 mothers for this study who have given birth at LHSC, specifically during the pandemic. Interested participants can email the Pregnancy Research Group at @email. Once all the data is collected the goal will be to use the findings to improve post-partum care for mothers and their babies within this population group.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study validates methods for tracking prevalence and service use of people who experience homelessness
A new population-based retrospective validation study, using ICES data collected between 2007 and 2014 in Ontario, has found that health records can be used to track service use as well as the needs of individuals experiencing homelessness. Researchers found that the algorithms tested were able to accurately identify up to 35 per cent of individuals who experience homelessness in a given year.
The best performing algorithm estimated a large increase in homelessness prevalence between 2007 and 2016, with approximately one in 200 adults in Ontario experiencing homelessness in 2016.
“We do not know how many people experience homelessness yearly in Ontario, or in the country as a whole. Current methods rely on shelter data, or large point-in-time counts that require large investments, and are only done in specific communities,” explains Lucie Richard, Lawson researcher and lead author of the study. “Also, not all people who are homeless use shelters. This approach gives us an alternative that can include a wide range of communities and different types of homelessness over time.”
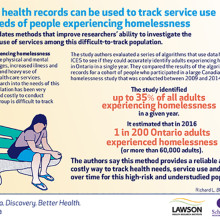
While numerous computer algorithms are already used to analyze administrative databases and identify disease populations to measure the burden of chronic diseases in Canada, this study, conducted by researchers at Lawson Health Research Institute and Western University, is one of the first to validate and track a social determinant of health with good accuracy.
People who experience homelessness often face mental and physical health challenges, have an increased risk of illness and death, and are among the highest users of emergency and other health care services. Homelessness is an important health issue for Canadians.
This ability to track individuals experiencing homelessness over time using administrative databases provides inexpensive, long-term monitoring, which will inform efforts to improve housing and health status in the community and across the country. Researchers and health care providers can now track health status and health care usage of individuals experiencing homelessness.
Understanding how many people experience homelessness and what demographics correlate with homelessness will allow for better service planning, and providers will have the information needed to more appropriately meet the needs of this vulnerable population.
The study, “Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada” is published in BMJ Open.
Study validates methods for tracking prevalence and service use of people who experience homelessness
LONDON, ON – A new population-based retrospective validation study, using ICES data collected between 2007 and 2014 in Ontario, has found that health records can be used to track service use as well as the needs of individuals experiencing homelessness. Researchers found that the algorithms tested were able to accurately identify up to 35 per cent of individuals who experience homelessness in a given year.
The best performing algorithm estimated a large increase in homelessness prevalence between 2007 and 2016, with approximately one in 200 adults in Ontario experiencing homelessness in 2016.
“We do not know how many people experience homelessness yearly in Ontario, or in the country as a whole. Current methods rely on shelter data, or large point-in-time counts that require large investments, and are only done in specific communities,” explains Lucie Richard, Lawson researcher and lead author of the study. “Also, not all people who are homeless use shelters. This approach gives us an alternative that can include a wide range of communities and different types of homelessness over time.”
While numerous computer algorithms are already used to analyze administrative databases and identify disease populations to measure the burden of chronic diseases in Canada, this study, conducted by researchers at Lawson Health Research Institute and Western University, is one of the first to validate and track a social determinant of health with good accuracy.
People who experience homelessness often face mental and physical health challenges, have an increased risk of illness and death, and are among the highest users of emergency and other health care services. Homelessness is an important health issue for Canadians.
This ability to track individuals experiencing homelessness over time using administrative databases provides inexpensive, long-term monitoring, which will inform efforts to improve housing and health status in the community and across the country. Researchers and health care providers can now track health status and health care usage of individuals experiencing homelessness.
Understanding how many people experience homelessness and what demographics correlate with homelessness will allow for better service planning, and providers will have the information needed to more appropriately meet the needs of this vulnerable population.
The study, “Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada” is published in BMJ Open.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western University’s Faculty of Health Sciences (FHS) is committed to bettering the human condition through outstanding training of health professionals, the education of students in the fundamentals of health, disability, and sport, and through the actions of our graduates who integrate the art and science of their disciplines.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Supporting a rapid research response during the pandemic
LONDON, ON – Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Supporting a rapid research response during the pandemic
Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
Congratulations to all of the researchers and their teams who have been awarded funding:
- Dr. Ian Ball - Predictors of clinical deterioration in hospitalized patients with COVID-19: The CORAL study
- Dr. Doug Fraser - Translational Research Centre: Repository of biological specimens from patients
- Dr. Sean Gill - Rapid identification of therapeutic targets mediating pulmonary microvascular endothelial cell dysfunction in COVID-19 patients
- Dr. Marnin Heisel - Testing Online Meaning-Centered Men’s Groups to Promote Psychological Well-Being and Reduce Despair in the Face of the COVID-19 Pandemic
- Dr. Kimia Honarmand - The impact of the COVID-19 pandemic on frontline healthcare workers: A Southwest Ontario survey
- Dr. Michael Knauer - Improving diagnostic and epidemiologic detection of SARS-CoV-2
- Dr. Jim Koropatnick - Targeting the SARS-CoV-2 receptor with candidate antisense drugs to prevent infection and disease progression
- Dr. Eldon Loh - COVID-19 and Disability: The Impact of a Societal Lockdown on those with Spinal Cord and Brain Injuries
- Dr. Len Luyt - Stapled Peptides as SARS-CoV-2 Fusion Inhibitors
- Dr. Claudio Martin - COVIDOPATHY – An observational study of coagulation abnormalities in patients with COVID-19
- Dr. Tianqing Peng - Developing new ssDNA aptamers targeting S protein receptor binding domain of SARS-CoV-2 to disrupt virus infection cycle as a potential therapy
- Dr. Eva Turley - Hyaluronan signaling through the inflammasome is a target for blunting acute respiratory distress syndrome (ARDS) in COVID-19 patients
- Dr. Ruud Veldhuizen - Next generation exogenous surfactants for COVID-19 and future respiratory pandemics
- Dr. Blayne Welk - Characterizing the burden of surgical care in COVID-19 positive patients
The invisible world inside us
The human microbiome is a wonder of nature.
Trillions of microbes call our body home. They live in our gut and many other places throughout our body. They are involved in virtually every aspect of how we function and we are learning that they are essential to staying healthy. An unhealthy microbiome has been linked to many diseases from allergies to cancer and even mental health.
Most people out there have heard about probiotics and fermented foods, and chances are you’re trying to get more of them in your diet.
Drinking kombucha or eating yogurt, anyone?
Join Lawson Health Research Institute for our next Café Scientifique event, "The invisible world inside us: Exploring the human microbiome."
Hear from a panel of researchers who are unraveling the mysteries about the microbiome and using that knowledge to improve health and health care. They will also bust some myths and share the important facts when it comes to probiotics, prebiotics and the microbiome.
Image

SPEAKERS
- Dr. Gregor Reid, Lawson Scientist and Professor of Microbiology & Immunology and Surgery at Western University.
Presenting: Probiotics and Prebiotics - Look beyond the fake news - Dr. Michael Silverman, Lawson Associate Scientist, Chair of Infectious Diseases, Schulich School of Medicine & Dentistry at Western University and Chief of Infectious Diseases for St. Joseph’s Health Care London and London Health Sciences Centre.
Presenting: Fecal Transplants: What does this crap have to do with me? - Dr. Jeremy Burton, Lawson Scientist and Assistant Professor of Surgery (Urology) and Microbiology & Immunology at Western University.
EVENT DETAILS
Date: Wednesday, November 27, 2019
Time: 7-9 pm (doors open at 6:30 pm)
Location: Best Western Plus Lamplighter Inn & Conference Centre (Regency Room), 591 Wellington Rd, London, ON N6C 4R3
Map and directions.
Parking: Free on-site parking
This is a free event and online registration is REQUIRED.
Registration for this evengt is now FULL.
Please fill out the form here to be added to the waitlist.
You will be notified should a spot open up.
Therapeutic seizure for depression: The positive and not so positive effects
You are invited to the second in a series of Research Bites. These informative and interactive talks focus on specific illnesses, their prevention and related research being conducted by researchers in London, Ontario.
Topic: Therapeutic seizure for depression: The positive and not so positive effects

The talk will include an overview of convulsive therapy, the benefits and risks, and new research to overcome some of the cognitive side effect of the treatment. It will also include a dialogue between Dr. Burhan and a family that went through the experience of electroconvulsive therapy to elicit the experience from the consumer perspective.
Date: Thursday, June 6, 2019
Time: 4 - 5 pm
Location: Parkwood Institute, Mental Health Building, Auditorium (F2-235)
550 Wellington Road South
London, Ontario N6C 0A7
Maps and Directions for Parkwood Institute.
Parking: The lot rate is $4.00 when you enter. $1 and $2 coins and credit card accepted (press the start button then insert payment)
Registration is required and spots will fill up quickly.
Click here to register.
These talks are hosted by Parkwood Institute Research, a program of Lawson Health Research Institute.