Search
Search
Cafe Scientifique
Approximately nine per cent of Canadian adults will experience post-traumatic stress disorder (PTSD) at some point in their lifetime (Canadian Mental Health Association). As trauma and trauma-related disorders have become more recognized in society, the need for research has accelerated. At London Health Sciences Centre and St. Joseph’s Health Care London, our researchers are leading the way in advancing understanding, diagnosis and treatment in this critical area of mental health.
Join Lawson Health Research Institute on Thursday, September 28th at Goodwill Industries for a special Café Scientifique event, “Uncovering Trauma: A Conversation about PTSD and Moral Injury.”
Our world-renowned researchers and those with lived experience will share the importance of addressing trauma, PTSD and moral injury. They will discuss diagnosis, prognosis and treatment advancements developed through studies involving at-risk populations, including Canadian Veterans, health-care workers and those with developmental trauma.
EVENT DETAILS
- Date: Thursday, September 28, 2023
- Time: 6:30-9:00 p.m. (Doors open at 6:00 pm)
- Location: Goodwill Industries
- 255 Horton Street, London, ON (3rd floor event space)
https://goo.gl/maps/J65qJy6HKtg4aDxEA - Parking: Free on-site parking
PANELISTS
- Dr. J. Don Richardson, Associate Scientist at Lawson, Consultant Psychiatrist and Medical Director of the Parkwood Operational Stress Injury (OSI) Clinic at St. Joseph’s Health Care London, Scientific Director of the MacDonald Franklin OSI Research Centre at the Parkwood Institute, Fellow with the Canadian Institute for Military and Veteran Health, Tanna Schulich Chair in Neuroscience & Mental Health and Professor of Psychiatry at Western University
- Dr. Ruth Lanius, Associate Scientist at Lawson, Psychiatrist at London Health Sciences Centre, Harris-Woodman Chair in Mind-Body Medicine and Professor of Psychiatry at Western University’s Schulich School of Medicine & Dentistry
- Teresa Kinney, research participant who has contributed to studies with Dr. Lanius
- Laryssa Lamrock, National Strategic Advisor for families at Atlas Institute for Veterans and Families, Veterans Family Advisor on the MacDonald Franklin OSI Research Centre Advisory Council
MODERATOR
- Dr. Arlene MacDougall, Scientist at Lawson, Director of Research and Innovation for Mental Health at St. Joseph’s Health Care London, Director for MINDS, the Mental Health Incubator for Disruptive Solutions of London-Middlesex, Assistant Professor of Psychiatry and Epidemiology & Biostatistics at Western University
This is a free event and online registration is REQUIRED. Click here to register.
Café Scientifique is a free community event providing an informal opportunity to get involved with science. Through an open-forum discussion in a casual setting, these events address health-related issues of popular interest to the general public. A panel of Lawson researchers talk about what they do and why, and share their unique research perspectives. Guests can then ask questions, participate in discussion, and gain insights from the speakers and from one another.
This event is made possible by funding from the Canadian Institutes of Health Research (CIHR).
Thanks to our media partner:

Café Scientifique: The invisible world inside us
The human microbiome is a wonder of nature, with trillions of microbes calling our body home. They live in our gut and many other places throughout our body. They are involved in virtually every aspect of how we function and we are learning that they are essential to staying healthy. An unhealthy microbiome has been linked to many diseases from allergies to cancer and even mental health.
Most people out there have heard about probiotics and fermented foods, and chances are you’re trying to get more of them in your diet. Drinking kombucha or eating yogurt, anyone?
On November 27, 2019, Lawson Health Research Institute held the latest in its Café Scientifique event series, "The invisible world inside us: Exploring the human microbiome.”
The panel of researchers helped to unravel the mysteries about the micirobiome and how we are using that knowledge to improve health and health care. They also busted some myths and shared the important facts when it comes to probiotics, prebiotics and the microbiome.
Watch their talks:
Researchers:
Probiotics and Prebiotics - Look beyond the fake news
Dr. Gregor Reid, Lawson Scientist and Professor of Microbiology & Immunology and Surgery at Western University.
Time stamp: 10:02
Fecal Transplants: What does this crap have to do with me?
Dr. Michael Silverman, Lawson Associate Scientist, Chair of Infectious Diseases, Schulich School of Medicine & Dentistry at Western University and Chief of Infectious Diseases for St. Joseph’s Health Care London and London Health Sciences Centre.
Time stamp: 31:48
Does eating bacteria make sense?
Dr. Jeremy Burton, Lawson Scientist and Assistant Professor of Surgery (Urology) and Microbiology & Immunology at Western University.
Time stamp: 55:02
See the event photos on Facebook.
CAISA Fashion Show – COMME des GARCONS
The Canadian Asian International Students’ Association (CAISA) is delighted to present its 19th annual fashion show – COMME des GARCONS, on Saturday, March 18, 2017 at Centennial Hall.
Drawing a crowd of over 1,500 attendees, CAISA Fashion Show is one of the largest student-run charity fashion shows in Ontario. COMME des GARCONS will be pushing creative boundaries with a number of unique acts, on-stage illusions in the ‘House of Magic’, and a roster of independent designers who will debut their custom collections on the runway.
On Friday, October 21st the Metropolitan Museum of Art revealed that the 2017 gala will be celebrating the one and only Rei Kawakubo, founder of Comme des Garçons. This marks an important event in history for the gala as it is the first time a living designer will be the sole focus of the exhibit since Yves Saint Laurent in 1983.
With over $230,000 donated to our charity, CAISA Fashion Show is thrilled to continue its partnership with Children’s Health Foundation for the eleventh year.
This year, the funds will support Stem Cell Research at Children’s Health Research Institute.
For more information, please visit the CAISA Fashion Show website.
Canadian researchers will test a promising new fecal microbiota treatment on patients to cure advanced melanoma
The Canadian Cancer Society (CCS) is uniting with a team of 12 researchers and collaborators to lead one of the world’s largest randomized controlled clinical trials using fecal microbiota transplantation (FMT) to improve the effectiveness of the standard of care for advanced melanoma. This phase II trial is made possible by investments of $1 million each from CCS and the Weston Family Foundation and will be overseen by the Canadian Cancer Trials Group.
An estimated 11,300 Canadians are expected to be diagnosed with melanoma in 2024. The current standard of care for patients with advanced melanoma is a type of immunotherapy called immune checkpoint blockade (ICB) and while it plays an important role in treatment, more than half of patients will still experience disease progression and unfortunately die of the disease. Finding a path to make this treatment effective for more people would have enormous impact on patient care and significantly improve the odds of surviving advanced melanoma.
The funding from CCS and the Weston Family Foundation supports all translational research and part of the trial costs (study ME17). The study is being co-led by researchers from Université de Montréal's affiliated hospital research centre (CRCHUM) and Lawson Health Research Institute, alongside collaborators and close to 130 patients with advanced melanoma who will be recruited throughout Canada to participate in this study.
The phase II trial builds on previous research that also received funding support from CCS. Those studies showed the safety and therapeutic potential of using healthy donors’ stool to influence a patient’s gut microbiota and make treatment for advanced melanoma more effective. The study will administer fecal microbiota transplants using specially-prepared oral capsules produced and pioneered at Lawson Health Research Institute, which have been a game changer in patient acceptance and ease of use.
For the past five years, the Weston Family Foundation has supported Canadian researchers working to leverage the microbiome to improve cancer diagnostics, therapy and patient care.
The biggest and most critical issues related to cancer, such as improving treatment effectiveness for people living with melanoma, are issues that require collaboration. From researchers to clinical trial leaders, to academic and scientific institutions, to caring funders and generous donors, it takes a society to transform cancer. To support cancer research and clinical trials, visit cancer.ca.
Quotes
“What saved me was trusting the scientists who knew what they were doing and the promising results of the clinical trial. To someone who is diagnosed, I would say that if you are offered this treatment, it may sound strange, but it is to help you. Thank you to the partners and the CRCHUM team for their support and for the treatments that went wonderfully well and saved my life." - Louise-Hélène Giroux, diagnosed in 2021 with stage 4 melanoma, first patient in the phase I clinical trial in Quebec to try FMT treatment
“Because of the generosity of our donors, we are able to invest in world-leading cancer research and clinical trials like this trial focused on advanced melanoma. In 2020, together with the Lotte and John Hecht Memorial Foundation, we committed nearly $1.5M into this research through an Impact Grant. Today, we are joining with the Weston Family Foundation to double down on our original investment through this clinical trial because we believe this work will transform the future of melanoma, saving lives and bringing hope to thousands of people facing the disease every year in this country.” – Dr. Stuart Edmonds, Executive Vice President, Mission, Research and Advocacy, Canadian Cancer Society
“The Weston Family Foundation is thrilled to support this pioneering research into the role of the microbiome in the fight against cancer, which has real potential to transform treatments and care for this devastating disease. It's a bold step forward in our mission to invest in innovation that delivers measurable impacts to the well-being of Canadians. Working alongside forward-thinking researchers and partners like the Canadian Cancer Society will make way for advancements that help to bring hope to patients and families affected by melanoma.” – Garfield Mitchell, Chair, Weston Family Foundation
“We are aiming to safely change the patient’s gut microbiota to improve the benefit of immunotherapy in several cancers, including melanoma. This experimental treatment consists of transplanting stool from healthy donors using a Health Canada-approved process - known as fecal microbiota transplantation (FMT). With this investment, we can pursue our randomized trial, with the goal of improving the lives of patients with advanced melanoma. We are optimistic that we will see promising results.” – Dr. Arielle Elkrief, principal investigator, Clinician-Scientist, Université de Montréal-affiliated hospital research centre (CRCHUM)
“Our early research has shown the safety of combining FMT with immunotherapy and that it may improve outcomes for patients with melanoma. Through this new trial, we hope to demonstrate that the combination is more effective than immunotherapy alone. A positive result would lead to a phase III trial with the potential to make FMT with immunotherapy the new standard of care.” - Dr. John Lenehan, Medical Oncologist at the Verspeeten Family Cancer Centre at London Health Sciences Centre and Associate Scientist at Lawson Health Research Institute, Co-chair of ME17 trial
The researchers and collaborators
The phase II clinical trial, known as the ME17 Fecal microbiota transplantation (FMT) in combination with immune checkpoint blockade in patients with advanced melanoma: A randomized phase II trial, involves several highly collaborative experts who will be working with the Canadian Cancer Trials Group (CCTG) who will administer the trial nationally. For the translational research associated with the trial, the project team includes:
Co-Principal Investigators:
Dr. Janet Dancey, Medical Oncologist and Professor, Queen’s University, Director of the Canadian Cancer Trials Group
Dr. Arielle Elkrief, Clinician-Scientist and Assistant Professor, Université de Montréal-affiliated hospital research centre (CRCHUM)
Dr. John Lenehan, Medical Oncologist at LHSC’s Verspeeten Family Cancer Centre, Associate Scientist, Lawson Health Research Institute
Dr. Bertrand Routy, Clinician-Scientist and Associate Professor, Université de Montréal-affiliated hospital research centre (CRCHUM)
Dr. Saman Maleki, Scientist, Lawson Health Research Institute, London Health Sciences Centre's (LHSC) Verspeeten Family Cancer Centre and Ontario Institute of Cancer Research (OICR)
Dr. Michael Silverman, Scientist, Lawson Health Research Institute, Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London
Collaborators:
Dr. Seema Parvathy, Lawson Health Research Institute
Dr. Marcus Butler, Leader of the CCTG Melanoma Disease Site Committee, Princess Margaret Cancer Center
Dr. Rahima Jamal, hemato-oncologist, researcher and medical director at the Unit for Innovative Therapies (Phase I-II Unit), Université de Montréal-affiliated hospital research centre (CRCHUM)
Dr. Ian Watson, Associate Professor and Co-chair CCTG Melanoma Disease Committee, McGill University
Dr. Bingshu Chen, Professor, Queen’s University
Dr. Meriem Messaoudene, Research Associate, Université de Montréal-affiliated hospital research centre (CRCHUM)
About the Canadian Cancer Society
The Canadian Cancer Society works tirelessly to save and improve lives. We raise funds to fuel the brightest minds in cancer research. We provide a compassionate support system for all those affected by cancer, across Canada and for all types of cancer. Together with patients, supporters, donors and volunteers, we work to create a healthier future for everyone. Because to take on cancer, it takes all of us. It takes a society. Help us make a difference. Call 1-888-939-3333 or visit cancer.ca today.
About the Weston Family Foundation
At the Weston Family Foundation (formerly The W. Garfield Weston Foundation), more than 60 years of philanthropy have taught us that there’s a relationship between healthy landscapes and healthy people. That’s why we champion world-class health research and innovation with the same passion that we support initiatives to protect and restore biodiversity on our unique landscapes. We take a collaborative approach to philanthropy, working alongside forward-thinking partners to advance Canada and create lasting impacts. We aspire to do more than provide funding; we want to enable others to find transformational ways to improve the well-being of Canadians.
Celebrating Clinical Trials Day
Clinical trials are the gold standard in medical research, used to test new treatments and medical devices to ensure they are safe and improve patient outcomes.
Each year on May 20, Clinical Trials Day aims to raise awareness about the importance of clinical trials. At Lawson Health Research Institute, our researchers, research staff and learners across London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s) are working daily to advance clinical trials for some of the most pressing health challenges.
“If you look at many areas of medicine, like cancer and cardiovascular disease, part of why those conditions have had dramatic improvements in outcomes over the last several decades is because of clinical trials,” says Dr. Amit Garg, Scientist at Lawson, Lead for the Kidney, Dialysis & Transplantation Research Program at ICES Western, and a Nephrologist at LHSC.
Clinical trials can also provide patient participants with new treatment options and can demonstrate when existing treatments have applications for other diseases.
“We could not conduct clinical trials without patients participating in them,” adds Dr. David Palma, Associate Scientist at Lawson and Radiation Oncologist at LHSC. “A clinical trial is a very rigorous process where we carefully define a treatment and follow patients very closely with extra interventions and tests to see not only how the disease is responding to treatment, but also any effects on a patient’s quality of life.”
It also takes a team to make clinical trials a success, including the critical work of research coordinators, associates and assistants, adds Dr. Swati Mehta, Lawson Scientist based at St. Joseph’s Parkwood Institute.
Dr. Palma also notes that while clinical trials require investment to conduct them, they can ultimately lead to savings in the health system.
“While the primary goal of a clinical trial is to improve or save lives, they often lead to cost savings down the road. Improving cure rates means people don’t need as much treatment and that can save the initial investment many, many times over,” Palma says.
Looking ahead, work is ongoing to make clinical trials more efficient and equitable.
“Eliminating specialized infrastructure would help make trials more equitable, so they are available in smaller communities and at distant sites that otherwise would not have access. Making study materials available in multiple languages and to anyone with accessibility issues can also help,” Garg adds.
“Future clinical trials will need to follow more pragmatic, adaptive study designs that allow us to evaluate therapies or interventions in a more realistic setting,” Dr. Mehta says. “These would also allow us to follow-up with patients that were potentially underrepresented in past research.”
According to researchers at Lawson, the future of clinical trials is bright with hundreds of trials currently underway at LHSC and St. Joseph’s with the goal of improving patient outcomes.
Celebrating health research excellence with the 2023 Lawson Impact Awards
For the first time since 2019, Lawson Health Research Institute hosted its annual Lawson Impact Awards in-person on November 28 at RBC Place London. Approximately 130 people gathered to celebrate scientists, staff members, learners and partners who have made remarkable contributions to hospital-based research at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s).
“Important and groundbreaking science is conducted daily at Lawson, improving patient care locally and around the globe,” says Dr. David Hill, Scientific Director at Lawson. “The Lawson Impact Awards provides an opportunity for us to recognize the scientists, staff members, learners and partners who drive medical research forward.”

Eight Lawson Impact Award recipients were celebrated at the event, including:
- Leadership Award for Fellows & Students: Dr. John Tran
- Staff Award of Excellence: Alexandria Roa Agudelo
- Community Partner of the Year Award: Keith and Leanne Lavergne
- Community Partner of the Year Award: Jack and Jean Wettlaufer Family
- Community Partner of the Year Award: Ryan Finch
- Dr. Joseph Gilbert Research Contribution of The Year Award: Dr. David Palma for “Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial”
- Innovation Award: Dr. Manuel Montero-Odasso
- Scientist of The Year Award: Dr. Cheryl Forchuk
Two Children’s Health Research Institute (CHRI) award recipients were also recognized. As a program of Lawson, CHRI awards a Scientist and Trainee of the Year annually, sponsored by the Children’s Health Foundation. CHRI’s 2022 award recipients are: Dr. Emma Duerden (CHRI Scientist of the Year) and Kendrick Lee (CHRI Deb Comuzzi Trainee of the Year).
“This year, we recognized a number of leading research professionals from across LHSC and St. Joseph’s who are helping to advance patient care in London and around the world,” adds Dr. Hill. “We were also honoured to recognize three Community Partners of the Year for their generous support of health research.”
Learn more about each recipient on our Impact Awards page and visit the Lawson YouTube channel to watch videos highlighting each of the award recipients.
Celebrating remarkable women in science
Chronic pain can affect every facet of a person’s life. “When someone is in pain, they can have significant difficulty with activities we all do in our daily life, from getting out of bed to walking to the mailbox. It can also impact their mental wellness,” shares Lawson Health Research Institute Scientist Dr. Siobhan Schabrun, PhD. Dr. Schabrun, who is the first ever William and Lynne Gray Endowed Research Chair in Mobility and Activity at St. Joseph’s Health Care London, has dedicated much of her career to unravelling the complex connection between the body and the mind known as neuroscience, with a focus on persistent pain.
She is currently leading groundbreaking work in understanding, treating and preventing persistent pain, offering hope for enhanced mobility and activity in individuals with musculoskeletal and neurological conditions at St. Joseph’s Gray Centre for Mobility and Activity, located at Parkwood Institute.
Dr. Schabrun’s research program has extended beyond conventional approaches, delving into the use of non-invasive brain stimulation technologies such as repetitive transcranial magnetic stimulation, more commonly known as rTMS, a therapeutic tool used in mental health treatments for decades, to augment neuroplasticity and optimize outcomes in rehabilitation.
Bridging the gap between human pain models and clinical trials, Dr. Schabrun’s work is contributing to the understanding of clinical pain populations and bringing new treatment methods to the forefront to improve patient care and outcomes.

Celebrating the 2022 Lawson Impact Award winners
The Lawson Impact Awards are a pinnacle of celebration in the Lawson Health Research Institute community, celebrating innovation across London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. The Impact Awards recognize hospital-based research that makes a difference by advancing scientific knowledge and applying it directly to patient care.
With awards in eight categories, the annual awards honour Lawson scientists, staff, trainees and partners who demonstrate excellence.
“The Lawson Impact Awards are a celebration of the research mission of LHSC and St. Joseph’s,” says Dr. David Hill, Scientific Director at Lawson. “There is innovation happening every day here in London, Ontario. The environment and close proximity to patient care allow us to hire great scientists that flourish in our research space.”
Recognized for his high-impact work over the past several years, Dr. Douglas Fraser was named as Lawson’s Scientist of the Year – the Lawson Impact Awards’ highest honour. Dr. Fraser, who is a Scientist at Lawson and Critical Care Physician at Children’s Hospital at London Health Sciences Centre (LHSC), has led the way in a number of areas of research. Over the past few years, he has published numerous studies and signed multiple licensing agreements that show promise for improving the diagnosis and treatment of concussion, COVID-19 and long COVID.
“Research is exciting to me and I love showing up to work. We have great colleagues, wonderful resources which allows us to ask good questions and it is a pleasure coming to work each day,” says Dr. Fraser, who is also a Professor at Western University’s Schulich School of Medicine & Dentistry. “It I always an honor to be recognized and humbling as well, because most of the work we have done has always been a group effort.”
Dr. Fraser is one of eight 2022 Lawson Impact Award recipients.
A big congratulations to all of this year’s winners, as well as our 2022 Lawson Strategic Research Fund recipients:
Scientist of The Year Award: Dr. Douglas Fraser
Dr. Joseph Gilbert Research Contribution of The Year Award: Dr. Daniel Hardy
Innovation Award: Dr. Dalton Wolfe
London Health Sciences Foundation Community Partner Of The Year Award: Archie Verspeeten
St. Joseph's Health Care Foundation Community Partner Of The Year Award: Dr. Joseph Rea
Children's Health Foundation Community Partner Of The Year Award: Dr. Paul and Mrs. Mary Harding
Leadership Award for Fellows & Students: Karnig Kazazian
Staff Award Of Excellence: Dr. Jeff Weiler
Strategic Research Fund Recipients: Dr. Matthew Teeter & Dr. Jonathan Thiessen and Dr. Luciano Sposato & Dr. Frank Prato
You can visit the full Impact Awards site by clicking here
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Changing our MINDS
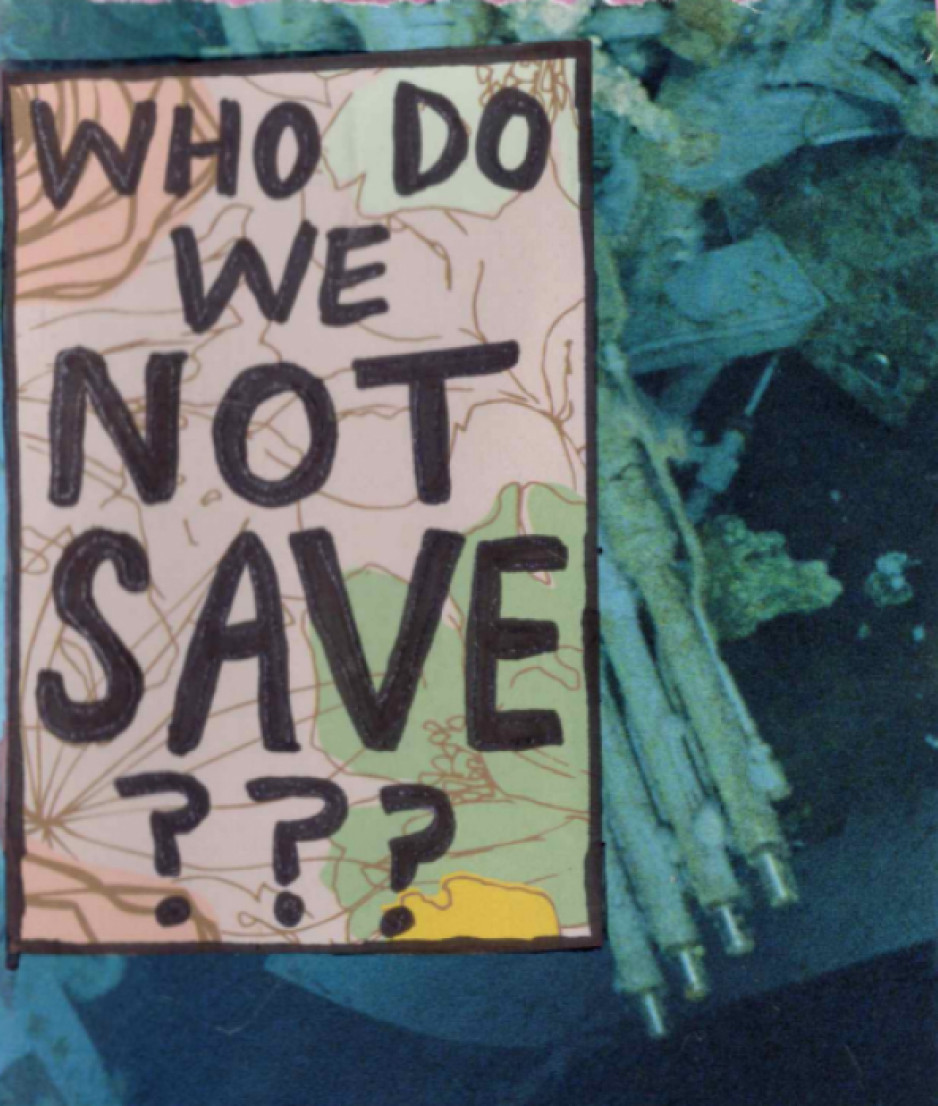
Local youth use art and storytelling to illustrate the personal and system challenges in mental health.
The words and images are both heartbreaking and hopeful.
“Nobody likes you if you are sad.”
you are enough. stay strong. let life surprise you.
“Please don’t leave like everyone else.”
1 year sober. 1 year of school. 1 year building a safe home. 1 year loving myself.
Zine-writing, a personal and introspective medium often used by people who have been marginalized, is an important part of local research that is finding solutions to complex mental health challenges among young adults. Its name derives from its magazine (“zine”) format.
“When we make the voices of people with lived experience central to our research, we can learn from each other and then change the system together,” says Dr. Arlene MacDougall, founder of MINDS of London-Middlesex.
The social innovation and research lab based at St. Joseph’s Health Care London (St. Joseph’s) is dedicated to designing, piloting and testing mental health innovations for teens and young adults. Its recent evolution into MINDS 2.0 adds insights by and for people up to age 35 who have complex, pervasive mental health and addiction issues.
Learning from experts
Rin, a London artist, who has published independent zines for a decade, created three for this project, including one that, with irony, asks the reader to ponder which vulnerable people aren’t worth saving.
“I believe making art can be very healing,” says Rin. “I wanted to share some of my story to help myself and help others. I want to play a part in shaping a mental health system that’s better than the one I encountered.”
The zines weave art, prose and poetry into story:
3 things I would change: affordability, stigma, waitlists.
“If I had a magic wand, I would use it to heal the waters, grow the trees, foster animal growth.”
Look in the mirror, see how far you’ve come.
They also raise and propose solutions to troubling issues among people with mental illness: housing and homelessness, sparse resources for people with addictions, lack of coordination among service providers, and dehumanizing attitudes in health and criminal justice systems.
“Participants experienced catharsis just in telling their stories,” says Renee Hunt PhD, Associate Director of Research and Operations at MINDS. “And because they’re the experts, they’re also playing an important part in changing systems that need an overhaul.”
Adds Rin, “It feels empowering knowing people are listening to us – people who care and are committed to making change to the system.”
MacDougall notes the pivotal role of St. Joseph’s Health Care Foundation – in particular, a groundbreaking $5-million donation towards mental health research from philanthropist Ryan Finch – in advancing mental health innovation through MINDS and MINDS 2.0.
“They’ve been our biggest supporters since day one. This wouldn’t have happened without support from Ryan and the foundation and all the many donors who believe in mental health research,” says MacDougall, who is also Director of Research and Innovation with St. Joseph’s Mental Health Care Program.
“MINDS has been a catalyst for system change,” MacDougall adds. “Research is always about finding answers and generating impact.”
Many findings from MINDS research have been put into practice, among them are the creation of guidebooks for peer support, free taxi service for rural youth needing urban mental health or addiction services, and educational resources to support 2SLGBTQI+ students.
MacDougall says MINDS 2.0 expands that work with new voices and the exploration of more in-depth solutions.
What’s next for MINDS 2.0
- Workshopping ideas and prototypes for mental health systems change. Sessions will be held where people with lived/living experience and service providers propose and develop potential solutions.
- Leadership-building. Twenty mental health practitioners will be trained to become “agents of change” who will collectively create, implement and evaluate mental health programs, technology, interventions and training.
- Imaginarium conference. In 2025, a first-of-its-kind national conference will take place to share system innovations in mental health and addiction.
CIHR funding for COVID-19 enables researchers to investigate virus transmission during surgery and pandemic planning
Researchers at Western University and Lawson Health Research Institute continue to make important contributions to help mitigate the spread of COVID-19 and its negative consequences. Two projects in London will address virus transmission during surgery and pandemic planning for COVID-19, thanks to new funding announced by the Government of Canada, through the Canadian Institutes of Health Research (CIHR), along with provincial partners.
Researchers in London received more than $400,000 in funding through this latest round.
“Accelerating high-quality research and real-time evidence is a priority for Canada in its fight against COVID-19. I congratulate the successful teams for their essential work aimed at better preventing, detecting and treating COVID-19 at the individual and population levels,” said Patty Hajdu, Minister of Health in a press release. “Our government believes that it’s through collaboration and data sharing that we will respond efficiently to this global health emergency.”
Virus transmission in surgical smoke
In an effort to perform surgery during the pandemic as effectively and safely as possible, Dr. Leigh Sowerby, Associate Professor at Schulich Medicine & Dentistry and Associate Scientist at Lawson, will be investigating whether or not the virus that causes COVID-19 can be transmitted in surgical smoke. Surgical smoke is the aerosol produced by an essential surgical tool called electrocautery.
“Electrocautery is a ubiquitous tool for surgery, and is known to generate aerosol and smoke. We do not know if the SARS-CoV-2 virus can be transmitted in this plume, and this is important to answer for all surgeons, but in particular, for surgeons working in the respiratory and aerodigestive tract,” said Dr. Sowerby, who is also a head and neck surgeon at London Health Sciences Centre and St. Joseph’s Health Care London. “CIHR funding will allow us to rapidly execute this project. Without this funding, the project would not be possible.”
Dr. Sowerby says the results from this study, whether positive or negative, will have important implications. If positive, it will have a critical and direct impact on ensuring the safety of health care workers performing procedures on patients. Procedures using cautery will continue to require high level protection if the COVID-19 status of the patient is unknown. If negative, it will allow these surgical procedures to continue safely and effectively while conserving critical protective equipment for cases that need it.
The family physician’s role in pandemic plans
Maria Mathews, PhD, Associate Professor at Schulich Medicine & Dentistry, is investigating how the role of family physicians can be better incorporated into pandemic plans. Family physicians play important roles during a pandemic, from detecting potential outbreaks and screening and testing patients to providing care to infected patients and contributing to surge capacity in hospitals.
“During the early stages of the COVID-19 pandemic, family physicians had concerns about roles they were asked to fill for a variety of reasons, including the lack of appropriate personal protective equipment, availability of tests, and concerns about infection risks to other patients and staff in a family practice clinic,” said Mathews.
Mathews will examine the experiences in four regions in Canada – Newfoundland and Labrador, Nova Scotia, Ontario and British Columbia – to identify key roles, supports and best practices. The results will provide government ministries, public health units, and other health organizations with evidence and tools in order to incorporate family physicians in the response to a potential second COVID-19 wave and plan for future pandemics.