Search
Search
New study sheds light on the connection between the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
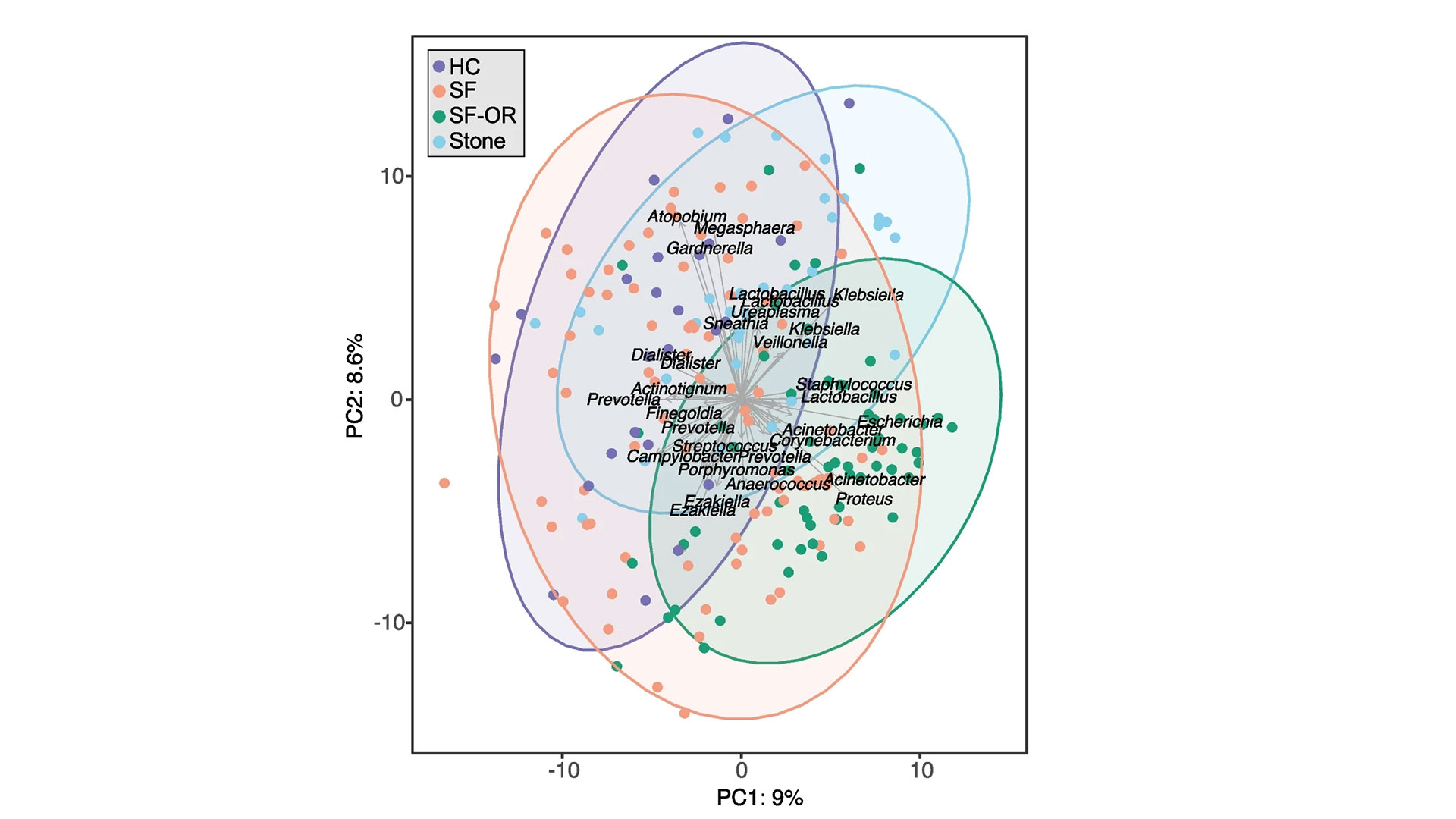
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
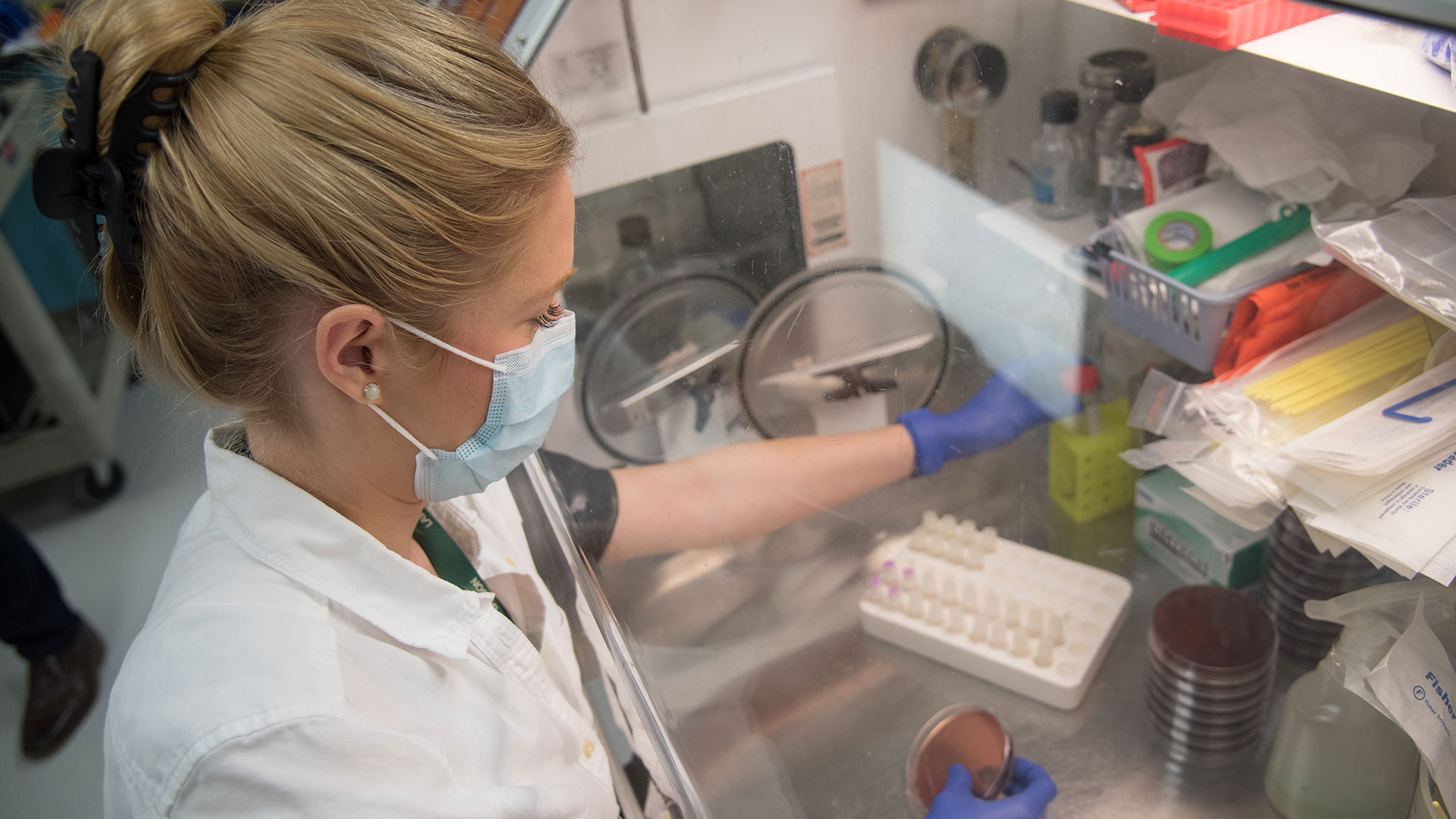
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Preventing infertility in men who undergo lymph node removal surgery for testicular cancer
When patients with testicular cancer undergo lymph node removal surgery there is a risk that their fertility will be affected if proper nerve sparing techniques are not used. Up to 75 per cent of men will not be able to father children if they receive the surgery without these techniques.
Lawson’s Internal Research Fund (IRF) has awarded a grant to Dr. Nicholas Power, a researcher at Lawson and urologic oncologist at London Health Sciences Centre (LHSC), who is leading a study to identify the nerves involved in fertility that are affected in lymph node removal surgery for testicular cancer.
“Sometimes patients go through a lot to be cured of testicular cancer only to be left dealing with long-term survivorship issues such as fertility. We hope to gain new insights into how fertility can be preserved after these men receive lymph node removal surgery,” says Dr. Power, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
In collaboration with Schulich assistant professors Dr. Marjorie Johnson and Dr. Brian Allman, and PhD candidate Tyler Beveridge, Dr. Power published initial results in The Journal of Urology announcing their discovery of a brand new anatomic structure, the pre-hypogastric ganglion, which needs to be spared in surgery to maintain fertility. They were also able to describe the first roadmap of retroperitoneal neuroanatomy – the anatomy of nerves in the space where surgeons locate lymph nodes most commonly affected by testicular cancer that has spread.
“There has never been a definitive anatomic study of the nerves of the retroperitoneum so it was our goal to provide the first comprehensive study of the nerves as they relate directly to patients who have testicular cancer,” explains Dr. Power. “After we published the initial results we were approached by textbook authors to use our data in upcoming editions of anatomy and surgical atlases. This will help to provide insight into nerve sparing techniques for surgeons who have not been trained at high-volume centers and ultimately improve the quality of care in testicular cancer patients overall.”
Already Dr. Power has found that using this knowledge when he performs lymph node removal surgery for testicular cancer has led to a 95 per cent success rate of preserving fertility.
The IRF will go towards their research to further investigate the actual function and physiology of the retroperitoneal neuroanatomy using a pig model.
“Lawson’s IRF provides incredible support for a field of study such as ours that is not yet at the stage of applying for a large grant. Receiving the funding gives us the independence to test out novel yet important hypotheses that will then lead us to further grants,” says Dr. Power.

Above: Dr. Nicholas Power
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
Simple device improves care after kidney transplantation
LONDON, ON – In a published study, a team from Lawson Health Research Institute has found that a simple device can reduce swelling after kidney transplantation. The geko™ device, manufactured by Sky Medical Technology Ltd and distributed in Canada by Trudell Healthcare Solutions Inc., is a muscle pump activator which significantly improves blood flow by stimulating the body’s ‘muscle pumps.’ Patients using the device following kidney transplantation experienced shorter hospital stays and reduced surgical site infections by nearly 60 per cent.
Kidney and simultaneous pancreas-kidney transplantations can significantly reduce mortality and improve the quality of life for patients with end stage renal disease. “After surgery, many of these organ recipients require a longer hospital stay due to delayed kidney function, infection, lack of mobility or edema,” says Dr. Alp Sener, Lawson Scientist and Transplant Surgeon in the Multi-Organ Transplant Program at London Health Sciences Centre (LHSC).
Edema is swelling caused by excess fluid trapped in the body’s tissues which can impact wound healing. The current standard of care for managing lower-limb edema and improving blood flow is thrombo-embolic-deterrent (“TED”) stockings used with compression devices. Sleeves pumped with air squeeze the lower legs to boost circulation. They can be uncomfortable to wear, and the large pump can inhibit early mobility and disrupt sleep after surgery.
In a randomized controlled clinical trial spanning two years, 221 transplant recipients at LHSC either wore the standard TED stocking and pump or the geko™ device for six days after surgery. Dr. Sener’s research team found that wearing the device increased urine output by 27 per cent and lowered weight gain by over a kilogram. With more urine produced and less fluid retention, patients experienced 31 per cent less swelling. The duration of costly hospitalization was shortened by over one day after kidney transplantation compared to the standard of care.
A 60 per cent reduction in wound infection rates was a striking observation. “Transplant patients are at a higher risk of infection due to the immunosuppressant medications needed after surgery,” explains Dr. Sener, who is also the President of the Urologic Society for Transplantation and Renal Surgery, a global organization affiliated with the American Urological Association. “Reducing infection means a much better outcome for the patient and considering that recent data shows wound infections can cost the health care system thousands of dollars per person, it’s a win-win situation.”
Some of the study participants wore pedometers to track their steps, and those using the geko™ device had improved mobility after surgery. The team suspects this may be due to reduced swelling which could improve ease and comfort when moving.
“The study results have been both surprising and exciting. Not only have we cut down wound infection rates but we have also seen a considerable improvement in the new organ’s function following transplantation. Patients report feeling more satisfied with the transplant process and are more mobile,” says Dr. Sener. The geko™ device is now being offered to patients at LHSC in recovery after receiving a new kidney.
Ruben Garcia, 68 years old, recently received a new kidney from his daughter, Ruby, who was a match as a living kidney donor. Following his surgery, Garcia found it difficult to get out of bed due to the pain and swelling, and the function of his new kidney was very low. “My surgeon explained in very simple terms that it was as if my new kidney wasn’t awake yet,” describes Garcia.
Dr. Sener recommended that Garcia use the geko™ device to help stimulate blood flow in a way that is similar to walking. Garcia was soon able to sit up on a chair and by the next day he was walking. “My kidney woke up and starting working again! I could feel the device working and it was comfortable to wear, almost like a massage for my legs. I’m very grateful for the care that I received.”
Dr. Sener adds that “using a muscle pump activator could be a game changer for other procedures like orthopedic implants where wound infection can have disastrous consequences or in surgeries where wound infections are more common such as in cancer and intestinal surgery.”
The geko™ device is non-invasive, self-adhering, battery-powered and recyclable. It generates neuromuscular electro-stimulation and unparalleled systemic blood flow that equates to 60 per cent of that achieved by walking. Pain-free muscle contraction compresses deep veins in the lower legs to create better blood flow in these vessels and return blood to the heart. It is particularly well suited to hospital settings as it portable and requires minimal training. For the indications for the use of the geko™ device, go to www.gekodevices.com.
“The results of the study provide further evidence that the geko™ device is an effective treatment option that can improve outcomes for patients and help them return home sooner, while reducing costs for the health-care system,” says George Baran, Executive Chairman of the Trudell Medical Group and a Director of Sky Medical.
-30-
DOWNLOADABLE MEDIA

Dr. Alp Sener, Lawson Scientist and Transplant Surgeon in the Multi-Organ Transplant Program at London Health Sciences Centre

The geko™ device being applied on the leg

The geko™ device
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
The invisible world inside us
The human microbiome is a wonder of nature.
Trillions of microbes call our body home. They live in our gut and many other places throughout our body. They are involved in virtually every aspect of how we function and we are learning that they are essential to staying healthy. An unhealthy microbiome has been linked to many diseases from allergies to cancer and even mental health.
Most people out there have heard about probiotics and fermented foods, and chances are you’re trying to get more of them in your diet.
Drinking kombucha or eating yogurt, anyone?
Join Lawson Health Research Institute for our next Café Scientifique event, "The invisible world inside us: Exploring the human microbiome."
Hear from a panel of researchers who are unraveling the mysteries about the microbiome and using that knowledge to improve health and health care. They will also bust some myths and share the important facts when it comes to probiotics, prebiotics and the microbiome.
Image

SPEAKERS
- Dr. Gregor Reid, Lawson Scientist and Professor of Microbiology & Immunology and Surgery at Western University.
Presenting: Probiotics and Prebiotics - Look beyond the fake news - Dr. Michael Silverman, Lawson Associate Scientist, Chair of Infectious Diseases, Schulich School of Medicine & Dentistry at Western University and Chief of Infectious Diseases for St. Joseph’s Health Care London and London Health Sciences Centre.
Presenting: Fecal Transplants: What does this crap have to do with me? - Dr. Jeremy Burton, Lawson Scientist and Assistant Professor of Surgery (Urology) and Microbiology & Immunology at Western University.
EVENT DETAILS
Date: Wednesday, November 27, 2019
Time: 7-9 pm (doors open at 6:30 pm)
Location: Best Western Plus Lamplighter Inn & Conference Centre (Regency Room), 591 Wellington Rd, London, ON N6C 4R3
Map and directions.
Parking: Free on-site parking
This is a free event and online registration is REQUIRED.
Registration for this evengt is now FULL.
Please fill out the form here to be added to the waitlist.
You will be notified should a spot open up.