Search
Search
Simple device improves care after kidney transplantation
LONDON, ON – In a published study, a team from Lawson Health Research Institute has found that a simple device can reduce swelling after kidney transplantation. The geko™ device, manufactured by Sky Medical Technology Ltd and distributed in Canada by Trudell Healthcare Solutions Inc., is a muscle pump activator which significantly improves blood flow by stimulating the body’s ‘muscle pumps.’ Patients using the device following kidney transplantation experienced shorter hospital stays and reduced surgical site infections by nearly 60 per cent.
Kidney and simultaneous pancreas-kidney transplantations can significantly reduce mortality and improve the quality of life for patients with end stage renal disease. “After surgery, many of these organ recipients require a longer hospital stay due to delayed kidney function, infection, lack of mobility or edema,” says Dr. Alp Sener, Lawson Scientist and Transplant Surgeon in the Multi-Organ Transplant Program at London Health Sciences Centre (LHSC).
Edema is swelling caused by excess fluid trapped in the body’s tissues which can impact wound healing. The current standard of care for managing lower-limb edema and improving blood flow is thrombo-embolic-deterrent (“TED”) stockings used with compression devices. Sleeves pumped with air squeeze the lower legs to boost circulation. They can be uncomfortable to wear, and the large pump can inhibit early mobility and disrupt sleep after surgery.
In a randomized controlled clinical trial spanning two years, 221 transplant recipients at LHSC either wore the standard TED stocking and pump or the geko™ device for six days after surgery. Dr. Sener’s research team found that wearing the device increased urine output by 27 per cent and lowered weight gain by over a kilogram. With more urine produced and less fluid retention, patients experienced 31 per cent less swelling. The duration of costly hospitalization was shortened by over one day after kidney transplantation compared to the standard of care.
A 60 per cent reduction in wound infection rates was a striking observation. “Transplant patients are at a higher risk of infection due to the immunosuppressant medications needed after surgery,” explains Dr. Sener, who is also the President of the Urologic Society for Transplantation and Renal Surgery, a global organization affiliated with the American Urological Association. “Reducing infection means a much better outcome for the patient and considering that recent data shows wound infections can cost the health care system thousands of dollars per person, it’s a win-win situation.”
Some of the study participants wore pedometers to track their steps, and those using the geko™ device had improved mobility after surgery. The team suspects this may be due to reduced swelling which could improve ease and comfort when moving.
“The study results have been both surprising and exciting. Not only have we cut down wound infection rates but we have also seen a considerable improvement in the new organ’s function following transplantation. Patients report feeling more satisfied with the transplant process and are more mobile,” says Dr. Sener. The geko™ device is now being offered to patients at LHSC in recovery after receiving a new kidney.
Ruben Garcia, 68 years old, recently received a new kidney from his daughter, Ruby, who was a match as a living kidney donor. Following his surgery, Garcia found it difficult to get out of bed due to the pain and swelling, and the function of his new kidney was very low. “My surgeon explained in very simple terms that it was as if my new kidney wasn’t awake yet,” describes Garcia.
Dr. Sener recommended that Garcia use the geko™ device to help stimulate blood flow in a way that is similar to walking. Garcia was soon able to sit up on a chair and by the next day he was walking. “My kidney woke up and starting working again! I could feel the device working and it was comfortable to wear, almost like a massage for my legs. I’m very grateful for the care that I received.”
Dr. Sener adds that “using a muscle pump activator could be a game changer for other procedures like orthopedic implants where wound infection can have disastrous consequences or in surgeries where wound infections are more common such as in cancer and intestinal surgery.”
The geko™ device is non-invasive, self-adhering, battery-powered and recyclable. It generates neuromuscular electro-stimulation and unparalleled systemic blood flow that equates to 60 per cent of that achieved by walking. Pain-free muscle contraction compresses deep veins in the lower legs to create better blood flow in these vessels and return blood to the heart. It is particularly well suited to hospital settings as it portable and requires minimal training. For the indications for the use of the geko™ device, go to www.gekodevices.com.
“The results of the study provide further evidence that the geko™ device is an effective treatment option that can improve outcomes for patients and help them return home sooner, while reducing costs for the health-care system,” says George Baran, Executive Chairman of the Trudell Medical Group and a Director of Sky Medical.
-30-
DOWNLOADABLE MEDIA

Dr. Alp Sener, Lawson Scientist and Transplant Surgeon in the Multi-Organ Transplant Program at London Health Sciences Centre

The geko™ device being applied on the leg

The geko™ device
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Smart technology in the home effective for supporting mental health care, study finds
A research team from Lawson Health Research Institute has announced promising results from a one-of-a-kind demonstration study that evaluated the use of smart technologies in the home for people with severe mental illness.
“Our Smart Homes solution is for people who are having difficulty managing their everyday life and need a high level of care to maintain community living,” says Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and project lead for Smart Home Community Model Phase.
“We have strong initial evidence showing that technology and applications embedded in the lived environment are safe, secure and appropriate for use in health care.”
After prototyping this approach within a hospital setting through St. Joseph’s Health Care London, the research team outfitted affordable housing units at Canadian Mental Health Association (CMHA) Elgin-Middlesex and London and Middlesex Community Housing (LMCH) with smart home technology.
The team presented the full study results during a virtual event.
There were 13 participants as part of this project phase who had different living situations such as individual apartments, group homes or family homes. Anxiety, mood and psychotic disorders were the most common mental health diagnoses, with many also suffering from chronic pain that make the activities of daily life difficult.

Each study participant selected from a wide range of tools that would best meet their individual needs, with all but one participant selecting more than one tool. Devices such as smartphones and touch-screen monitors connect with applications to provide video-conferencing, questionnaires, and prompts and reminders based on the person’s care plan. They also had access to automated medication dispensers and smart health monitoring devices for tracking heart rate, activity and sleep.
“All of the data is viewable by both the client and health care provider, allowing for more seamless care and identification of issues earlier on,” adds Dr. Forchuk.
The study found that visits to a health or social service provider and the emergency department decreased, as did home visits from a provider. Telephone appointments increased and communication between the client and provider were enhanced. Almost 80 per cent of the participants felt that the technologies improved their health care overall.
Higher levels of community integration and a greater sense of independence were also reported, including a better ability to remain connected with friends and family during the pandemic. When medication dispensers were used, no medication doses were missed. Participants felt they were better able to track their own health and more motivated to lead healthier lives.
“The compliment of smart technology in our Supportive Independent Living Program has proven to improve the quality of life of participants by reducing use of emergency services and fostering learning opportunities for independent living skills to create a good quality of life,” says Nedrita Shemshedini, Manager of Supportive Independent Living at CMHA Elgin-Middlesex. “In a large-scale rollout, this model could improve wellbeing and empower persons to better manage their care.”
The research team hopes this work will help inform the integration of smart technology more fully into mental health care delivery. Laura Pearson, Executive Director at Ontario Peer Development Initiative, urges that “there is a need for key policies to be addressed and changed in order to support funding and access for technology at a system level for the purpose of mental health care.”
The community model phase of the Smart Homes project was generously funded by the Canada Mortgage and Housing Corporation (CMHC).
Smart technology in the home effective for supporting mental health care, study finds
LONDON, ON – A research team from Lawson Health Research Institute has announced promising results from a one-of-a-kind demonstration study that evaluated the use of smart technologies in the home for people with severe mental illness.
“Our Smart Homes solution is for people who are having difficulty managing their everyday life and need a high level of care to maintain community living,” says Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and project lead for Smart Home Community Model Phase. “We have strong initial evidence showing that technology and applications embedded in the lived environment are safe, secure and appropriate for use in health care.”
After prototyping this approach within a hospital setting through St. Joseph’s Health Care London, the research team outfitted affordable housing units at Canadian Mental Health Association (CMHA) Elgin-Middlesex and London and Middlesex Community Housing (LMCH) with smart home technology.
There were 13 participants as part of this project phase who had different living situations such as individual apartments, group homes or family homes. Anxiety, mood and psychotic disorders were the most common mental health diagnoses, with many also suffering from chronic pain that make the activities of daily life difficult.
“More and more, smart technologies like phone applications or virtual care are being used for mental health care. A smart home solution like the one we have tested could be considered a higher dose of technology, offered to clients with higher needs. The right dose for one may not work for another – the technological solutions used should vary depending on the individual,” explains Dr. Forchuk.
Each study participant selected from a wide range of tools that would best meet their individual needs, with all but one participant selecting more than one tool. Devices such as smartphones and touch-screen monitors connect with applications to provide video-conferencing, questionnaires, and prompts and reminders based on the person’s care plan. They also had access to automated medication dispensers and smart health monitoring devices for tracking heart rate, activity and sleep.
“All of the data is viewable by both the client and health care provider, allowing for more seamless care and identification of issues earlier on,” adds Dr. Forchuk.
The study found that visits to a health or social service provider and the emergency department decreased, as did home visits from a provider. Telephone appointments increased and communication between the client and provider were enhanced. Almost 80 per cent of the participants felt that the technologies improved their health care overall.
Higher levels of community integration and a greater sense of independence were also reported, including a better ability to remain connected with friends and family during the pandemic. When medication dispensers were used, no medication doses were missed. Participants felt they were better able to track their own health and more motivated to lead healthier lives.
“The compliment of smart technology in our Supportive Independent Living Program has proven to improve the quality of life of participants by reducing use of emergency services and fostering learning opportunities for independent living skills to create a good quality of life,” says Nedrita Shemshedini, Manager of Supportive Independent Living at CMHA Elgin-Middlesex. “In a large-scale rollout, this model could improve wellbeing and empower persons to better manage their care.”
The research team hopes this work will help inform the integration of smart technology more fully into mental health care delivery. Laura Pearson, Executive Director at Ontario Peer Development Initiative, urges that “there is a need for key policies to be addressed and changed in order to support funding and access for technology at a system level for the purpose of mental health care.”
The community model phase of the Smart Homes project was generously funded by the Canada Mortgage and Housing Corporation (CMHC).
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Top 12 research stories of 2022
As the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, our teams impact the lives of people in Ontario, Canada and around the globe with groundbreaking studies, world firsts and translational research that enhances care, health and wellbeing. Here are some of Lawson Health Research Institute’s top research highlights of 2022.
Researchers looking to better personalize treatment for PTSD

In a new study through Lawson and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from post-traumatic stress disorder (PTSD). Read more.
Virtual care associated with significant environmental and patient cost savings

A new study by researchers at ICES, Lawson and Western finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs. Read more.
Novel test that could easily diagnose blast injury created by local scientists

In a world first, researchers at Lawson and Defence Research and Development Canada have developed a breath test that could be used to diagnose repetitive blast injury – a mild traumatic brain injury resulting from pressure changes that occur during explosions. The device will soon go through clinical trials to validate its efficacy. Read more.
Local researchers using artificial intelligence to lead the way in bedside lung imaging
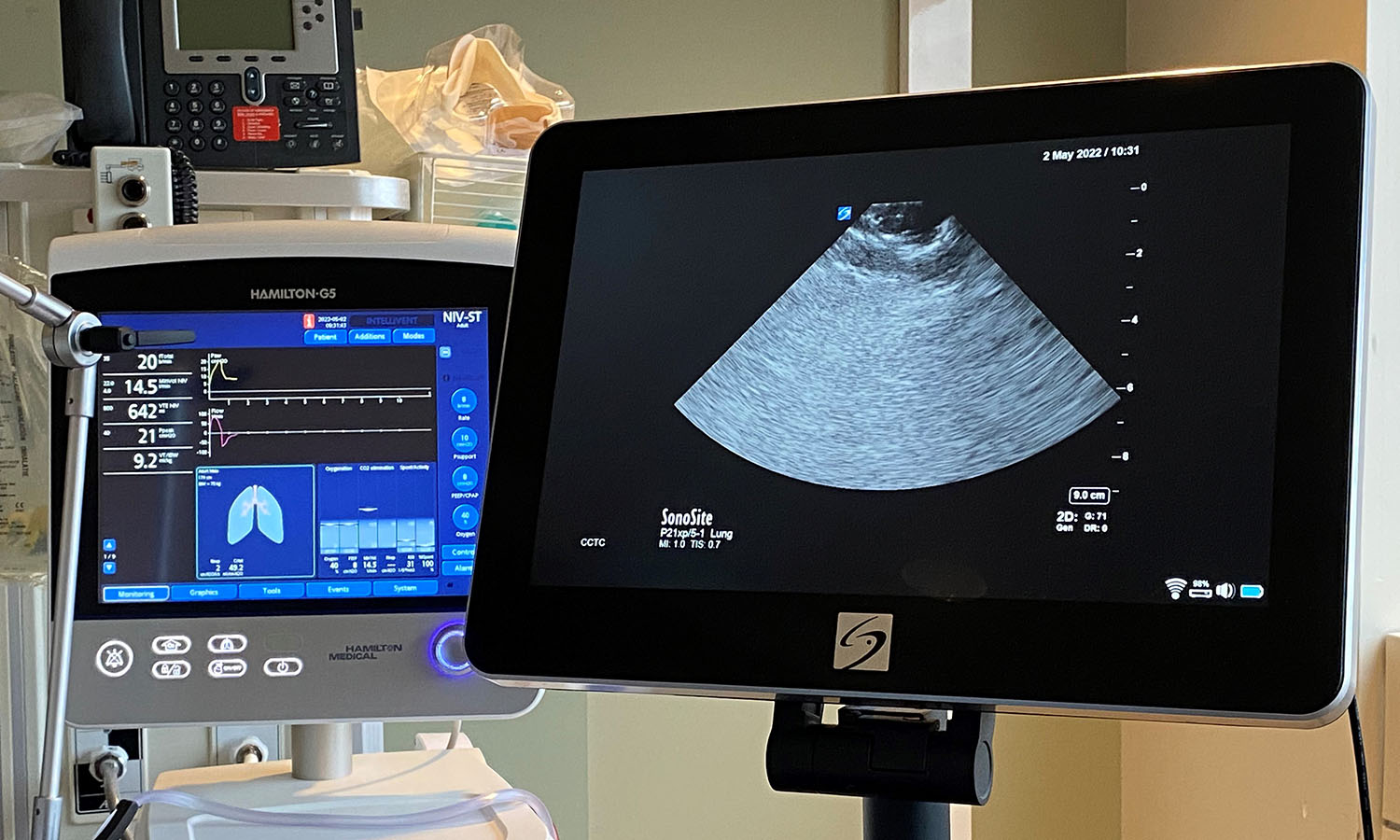
A team at Lawson is testing a new form of artificial intelligence (AI), paired with portable ultrasound machines, to image and identify lung concerns in real time, right at the beside of critically ill patients. Approximately 100 critical care patients at LHSC will be part of this study. Read more.
New tool shows promise in helping people manage traumatic brain injuries one pace at a time

A team at Lawson has developed a new app called MyBrainPacer™ which aims to better assist and treat those living with mild traumatic brain injuries (mTBI), including concussions. mTBI may come with lasting effects that can alter a person’s life. Although a person with a mTBI may appear fine on the outside, many have to pace their day-to-day activities in order to allow the time needed for the brain to properly heal. Much like point tracking used by dieters to monitor food choices, through MyBrainPacer™ App, users can assign values to tasks like driving, grocery shopping, screen use and exercise so they can plan and pace their daily activity. Read more.
Study shows a decline in Veterans' mental health throughout the pandemic

When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population. They found that more than half of Canadian Veterans reported a decline in their mental health. Read more.
Growing evidence that PSMA imaging improves prostate cancer detection
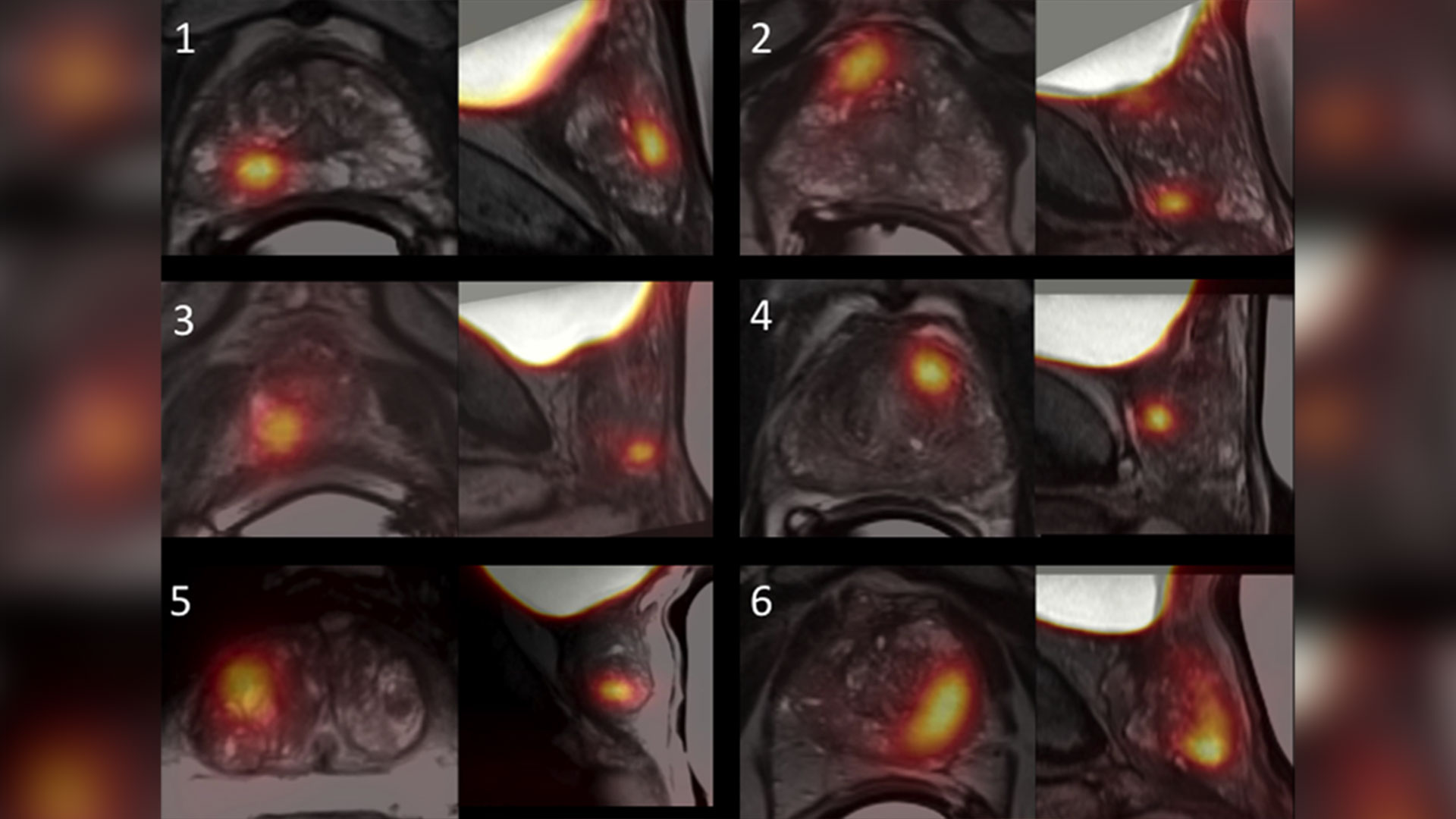
Scientists at Lawson are leading the way in using specialized imaging to detect prostate cancer – the fifth leading cause of cancer death in men around the world. Early evidence indicates that PSMA PET scans have changed how prostate cancer is being treated, but more work is underway to understand the impact of those treatment changes. Read more.
Leveraging virtual reality to manage pain in paediatric patients

A study underway through Lawson and Children’s Hospital at LHSC is using virtual reality (VR) to help paediatric patients during painful and distressing procedures. The study is focusing on paediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in paediatric cancer patients. Read more.
Team players: FMT and microbiome research could have widespread impact

There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system. FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis. Read more.
London researchers adapt MRI technology to image salt within the kidneys

Scientists at Lawson have adapted PET/MRI technology to accurately image salt within the kidneys of patients with kidney disease. Imaging salt within the kidneys has never been accurately accomplished in patients with kidney disease, but Dr. McIntyre and his team developed new technology and software that was adaptable to a PET/MRI machine at St. Joseph’s. Read more.
London researchers discover novel method to diagnose long COVID
Published in Molecular Medicine, researchers at Lawson have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition. Read more.
Largest trial ever done in hemodialysis care examines optimal dialysis temperature

Published in the Lancet findings from a large clinical trial through Lawson, ICES Western and Western University suggest that lowering dialysis temperatures does not lead to improved patient outcomes, despite previous studies suggesting otherwise. Read more.
To learn more about Lawson research studies, please visit our News and Media page
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca