Search
Search
Study casts doubt on clinical significance of gadolinium brain deposits
A new study from Lawson Health Research Institute and the Institute for Clinical Evaluative Sciences (ICES) has cast doubt on the clinical significance of brain deposits of gadolinium (a chemical contrast agent commonly used to enhance MRI imaging).
In 2015, the US Food and Drug Administration raised safety concerns over reports of retained gadolinium in the brain for patients undergoing four or more gadolinium-enhanced MRIs. The FDA launched an inquiry at the time, stating that “it is unknown whether these gadolinium deposits are harmful.” Pending further investigation, the FDA suggested limiting the use of gadolinium-based contrast agents (GBCAs) to circumstances where contrast information is clinically necessary, and to evaluate the need for repetitive GBCA MRIs based on treatment protocols.
Studies since that time have shown deposits of gadolinium may be found long after they are administered. They tend to concentrate in the globus pallidi, a region of the brain that can cause parkinsonian symptoms if it is damaged. Parkinson’s disease is an example of a specific brain disorder that is commonly associated with parkinsonian symptoms.
“Given the concern around possible neurotoxicity of gadolinium, and because these deposits were found in the globus pallidi region of the brain, we wanted to see if people exposed to gadolinium MRIs have higher rates of subsequent parkinsonism,” says Dr. Blayne Welk, the lead author of the study who is an adjunct scientist with ICES Western and Lawson.
To test a possible link between GBCAs and parkinsonism, Welk and his team examined anonymized health care records for 246,557 patients in Ontario over the age of 66 who underwent an initial MRI in a 10-year period between 2003 and 2013. They excluded patients whose initial MRI was of the brain or spinal cord and those with prior parkinsonism or neurosurgery. Comparing patients who were exposed to gadolinium-enhanced MRIs with patients whose MRIs did not include gadolinium enhancement, they looked for differences in rates of future parkinsonism symptoms or treatment.
They found that the rates of parkinsonism for exposed vs non-exposed patients were virtually identical, at 1.2 per cent. These findings indicate that there is no increased risk for parkinsonism associated with the use of gadolinium in MRIs.
However, the researchers caution that this study does not clear up all the worries about gadolinium, since they investigated only its connection to parkinsonism.
“While these findings should be reassuring for patients and their care providers that gadolinium exposure does not appear to be associated with higher risk of developing parkinsonism symptoms, there have been other reports of nonspecific neurologic symptoms including pain and cognitive changes associated with prior gadolinium exposure which do require further study,” comments Dr. Welk.
The researchers also note that gadolinium may have different effects in younger patients (who were not included in this study), or in those with neurologic diseases (who may have been excluded based on the types of MRIs included in this study).
“Association between Gadolinium contrast exposure and the risk of parkinsonism” was published on July 5, 2016 in the journal JAMA.
Author block: Blayne Welk, Eric McArthur, Sarah A. Morrow, Penny MacDonald, Jade Hayward, Andrew Leung, Andrea Lum.
Study offers hope for hard-to-treat type 2 diabetes
A landmark international study involving patients and researchers at St. Joseph’s Health Care London shows automated insulin pump delivery can be ‘life-changing’ for people with type 2 diabetes
Lisa Mercer had tried just about everything to regulate the ups and downs of her blood sugars, from a strict diet to medication to four-a-day-day insulin shots.
But her busy life with type 2 diabetes finally started to feel better when she enrolled in a clinical trial at St. Joseph’s Health Care London to test the effectiveness of a system that combined glucose monitoring with an automated insulin pump.
“It was life-changing for me. I was diagnosed with type 2 diabetes 25 years ago and my blood sugars have always been all over the map. I felt sort of helpless. I said yes to this clinical trial because I hoped it would return some normalcy to my life,” she says. Now that study, with results newly published in the prestigious New England Journal of Medicine, is being heralded as a big step forward for patients with hard-to-treat type 2 diabetes.
“This is an exciting finding because it shows we can improve patients’ blood sugars and hopefully prevent long-term negative consequences of high sugars while at the same time making it easier for patients to manage the disease,” says Dr. Tamara Spaic, Medical Director of St. Joseph’s Diabetes Education Centre and the lead Canadian researcher for the multi-site international study based at the Jaeb Center for Health Research in Tampa, Fla.
Study participants were placed either in a group testing the effectiveness of a new system called Control IQ+ or a control group continuing their existing diabetes management regimen.
The intervention group wore glucose monitors that electronically talked with high-tech pumps that delivered insulin – automatically, in the right dose and at the right time – with minimal patient input.
While the device was approved about five years ago for people with type 1 diabetes, this is the first examination of its effectiveness managing the complexities of type 2 diabetes.
“The biggest burden in diabetes control is that it’s 24/7 vigilance: did I eat or not; what did I eat and how much; did I exercise; do I need to wake up for an insulin shot in the middle of the night? This system largely removes those variables to bring blood sugars to target levels,” says Spaic, who is also a Lawson Research Institute scientist and professor of endocrinology and metabolism at Western University’s Schulich School of Medicine & Dentistry.
“What surprised us was that this worked so well across all populations regardless of duration of the disease, amount of insulin needed, whether they used other medications or not, whether they were tech-savvy or not. It worked for everyone regardless of their ethnicity, socioeconomics, and whether they were male or female, old or young,” she adds.
Researchers even asked participants in the intervention group to skip insulin with meals on occasion – generally a no-no in the highly regimented life of someone with insulin-managed diabetes – and the automated system responded appropriately and quickly to adjust blood sugars.
Mercer found improvement within a couple of weeks: “Before the pump, I felt awful. When my sugars were too low, I got the shakes, I had trouble communicating and thinking clearly and I got extremely tired. When my sugars were too high, I was exhausted. It dominated every day and was tough on my job as a police officer. Now I feel better. I feel more in control.
“Is it perfect? No. But my sugars are stable and consistent more often than not.”
Not yet approved in Canada
In February, the US Food and Drug Administration cleared the use of the Control IQ+ system in adults with type 2 diabetes – approval that also meant the expense could be covered through health insurance.
However, it has not yet been brought to Health Canada regulators for approval, Spaic says.
Even so, several of her patients, including Foster, decided to continue using the system after the 13-week trial, paying out-of-pocket or through private insurance.
Spaic and St. Joseph’s colleagues, endocrinologist Dr. Selina Liu and nurse coordinator Marsha Driscoll, were extensively involved in the design of the study, recruiting and monitoring participants and reporting results.
Diabetes type 2 usually develops in adulthood and is a condition in which body cannot make enough insulin or does not properly use the insulin it makes to regulate the amount of glucose (sugar) in the blood.
While most people with type 2 diabetes can control their blood sugars through lifestyle changes or with new treatments such as non-insulin glucose-lowering medications, the sub-set of North Americans who require insulin still numbers in the millions.
THE STUDY:
What: 13-week, large-scale clinical trial to test the effectiveness of a system combining automated insulin delivery with continuous glucose monitoring for people with type 2 diabetes.
Who: 319 study participants – including 13 at Lawson Research Institute of St. Joseph’s Health Care London – all needing multiple daily insulin doses. Age range 19 to 87, from 21 centres across the U.S. and Canada. Study led by Jaeb Centre for Health Research in Tampa, Fla., and funded by Tandem Diabetes Care, which also provided the automated insulin-delivery systems
How: Two-thirds of patients received an automated insulin pump, continuous glucose monitor and transmitter to track and automatically administer insulin to regulate their blood sugars. A control group continued their existing insulin-delivery method and also received glucose monitors.
Results: The intervention group had more stable blood sugar levels – with 3.4 more hours per day in the target glucose range – than the control group. Use of automated insulin devices was successful and safe even for patients without previous experience with an insulin pump
Why it matters: Automated insulin delivery can help insulin-dependent patients manage their type 2 diabetes better than before. Better management means improved quality of life and may result in fewer diabetes complications such as heart disease and damage to the eyes, kidneys and nerves.
Study testing benefit of antibodies from people recovered from COVID-19 on severe cases of infection
LONDON, ON – Researchers at Lawson Health Research Institute are taking part in a large, multi-centre study examining the use of convalescent plasma transfusions from people who have recovered from COVID-19 as a possible treatment for infected patients.
When a person is infected with a virus, their immune system produces protein antibodies, specific to that virus, that help the body fight the infection. These antibodies stay in the bloodstream after the person has recovered, and provide a degree of long-term immunity. Convalescent plasma is a term that describes plasma from a person who has recovered from illness. The hope is that naturally derived antibodies for COVID-19 will help fight serious infection in other individuals.
The CONCOR-1 Trial, led by Canadian researchers, will recruit 1,200 participants from Canada and New York. Researchers are collecting blood plasma from recovered COVID-19 patients and transfusing it into seriously ill patients. Measurable outcomes include the rate of intubation and mortality rate after 30 days of enrollment in the trial.
Convalescent plasma donation is being coordinated through Canadian Blood Services. For this study, they are currently collecting plasma from eligible donors under the age of 67 who have fully recovered from COVID-19 and have been symptom free for at least 28 days. Those who are interested in donating can find more information on the Canadian Blood Services website.
Dr. Ziad Solh, Lawson Associate Scientist, and Hematologist and Transfusion Medicine Specialist at London Health Sciences Centre explains, “this is an experiment; we don’t yet know if this treatment will show benefit, but it does show promise as similar treatments have had some success in studies of other viral infections such as SARS.”
Trial participants must be over 16 years of age, requiring oxygen, have been sick for less than 12 days, and their plasma must be compatible with donor plasma.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study validates methods for tracking prevalence and service use of people who experience homelessness
A new population-based retrospective validation study, using ICES data collected between 2007 and 2014 in Ontario, has found that health records can be used to track service use as well as the needs of individuals experiencing homelessness. Researchers found that the algorithms tested were able to accurately identify up to 35 per cent of individuals who experience homelessness in a given year.
The best performing algorithm estimated a large increase in homelessness prevalence between 2007 and 2016, with approximately one in 200 adults in Ontario experiencing homelessness in 2016.
“We do not know how many people experience homelessness yearly in Ontario, or in the country as a whole. Current methods rely on shelter data, or large point-in-time counts that require large investments, and are only done in specific communities,” explains Lucie Richard, Lawson researcher and lead author of the study. “Also, not all people who are homeless use shelters. This approach gives us an alternative that can include a wide range of communities and different types of homelessness over time.”
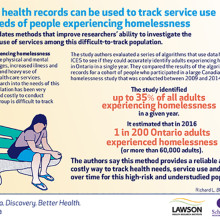
While numerous computer algorithms are already used to analyze administrative databases and identify disease populations to measure the burden of chronic diseases in Canada, this study, conducted by researchers at Lawson Health Research Institute and Western University, is one of the first to validate and track a social determinant of health with good accuracy.
People who experience homelessness often face mental and physical health challenges, have an increased risk of illness and death, and are among the highest users of emergency and other health care services. Homelessness is an important health issue for Canadians.
This ability to track individuals experiencing homelessness over time using administrative databases provides inexpensive, long-term monitoring, which will inform efforts to improve housing and health status in the community and across the country. Researchers and health care providers can now track health status and health care usage of individuals experiencing homelessness.
Understanding how many people experience homelessness and what demographics correlate with homelessness will allow for better service planning, and providers will have the information needed to more appropriately meet the needs of this vulnerable population.
The study, “Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada” is published in BMJ Open.
Study validates methods for tracking prevalence and service use of people who experience homelessness
LONDON, ON – A new population-based retrospective validation study, using ICES data collected between 2007 and 2014 in Ontario, has found that health records can be used to track service use as well as the needs of individuals experiencing homelessness. Researchers found that the algorithms tested were able to accurately identify up to 35 per cent of individuals who experience homelessness in a given year.
The best performing algorithm estimated a large increase in homelessness prevalence between 2007 and 2016, with approximately one in 200 adults in Ontario experiencing homelessness in 2016.
“We do not know how many people experience homelessness yearly in Ontario, or in the country as a whole. Current methods rely on shelter data, or large point-in-time counts that require large investments, and are only done in specific communities,” explains Lucie Richard, Lawson researcher and lead author of the study. “Also, not all people who are homeless use shelters. This approach gives us an alternative that can include a wide range of communities and different types of homelessness over time.”
While numerous computer algorithms are already used to analyze administrative databases and identify disease populations to measure the burden of chronic diseases in Canada, this study, conducted by researchers at Lawson Health Research Institute and Western University, is one of the first to validate and track a social determinant of health with good accuracy.
People who experience homelessness often face mental and physical health challenges, have an increased risk of illness and death, and are among the highest users of emergency and other health care services. Homelessness is an important health issue for Canadians.
This ability to track individuals experiencing homelessness over time using administrative databases provides inexpensive, long-term monitoring, which will inform efforts to improve housing and health status in the community and across the country. Researchers and health care providers can now track health status and health care usage of individuals experiencing homelessness.
Understanding how many people experience homelessness and what demographics correlate with homelessness will allow for better service planning, and providers will have the information needed to more appropriately meet the needs of this vulnerable population.
The study, “Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada” is published in BMJ Open.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western University’s Faculty of Health Sciences (FHS) is committed to bettering the human condition through outstanding training of health professionals, the education of students in the fundamentals of health, disability, and sport, and through the actions of our graduates who integrate the art and science of their disciplines.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca


