Search
Search
Genetic testing could personalize care for patients with Crohn’s disease, particularly women
LONDON, ON - In a study involving 542 Crohn’s disease patients, researchers at Lawson Health Research Institute examined whether a patient’s DNA can be used to identify their risk of severe disease. They found that patients with a genetic variant in a gene called FXR (farnesoid X-receptor) are much more likely to need surgery and to need it earlier in their care journey. Surprisingly, they found that women with the genetic variant are at an even higher risk than men.
Crohn’s disease is an often debilitating condition that affects one in every 150 Canadians. The condition is characterized by intestinal inflammation caused by unnecessary attacks from the body’s immune system. It’s a disease that can behave and progress differently from one person to the next, with some requiring surgery to remove affected parts of the intestine.
“While medications are prescribed to manage Crohn’s disease, physicians have to balance the risk of side effects with the risk of undertreating severe cases of the disease,” explains Dr. Aze Wilson, Associate Scientist at Lawson Health Research Institute and Gastroenterologist at London Health Sciences Centre (LHSC). “In order to personalize treatment, it would be great to have a tool for identifying which patients will have the most severe cases of illness.”
Dr. Wilson and her colleagues became interested in the FXR gene because of its role in intestinal health. The FXR gene is a part of human DNA that controls how we process drugs and has also been linked to how well our intestines work. The research team suspected that variation in the gene could lead to poorer outcomes in Crohn’s disease patients.
“Given the importance of FXR to intestinal health, we wanted to see whether it plays a role in disease severity and we discovered that it does,” says Dr. Wilson. “Our findings suggest that genetic testing could be used to identify patients at a high risk of poor outcomes. This would allow physicians to tailor treatments to give patients the best chance at success.”
The team also discovered that women who carried the genetic variant were at the highest risk of needing surgery and the highest risk of early surgery, even when compared to men with the genetic variant. Struck by this finding, they conducted further testing using laboratory-based cell models. They found that estrogen (a female sex hormone) in combination with the genetic variant reduced the function of FXR even further.
“Differences between men and women with Crohn’s disease are not often considered in research or clinical practice. We apply treatments in the same way to both sexes, which may not be the best approach,” explains Dr. Wilson. “We identified a group of women who may benefit from a different approach to care. The study highlights the need for evaluating the effect of biological sex on disease and the interaction it may have with our DNA.”
Looking forward, the team hopes to further explore the effect of this genetic variant on intestinal health using laboratory-based cell models. They also hope to assess the value of genetic testing as a tool for informing treatment decisions made by patients and their physicians.
“One of our larger goals as a research group is to develop a personalized care plan for patients with Crohn’s disease and ulcerative colitis – one that integrates genetic information and other biomarkers to improve how care is delivered to these patient populations,” notes Dr. Wilson.
The study, “Genetic variation in the farnesoid X-receptor predicts Crohn’s disease severity in female patients,” is published in Nature’s Scientific Reports.
-30-
DOWNLOADABLE MEDIA

Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Growing Tissues in the Lab
When challenged by surgeons to find better treatments for difficult-to-manage connective tissue diseases, Dr. David O’Gorman gladly accepted.
Dr. O’Gorman is a Molecular Biologist and Lawson Scientist based at St. Joseph’s Hospital, a part of St. Joseph’s Health Care London. His research focuses on understanding normal and abnormal connective tissue repair. He collaborates with researchers and clinicians working in many different disciplines, including those specializing in reconstructive surgery, orthopedics and urology.
Surgical reconstructions can be hampered by a lack of graft tissue, or graft tissue of insufficient quality, making it difficult to achieve optimal outcomes for the patients.
An example is a condition called urethral stricture disease (urethral scarring). This condition occurs in males and typically causes symptoms such as frequent and urgent urination, and slow urinary stream. In extreme cases, it can cause urinary tract infections, permanent bladder dysfunction and renal failure. Recurrence rates after minimally invasive treatments are high, and so many urologists recommend open surgical approaches.
Surgeons can use the patient’s own tissues to reconstruct the urethra after stricture removal. This tissue is normally sourced from the buccal cavity in the mouth but taking large tissue grafts can result in complications. In cases where buccal grafts have been used for previous reconstructions, there may not be enough intact tissue left.
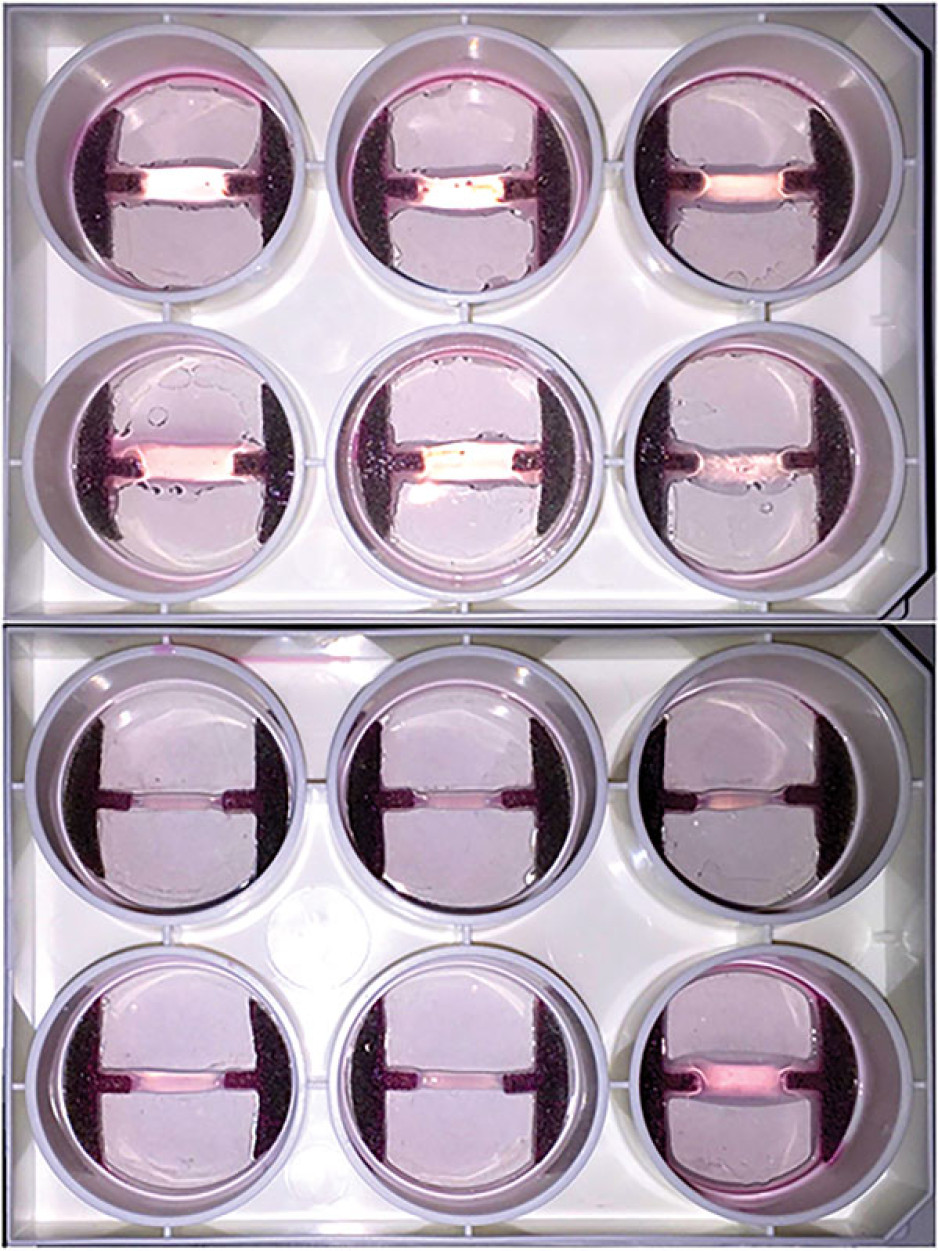
Dr. O’Gorman sees a solution in growing sheets of human buccal tissues in the lab.
“We are currently using buccal graft trimmings as a source of cells, culturing them in a 3D environment and expanding them to create tissues of suitable size, density and elasticity.”
The patient’s own cells are used to generate a tissue graft for urethral reconstruction. While several research groups have developed this approach in the past, few have attempted to translate their models for clinical use.
“Our immediate goal is to provide proof of principle – that we can consistently generate grafts of suitable size and functional characteristics,” explains Dr. O’Gorman, “In the future, we could be providing bioengineered graft tissues for reconstructive surgeries here in London.”
Bioengineered human tissues can also be used as ‘mimetics’ – replications of human tissues – to study diseases, especially those difficult to model using routine laboratory methods.
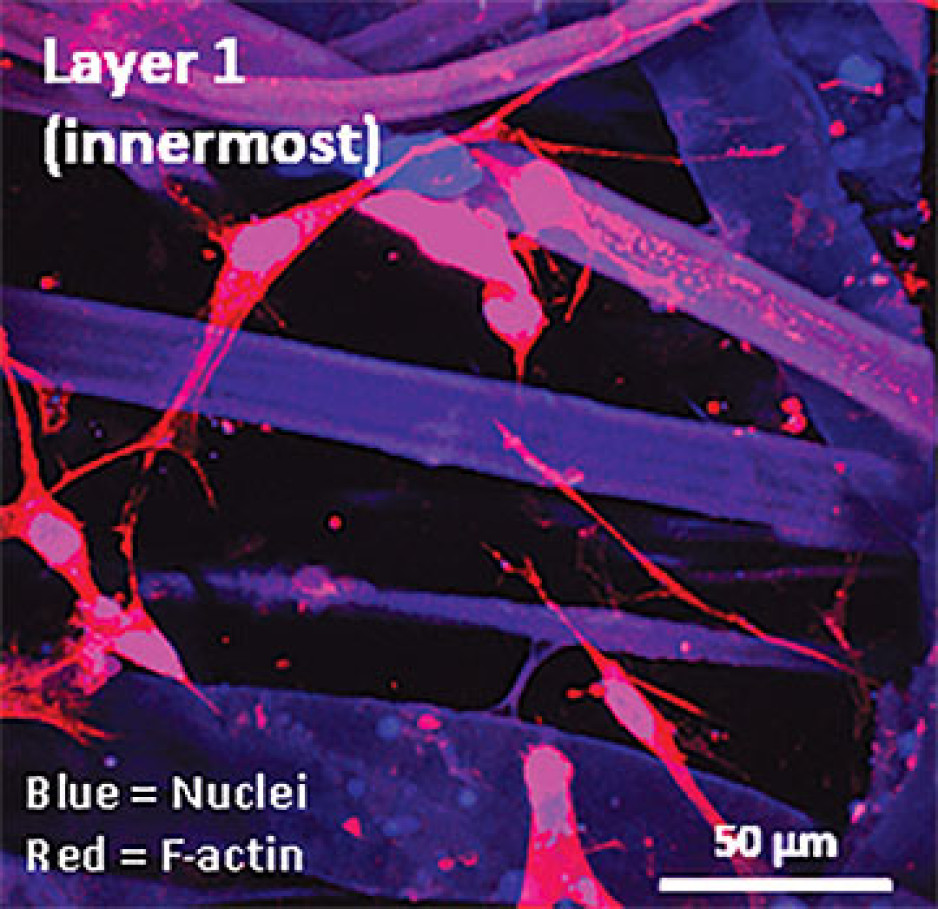
Instead of a using a growth media or sterile plastic dishes, 3D cell culture is achieved by embedding cells in a matrix of proteins and other molecules normally found in those tissues. In this environment, gene expression and growth is more similar to cells of connective tissues in the body being replicated.
Dupuytren’s disease (or Dupuytren’s Contracture) affects the palmar fascia in the hand, a connective tissue beneath the skin that extends from the base of the palm into the fingers. This disease can be understood as a type of excessive scarring, where normal tissue repair processes have gone awry and dense scar tissue forms, typically causing permanent palm or finger flexion that restricts hand function.
This condition is surprisingly common and may affect more than one million people in Canada. While there are surgical treatment options available, none consistently prevent this disease from recurring in at least a third of patients.
“Due to its high recurrence rate after treatment, Dupuytren’s disease is currently considered incurable. Our challenge is to understand it well enough to develop truly effective treatments,” says Dr. O’Gorman.
Human hands have unique characteristics not found in other species, making animal models impractical. Instead, Dr. O’Gorman’s team extracts cells from the diseased palmar fascia of patients undergoing hand surgeries and bioengineers them into palmar fascia ‘contractures’ in the lab.
“Since the cells from a single palmar fascia sample can be used to grow dozens of little contractures, we can test many different treatments simultaneously to see what works best for each patient.”
This approach may also allow them to determine if Dupuytren’s disease is truly one disease, or a group of similar diseases that cause palm and finger contractures.
“Often, Dupuytren’s disease is clearly heritable, but some individuals have no family history of it and develop apparently sporadic disease,” notes Dr. O’Gorman. “We want to determine if these are truly the same disease at the molecular level.”
Another major cause of abnormal connective tissue repair is infection, and tissue mimetics can play a role here, too. While rare, infections of artificial joint replacements are particularly devastating for patients, as they typically require readmission to hospital to remove the infected joint, weeks of antibiotic-based treatment, and an additional surgery to replace the artificial joint.
In addition to the associated pain and suffering, these procedures are technically challenging and costly to our health care system.
Artificial shoulder joint infections are most frequently caused by the microorganism Cutibacterium acnes (C. acnes). C. acnes infections disrupt normal tissue repair processes after surgery, cause shoulder tissues to die and promote loosening of the artificial joint. These infections are difficult to diagnose, and there is a lack of reproducible
models in which to study them. Dr O’Gorman’s team has set out to create the first human Shoulder-Joint Implant Mimetic (S-JIM) of C. acnes infection.
“While S-JIMs are more complex, they are 3D in vitro cell culture systems designed to mimic human tissues, like those that we use for studying Dupuytren’s disease.”
S-JIMs include layers of artificial human tissue, wrapped around cores of titanium alloy or cobalt chrome, the metals used to create artificial joints. They are co-cultured with C. acnes under low oxygen conditions similar to those that normally occur around artificial shoulder joints.
“We are bioengineering simple 3D cell cultures to more closely mimic the complexity of human tissues, with blood supply, nerves and interactions with other cells.” – Dr. David O’Gorman
Studying the connective tissue layers close to the infection allows researchers to investigate processes that promote infection, such as the formation of a biofilm that harbours and protects the bacteria from the body’s immune system. They are also able to test whether novel treatments can disrupt biofilm formation and increase the effectiveness of antibiotics.
Dr. O’Gorman predicts that in the future, medical researchers will routinely use bioengineered 3D human tissue and organ mimetics to accelerate our understanding of disease.
“The technology is in its infancy, but the potential for using bioengineered human tissues for surgical reconstructions or as disease models is huge. At Lawson, we’re ready to take on health care challenges and build on innovative approaches to improve the quality of life for patients.”
ONLINE EXCLUSIVE: What is 3D cell culture?
Medical researchers have grown human cells in culture media on or in sterile plastic dishes, such as Petri dishes, for more than 50 years.
Some cells, such as blood cells, can survive and grow in suspension, while others like smooth muscle cells need¬ to adhere to a surface to survive and grow. These are often called “2D cell cultures” because the cells grow horizontally across the bottom of the dish.
Some cells derived from connective tissues, such as fibroblasts, are not only adherent, but also very sensitive to the stiffness of their environment (“biomechanically sensitive” cells). Plastic dishes are at least 10,000 times stiffer than most connective tissues, and when biomechanically sensitive cells detect stiff surfaces, they can change the expression of their genes and behave abnormally.
The most common proteins in these tissues - and in the entire human body - are collagens, and one routine 3D cell culture approach is to embed fibroblasts in a collagen gel (gelatin). Fibroblasts in this environment can grow in any direction they choose, and their gene expression is more similar to cells in connective tissues.
These simple 3D cell cultures represent tissue engineering in its most basic form.
“Our challenge is to bioengineer simple 3D cell cultures in the lab to more closely mimic the complexity of human tissues, which have blood supply, nerves and interactions with other cells and tissues that modify their function and ability to heal after injury,” explains Dr. O’Gorman.
Dr. David O’Gorman is a Lawson Scientist and Co-director, Cell and Molecular Biology Laboratory at The Roth | McFarlane Hand and Upper Limb Centre in London, Ontario. He is also an Assistant Professor at Western University.
Health research in London receives millions in funding from federal government
Lawson Health Research Institute was awarded over $1.2 million in the Canadian Institutes of Health Research’s Fall 2019 Project Grant competition, for three projects including one Priority Announcement.
“This is a great accomplishment for the successful researchers at Lawson and those working across the city,” says Dr. David Hill, Lawson Scientific Director. “At Lawson, our scientists target rapid response research that can be quickly incorporated into improved care for patients and families. Our research happens within hospital walls, where care is delivered, with innovations that improve lives every day.”
Western University received more than $11.9 million in research funding through the project grant competition for 17 projects. A special congratulation to Lawson researchers Drs. Samuel Asfaha, Thomas Appleton, Neil Duggal, David Spence and Zhu-Xu Zhang, as well as Dr. Subrata Chakrabarti, recipient of the CIHR Priority Announcement for “Novel mechanisms in diabetic cardiomyopathy.”
Selective Brain Hypothermia via Intranasal Cooling to Limit Brain Injury Post Cardiac Arrest
Dr. Ting-Yim Lee
There are 40,000 cardiac arrests per year in Canada. Within the body, it triggers a complex cascade of dysfunction resulting in cell death, even after successful cardiopulmonary resuscitation, with only three to seven per cent of survivors returning to normal function.
To reduce the high incidence of brain damage and the burden on families, the American Heart Association has recommended hypothermia for neuroprotection in post cardiac arrest care.
However, current clinical hyperthermia cools the whole body instead of just the brain. Simple, effective and non-invasive methods to selectively cool the brain that can be readily used in and out of hospitals are not available.

“The grant is allowing us to collect validative data on the protective effect of brain cooling in limiting brain injury from cardiac arrest,” explains Dr. Lee. “The device is very convenient to use. It is compact and can be set up right by the bedside of patients in intensive care units.”
Dr. Lee sees the device as having the potential to be used widely to limit brain injury following stroke, head trauma and sepsis.
“This kind of investment in hospital-based research allows us to identify important clinical problems and find ways to solve them, working closely with research patients along the way.”
Multi-centre diagnostic performance of dynamic CT perfusion for functional assessment of multi-vessel coronary artery disease with dense coronary calcification
Dr. Aaron So
Coronary artery disease (CAD) occurs when plaque forms in one or more coronary arteries of the heart. It is one of the leading causes of mortality and morbidity in the world.
Patients with CAD can go to a cardiac catheterization laboratory where the narrowed coronary artery can be reopened using a catheter-based technique. However, this approach is invasive for the patient and costly for the system. Studies have shown that for various reasons not all patients benefit from this treatment.

With the funding, they are testing the technique at several hospitals and national cardiovascular centres in Canada, China, Germany and Japan. With larger clinical studies in the future, they could determine the optimal diagnostic strategy for patient triage and reduce unnecessary procedures.
“Health research has been and will continue to be very important, with the commitment of patients and clinicians playing a crucial role in the success of medical research and advancement,” says Dr. So. “It’s important for the Canadian government to continue to support research in academic hospitals.”
He adds that the success of the CIHR grant application shows that Canadian researchers can be leaders in health research that benefits people around the world.
Filling Knowledge Gaps for the Success of Ontario Renal Plan 3
Dr. Matthew Weir
The Ontario Renal Network (ORN) is the agency responsible for distribution of funding for kidney care in Ontario. They have released three policy statements outlining strategic objectives for kidney care, with the most recent being the recently released Ontario Renal Plan 3 (ORP3).
“Within the strategic objective, gaps in our understanding of kidney disease have been identified as barriers to successful implementation,” explains Dr. Weir. “We have proposed a suite of 32 related retrospective cohort analyses designed using integrated knowledge translation to address those gaps.”
The Priority funding will help get the first projects underway and build momentum. “The ORP3 had extensive consultation with patients, families and other stakeholders. By supporting its successful implementation, our findings will have a direct and immediate effect on patients in areas that are a priority to them.”

Health researchers in London bring in over $11 million of national funding
The Canadian Institutes of Health Research (CIHR) announced more than $11.3 million in funding through their project grants program for 17 health research projects across Lawson Health Research Institute and Western University.
“The funded projects represent a wide range of research and expertise from London’s health research community, with real impacts for health and health care,” says Dr. David Hill, Lawson Scientific Director. “Congratulations to those successful applicants who have secured this funding on a very tough competition.”
Projects include a national study on transgender health; a community-based family treatment program for children with epilepsy; imaging of blood clots in the brain; equity in mental health care for children and youth; and, a smartphone intervention focused on diet and food literacy.
See the full list of successful applicants.
Cooling the Brain after Resuscitated Cardiac Arrest to Prevent Brain Injury
There are 40,000 cardiac arrests each year in Canada. A high number of patients won’t survive the event and nearly half of the survivors suffer from brain damage that can have a huge impact on their ability to live independently. The current guidelines recommend cooling of the whole body to protect the brain against the damaging effects of cardiac arrest. However, in the clinic there are several hurdles for this treatment that can create complications. Enhanced brain protection may be achieved by selectively cooling the brain but a simple, effective and non-invasive method to do so is needed.
Dr. Ting-Yim Lee and his research team are studying a simple means to cool down the brain by blowing compressed air into the nostrils which would essentially chill the warm blood coming through the nasal cavity on its way to the brain. Using an animal model, their aim is to show that the method can be used safely and is able to protect the brain after cardiac arrest.
Image


The DECIPHER Study
Shoulder fractures are becoming increasingly common for older adults and cause considerable limitations and impacts for their daily life. While different approaches are taken to treat shoulder fractures, there is a lack of knowledge and evidence to show which of those methods are the most effective and for which patients.
Dr. Emil Schemitsch and his research team are proposing the first nation-wide, multi-centre observational study with over 600 patients with the ultimate goal of determining what specific factors influence important outcomes for patients. The DECIPHER study will seek to answer important questions about which treatment and rehabilitation strategies are best for different patients, strengthening the clinical strategy for managing these difficult and prevalent injuries. It will also provide an economic analysis to understand the impact for healthcare system costs.

Congratulations to all of the successful applicants:
- Greta Bauer and Ayden Scheim - Trans PULSE Canada: A National Study of Transgender Health
- Maria Drangova - Characterizing cerebral thrombus composition with Phase‐based MRI
- David Edgell, Bogumil Karas, and Gregory Gloor - ConCRISPR: Conjugative delivery of a hybrid CRISPR/Tev nuclease system for specific microbiota modulation in the mammalian gut
- Jason Gilliland - Evaluation of a Smartphone Based Intervention for Improving Food Literacy, Food Purchasing, and Diet Quality Among Youth in Urban, Suburban, and Rural Environments
- Douglas Hamilton - Novel Biomaterials‐Based Strategies to Stimulate Periodontal Tissue Regeneration
- David Haniford - Regulation of Salmonella pathogenesis by transposon‐encoded small regulatory RNAs
- Steven Laviolette - Effects of Neurodevelopmental Exposure to Cannabinoids on Prefrontal Cortical Function: Implications for Neuropsychiatric Disorders
- Ting-Yim Lee - Selective Brain Hypothermia via Intranasal Cooling to Limit Brain Injury Post Cardiac Arrest (Funded through Lawson Health Research Institute)
- Stephen Lomber - Cortical Plasticity Following Deafness
- Vania Prado - Cholinergic influence in aging and brain pathology
- Graham Reid and William Gardner - Equity in Mental Health Care for Children and Youth
- Jason Roberts - The Role of Electrophysiology Testing in Survivors of Unexplained Cardiac Arrest: The EPS ARREST Study
- Emil Schemitsch - The DECIPHER Study: DEterminants of Function and Clinically Important outcomes in Proximal Humerus Fractures in the Elder Population: A National CohoRt (Funded through Lawson Health Research Institute)
- Walter Siqueira and Elizabeth Gillies - Novel Drug Delivery System for the Combat of Dental Caries by using Salivary Peptides
- Kathy Speechley and Karen Bax - A Community-Based Family Treatment Program for Children with Epilepsy: A Randomized Controlled Trial
- Andrew Watson - Understanding and Treating Obesity Related loss of Embryo Developmental Competence
- Donald Welsh - Kir Channel Regulation by Membrane Lipids: An Enabler of Hemodynamic Sensing in the Cerebral Circulation