Search
Search
About Lawson Research
Lawson Research Institute is discovery-driven and patient-focused
Excellent patient care stems from outstanding health research.
At Lawson Research Institute we are revolutionizing health care through discoveries that transform lives and communities.
Contact Lawson Research Work with Us Data Management EDI-B
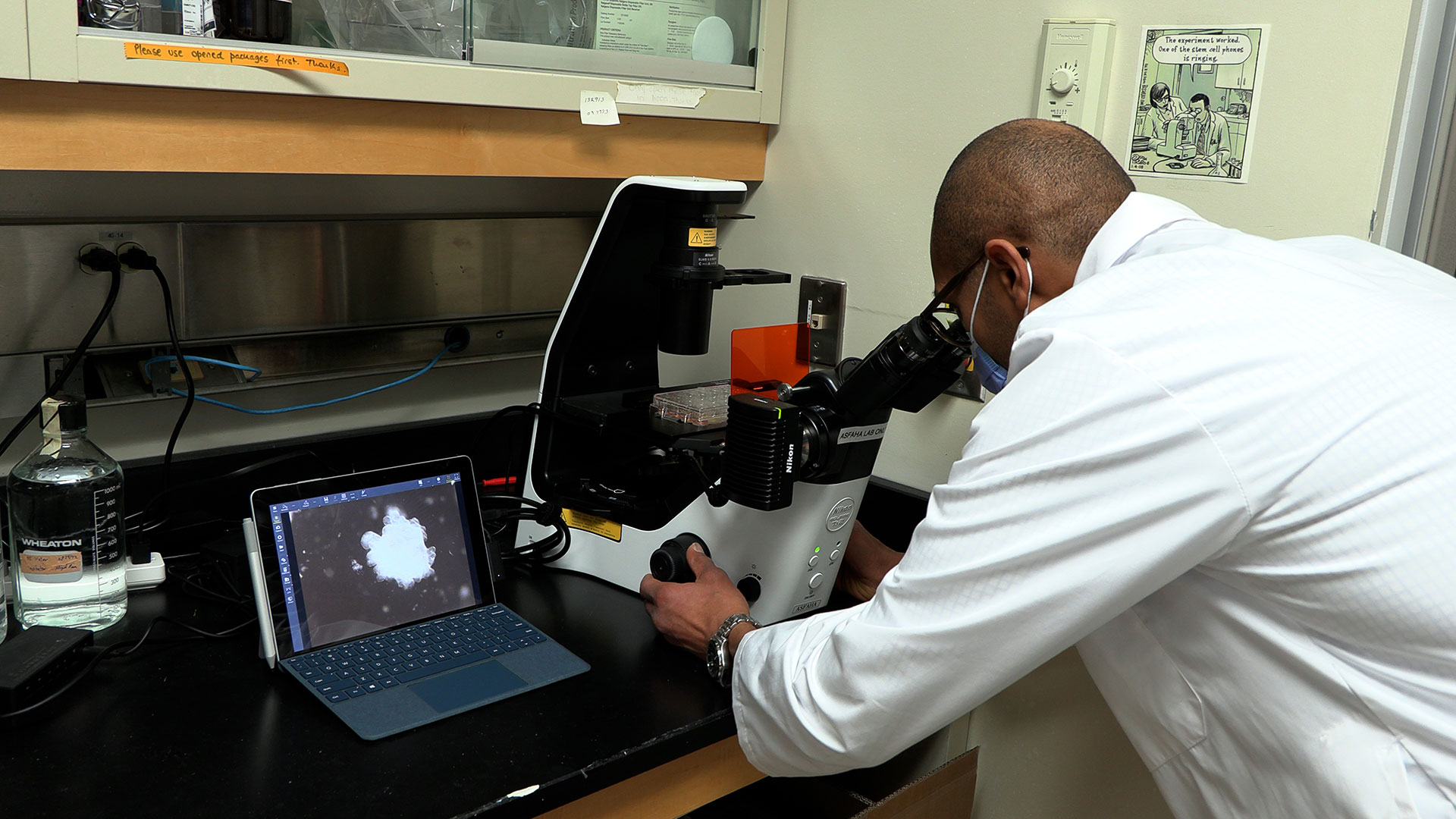
As the research arm of St. Joseph’s Health Care London, Lawson is one of Canada’s premier health research institutes. For more than 40 years, a culture of curiosity and innovation has propelled Lawson to become a renowned leader in research that is making a difference in patient lives here and around the globe:
- We conducted the world’s first non-invasive images measuring blood flow to the brain and were the first research site in Canada with PET/MRI and PET/CT scanners – the latest version now diagnosing complex conditions better and faster than any other in the country.
- We’re international pioneers in the causes and early treatment of dementia.
- Innovators in probiotics for a healthy immune system, diabetes care and surgical interventions.
- Trailblazers in mental health research, and in understanding strokes, brain injury and rehabilitation.
This is Lawson.
We’re driven by the conviction that patient care improves when research includes everyone, everywhere.
That’s why Lawson’s 200 researchers and associate scientists – along with hundreds of other staff members, physicians, students, patients, donors, and academic and funding partners – are laser-focused on embedding research into the work of improving health for all.
Lawson Research Institute leads.
Read more to discover where it can lead you.
Academic Affiliation
Lawson Research Institute of St. Joseph’s Health Care London is proud to be affiliated with Western University. Through shared faculty appointments, collaborative research programs and clinical education, we work together to advance health research and improve patient care. St. Joseph’s plays a key role in training the next generation of health professionals and supporting discoveries that have impact for health care locally and beyond.
Ali Bateman
Ali Bateman, MD
Assistant Professor, Schulich School of Medicine and Dentistry
Acquired and Traumatic Brain Injury; Spinal Cord Injury
Dr. Ali Bateman is a physiatrist at Parkwood Institute and an Assistant Professor in the Department of Physical Medicine and Rehabilitation Schulich School of Medicine & Dentistry at Western University. She is also an Associate Scientist at Lawson Health Research Institute, and the Quality Improvement Lead in the Department of Physical Medicine & Rehabilitation.
Dr. Bateman completed her medical degree and residency training at Western University, and is currently completing a master’s degree in Quality Improvement and Patient Safety through the Institute of Health Policy, Management, and Evaluation at the University of Toronto. She is also certified by the Canadian Society of Clinical Neurophysiologists and holds the designation of CSCN Diplomate (EMG). As a consultant physiatrist, Dr. Bateman provides care in acquired brain injury and spinal cord injury rehabilitation programs and the electrodiagnostic laboratory at Parkwood Institute.
Her research interests centre on quality improvement, patient safety, and knowledge translation with the aim of achieving best practices so that all persons with spinal cord and/or brain injury receive the best quality care.

An innovative year: Top 12 research stories of 2023
It’s been another year of transformational research at Lawson Health Research Institute. Our teams have published groundbreaking findings and launched new studies that will have a profound impact on patient care.
The following are 12 highlights of research and innovation from across London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s). From trialing new cancer treatments to advancing understanding of mental health, our research teams have achieved a number of important milestones.

1. New study suggests blood plasma proteins hold answers to better understanding long COVID
Lawson researchers continued to advance understanding of COVID-19 this past year. In one study, researchers found that unique patterns in blood plasma proteins of patients with suspected long COVID could act as a drug target to improve patient outcomes. Read more.

2. New study finds exercise, cognitive training combo boosts mental sharpness in seniors
A study from Lawson and Western University found that a combination of computerized cognitive training and aerobic-resistance exercises can improve functions like memory, attention, recognition and orientation in older adults with mild cognitive impairment. The results suggest a new way to address declining mental sharpness in older adults. Read more.

3. $7.55 million in funding to take LHSC-developed technology global
Technology to diagnose rare genetic disorders developed by researchers at Lawson and LHSC will be going global thanks to $7.55 million in funding from Genome Canada grant and Illumina Inc. The new artificial intelligence-led technology could allow rare diseases to be diagnosed with a simple blood test. Read more.
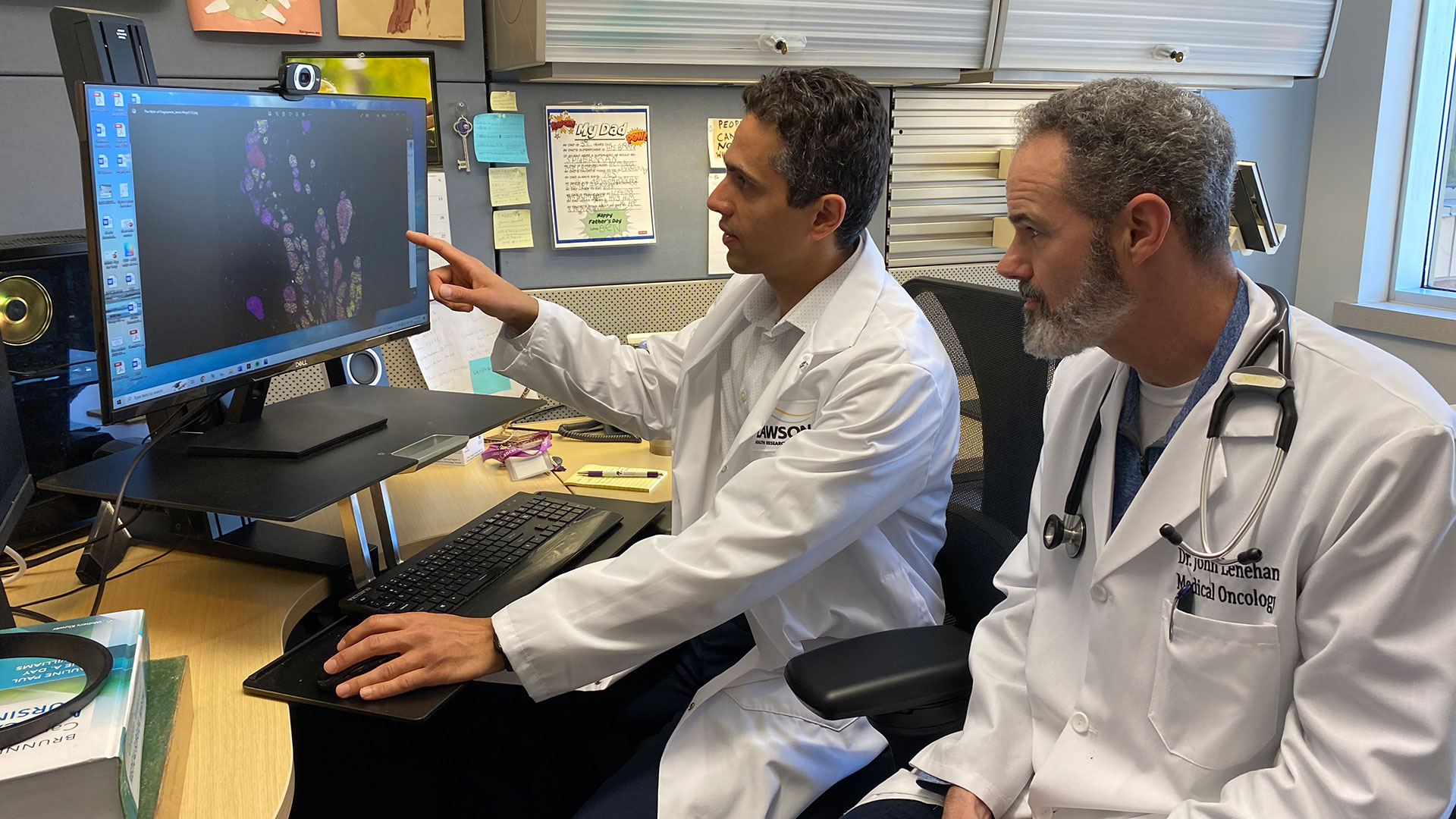
4. Fecal transplants show promise in improving melanoma treatment
Fecal microbiota transplants (FMT) from healthy donors are safe and could improve response to immunotherapy in patients with advanced melanoma, according to results from a world-first multi-centre clinical trial led by Lawson researchers. Read more.

5. New study shows technology could play an important role in mental health support
A team of Lawson researchers found that the use of ‘smart home’ technology like touch screen devices, activity trackers, weigh scales and medication dispensers may lead to better outcomes for those living with both mental health and physical disorders. The study found that participants using the technology started logging more exercise, making healthier food choices and not missing medication doses. Read more.

6. Canadian children’s hospital visits for suicidal thoughts, self-poisoning and self-harm up during pandemic, study finds
A national study with Lawson researchers found that during the first two years of the COVID-19 pandemic, adolescent emergency department (ED) visits and hospitalizations for suicidal thoughts, self-harm and self-poisoning increased across Canada, with the greatest increase occurring among adolescent girls. Read more.

7. St. Joseph’s to become Canada’s first centre of excellence in molecular imaging and theranostics
A partnership between Lawson, St. Joseph’s Health Care London and GE HealthCare will create Canada’s first centre of excellence in molecular imaging and theranostics at St. Joseph’s. The centre will focus on using precision diagnostic imaging and targeted therapy to advance personalized treatment of cancer and other diseases. Read more.

8. Researchers investigate a new method of sedation for paediatric patients
Intravenous sedatives are normally used to sedate critically ill children. However, they can contribute to a complication called delirium, which includes symptoms of confusion, disorientation, agitation, excessive drowsiness and poor attention. To improve outcomes, scientists at Children’s Health Research Institute (a program of Lawson), Sunnybrook Research Institute and The Hospital for Sick Children (SickKids) are collaborating on a pilot study to understand whether inhaled sedation could be a better alternative to keep critically ill children sedated and comfortable. Read more.
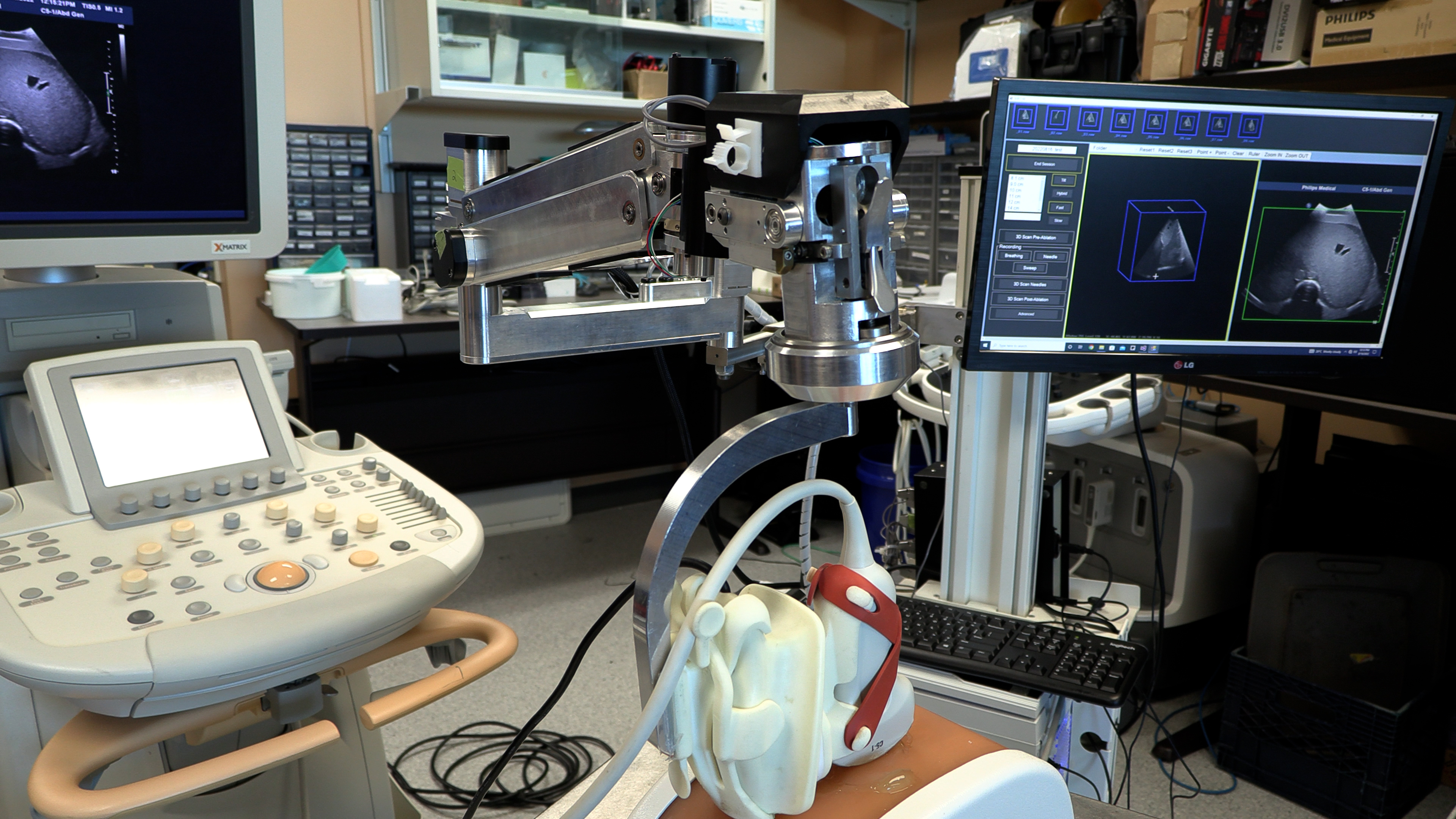
9. New robotic 3D ultrasound may improve accuracy of liver cancer ablation therapy
A technique that turns a normal ultrasound into a 3D image is showing promise in making thermal ablation for liver cancer treatment more accurate in a study from Lawson and Western University. Thermal ablation – using heat to destroy a cancerous tumour – can have fewer complications and a shorter recovery time than surgery. Read more.

10. Assessing neurofeedback in stroke survivors
Functional near-infrared spectroscopy (fNIRS) is used to detect changes in brain oxygen levels using light, but more recently it has also been used to develop brain-computer interfaces – allowing patients with brain injuries to control a device with their thoughts. Researchers at Lawson launched a new study to assess whether fNIRS can be used to improve patient outcomes during stroke rehabilitation. Read more.
11. Specific type of inflammation may be linked to risk of colorectal cancer
A preclinical study found that a specific type of inflammation may be linked to an increased risk of colorectal cancer. Previously, the degree of inflammation caused by illnesses like colitis, Crohn’s disease and other forms of inflammatory bowel disease were shown to be an important indicator of the development of colorectal cancer. However, this new study found the type of inflammation, rather than the severity and duration, may be more important in determining cancer risk. Read more.

12. New study examining if probiotics can improve outcomes in knee replacement surgeries
Lawson researchers launched a study to assess whether daily probiotics can improve outcomes in patients undergoing a total knee replacement surgery. Of the more than 70,000 knee replacement surgeries in Canada each year, nearly 10 per cent of patients experience complications. With patients who are considered healthy likely to have better outcomes, the research team is interested in improving the gut microbiome as a way to support patients’ overall health. Read more.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
