Search
Search
Café Scientifique: The invisible world inside us
The human microbiome is a wonder of nature, with trillions of microbes calling our body home. They live in our gut and many other places throughout our body. They are involved in virtually every aspect of how we function and we are learning that they are essential to staying healthy. An unhealthy microbiome has been linked to many diseases from allergies to cancer and even mental health.
Most people out there have heard about probiotics and fermented foods, and chances are you’re trying to get more of them in your diet. Drinking kombucha or eating yogurt, anyone?
On November 27, 2019, Lawson Health Research Institute held the latest in its Café Scientifique event series, "The invisible world inside us: Exploring the human microbiome.”
The panel of researchers helped to unravel the mysteries about the micirobiome and how we are using that knowledge to improve health and health care. They also busted some myths and shared the important facts when it comes to probiotics, prebiotics and the microbiome.
Watch their talks:
Researchers:
Probiotics and Prebiotics - Look beyond the fake news
Dr. Gregor Reid, Lawson Scientist and Professor of Microbiology & Immunology and Surgery at Western University.
Time stamp: 10:02
Fecal Transplants: What does this crap have to do with me?
Dr. Michael Silverman, Lawson Associate Scientist, Chair of Infectious Diseases, Schulich School of Medicine & Dentistry at Western University and Chief of Infectious Diseases for St. Joseph’s Health Care London and London Health Sciences Centre.
Time stamp: 31:48
Does eating bacteria make sense?
Dr. Jeremy Burton, Lawson Scientist and Assistant Professor of Surgery (Urology) and Microbiology & Immunology at Western University.
Time stamp: 55:02
See the event photos on Facebook.
DocTalks - Kidney Stones: From Ancient Times to Modern Practice and Prevention

Kidney Stones: From Ancient Times to Modern Practice and Prevention
Where: Shuttleworth Auditorium (Cheapside entrance)
Dr. John Denstedt is a surgeon at St. Joseph’s Hospital and professor at Western University’s Schulich School of Medicine & Dentistry. He is also the former Chair/Chief of the Department of Surgery and a world renowned leader in the field of urology. Dr. Denstedt will discuss how treatments for kidney stones have evolved over time, including current prevention strategies and how new research is unlocking new possibilities for the future.
Registration opens February 7.
DocTalks is a series of community health discussions featuring leading physicians and researchers at St. Joseph’s Health Care London. Learn from the experts how St. Joseph’s is tackling the pressing health issues of our time and why it matters to you and your family.
DocTalks is a joint initiative presented by St. Joseph’s Health Care London and St. Joseph’s Health Care Foundation.
Growing Tissues in the Lab
When challenged by surgeons to find better treatments for difficult-to-manage connective tissue diseases, Dr. David O’Gorman gladly accepted.
Dr. O’Gorman is a Molecular Biologist and Lawson Scientist based at St. Joseph’s Hospital, a part of St. Joseph’s Health Care London. His research focuses on understanding normal and abnormal connective tissue repair. He collaborates with researchers and clinicians working in many different disciplines, including those specializing in reconstructive surgery, orthopedics and urology.
Surgical reconstructions can be hampered by a lack of graft tissue, or graft tissue of insufficient quality, making it difficult to achieve optimal outcomes for the patients.
An example is a condition called urethral stricture disease (urethral scarring). This condition occurs in males and typically causes symptoms such as frequent and urgent urination, and slow urinary stream. In extreme cases, it can cause urinary tract infections, permanent bladder dysfunction and renal failure. Recurrence rates after minimally invasive treatments are high, and so many urologists recommend open surgical approaches.
Surgeons can use the patient’s own tissues to reconstruct the urethra after stricture removal. This tissue is normally sourced from the buccal cavity in the mouth but taking large tissue grafts can result in complications. In cases where buccal grafts have been used for previous reconstructions, there may not be enough intact tissue left.
Dr. O’Gorman sees a solution in growing sheets of human buccal tissues in the lab.
“We are currently using buccal graft trimmings as a source of cells, culturing them in a 3D environment and expanding them to create tissues of suitable size, density and elasticity.”
The patient’s own cells are used to generate a tissue graft for urethral reconstruction. While several research groups have developed this approach in the past, few have attempted to translate their models for clinical use.
“Our immediate goal is to provide proof of principle – that we can consistently generate grafts of suitable size and functional characteristics,” explains Dr. O’Gorman, “In the future, we could be providing bioengineered graft tissues for reconstructive surgeries here in London.”
Bioengineered human tissues can also be used as ‘mimetics’ – replications of human tissues – to study diseases, especially those difficult to model using routine laboratory methods.
Instead of a using a growth media or sterile plastic dishes, 3D cell culture is achieved by embedding cells in a matrix of proteins and other molecules normally found in those tissues. In this environment, gene expression and growth is more similar to cells of connective tissues in the body being replicated.
Dupuytren’s disease (or Dupuytren’s Contracture) affects the palmar fascia in the hand, a connective tissue beneath the skin that extends from the base of the palm into the fingers. This disease can be understood as a type of excessive scarring, where normal tissue repair processes have gone awry and dense scar tissue forms, typically causing permanent palm or finger flexion that restricts hand function.
This condition is surprisingly common and may affect more than one million people in Canada. While there are surgical treatment options available, none consistently prevent this disease from recurring in at least a third of patients.
“Due to its high recurrence rate after treatment, Dupuytren’s disease is currently considered incurable. Our challenge is to understand it well enough to develop truly effective treatments,” says Dr. O’Gorman.
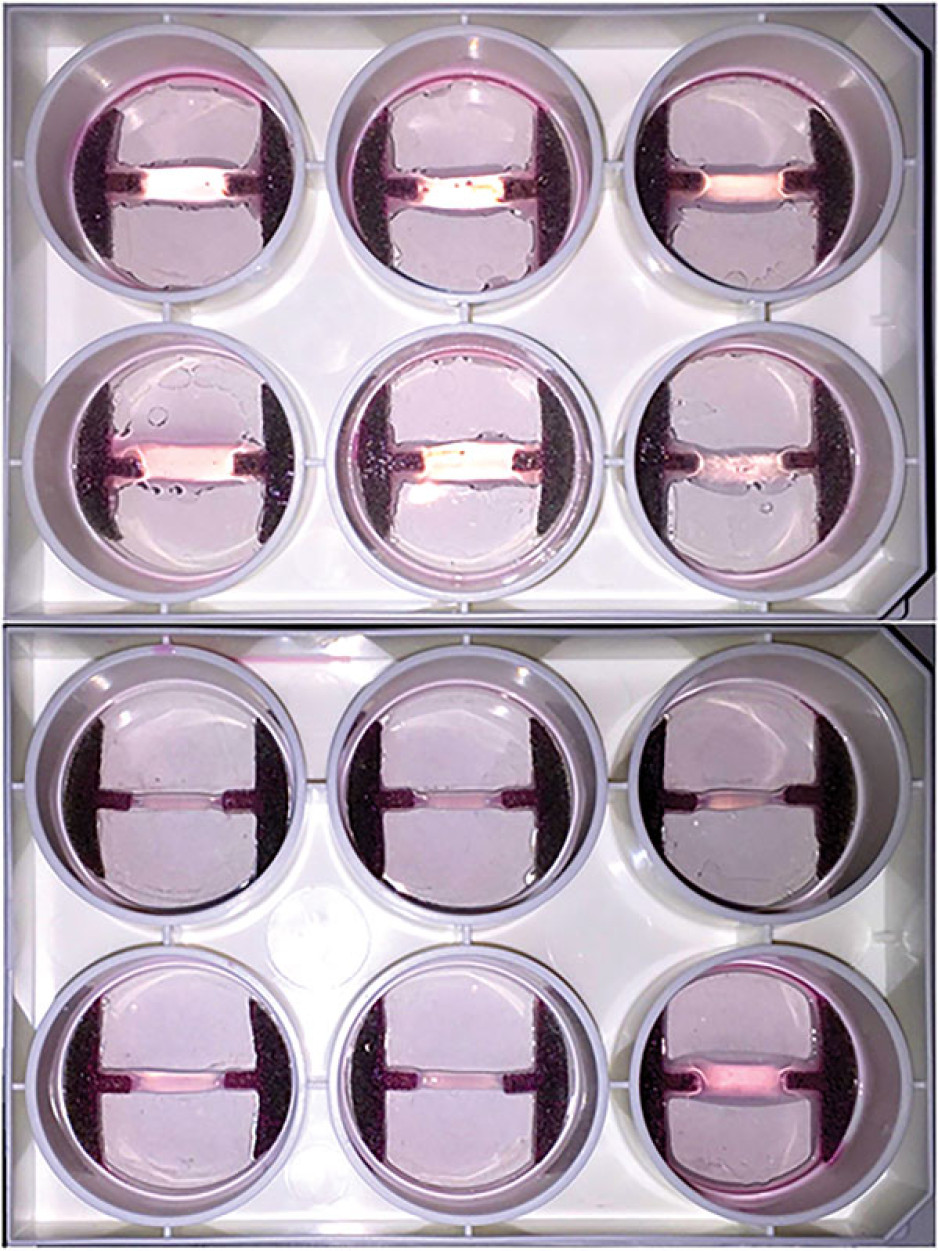
Human hands have unique characteristics not found in other species, making animal models impractical. Instead, Dr. O’Gorman’s team extracts cells from the diseased palmar fascia of patients undergoing hand surgeries and bioengineers them into palmar fascia ‘contractures’ in the lab.
“Since the cells from a single palmar fascia sample can be used to grow dozens of little contractures, we can test many different treatments simultaneously to see what works best for each patient.”
This approach may also allow them to determine if Dupuytren’s disease is truly one disease, or a group of similar diseases that cause palm and finger contractures.
“Often, Dupuytren’s disease is clearly heritable, but some individuals have no family history of it and develop apparently sporadic disease,” notes Dr. O’Gorman. “We want to determine if these are truly the same disease at the molecular level.”
Another major cause of abnormal connective tissue repair is infection, and tissue mimetics can play a role here, too. While rare, infections of artificial joint replacements are particularly devastating for patients, as they typically require readmission to hospital to remove the infected joint, weeks of antibiotic-based treatment, and an additional surgery to replace the artificial joint.
In addition to the associated pain and suffering, these procedures are technically challenging and costly to our health care system.
Artificial shoulder joint infections are most frequently caused by the microorganism Cutibacterium acnes (C. acnes). C. acnes infections disrupt normal tissue repair processes after surgery, cause shoulder tissues to die and promote loosening of the artificial joint. These infections are difficult to diagnose, and there is a lack of reproducible
models in which to study them. Dr O’Gorman’s team has set out to create the first human Shoulder-Joint Implant Mimetic (S-JIM) of C. acnes infection.
“While S-JIMs are more complex, they are 3D in vitro cell culture systems designed to mimic human tissues, like those that we use for studying Dupuytren’s disease.”
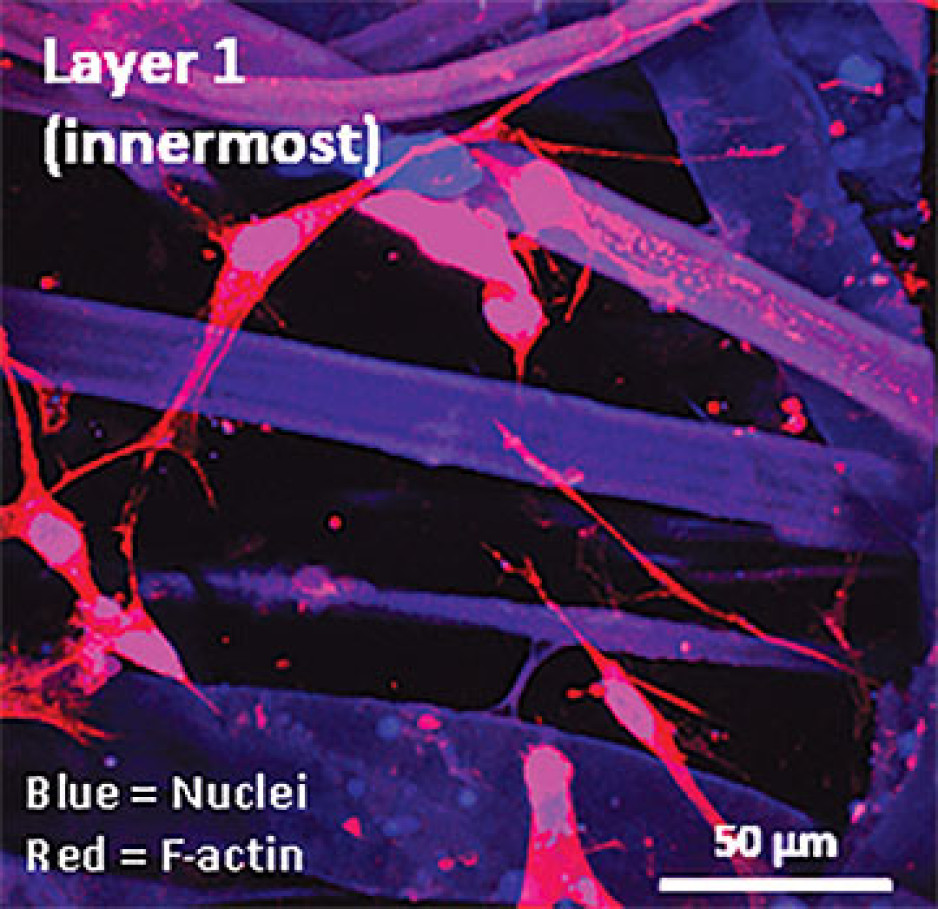
S-JIMs include layers of artificial human tissue, wrapped around cores of titanium alloy or cobalt chrome, the metals used to create artificial joints. They are co-cultured with C. acnes under low oxygen conditions similar to those that normally occur around artificial shoulder joints.
“We are bioengineering simple 3D cell cultures to more closely mimic the complexity of human tissues, with blood supply, nerves and interactions with other cells.” – Dr. David O’Gorman
Studying the connective tissue layers close to the infection allows researchers to investigate processes that promote infection, such as the formation of a biofilm that harbours and protects the bacteria from the body’s immune system. They are also able to test whether novel treatments can disrupt biofilm formation and increase the effectiveness of antibiotics.
Dr. O’Gorman predicts that in the future, medical researchers will routinely use bioengineered 3D human tissue and organ mimetics to accelerate our understanding of disease.
“The technology is in its infancy, but the potential for using bioengineered human tissues for surgical reconstructions or as disease models is huge. At Lawson, we’re ready to take on health care challenges and build on innovative approaches to improve the quality of life for patients.”
ONLINE EXCLUSIVE: What is 3D cell culture?
Medical researchers have grown human cells in culture media on or in sterile plastic dishes, such as Petri dishes, for more than 50 years.
Some cells, such as blood cells, can survive and grow in suspension, while others like smooth muscle cells need¬ to adhere to a surface to survive and grow. These are often called “2D cell cultures” because the cells grow horizontally across the bottom of the dish.
Some cells derived from connective tissues, such as fibroblasts, are not only adherent, but also very sensitive to the stiffness of their environment (“biomechanically sensitive” cells). Plastic dishes are at least 10,000 times stiffer than most connective tissues, and when biomechanically sensitive cells detect stiff surfaces, they can change the expression of their genes and behave abnormally.
The most common proteins in these tissues - and in the entire human body - are collagens, and one routine 3D cell culture approach is to embed fibroblasts in a collagen gel (gelatin). Fibroblasts in this environment can grow in any direction they choose, and their gene expression is more similar to cells in connective tissues.
These simple 3D cell cultures represent tissue engineering in its most basic form.
“Our challenge is to bioengineer simple 3D cell cultures in the lab to more closely mimic the complexity of human tissues, which have blood supply, nerves and interactions with other cells and tissues that modify their function and ability to heal after injury,” explains Dr. O’Gorman.
Dr. David O’Gorman is a Lawson Scientist and Co-director, Cell and Molecular Biology Laboratory at The Roth | McFarlane Hand and Upper Limb Centre in London, Ontario. He is also an Assistant Professor at Western University.
Imaging the microbiome
Normally samples of bacteria must be removed from their microbiome environment for analysis, which can lead to changes in their metabolic activity and other behaviors, hindering our ability to accurately study the gut or urogenital microbiome.
“This could be avoided if we are able to observe the bacteria in the body using Magnetic Resonance Imaging (MRI),” says Sarah Donnelly, MSc student at Lawson Health Research Institute and the Department of Microbiology and Immunology and collaborative Molecular Imaging program at Western University’s Schulich School of Medicine & Dentistry.
She is investigating the possibility of using magnetically-labelled bacteria with MRI to more directly study microbial interactions in urological and other conditions.
“The hope is that in the future we can use imaging technologies to visualize aspects of the microbiome in its healthy state compared to diseased states to see the early signs of disease and take preventative measures or allow for early intervention,” she says.
Donnelly has received a Lawson Internal Research Fund (IRF) Studentship to conduct the study, which will be supervised by Dr. Jeremy Burton, scientist in Lawson’s Human Microbiome and Probiotics research program at St. Joseph’s Health Care London (St. Joseph’s) and appointed to the Departments of Surgery and Microbiology & Immunology at Schulich Medicine & Dentistry; and Dr. Donna Goldhawk, scientist in Lawson’s Imaging research program at St. Joseph’s and assistant professor in the Department of Medical Biophysics at Schulich Medicine & Dentistry.
Escherichia coli (E. coli) are a common bacterium found in the human gut microbiome and frequently cause non-intestinal conditions like urinary tract infections. The researchers will program E. coli to express an iron uptake gene, magA. This gene is taken from another type of bacteria called magnetotactic because of their response to Earth’s magnetic field. The researchers will study whether the increase in iron uptake caused by magA expression will allow MRI to detect the magnetic signal more clearly than it would in images of untransformed E.coli. This would make it possible to see the bacteria’s behavior in living subjects without removing the bacteria cells from the microbiome environment.
They will then use this technique to study how magA labelled bacteria affect biofilm on medical devices. A biofilm is a structure produced when certain bacteria adhere to a surface and then stick together.
They will also analyze how lithotripsy affects the bacteria’s spatial distribution and interactions in three-dimensional models of kidney stones. Lithotripsy uses shockwaves to break up kidney stones into smaller pieces that are able to pass naturally out of the body. However, these shockwaves not only affect kidney stones. The waves are sent throughout the tissue, and the bacteria living on these tissues may also be affected.
“While lithotripsy is effective in treating kidney stones, we don’t know the side effects of lithotripsy on the microbiome. The shockwaves could disturb the bacteria, potentially leading to diseases caused by an imbalance between helpful and harmful bacteria,” says Donnelly.
These laboratory models will allow the researchers to perform studies in vivo (in animal models) in the future.
“Health research is very important for the development of new technologies and treatments but it is often difficult to secure funding. The IRF program allows students to pursue research that would not otherwise be possible,” explains Donnelly.
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
New study sheds light on the connection between the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
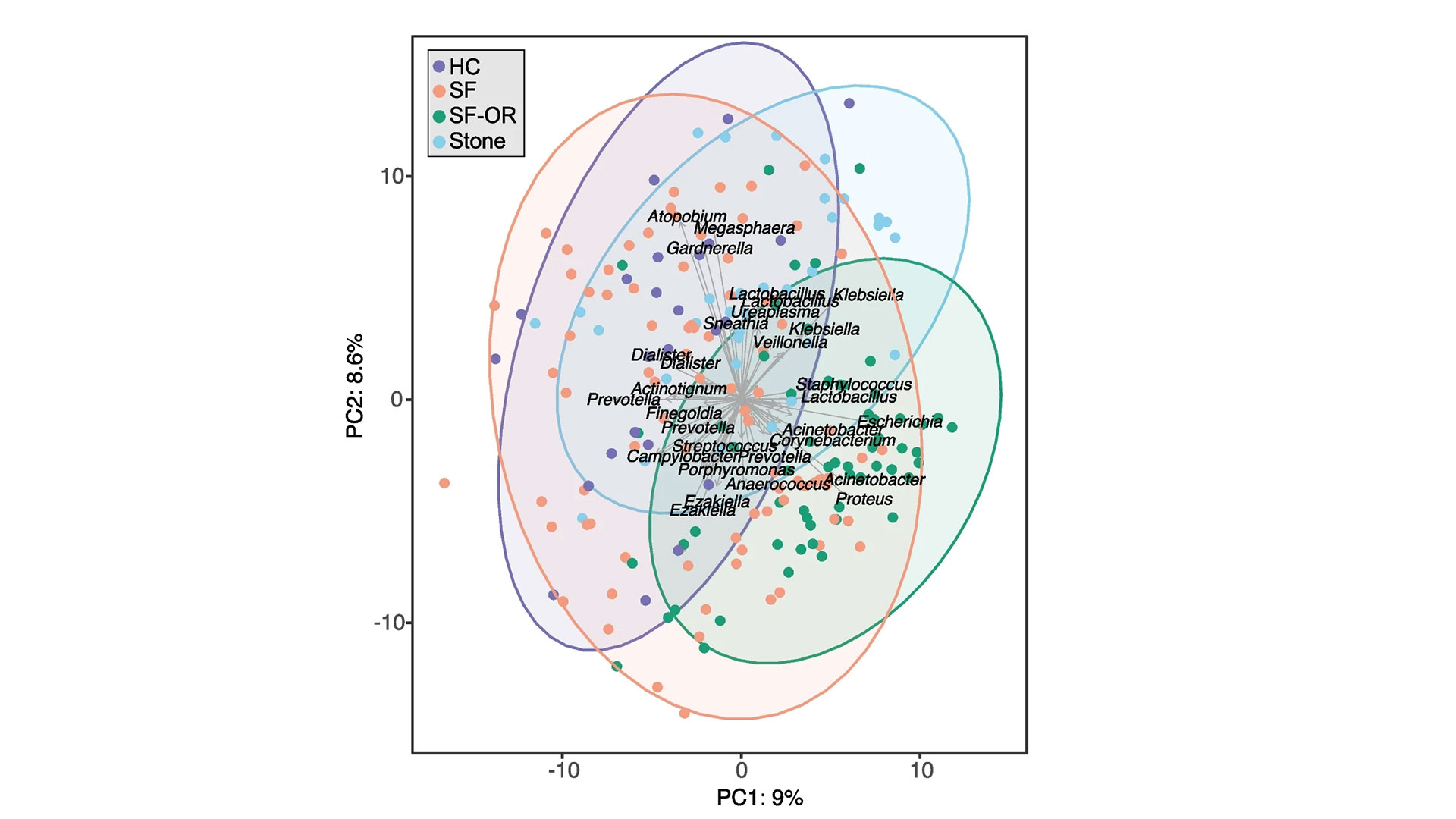
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email