Search
Search
New Alzheimer’s research aims to improve treatment and support for patients with agitation
Two new interventional studies have been brought to London, focused on improving quality of life for patients with Alzheimer’s disease and their caregivers. Both hope to improve upon standard approaches to treating agitation, a core symptom of Alzheimer’s.
Agitation is a significant source of stress for patients and caregivers. It is complex and difficult to treat. Often, families do not know about this particular symptom of Alzheimer’s and are not properly trained on how to manage care while dealing with agitation.
“These studies are designed to have a direct impact on patients, families and care providers, to improve quality of life and function in those suffering from agitation due to Alzheimer’s,” says Dr. Amer Burhan, Associate Scientist at Lawson Health Research Institute (Lawson) and Geriatric Neuropsychiatrist, St. Joseph’s Health Care London (St. Joseph’s).
Parkwood Institute, a part of St. Joseph’s, is one of multiple sites participating in these studies across Canada and the United States.
One study aims to identify patients early in their diagnosis, while they are living at home or in the community, and apply a comprehensive psychosocial approach, with or without medication, to help with the management of agitation. “We hope to identify participants and have them participating in our program before they experience a crisis due to agitation,” explains Dr. Burhan.
Psychosocial intervention is a way of helping patients and caregivers understand the reasons for agitation. Agitation can develop due to a wide range of causes. For example, patients may just be bored and need help to find something meaningful to occupy their time, they could be upset about something in their current environment, or may be suffering from physical discomfort or pain.
Interventions can include communicating with patients in a manner that creates calm, scheduling meaningful activities, and maintaining routine and rhythm in life. The research team will connect with families early after diagnosis to give them the tools and support they need.
Initially, participants will be treated using structured psychosocial intervention to help reduce and manage their agitation. After three weeks, they will be reassessed and if significant agitation continues to persist, the patient will be randomly selected to receive either a placebo, or medication known as S-Citalopram to treat agitation while they continue to receive psychosocial care.
Sylvia Wilson is the wife of one of the study participants. By enrolling in this trial, she feels she has gained a much better understanding of her husband’s disease, and is grateful for the support that study participants receive.
“My husband typically does not like going to visit doctors, but Dr. Burhan and his team are great,” says Wilson. “They understand agitation, and other symptoms of the disease very well, and I notice a difference in his mood with the treatment he receives through the study.”
Participants are still able to receive care from their primary physician and care teams, with the study providing an added layer of support.
Another study is focused on Alzheimer’s patients who are admitted to hospital or living in long-term care. The aim is to standardize the approach to care for agitation related to Alzheimer’s. After baseline assessment, participants will be randomized to receive the current treatment as per usual, or an integrated care pathway derived from evidence-informed treatment guidelines. These include washing out medications that have not helped, adding individualized behavioral and environmental support, and if medications are needed, use a specific set of medications and dosages based on best evidence.
“Better understanding agitation is a growing area of interest in geriatric research. The work being done locally is part of an international effort to create a paradigm shift in treating patients with Alzheimer’s disease and agitation,” explains Dr. Burhan.
Researchers are ready to offer these studies to patients and their families, hoping to make these treatment protocols an integral part of care for patients with agitation due to Alzheimer’s disease. Those interested in learning more about these studies can contact Dr. Burhan at @email or call 519-646-6100 x. 48170.
In the media: Study on 'agitation' in Alzheimer's patients seeks participants
New clinical protocol after general surgery cuts opioid prescribing in half
In recent years deaths from opioid overdoses have become one of the most common injury-related deaths in North America. The continent also has the highest per capita rate of opioid prescription in the world.
Recognizing the role that opioid prescribing plays in the national opioid crisis, a team of researchers at Lawson Health Research Institute and Western University have developed a new clinical protocol called STOP Narcotics. A study demonstrating the efficacy of their protocol was presented at the American College of Surgeons Clinical Congress in Boston, Massachusetts on October 24.
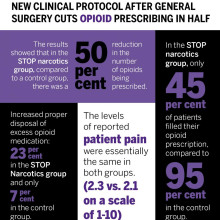
The protocol includes a combination of patient and health care provider education and an emphasis on non-opioid pain control. The study found that they were able to reduce the overall amount of opioids being prescribed after general surgery by 50 per cent while still adequately treating a patient’s post-operative pain.
“By significantly reducing the amount of opioids prescribed, this decreases the exposure risk and potential for misuse of narcotic medication,” said Dr. Luke Hartford, a resident in general surgery at Western’s Schulich School of Medicine & Dentistry and first author on the study. “This also decreases excess medication available to be diverted to individuals for whom it was not intended.”
The study involved 416 patients at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London who underwent laparoscopic cholecystectomy or open hernia repair. They received medication for post-operative pain through the standardized protocol, specifically acetaminophen (Tylenol) and a non-steroidal anti-inflammatory drug (Naproxen) for the first 72 hours post-surgery.
The protocol instructs physicians to write a limited prescription of ten pills of opioids (Tramadol), with an expiry date of seven days after surgery, with instructions for the patient to fill this prescription only if adequate pain control was not otherwise achieved. There are also instructions on proper disposal of unused medication for the patient.
Dr. Ken Leslie, scientist at Lawson, associate professor in the Department of Surgery at Schulich Medicine & Dentistry, and Chair/Chief of the Division of General Surgery at London Health Sciences Centre led the implementation of the new protocol.
“We recognized that before STOP Narcotics, every surgeon had a different approach to pain control, and that most surgeons were prescribing more narcotics than are actually needed,” said Dr. Leslie. “When we looked at the data from this new protocol, we saw that the patient’s pain-control was just as good with this pathway, without a huge prescription for narcotics.”
The results showed that in the STOP narcotics group, compared to a control group, there was a 50 per cent reduction in the number of opioids being prescribed. They also demonstrated that only 45 per cent of patients actually filled their opioid prescription, compared to 95 per cent in the control group, and they were also able to increase appropriate disposal of excess opioid medication from 7 per cent in the control group to 23 per cent in the STOP Narcotics group. The levels of reported post-operative pain were the same in both groups.
The group now hopes to expand the protocol for applications beyond general surgery.
“If we can decrease the opioid exposure risk in our patients, and decrease the amount of excess medication available for diversion, and spread this to other institutions and surgical procedures and specialties, this has the potential to significantly impact the opioid crisis,” said Dr. Patrick Murphy, a resident in general surgery at Schulich Medicine & Dentistry and co-author on the study.
The study, “The Standardization of Outpatient Procedure (STOP) Narcotics: A Prospective Noninferiority Study to Reduce Opioid Use in Outpatient General Surgical Procedures,” is published in the Journal of the American College of Surgeons.
| Dr. Ken Leslie | Dr. Luke Hartford | Dr. Patrick Murphy |
Image

|
Image

|
Image
|
New imaging tool for diagnosing heart disease
An international team led by scientists from Lawson Health Research Institute and Cedars-Sinai Medical Center are the first to show that Magnetic Resonance Imaging (MRI) can be used to measure how the heart uses oxygen for both healthy patients and those with heart disease.
Reduced blood flow to the heart muscle is the leading cause of death in the Western world. Currently, the diagnostic tests available to measure blood flow to the heart require injection of radioactive chemicals or contrast agents that change the MRI signal and detect the presence of disease. There are small but finite associated risks and it is not recommended for a variety of patients including those with poor kidney function.
Standard methods
More than 500,000 of these tests are performed each year in Canada. A patient suspected of coronary heart disease for example may have reasonably normal blood flow at rest but as soon as they exercise they have pain or feel out of breath. They need more oxygen delivered to the heart tissue but due to vessels being compromised that doesn’t happen.
The standard technique is usually done in two days with the goal of seeing if the heart can increase blood flow when more oxygen is needed. The first test studies the patient at rest to see what the blood flow is like in the heart. This is a nuclear medicine imaging test that requires radioactive material to be injected and takes about an hour or more to complete.
They next day, they come for the same test but with the introduction of a stressor. That can be physical exercise but more often they are given an injection of a chemical drug which stimulates the heart and increases blood flow. This is in addition to a second injection of the radioactive material. The heart is imaged to see the level of oxygen getting to different parts of the heart and whether there are obstructions or reduction in size of the surrounding arteries.
A new stress test
“We wanted a non-invasive way to image the heart and replace the stress stimulus, and drastically reduce the amount of time needed for testing,” says Dr. Frank Prato, Lawson Assistant Director for Imaging. “This new method, cardiac functional MRI (cfMRI), does not require needles or chemicals being injected into the body. It eliminates the existing risks and can be used on all patients."
The team included researchers from Lawson; Cedars-Sinai Medical Center and University of California; King’s College in the United Kingdom; University Health Network and the University of Toronto; Siemens Healthineers; and, University of Edinburgh in the United Kingdom.
“Our discovery shows that we can use MRI to study heart muscle activity,” explains Dr. Prato. “We’ve been successful in using a pre-clinical model and now we are preparing to show this can be used to accurately detect heart disease in patients.”
To replace the stress test, this new technique uses repeat exposure to carbon dioxide to test how well the heart’s blood vessels are working to deliver oxygen to the muscle. A breathing machine changes the concentration of carbon dioxide in the blood. Levels are brought up for three minutes and then back down to normal four times. These changes should result in a change in blood flow to the heart, but does not happen when disease is present.
The cfMRI method reliably detects whether these changes are present and is comparable to the information gathered from the current two-day technique – in much less time and without injections. Dr. Prato notes that “we don’t want to stress the heart. We want to see whether there is capacity in the heart to increase blood flow if the heart needs to work harder.”
A brilliant discovery
Other researchers have explored oxygenation-sensitive MRI but initial results contained a high level of ‘noise’ with blurry images. Project leader and partner Dr. Rohan Dharmakumar, Associate Director of the Biomedical Imaging Research Institute at Cedars-Sinai Medical Center, believed that the noise was actually variation in the heart’s processing of oxygen. He engineered a way to average this variation and through testing at Lawson the team discovered that the noise is actually a new way to study how the heart works.
“We’ve opened the door to a new era and totally novel way of doing cardiac stress testing to identify patients with ischemic heart disease” says Dr. Dharmakumar. “This approach overcomes the limitations of all the current diagnostics – there would no longer be a need for injections or physical stress testing like running on treadmills.”
Through investigating this technique, they learned that the blurry images were showing normal physiological variability. People often think of heart rate as being stable, but in fact a heart that is unable to keep up with stressors indicates that disease is developing. In a healthy heart, the oxygen distribution to the tissue needs to vary.
“It’s a very exciting time. We had to bring all the technologies together to be able to image these kinds of changes in blood flow moment to moment,” says Dr. Prato.
He adds that “using MRI will not only be safer than present methods, but also provide more detailed information and much earlier on in the disease process.” Following initial testing through clinical trials, he sees this being used with patients clinically within a few years.
Moving forward
In addition to studying coronary artery disease, the method could be used in other cases where heart blood flow is affected such as the effects of a heart attack or damages to the heart during cancer treatment. Due to its minimal risk, this new tool could be safely used with the same patient multiple times to better select the right treatment and find out early on if it is working. Dr. Prato notes that “with this new window into how the heart works, we have a lot to explore when it comes to the role of oxygen in health and disease.”
The next steps of the research include a proof of principle study in London, Ontario with 20 patients. Following standard tests using the conventional technique at other sites, the participants will then come in for the experimental test to show that it produces the same result. The research would then move into a multi-centre clinical trial internationally.
The study “Accurate needle-free assessment of myocardial oxygenation for ischemic heart disease in canines using Magnetic Resonance Imaging” is published in Science Translational Medicine.
New study aims to improve treatment for rheumatoid arthritis
A research team led by Lawson scientist Dr. Mamadou Diop has been awarded a Lawson Internal Research Fund to investigate whether a previously developed optical technique that can detect arthritis within one week of onset could also be used to provide early assessment of treatment response for rheumatoid arthritis (RA).
RA is a disease that causes chronic inflammation of the joints, which results in pain, reduced quality of life and loss of productivity. There is no cure for RA but a new category of drugs – biologic agents that can reduce pain and slow down or even halt disease progression – has revolutionized treatment.
However, these new drugs are expensive and only work in 30 per cent of patients, which means many RA sufferers are treated with no benefit for up to six months – the time it takes for current monitoring methods to reliably determine whether a treatment is working or not. “This is a direct consequence of the lack of sensitivity of current monitoring methods,” says Dr. Diop, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
Since their recently developed optical technique has a high sensitivity to arthritis, Dr. Diop and his team believes it could also be used as a safe and convenient method of assessing treatment efficacy in RA patients. Additionally, there are striking similarities between RA and cancer, and it has been shown that optical techniques can predict cancer in as early as one day after therapy starts.
At St. Joseph’s Health Care London, they will test this theory in a rat model of RA and compare the results of the optical technique to histology and CT imaging, other established methods of determining whether a treatment is effective.
“If successful, this project will generate a safe, low-cost technique that can detect treatment response in RA within days of starting treatment. This would reduce the risk of further joint damage experienced by many patients for whom the drugs are ineffective,” says Dr. Diop. “We hope this will enable early redirection of patients with non-responding RA to alternative treatments, such as a combination of multiple drugs and more frequent monitoring.”
Dr. Diop adds, “The Lawson IRF grant will enable us to test the validity of our hypothesis and subsequently generate valuable preliminary results to support grant proposals for larger external funding.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
New study examining if probiotics can improve outcomes in knee replacement surgeries
Researchers at Lawson Health Research Institute are examining whether the use of a daily probiotic can improve outcomes in patients who undergo a total knee replacement surgery.
There are more than 70,000 knee replacement surgeries in Canada each year, and up to 10 per cent of patients experience complications following the procedure.
“One in five patients are dissatisfied after surgery due to pain and discomfort, and some patients need a repeat surgery because there is complication, infection or loosening of the joint,” says Dr. Matthew Teeter, Lawson Scientist at London Health Sciences Centre (LHSC).

Dr. Teeter and the research team are focused on improving patient outcomes. Recognizing that knee replacement patients who are considered healthy tend to have better outcomes, they are interested in how they can better support patients’ overall health as one way to optimize their outcomes.
“The knee replacement patients I see in clinic are very diverse - from young healthy active patients to medically complex to socioeconomically disadvantaged,” says Dr. Brent Lanting, Lawson Scientist and Orthopaedic Surgeon at LHSC. “We know those with poor health do not do as well as those with good health, good diet, and good supports. This study is profound in that it investigates a core aspect of our health – the gut microbiome.”

The research team will recruit 30 participants who are scheduled for a knee replacement surgery. Half of the participants will receive a daily probiotic for six-weeks ahead of the surgery, and the other half will act as a control group.
“Our microbiome is a large part of why we are healthy. A healthy person has a microbiome that produces vitamins and other things which cross over to our system and helps promote healing,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London. “We are hoping it will improve more deep healing and prevention of the rejection of the joint by improving the microbiota by giving probiotics.”
The team will assess outcomes using CT imaging, looking at the bone and implant and how it is fixing into place. They will also use PET/MRI to look at the cellular activity around the joint and inflammation.
“This should give us a sharp focus of what is going on with the joint and help us determine if there was a positive effect by using probiotics,” explains Dr. Teeter.
If the pilot study proves to be promising, the team will then work towards a larger clinical trial, combining probiotics into pre-surgical care.
“Ultimately, we want better patient outcomes with a simple treatment,” adds Dr. Burton. “If we can help improve outcomes with the use of a daily probiotic, that is a great win.”
The research team received a New Frontiers in Research Fund (NFRF) of $250,000 over three years to conduct this study.