Search
Search
New research on reducing harm for people who use methamphetamine in hospital
LONDON, ON – At a virtual event today, a research team from Lawson Health Research Institute is announcing details of the Methamphetamine Harm Reduction Project that will test the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose. “Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk. “We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study aims to improve treatment for rheumatoid arthritis
A research team led by Lawson scientist Dr. Mamadou Diop has been awarded a Lawson Internal Research Fund to investigate whether a previously developed optical technique that can detect arthritis within one week of onset could also be used to provide early assessment of treatment response for rheumatoid arthritis (RA).
RA is a disease that causes chronic inflammation of the joints, which results in pain, reduced quality of life and loss of productivity. There is no cure for RA but a new category of drugs – biologic agents that can reduce pain and slow down or even halt disease progression – has revolutionized treatment.
However, these new drugs are expensive and only work in 30 per cent of patients, which means many RA sufferers are treated with no benefit for up to six months – the time it takes for current monitoring methods to reliably determine whether a treatment is working or not. “This is a direct consequence of the lack of sensitivity of current monitoring methods,” says Dr. Diop, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
Since their recently developed optical technique has a high sensitivity to arthritis, Dr. Diop and his team believes it could also be used as a safe and convenient method of assessing treatment efficacy in RA patients. Additionally, there are striking similarities between RA and cancer, and it has been shown that optical techniques can predict cancer in as early as one day after therapy starts.
At St. Joseph’s Health Care London, they will test this theory in a rat model of RA and compare the results of the optical technique to histology and CT imaging, other established methods of determining whether a treatment is effective.
“If successful, this project will generate a safe, low-cost technique that can detect treatment response in RA within days of starting treatment. This would reduce the risk of further joint damage experienced by many patients for whom the drugs are ineffective,” says Dr. Diop. “We hope this will enable early redirection of patients with non-responding RA to alternative treatments, such as a combination of multiple drugs and more frequent monitoring.”
Dr. Diop adds, “The Lawson IRF grant will enable us to test the validity of our hypothesis and subsequently generate valuable preliminary results to support grant proposals for larger external funding.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
New study sheds light on the connection between the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
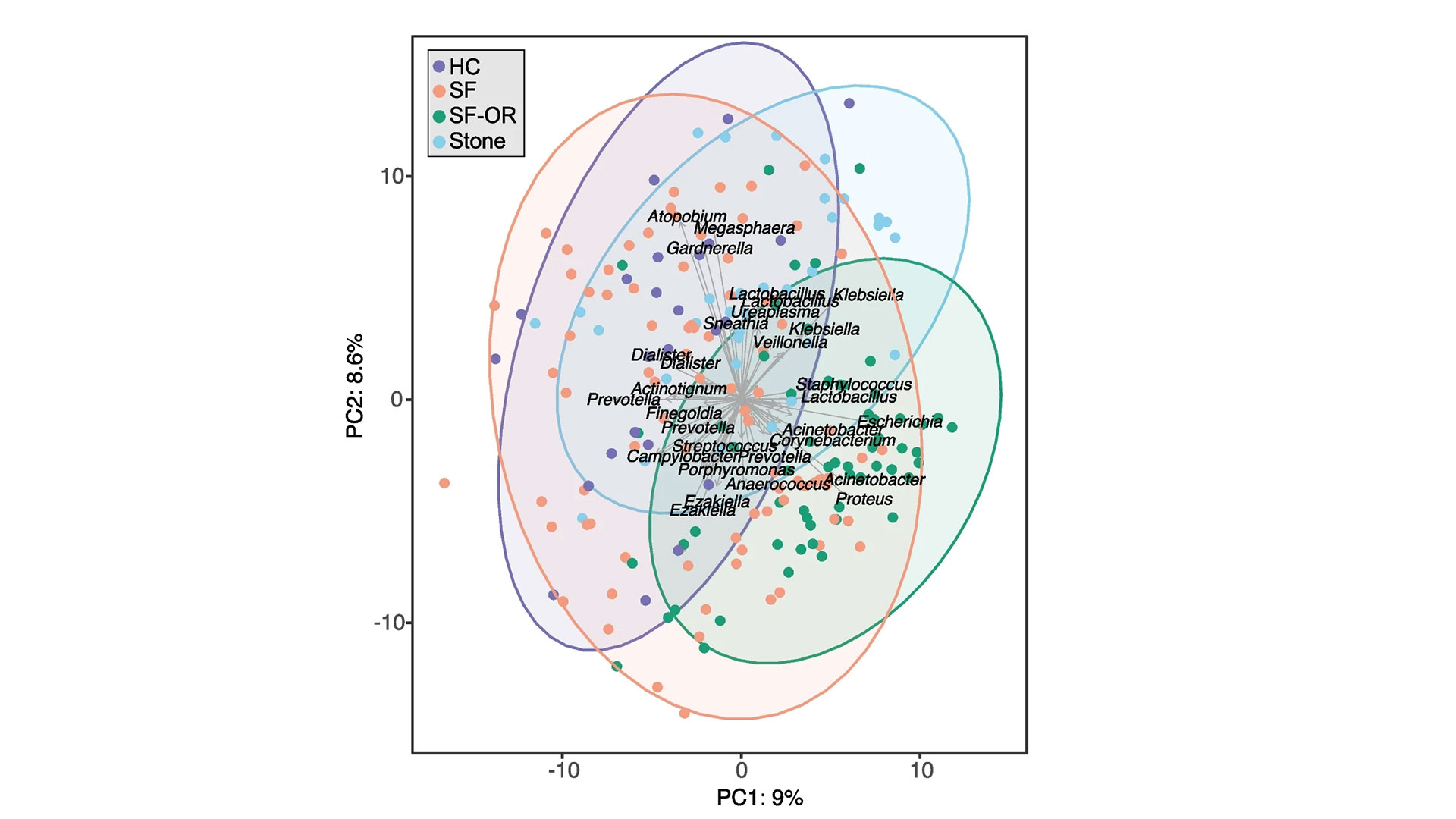
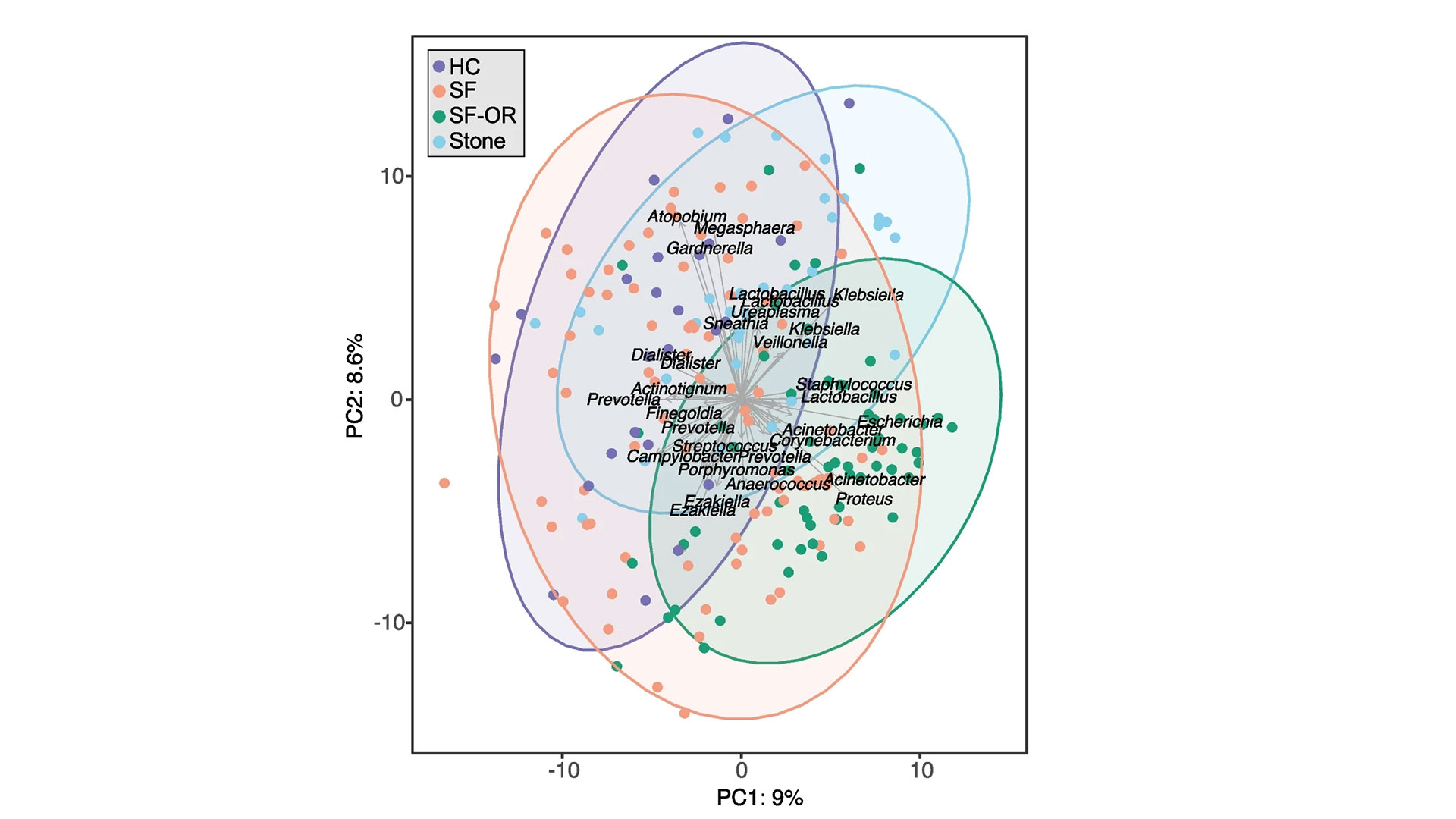
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study sheds light on the connection between the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study shows technology could play an important role in mental health support
LONDON - In a study published in MDPI Journal, a team of researchers at Lawson Health Research Institute have shown that the use of technology may assist in better outcomes for those living with both mental health and physical disorders.
Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson, and her team embarked on a pilot study that used smart home monitoring solutions to assist those living with both a mental health disorder and other health challenges. The purpose of this pilot study was to see if technology could improve overall lifestyle and wellbeing.
“We began our research by using hospital prototype apartments – apartment style care spaces within hospital settings – that were equipped with smart home technology solutions such as a screen device, activity trackers, weigh scales and medication dispensers,” says Dr. Forchuk who is also the Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery at St. Joseph’s Health care London. “Once we tested it in a hospital setting, we wanted to find a way to take this idea out into the community in different kinds of housing and living situations to see if it would be beneficial.”
The research team partnered with the Canadian Mental Health Association (CMHA) and the London and Middlesex Community Housing (LMCH) to work together to retrofit the homes of the 13 study participants.
“We worked together with the participants and their care providers to choose what combination of technology they felt would be best for them,” says Dr. Forchuk. “No matter their health condition each participant wanted to be more active and independent, with the goal of staying out of hospital.”
All smart devices were connected to the Lawson Integrated Database, which is a database that can securely collect data from multiple sources such as health devices. This allowed care providers to send reminders to participants, while also tracking usage and results.
“The key benefits we noted was that study participants started to live healthier lives,” says Jonathan Serrato, Lawson Research Associate. “Participants logged going for walks and exercising more often, as well as making healthier food choices. Those who used the medication dispensers did not miss a single dose. The touch screen devices also allowed participants to easily communicate with care providers and support networks, and access more resources.”
Following the pilot study, the research team also published a subsequent paper, as a ‘how-to guide’ for utilizing smart home technology interventions as a health care tool.
“This paper is a helpful resource that outlines implications and considerations when it comes to smart home technologies,” adds Serrato. “There are many areas we touch upon such as security, privacy and feasibility as well as hardware and software information for those who would like to take on their own similar type of smart home technology project.”
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study testing whether virtual groups can improve well-being in older adults
LONDON, ON- The COVID-19 pandemic has taken a toll on social connections, emotional health and well-being, especially for older adults. A new study through Lawson Health Research Institute will examine whether online/virtual ‘meaning-centered’ groups can help promote social connections and reduce risk for psychological distress.
Online meaning-centered groups are a promising approach developed by a research team led by Dr. Marnin Heisel, a Lawson Scientist, Clinical Psychologist at London Health Sciences Centre and Professor at the Schulich School of Medicine and Dentistry at Western University.
In his previous research, which began in-person and pivoted online during the pandemic, Dr. Heisel found that Meaning-Centered Groups helped men transitioning into retirement, a time when there is often a struggle with issues of identity, purpose and lost social connections.
“We found that people really enjoyed the camaraderie, they supported one another and many of them started getting involved in community activities, including outreach activities of their own and volunteering,” says Dr. Heisel.
Now, Dr. Heisel and his colleagues are looking to recruit participants from one of the populations hardest hit by the mental health impacts of the pandemic – older adults, who have become even more socially isolated.
“A lot of my research is focused on suicide prevention in older adults and I realized over time that one of the best ways of doing that is not waiting until people have to come for a psychologist or psychiatrist’s help, but rather to intervene much earlier and help people find those things that make life worth living,” notes Dr. Heisel.
The sessions will be 75 to 90 minutes and convened online once a week for eight weeks. The hope is to include approximately 10 people per group, with multiple groups underway at the same time.
“The meetings will focus on supporting one another, trying to build and enhance psychological resiliency, focusing on finding meaning in creative outlets, in relationships and other experiences,” explains Dr. Heisel. “They will also focus on attitudes towards challenges in life including adversities, the pandemic, being socially isolated, and also positive experiences.”
Dr. Heisel says he recognizes that the virtual format can be a challenge for some, but his team will help participants to both access and successfully use the technology.
Recruitment for the study is underway. Those interested in participating or who have friends or loved ones who might be interested can contact Dr. Heisel at Marnin.Heisel@lhsc.on.ca or view the study website at https://meaningfulgroups.com/groups for details.
Funding for the study is being provided by the Centre for Aging and Brain Health Innovation at the Baycrest Centre and the Canadian government.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study will assess fecal transplants in treatment of pancreatic cancer
Scientists examining microbiome to improve cancer therapies
MEDIA RELEASE
For Immediate Release
LONDON, ON- Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes.
“Pancreatic cancer is very hard to treat, partially because when it’s detected, the cancer is usually in a later stage and spreads very quickly,” explains Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s London Regional Cancer Program (LRCP) and Associate Scientist at Lawson. “Our best chemotherapy treatments for the average patient, will give them a little less than a year to live.”
With the goal of improving treatments for these patients the research team led by Dr. Saman Maleki, Scientist at Lawson, is studying whether changing the gut microbiome can result in better response to cancer treatments.
“We know that the microbiome plays an important role in patients’ response to various forms of systemic treatments such as immunotherapy and chemotherapy for different cancers,” says Dr. Maleki.
This unique study will happen in three stages. The first stage is an observational study to examine fecal samples of 52 patients at LRCP with advanced pancreatic cancer. The second stage will focus on using the samples from these patients in preclinical models to test new combinations of treatments. The final stage of the study will focus on intervention through human clinical trials by modifying a patient’s microbiome with something called a fecal transplant prior to treatment.
“The microbiome is involved in many aspects of cancer development and these organisms aren’t just living in the gut but also within the tumor,” says Dr. Michael Silverman, Lawson Scientist and Chair/Chief of Infectious Diseases at LHSC and St. Joseph’s Health Care London. “We believe that by giving people a fecal transplant, we can change the bacteria that live within the tumor and gut and then optimize the immune response to both the tumour and to treatment, with the goal of improving patient outcomes.”
Fecal transplants involve collecting stool from a healthy donor, preparing it in a lab and safely transplanting it to the patient, in this case with a capsule. The goal is to transplant the donor’s microbiome so that healthy bacteria will colonize in the patient’s gut.
“If you think of microbiome, each bacterium is like a little factory and all together they are a giant factory within us producing things we need,” explains Dr. Jeremy Burton, Lawson Scientist who specializes in human microbiome research. “Over time, a person’s diet, medications, and lifestyle can change the microbiome and it can have a big impact to the rest of our body.”
The research team was recently awarded a $450,000 Catalyst 2021 grant from the Weston Family Foundation to conduct this study, which is the first in the world focusing on prospectively modifying the microbiome in pancreatic cancer patients for treatments and outcomes.
“We normally don’t see this in one study where we go through the full spectrum of learning from patients, to looking at treatments, and then moving to a final intervention stage,” explains Dr. Maleki. “This has not been tried in pancreatic cancer before, but we think leveraging the microbiome and improving the immune response can potentially move the needle in this patient population.”
The team is recruiting both pancreatic cancer patients, as well as healthy volunteers for fecal transplant samples. Those interested in helping with fecal transplant donations can contact Dr. Seema Parvathy at 519-646-6100 ext. 61726 or email seemanair@@email
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study will assess fecal transplants in treatment of pancreatic cancer
Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes.
“Pancreatic cancer is very hard to treat, partially because when it’s detected, the cancer is usually in a later stage and spreads very quickly,” explains Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s London Regional Cancer Program (LRCP) and Associate Scientist at Lawson. “Our best chemotherapy treatments for the average patient, will give them a little less than a year to live.”
With the goal of improving treatments for these patients the research team led by Dr. Saman Maleki, Scientist at Lawson, is studying whether changing the gut microbiome can result in better response to cancer treatments. “We know that the microbiome plays an important role in patients’ response to various forms of systemic treatments such as immunotherapy and chemotherapy for different cancers,” says Dr. Maleki.

Dr. John Lenehan, Dr. Jeremy Burton and Dr. Saman Maleki
This unique study will happen in three stages. The first stage is an observational study to examine fecal samples of 52 patients at LRCP with advanced pancreatic cancer. The second stage will focus on using the samples from these patients in preclinical models to test new combinations of treatments. The final stage of the study will focus on intervention through human clinical trials by modifying a patient’s microbiome with something called a fecal transplant prior to treatment.
“The microbiome is involved in many aspects of cancer development and these organisms aren’t just living in the gut but also within the tumor,” says Dr. Michael Silverman, Lawson Scientist and Chair/Chief of Infectious Diseases at LHSC and St. Joseph’s Health Care London. “We believe that by giving people a fecal transplant, we can change the bacteria that live within the tumor and gut and then optimize the immune response to both the tumour and to treatment, with the goal of improving patient outcomes.”
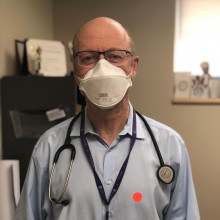
Dr. Michal Silverman, Lawson Associate Scientist
Fecal transplants involve collecting stool from a healthy donor, preparing it in a lab and safely transplanting it to the patient, in this case with a capsule. The goal is to transplant the donor’s microbiome so that healthy bacteria will colonize in the patient’s gut. “If you think of microbiome, each bacterium is like a little factory and all together they are a giant factory within us producing things we need,” explains Dr. Jeremy Burton, Lawson Scientist who specializes in human microbiome research. “Over time, a person’s diet, medications, and lifestyle can change the microbiome and it can have a big impact to the rest of our body.”
The research team was recently awarded a $450,000 Catalyst 2021 grant from the Weston Family Foundation to conduct this study, which is the first in the world focusing on prospectively modifying the microbiome in pancreatic cancer patients for treatments and outcomes.
“We normally don’t see this in one study where we go through the full spectrum of learning from patients, to looking at treatments, and then moving to a final intervention stage,” explains Dr. Maleki. “This has not been tried in pancreatic cancer before, but we think leveraging the microbiome and improving the immune response can potentially move the needle in this patient population.”
The team is recruiting both pancreatic cancer patients, as well as healthy volunteers for fecal transplant samples. Those interested in helping with fecal transplant donations can contact Dr. Seema Parvathy at 519-646-6100 ext. 61726 or email seemanair@@email
New transportation resource for youth in crisis
LONDON, ON – Transitional aged youth in Middlesex County now have access to a free transportation resource to access mental health services. Called the County Transport initiative, it will help youth ages 16 to 25 in Lucan, Parkhill, Exeter and Strathroy-Caradoc get the mental health care they need, when they need it.
County Transport is being coordinated by MINDS of London-Middlesex, a program of Lawson Health Research Institute, in partnership with the Canadian Mental Health Association (CMHA) of Elgin-Middlesex, Star Taxi and Middlesex County through the Lucan and Parkhill Libraries.
“Through our collaborative work, we’ve heard from many youth that transportation is a barrier for them when trying to access mental health services when in crisis. Youth in rural areas find this very challenging since most services are not close to their location,” says Romaisa Pervez, Research Assistant at MINDS of London-Middlesex.
MINDS, a Mental Health INcubator for Disruptive Solution, is a social innovation lab with a mission to address the complexity of the mental health care system. Youth with lived experience, community members and researchers work together to understand and help those living with mental health challenges in London-Middlesex by designing, piloting and testing innovative solutions developed locally.
“We do not have the exact numbers of Transitional Aged Youth (TAY) living in rural Middlesex who would benefit from access to the County Transport Initiative, but we know that mental health services in rural communities are limited and that access to the services available in larger city centres is challenging due to transportation difficulties,” explains Cathy Burghardt-Jesson, Warden for Middlesex County. “Transportation from Middlesex to London, where the majority of mental health resources are located, is underdeveloped as there are limited bus routes and schedules. This leaves little in the way of affordable transit options for TAY in crisis.”
Youth in crisis who connect with CMHA’s Reach Out 24/7 line at www.reachout247.ca or by phone at 519-433-2023 will be supported and assessed by the Crisis Line staff. If it is determined that a visit to the London Crisis Centre is needed, the CMHA Crisis worker will ensure a smooth transition from the Crisis Line to the Star Taxi Service. The youth will be provided with free transportation to and from CMHA’s Mental Health and Addictions Crisis Centre located at 648 Huron Street.
To ensure the safety and wellbeing of the youth accessing this service, Star Taxi drivers have received training developed by CMHA regarding mental health and crisis de-escalation, as well as suicide prevention training by Living Works.
Funding for the initiative has been provided by St. Joseph’s Health Care Foundation and the generous support of individual donors in the community.
“With additional funding, the initiative could be scaled up to reach as many youth as possible in Middlesex County and beyond. We want to see all youth in rural areas who want to access mental health services able to do so, by removing the barriers of location and transportation,” adds Pervez. They will be collecting information regarding use of the transportation service and youth experience to refine and improve the initiative.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New transportation resource for youth in crisis
Transitional aged youth in Middlesex County now have access to a free transportation resource to access mental health services. Called the County Transport initiative, it will help youth ages 16 to 25 in Lucan, Parkhill, Exeter and Strathroy-Caradoc get the mental health care they need, when they need it.
County Transport is being coordinated by MINDS of London-Middlesex, a program of Lawson Health Research Institute, in partnership with the Canadian Mental Health Association (CMHA) of Elgin-Middlesex, Star Taxi and Middlesex County through the Lucan and Parkhill Libraries.
“Through our collaborative work, we’ve heard from many youth that transportation is a barrier for them when trying to access mental health services when in crisis. Youth in rural areas find this very challenging since most services are not close to their location,” says Romaisa Pervez, Research Assistant at MINDS of London-Middlesex.

Romaisa Pervez, Research Assistant at MINDS of London-Middlesex, is leading the County Transport initiative.
MINDS, a Mental Health INcubator for Disruptive Solution, is a social innovation lab with a mission to address the complexity of the mental health care system. Youth with lived experience, community members and researchers work together to understand and help those living with mental health challenges in London-Middlesex by designing, piloting and testing innovative solutions developed locally.
“We do not have the exact numbers of transitional aged youth living in rural Middlesex who would benefit from access to the County Transport Initiative, but we know that mental health services in rural communities are limited and that access to the services available in larger city centres is challenging due to transportation difficulties,” explains Cathy Burghardt-Jesson, Warden for Middlesex County.
“Transportation from Middlesex to London, where the majority of mental health resources are located, is underdeveloped as there are limited bus routes and schedules. This leaves little in the way of affordable transit options for youth in crisis.”
Youth in crisis who connect with CMHA’s Reach Out 24/7 line at www.reachout247.ca or by phone at 519-433-2023 will be supported and assessed by the Crisis Line staff. If it is determined that a visit to the London Crisis Centre is needed, the CMHA Crisis worker will ensure a smooth transition from the Crisis Line to the Star Taxi Service. The youth will be provided with free transportation to and from CMHA’s Mental Health and Addictions Crisis Centre located at 648 Huron Street.
To ensure the safety and wellbeing of the youth accessing this service, Star Taxi drivers have received training developed by CMHA regarding mental health and crisis de-escalation, as well as suicide prevention training by Living Works.
Funding for the initiative has been provided by St. Joseph’s Health Care Foundation and the generous support of individual donors in the community.
“With additional funding, the initiative could be scaled up to reach as many youth as possible in Middlesex County and beyond. We want to see all youth in rural areas who want to access mental health services able to do so, by removing the barriers of location and transportation,” adds Pervez.
They will be collecting information regarding use of the transportation service and youth experience to refine and improve the initiative.
Open Access Publications
The HULC Clinical Research Laboratory publishes a number of papers every year to share the important findings of our studies. The following are a list of open-access publications that anyone can access to read.
View open-access publications in the following categories:
Neck/Shoulder
- Appraisal of Clinical Practice Guideline: Management of Neck Pain
- The Contribution of Health and Psychological Factors in Patients with Chronic Neck Pain and Disability: A Cross-sectional Study
- Appraisal of: Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa)
- Design and implementation of the 2012 Canadian shoulder course for senior orthopedic residents
- Efficacy of workplace interventions for shoulder pain: A systematic review and meta-analysis
- A qualitative description of chronic neck pain has implications for outcome assessment and classification
- Does Deep Cervical Flexor Muscle Training Affect Pain Pressure Thresholds of Myofascial Trigger Points in Patients with Chronic Neck Pain? A Prospective Randomized Controlled Trial
- Psychophysical and Patient Factors as Determinants of Pain, Function and Health Status in Shoulder Disorders
- Intra and Inter-Rater Reliability and Convergent Validity of FIT-HaNSA in Individuals with Grade П Whiplash Associated Disorder
- Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis
- Manual therapy with exercise for neck pain
- The effect of pressure pain sensitivity and patient factors on self-reported pain-disability in patients with chronic neck pain
- Validity of pain and motion indicators recorded on a movement diagram of shoulder lateral rotation
- The kinematics of upper extremity reaching: a reliability study on people with and without shoulder impingement syndrome
- What is a successful outcome following reverse total shoulder arthroplasty?
- Rotational strength, range of motion, and function in people with unaffected shoulders from various stages of life
- Validation of a new test that assesses functional performance of the upper extremity and neck (FIT-HaNSA) in patients with shoulder pathology
- Cross-sectional and longitudinal construct validity of two rotator cuff disease-specific outcome measures
- The Shoulder Pain and Disability Index demonstrates factor, construct and longitudinal validity
- Suppl 4: What is the Experience of Receiving Health Care for Neck Pain?
- A Description of the Methodology Used in an Overview of Reviews to Evaluate Evidence on the Treatment, Harms, Diagnosis/Classification, Prognosis and Outcomes Used in the Management of Neck Pain
- What Does ‘Recovery’Mean to People with Neck Pain? Results of a Descriptive Thematic Analysis
- Suppl 4: An Overview of Systematic Reviews on Prognostic Factors in Neck Pain: Results from the International Collaboration on Neck Pain (ICON) Project
- Suppl 4: An ICON Overview on Physical Modalities for Neck Pain and Associated Disorders
- Suppl 4: Editorial: Management of Neck Pain
- Suppl 4: Pharmacological Interventions Including Medical Injections for Neck Pain: An Overview as Part of the ICON Project
- Suppl 4: Knowledge Translation Tools are Emerging to Move Neck Pain Research into Practice
- Suppl 4: The Relationship Between Neck Pain and Physical Activity
- Suppl 4: Psychological Care, Patient Education, Orthotics, Ergonomics and Prevention Strategies for Neck Pain: An Systematic Overview Update as Part of the ICON Project
- Suppl 4: Use of Outcome Measures in Managing Neck Pain: An International Multidisciplinary Survey
- Suppl 4: Results of an International Survey of Practice Patterns for Establishing Prognosis in Neck Pain: The ICON Project
Elbow
- Patient reported pain and disability following a distal radius fracture: a prospective study
- Patient-rated tennis elbow evaluation questionnaire
- Radial nerve mobilization reduces lateral elbow pain and provides short-term relief in computer users
- Pain and disability reported in the year following a distal radius fracture: a cohort study
- The patient-rated elbow evaluation (PREE)
- A survey of practice patterns for rehabilitation post elbow fracture
Wrist/Hand
- The Patient Rated Wrist Evaluation (PRWE) was successfully translated into Tamil
- Provocative maneuvers demonstrate excellent accuracy in the “virtual” diagnosis of carpal tunnel syndrome among people with upper limb conditions—a short technical report
- Rasch Analysis of The Patient-Rated Wrist Evaluation Questionnaire
- The Impact of Sensory, Motor and Pain Impairments on Patient-Reported and Performance Based Function in Carpal Tunnel Syndrome
- Is casting for non-displaced simple scaphoid waist fracture effective? A CT based assessment of union
- Reliability and validity of electro-goniometric range of motion measurements in patients with hand and wrist limitations
- Evaluation of an Image-Based Tool to Examine the Effect of Fracture Alignment and Joint Congruency on Outcomes after Wrist Fracture
- A hand brace improve symptoms and function in carpal tunnel syndrome
Work/Nerve/Other
- Agreement and participants’ preferences comparing: self-rated falls risk questionnaire (FRQ) and activities-specific balance confidence (ABC) scale in community-dwelling older adults using the Bland–Altman method
- Psychometric Properties of The Zephyr Bioharness Device: A Systematic Review
- Clinimetrics: Upper Extremity Functional Index
- Appraisal of Clinical Practice Guideline: American Academy of Orthopaedic Surgeons Clinical Practice Guideline on the Management of Osteoarthritis of the Hip
- Education and Social Support as Key Factors in Osteoarthritis Management Programs: A Scoping Review
- The relationship between physical fitness and simulated firefighting task performance
- Pain-QuILT: A user-friendly tool for the self-report and tracking of pain
- Prevalence and distribution of musculoskeletal disorders in firefighters are influenced by age and length of service
- Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis
- Correction to: Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature
- Depicting individual responses to physical therapist led chronic pain self-management support with pain science education and exercise in primary health care: multiple case studies
- Measurement properties of painDETECT: Rasch analysis of responses from community-dwelling adults with neuropathic pain
- A therapist-focused knowledge translation intervention for improving patient adherence in musculoskeletal physiotherapy practice
- Appraisal of: Role of physical therapists in the management of individuals at risk for or diagnosed with venous thromboembolism: Evidence-based clinical practice guideline
- Evaluating the design and reporting of pragmatic trials in osteoarthritis research
- Assessing reading levels of health information: uses and limitations of flesch formula
- Corrigendum to “Risk Factors for Falls and Fragility Fractures in Community-Dwelling Seniors: A One-Year Prospective Study
- Órteses para o paciente com osteoartrite do polegar: o que os terapeutas ocupacionais no Brasil indicam?
- Muscle strength differences in healthy young adults with and without generalized joint hypermobility: a cross-sectional study
- Evaluating and optimizing pragmatic trial design in osteoarthritis research
- Reliability of three landmarking methods for dual inclinometry measurements of lumbar flexion and extension
- Beyond silence: protocol for a randomized parallel-group trial comparing two approaches to workplace mental health education for healthcare employees
- A modified evidence-based practice- knowledge, attitudes, behaviour and decisions/outcomes questionnaire is valid across multiple professions involved in pain management
- Scoping review of patient-centered care approaches in healthcare
- Evidence-informed recommendations for rehabilitation with older adults living with HIV: a knowledge synthesis
- Fall efficacy scale-international (FES-I)
- Too Fit To Fracture
- Knee osteoarthritis
- The reliability and validity of the computerized double inclinometer in measuring lumbar mobility
- Development and initial validation of the Satisfaction and Recovery Index (SRI) for measurement of recovery from musculoskeletal trauma
- Translation of Oswestry Disability Index into Tamil with Cross Cultural Adaptation and Evaluation of Reliability and Validity
- The work limitations questionnaire (WLQ-25)
- Ice-water (cold stress) immersion testing
- Development and validation of the patient-rated ulnar nerve evaluation
- Reliability and validity of the AGREE instrument used by physical therapists in assessment of clinical practice guidelines
- The quality of websites addressing fibromyalgia: an assessment of quality and readability using standardised tools
- The ten test for sensation
- Advanced practice physiotherapy in patients with musculoskeletal disorders: a systematic review
Over $10 million in funding announced from CIHR
Health researchers from across London were awarded more than $10 million from Canadian Institutes of Health Research (CIHR), with $2.8 million through Lawson Health Research Institute and $7.3 million through Schulich Medicine & Dentistry. A total of 15 projects were funded.
CIHR’s Project Grant program is designed to capture ideas with the greatest potential for important advances resulting in the creation of new knowledge and its translation into improved health and health care for Canadians.
Congratulations to all of the successful applicants!
Projects through Lawson Health Research Institute:
Karen Bosma, and Laurent Brochard: “Proportional Assist Ventilation for Minimizing the Duration of Mechanical Ventilation: The PROMIZING Study.”
Critically ill patients frequently require the life-sustaining technology of mechanical ventilation, but prolonged use can place patients at risk for long-term functional impairment and increased mortality, and is also costly to the health care system.
The PROMIZING Study is an international, multi-centre randomized clinical trial that will identify ways to reduce the duration of mechanical ventilation for patients at greatest risk and to determine whether a novel mode of ventilation developed in Canada could replace the standard of care.
“It is vital that Canada continue to invest in high impact, hospital-based research such as the PROMIZING study which enable researchers to develop and test treatments, technologies, and procedures that will improve clinically relevant, patient-important outcomes while also improving the efficiency of our healthcare system.” – Dr. Karen Bosma
Diane Bryant, and Alan Getgood: “Anterior Cruciate Ligament Reconstruction using Bone Patellar Bone or Quad Tendon Autograft with or without Lateral Extra Articular Tenodesis in Individuals who are at High Risk of Graft Failure (STABILITY II)”
Anterior cruciate ligament reconstruction (ACLR) is complicated by high failure rates in young active individuals, which is associated with worse outcomes and higher rates of osteoarthritis.
Currently, there are different types of grafts being used to rebuild a torn ACL. There is a need to evaluate whether one method is better at reducing failure, minimizing complications and creating better outcomes in terms of functional performance. This study will determine the best graft choice for young patients at risk of ACLR failure which will ultimately lead to positive effects on activity and quality of life.
Patrick Luke and Rabindra Bhattacharjee: “Therapeutic potential of bloodless oxygenated perfusion of donor kidneys for prolonged storage and protection for transplantation.”
Kidney failure among Canadians has tripled over the last 20 years. Transplantation improves the quality of life and survival of patients at a much lower cost than dialysis. However, only 40 per cent of patients receive functional kidneys due to lack of living organ donors.
To increase the number of kidneys available for transplantation, surgeons are accepting orgrans from deceased donors. Currently, during storage, the organs can suffer injuries from a lack of oxygen as well as cold temperatures and the conditions are not conducive to use drugs that can prevent damage.
The study is looking at the effects of a bloodless oxygen carrying perfusion liquid that will allow the storage of human donor kidneys for long periods of time at room temperature, and will also evaluate if certain drugs can maximize the preservation of these organs.
“Hospital-based research institutes are uniquely positioned to conduct patient-centred research. Investment through CIHR supports the physicians and researchers who are committed to improving treatments for patients at the front line of care.” – Dr. Patrick Luke
Emil Schemitsch: “The DECIPHER Study: DEterminants of Function and Clinically Important outcomes in Proximal Humerus Fractures in the Elder Population: A National CohoRt.”
Shoulder fractures are becoming increasingly common for older adults and cause considerable limitations and impacts for their daily life. While different approaches are taken to treat shoulder fractures, there is a lack of knowledge and evidence to show which of those methods are the most effective and for which patients.
The DECIPHER study will seek to answer important questions about which treatment and rehabilitation strategies are best for different patients, strengthening the clinical strategy for managing these difficult and prevalent injuries. It will also provide an economic analysis to understand the impact for healthcare system costs.
“Such an analysis has the potential to significantly affect patient care and Canadian practice patterns, as well as inform the development of future pivotal clinical trials. DECIPHER will have an important impact on patient care, health system costs and future research directions locally, nationally and internationally.” - Dr. Emil Schemitsch.
Projects through Schulich Medicine & Dentistry:
Subrata Chakrabarti, with collaborators Bekim Sadikovic, Krishna Singh, and Stephanie Frisbee: “Novel mechanisms in diabetic cardiomyopathy.”
Peter Chidiac and Jeffrey Dixon: “Allosteric regulation of GPCR signaling by extracellular nucleotides.”
Bryan Heit: “Role of ELKS1 and Rab17 in Differential Antigen Sorting and MHC II Trafficking Following Efferocytosis and Phagocytosis.”
Marlys Koschinsky and Michael Boffa: “B Apo(a):apoB100 interactions as key determinants of Lp(a) biosynthesis.”
Shawn Li: “Novel anticancer immunotherapy targeting the molecular mechanisms of T cell suppression by immune checkpoints.”
Julio Martinez‐Trujillo and Michael Poulter: “Reverse engineering working memory circuits in the primate brain: Implications for the study of memory deficits.”
Maria Mathews and Jennifer Shea with collaborators, Ivy Bourgeault, Emily Marshall, Amy Bombay, Nicole Doria, Julia Lukewich, and Amanda Myers: “Increasing Indigenous Participation in the Physician Workforce.”
Charles McKenzie, and Timothy Regnault: “Hyperpolarised 13C MRI of Placental Metabolism in Intrauterine Growth Restriction.”
Marco Prado: “A Regulation of chaperone‐mediated proteostasis by STI1.”
Lloy Wylie and Lana Ray with collaborators Christopher Mushquash, Victoria Smye, Nadine Wathen, Cheryl Forchuk, and Brock Pitawanakwat: “Educating for Equity: Building Culturally Safe Care through Indigenous Narratives.”
Xiufen Zheng: “The role of circular RNA in heart transplantation”