Search
Search
Improving surgery for wrist arthritis
Wrist arthritis can cause debilitating pain, weakness and decreased range of motion. When patients are first diagnosed, the condition can often be managed with activity modification and pain medication. However, as symptoms progress, patients eventually require surgery.
Surgeons typically perform a procedure called four-corner fusion to preserve wrist motion and provide pain relief. This surgery involves removing one of the carpal bones and fusing four of the remaining carpal bones. Although this procedure is one of the most common treatments for wrist arthritis, it is not known how the position of the fusion of the wrist bones affects range of motion and joint contact.
Lawson associate scientist Dr. Nina Suh is leading a study with the goal of improving the surgical technique for four-corner fusion to maximize wrist function and symptom relief, and delay wrist arthritis progression.
Dr. Suh and her team will use a customized active-motion wrist simulator to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
“We hope this research will lead to new surgical techniques that will help us to more effectively manage wrist arthritis with four-corner fusion,” says Dr. Suh, who is also an orthopaedic surgeon at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London and an assistant professor at Western University’s Schulich School of Medicine & Dentistry. “The project will also advance our understanding of wrist biomechanics, providing a foundation for the development of enhanced patient-specific surgical tools, such as custom wrist fusion devices and implants.”
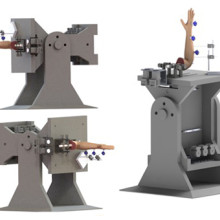
Image of the customized active-motion wrist simulator Dr. Nina Suh and her team are using to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
The study is being funded through the Lawson Internal Research Fund (IRF), designed to allow scientists the opportunity to obtain start-up funds for new projects with exciting potential.
“The IRF program is valuable for scientists as external funding sources routinely require preliminary data to strengthen applications,” says Dr. Suh. “Particularly for new scientists such as myself, these grants provide seed funding that allows us to demonstrate the validity of our methodology and the clinical usefulness of our results.”
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Jamie Fleet
Jamie Fleet, MD
Assistant Professor, Schulich School of Medicine and Dentistry
Stroke
Dr. Jamie Fleet is a physiatrist at Parkwood Institute and an Assistant Professor in the Department of Physical Medicine and Rehabilitation at the Schulich School of Medicine and Dentistry at Western University. Dr. Fleet completed medical school as well as residency training in Physical Medicine and Rehabilitation at McMaster University. She is currently enrolled in a Master’s program in Clinical Epidemiology through the Health Research Methodology program at McMaster University with a focus on fracture treatment and prevention in older patients after stroke. Her primary clinical area of focus is in stroke rehabilitation.
Though still early in her career, Dr. Fleet has developed a strong research background, primarily focusing on drug safety studies in older adults using large data through ICES. Her other research interests include exercise and health promotion/prevention strategies in patients after stroke, as well as fall prevention strategies and pain management. "

Laura Brunton
Laura Brunton, PT, PhD
Assistant Professor, School of Physical Therapy
Childhood Onset Conditions
Laura Brunton is an Assistant Professor in the School of Physical Therapy at Western University and is a registered Physiotherapist. Professor Brunton's current research focus is exploring and understanding fatigue and pain experienced by individuals with cerebral palsy and the possible relationships with physical activity, sleep, pain and mental health. Professor Brunton has an interest in developing novel approaches to increase and support the self-management skills for youth and adults with childhood-onset conditions. A secondary interest of Professor Brunton’s is the development and validation of clinical measures to support comprehensive assessment of clients in clinical practice.

Leveraging virtual reality to manage pain in paediatric patients
London - A new study underway through Lawson Health Research Institute and Children’s Hospital at London Health Sciences Centre (LHSC), using virtual reality (VR) to help pediatric patients during painful and distressing procedures.
“Technology holds immense potential for improving the experience of our young patients and their families,” explains Dr. Naveen Poonai, Lawson Scientist, principal investigator and Emergency Department Physician at Children’s Hospital. “VR is becoming increasingly popular amongst young people and some early research shows VR has been helpful in painful procedures, even in adults.”
The study is focusing on pediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in pediatric cancer patients.
“This can be very distressing for a patient and it can set the tone for their entire clinic day and course of treatment,” says Dr. Alexandra Zorzi, Lawson Associate Scientist and Pediatric Oncologist at Children’s Hospital. “Minimizing the stress, anxiety, and pain of the procedure is key to avoiding a negative experience.”
The study team is recruiting 90 pediatric patients with existing medical ports. Participants will be randomized into three groups. One group will be using a VR headset that will allow them to play interactive games. The second group will have access to tablet technology, and the final group will be provided with non-technology distractions. Each procedure and the patient’s response will be recorded. Responses will then be compared using a tool called the ‘Observational Scale of Behavioral Distress’ to determine which intervention leads to the best outcomes.
“My hopes are that we develop a variety of skills we can tailor to patients,” adds Dr. Zorzi. “There are patients who receive all kinds of support but still struggle, so having a variety of techniques available to see what works best is a positive step forward.”
The study is expected to be completed by the end of this year. The research team is already collaborating with Children’s Hospital staff and leadership to use VR as a clinical tool if the study proves the technology to be effective.
“We have plans in place to allow whatever we find as the best option to be part of routine care for kids needing port access,” notes Dr. Poonai. “We are also speaking with various medical teams to determine how we can incorporate this into practices across the hospital.”
The use of the VR devices has been made possible with generous support from the Children’s Health Foundation.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers adapt MRI technology to image salt within the kidneys
LONDON, ON – In a newly published study, scientists at Lawson Health Research Institute have adapted PET/MRI technology to accurately image salt within the kidneys of patients with kidney disease.
“Salt is very difficult to image in an MRI because the signal is much weaker than water,” explains Dr. Christopher McIntyre, Lawson Scientist and Nephrologist at London Health Sciences Centre (LHSC). “We wanted to find a way to look at the fundamental role of the kidney in getting rid of salt and water by using a functional MRI.”
Imaging salt within the kidneys has never been accurately accomplished in patients with kidney disease, but Dr. McIntyre and his team developed new technology and software that was adaptable to a PET/MRI machine at St. Joseph’s Health Care London. The new technology allowed the machine to image salt and water levels within the kidney.
“Salt within the kidneys have only been imaged in pre-clinical models, and low weight, healthy volunteers,” says Dr. McIntyre. “Since the kidney is further away from the MRI coils, and the organ moves when a person breathes, it is definitely very hard to image.”
This was the first study to use MRI to look at salt within the kidneys with a wide range of participant with different body types (10 healthy volunteers), as well as patients with kidney disease (five patients). The research team also imaged patients who had a combination of kidney disease and heart failure, because it is especially important for those patients specifically to be able to release salt and water as part of their treatments.
Currently clinicians rely on kidney biopsies to measure salt levels, but Dr. McIntyre says that method isn’t as accurate or effective as it could be.
“The problem is that the biopsies are painful, they have risks, and because it is a small sample of the kidney, we don’t get an accurate perspective of the kidney as a whole,” Dr. McIntyre explains.
The study, which is published in Radiology has now opened the door to new possibilities when it comes to clinical care for patients with kidney disease.
“Salt is very toxic in patients with kidney failure,” adds Dr. McIntyre. “This will now allow us to diagnose and manage both chronic and acute kidney disease. It is a significant step forward.”
The next steps for the research team will be to compare salt MRI’s to biopsies, while also examining potential new therapy developments.
“We are hoping we will have a higher degree of certainty moving forward to predict what will happen within the kidneys of these patients, with the possibility of using new targeted and effective treatments in the future,” notes Dr. McIntyre.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Metabolic syndrome commonly associated with early rheumatoid arthritis
A Canada-wide multicentre study of patients with early rheumatoid arthritis (ERA) has found an association between metabolic syndrome and rheumatoid arthritis, and that the prevalence is most common among men and postmenopausal women.
September is National Arthritis Awareness Month in Canada. With rheumatoid arthritis, the patient’s joints and organs are “attacked” by their own immune system. This is the most common type of autoimmune arthritis. Persons with the disease typically experience swollen joints, pain and stiffness, and chronic fatigue. In later stages of the disease, incessant inflammation breaks down the joint, causing permanent damage, and can impair nerves and blood vessels. It is important for patients to begin treatment as early as possible.
The Canadian Early Arthritis Cohort (CATCH) study collects data on over 3,000 patients across Canada with ERA. Patients in this cohort are defined as a person who is within one year of symptom onset.
Dr. Lillian Barra, Associate Scientist at Lawson Health Research Institute (Lawson), and Rheumatologist at St. Joseph’s Hospital London, was interested in learning about the association between ERA and other diseases and conditions that are commonly found among patients with ERA. Metabolic syndrome refers to a cluster of conditions that often occur together and increase the risk of heart disease, stroke, and type 2 diabetes. These include heart disease, high blood pressure, abnormal cholesterol, obesity and high blood sugar.
“It is interesting that we found these conditions of metabolic syndrome so early in the course of this disease. While previous researchers have demonstrated an association, it remains a question whether metabolic syndrome contributes to rheumatoid arthritis, or vice versa.” explains Dr. Barra.
“This information can help inform clinicians managing patients with rheumatoid arthritis. In the future, we hope to develop more precise guidelines around when these comorbidities should be screened for and co-managed over the course of treatment.”
Currently, if a newly diagnosed rheumatoid arthritis patient presents with severe symptoms, they are given therapies that work quickly to reduce the inflammation in addition to long-term disease modifying drugs that are the standard of care. These therapies include corticosteroids, such as prednisone, and non-steroidal anti-inflammatories (NSAIDs), such as Advil or Motrin. For the clinician, it is important to consider if the patient has any conditions of metabolic syndrome, as these fast-acting therapies are known to increase the risk of heart disease and stroke. The treatment approach may be altered if these conditions are present.
Dr. Barra plans to re-examine the CATCH data at a later time, to determine if metabolic syndrome and rheumatoid arthritis worsens or improves over time. In future research, she also hopes to discover some of the causes and mechanisms at play, to better understand why many patients with rheumatoid arthritis also have metabolic syndrome.