Search
Search
Standing up to falls
By merging world class care with research and artificial intelligence, St. Joseph’s Health Care London is catching falls before they happen.
They wreak havoc on independence and well-being, making them one Canada’s most pressing health challenges: falls.
A leading cause of injury-related hospitalizations, even death, among older adults, a fall can happen anytime, anywhere – with 50 per cent occurring at home. But what if we could predict and prevent falls before they happen?
A pioneering initiative at St. Joseph’s Health Care London (St. Joseph’s) is doing just that. The 3FM Clinic, short for Falls, Fractures, Frailty and Mobility, at St. Joseph’s Parkwood Insitute is at the leading edge of falls prevention in Canada, integrating research with clinical practice to offer hope and practical solutions to older adults.
Led by St. Joseph’s geriatrician Dr. Jaspreet Bhangu and Western University rehabilitation scientist and physiotherapist Janelle Unger, PhD, the visionary 3FM Clinic is working to prevent falls before they happen.
“We know there are a number of factors that can cause an older adult to fall such as illness, medication side effects, balance and gait issues, cognitive impairment, visual changes and environmental hazards,” says Bhangu. “What we’re working to understand is how those factors together impact individual patients and their risk of falling.”
To do so, the 3FM Clinic team – one of the largest, most diverse teams of its kind in the country – completes a multi-step evaluation of patients:
- Nurses gather their medical history, current medications, functional abilities and personal goals.
- Physical therapists measure the patient’s gait (how they walk) and balance to understand their physical capabilities.
- Occupational therapists test their vision, cognitive function and identify issues that might hinder the individual’s ability to perform routine tasks safely.
- A geriatrician focuses on medical risk factors such as bone health, medications and cardiovascular health to help manage risks associated with aging. The team then creates a customized care plan that incorporates exercises, therapeutic interventions and educational strategies.
On the research side, Unger and her team in the RED Neuro Lab at St. Joseph’s Gray Centre for Mobility and Activity are leveraging artificial intelligence (AI) to predict falls more accurately.
“Traditional fall prediction models often rely on limited data and lack real-world input from clinicians and patients,” explains Unger. “By partnering with Bhangu and the clinical team, as well as the patients in the 3FM Clinic, we’re able to integrate clinical information with biomechanical data collected from wearable sensors known as inertial measurement units (IMUs).”
An IMU is a device that tracks and measures a person’s movement and orientation and provides valuable data on how that person moves and stays stable.
“We plan to use AI to analyze the data collected through the IMU’s and are working to create accurate fall prediction models,” says Unger. “This research, funded by Western’s Bone and Joint Institute, has the potential to improve care decisions, enhance preventive strategies and ultimately reduce the incidence of fall-related injuries and hospitalizations for our patients and people across the globe.”
By embracing innovative research and compassionate care, the 3FM Clinic is a model for future efforts in fall prevention and geriatric care, offering a safer, more independent future for older adults.
You can prevent falls too:
- Use assistive devices: Properly fitted walkers or canes provide essential support and stability.
- Fitted footwear: Shoes (not slippers or flip-flops) with appropriate tread and low heels help prevent slips and falls. They should also fit your feet.
- Home improvements: Improved lighting, clear walkways and assistive bathroom fixtures.
- Exercise: Participate in strength and balance exercises to enhance physical fitness.
- Medication reviews: Regularly have your medications reviewed to identify if you are at risk of falling.
Study casts doubt on clinical significance of gadolinium brain deposits
A new study from Lawson Health Research Institute and the Institute for Clinical Evaluative Sciences (ICES) has cast doubt on the clinical significance of brain deposits of gadolinium (a chemical contrast agent commonly used to enhance MRI imaging).
In 2015, the US Food and Drug Administration raised safety concerns over reports of retained gadolinium in the brain for patients undergoing four or more gadolinium-enhanced MRIs. The FDA launched an inquiry at the time, stating that “it is unknown whether these gadolinium deposits are harmful.” Pending further investigation, the FDA suggested limiting the use of gadolinium-based contrast agents (GBCAs) to circumstances where contrast information is clinically necessary, and to evaluate the need for repetitive GBCA MRIs based on treatment protocols.
Studies since that time have shown deposits of gadolinium may be found long after they are administered. They tend to concentrate in the globus pallidi, a region of the brain that can cause parkinsonian symptoms if it is damaged. Parkinson’s disease is an example of a specific brain disorder that is commonly associated with parkinsonian symptoms.
“Given the concern around possible neurotoxicity of gadolinium, and because these deposits were found in the globus pallidi region of the brain, we wanted to see if people exposed to gadolinium MRIs have higher rates of subsequent parkinsonism,” says Dr. Blayne Welk, the lead author of the study who is an adjunct scientist with ICES Western and Lawson.
To test a possible link between GBCAs and parkinsonism, Welk and his team examined anonymized health care records for 246,557 patients in Ontario over the age of 66 who underwent an initial MRI in a 10-year period between 2003 and 2013. They excluded patients whose initial MRI was of the brain or spinal cord and those with prior parkinsonism or neurosurgery. Comparing patients who were exposed to gadolinium-enhanced MRIs with patients whose MRIs did not include gadolinium enhancement, they looked for differences in rates of future parkinsonism symptoms or treatment.
They found that the rates of parkinsonism for exposed vs non-exposed patients were virtually identical, at 1.2 per cent. These findings indicate that there is no increased risk for parkinsonism associated with the use of gadolinium in MRIs.
However, the researchers caution that this study does not clear up all the worries about gadolinium, since they investigated only its connection to parkinsonism.
“While these findings should be reassuring for patients and their care providers that gadolinium exposure does not appear to be associated with higher risk of developing parkinsonism symptoms, there have been other reports of nonspecific neurologic symptoms including pain and cognitive changes associated with prior gadolinium exposure which do require further study,” comments Dr. Welk.
The researchers also note that gadolinium may have different effects in younger patients (who were not included in this study), or in those with neurologic diseases (who may have been excluded based on the types of MRIs included in this study).
“Association between Gadolinium contrast exposure and the risk of parkinsonism” was published on July 5, 2016 in the journal JAMA.
Author block: Blayne Welk, Eric McArthur, Sarah A. Morrow, Penny MacDonald, Jade Hayward, Andrew Leung, Andrea Lum.
Study gives Ontario men access to advanced prostate cancer imaging
Prostate cancer can be elusive.
Wayne Smith’s journey with prostate cancer began 16 years ago when his family physician noticed increasing levels of prostate specific antigen (PSA) in his blood. PSA is a protein expressed by the prostate. A blood test is used to monitor levels of the protein as a screening tool for prostate cancer.
“My doctor referred me to Dr. Stephen Pautler, Urologist at St. Joseph’s Health Care London. Although we did a number of tests, we weren’t able to locate any spots of cancer,” says Wayne, a 71-year-old man from Ingersoll, Ontario. “We were able to manage my PSA levels for a number of years until they jumped up too high.”

Above: Wayne Smith
In 2012, Wayne was sent for a CT scan. This test finally revealed spots of cancer at the back of the prostate. “Dr. Pautler discussed my treatment options with me and I chose to have surgery to remove my prostate,” explains Wayne. “The team did a great job but we eventually realized some cancer remained. I asked about a PET scan to locate it but the technology was not available at that time.”
After consulting with Dr. Pautler and Dr. Glenn Bauman, Radiation Oncologist at London Health Sciences Centre, Wayne chose to postpone further treatment and monitor the cancer over time. It was undetectable for five years before his PSA levels started rising again. Earlier this year, the levels doubled.
“I was told a PET scan was available through research and that it could help locate the disease,” says Wayne. He went for the scan earlier this year at St. Joseph’s Hospital, part of St. Joseph’s Health Care London. “Nothing showed up on the scan, but that was good news; it meant the cancer was microscopically small.”
The PET scan helped Wayne and his care team in making decisions about his treatment. They decided on hormone therapy and radiation therapy to hopefully eradicate any cancerous cells. He was treated at London Health Sciences Centre’s (LHSC) London Regional Cancer Program.
“Early evidence suggests that a clear PET scan despite rising PSA levels is likely associated with persistent cancer at the original site,” explains Dr. Glenn Bauman, Lawson Scientist and Radiation Oncologist at LHSC. “Based on the scan, Wayne was able to do a much shorter round of hormone therapy – six months rather than being on hormone therapy indefinitely.”
“After the first hormone treatment, my PSA levels dropped significantly. With the added radiation, we’re confident this will be the end of my battle with prostate cancer,” says Wayne, who is currently enjoying retired life by spending time with his wife, two children and five grandkids. “Despite my diagnosis and treatments, I carried on with my life. I did what I had to do but still went places on weekends, did chores around the house and went golfing.”

Above: Dr. Glenn Bauman (left) and Wayne Smith (right)
Wayne is one of 1,500 Ontario men who will participate in the PSMA-PET Registry Trial. Led by researchers at Lawson Health Research Institute, the multi-centre registry trial is testing the use of a new imaging tracer, called a PSMA tracer, for early detection of recurrent prostate cancer. The registry gives patients access to a new type of imaging and will assess the impact on patient care.
PSMA tracers are used in positron emission tomography (PET) scans to target a protein found in prostate cancer cells called prostate specific membrane antigen (PSMA). Supported by Cancer Care Ontario and McMaster University’s Centre for Probe Development and Commercialization (CPDC), the goal of the registry trial is to capture detailed PET images to guide treatment decisions made by patients and their care teams.
Eligible participants are those with suspected prostate cancer that cannot be detected in conventional bone and CT scans. Participants have a PET scan using a specific PSMA tracer called 18F-DCFPyL. The tracer is injected and spreads out in the body to find spots of cancer which are then visible on the scan.
“With this trial, men in Ontario can access a promising test that could impact their treatment outcomes,” says Dr. Bauman. “The PSMA tracer may be able to locate prostate cancer that was once undiscoverable.”
Led by Dr. Bauman along with Drs. Ur Metser and Tony Finelli at University Health Network (UHN), the trial is currently available across multiple sites in Ontario: London Health Sciences Centre; St. Joseph’s Health Care London; St. Joseph’s Health Care Hamilton; Sunnybrook Health Sciences Centre; Princess Margaret Cancer Centre (UHN); and Thunder Bay Regional Health Sciences Centre. The trial is also expected to open at The Ottawa Hospital this year.
The PSMA tracer is considered an investigational agent in Canada and is currently only available through clinical trials. After studying the accuracy of the tracer in detecting early cancer recurrence, the research team hopes to have enough data to recommend when it could be used in the clinic.
Patients from London, Ontario and region who are enrolled in the PSMA-PET Registry Trial have their scans performed at St. Joseph's Hospital. In 2016, Lawson researchers were the first in Canada to use the 18F-DCFPyL PSMA tracer to capture PET images with a patient at St. Joseph’s Hospital. The tracer is provided by CanProbe, a joint venture between CPDC and UHN located in Toronto, and was set up with funding from the Movember Foundation.
“We conducted an initial trial that included 20 men with prostate cancer who were having their prostate removed. The goal was to determine how effective the PSMA probe was in detecting disease at the time of initial treatment,” explains Dr. Bauman. “We found the PET scan was able to detect spots of cancer in almost all participants, which corresponded to spots of cancer identified in the prostate after it was removed and examined under the microscope.”
The initial trial was made possible with donor funding through London Health Sciences Foundation, which provided initial funding to hire Research Associate, Catherine Hildebrand, who set up citywide cancer imaging workshops and helped the team prepare successful grant applications to secure key funding from CIHR and OICR.
Dr. Bauman notes that conventional imaging tests like bone scans and computed tomography (CT) are not always effective for detecting prostate cancer. While other PET probes can be used to detect a number of different cancer types, they are unable to identify prostate cancer. The PSMA probe opens new avenues for prostate cancer diagnosis, prognosis and treatment guidance.
For patients like Wayne Smith, access to this advanced imaging is critically important.
“It’s fantastic we have access to this PET scan. It certainly gave me relief knowing nothing showed up on the scan and that, even if something did, it would light up to show us where to treat,” says Wayne. “I know PET scans are used for other cancers too and I think they’re imperative. They give you more of a chance through knowledge of where the disease is located.”

Study identifies biomarkers that could be used in a quick, inexpensive COVID-19 blood screening tool
LONDON, ONTARIO - A new study from Lawson Health Research Institute, Western University and University of Alberta suggests that COVID-19 affects the human body’s blood concentration levels of specific metabolites – small molecules broken down in the human body through the process of metabolism. Three specific metabolites identified in this study could act as biomarkers and one day be measured through an inexpensive blood test to quickly screen patients for the disease and predict which patients will become most critically ill. The team also suspects those metabolites depleted by the virus could be delivered to patients as dietary supplements, acting as a secondary therapy. Published in Critical Care Explorations, the early findings add to the research team’s growing body of evidence on the bodily changes caused by the SARS-CoV-2 virus.
“As the second wave progresses and COVID-19 cases rise, there is an overwhelming demand for testing,” says Dr. Douglas Fraser, lead researcher from Lawson and Western’s Schulich School of Medicine & Dentistry, and Critical Care Physician at London Health Sciences Centre (LHSC). “While our findings need to be confirmed in a larger group of patients, they could lead to a rapid, cost-effective screening tool as a first line of testing in the community and in-hospital.”
The study was conducted by performing metabolomics profiling on blood samples from 30 participants at LHSC: 10 COVID-19 patients and 10 patients with other infections admitted to LHSC’s ICU, as well as 10 healthy control participants. Samples were sent to The Metabolomics Innovation Centre (TMIC) at University of Alberta where a team measured plasma concentrations of 162 metabolites.
“Metabolites are the final breakdown products in the human body and play key roles in cellular activity and physiology. By studying them, we can understand chemical processes that are occurring at any given moment, including those that regulate biological functions related to health and disease,” explains Dr. David Wishart, Codirector of TMIC and Professor of Biological Sciences, Computing Science and Laboratory Medicine & Pathology with the University of Alberta. “Because the human metabolome responds very quickly to environmental factors like pathogens, metabolomics can play an important role in early-stage disease detection, including for COVID-19.”
The team discovered four metabolites of importance to COVID-19 disease detection. The concentration of one metabolite called kynurenine was elevated in COVID-19 patients while concentrations of the other three metabolites (arginine, sarcosine and lysophosphatidylcholines) were decreased. After further analysis, they discovered that by studying the concentrations of only two metabolites – kynurenine and arginine – they could distinguish COVID-19 patients from healthy participants and other critically ill patients with 98 per cent accuracy.
The team also discovered that concentrations of two metabolites (creatinine and arginine) could be used to predict which critically-ill COVID-19 patients were most at risk of dying. When measured on a patient’s first and third day in ICU, these metabolites predicted COVID-19-associated death with 100 per cent accuracy.
“It’s our hope these findings can be validated in larger patient populations and then used to develop a simple blood test that shows high likelihood of infection and disease severity, providing rapid results in as little as 20 minutes,” explains Dr. Fraser. “This could ease the demand for current testing methods, perhaps being used as a portable, first-line screening tool in the community and for when undiagnosed patients present to hospital.”
The team also notes the reduction of key metabolites reflects changes to biochemical pathways or functions in the body which are important to maintaining health and fighting disease. They suggest their findings warrant further study to determine whether certain metabolites could be boosted through dietary supplements. A precision health approach like this could lead to repaired biochemical pathways and improved disease outcomes.
“Providing dietary supplements could be a simple adjunctive or secondary therapy with meaningful outcomes,” says Dr. Fraser. “For example, the metabolite arginine is essential to tissue repair while the metabolite sarcosine activates a process to remove damaged cells. Knowing that COVID-19 causes hyperinflammation that can damage cells and tissue, particularly in the lungs, supporting these processes may prove critical.”
In an earlier study, the team was the first to profile the body’s immune response to the SARS-CoV-2 virus and discover six potential therapeutic targets to improve outcomes. In other studies, they have discovered additional biomarkers that could be used to predict how severely ill a COVID-19 patient will become and uncovered a mechanism causing blood clots in COVID-19 patients and potential ways to treat them.
“We’re working to uncover hard evidence about how the virus invades the body. Ultimately, we hope our combined findings can lead to faster diagnosis, ways to identify patients most at risk of poor outcomes and targets for novel treatments,” notes Dr. Fraser.
This study was made possible through generous donor support. London Health Sciences Foundation is the lead funder with an investment of $90,800 through a significant estate donation and existing funds. Additional funding came from Lawson, Western and the AMOSO Innovation Fund.
-30-
DOWNLOADABLE MEDIA


Dr. Douglas Fraser, Researcher from Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry

Dr. David Wishart, Codirector of TMIC and Professor of Biological Sciences, Computing Science and Laboratory Medicine & Pathology with the University of Alberta
TMIC is a nationally funded core facility which provides cutting edge metabolomics technologies, service and data resources to the research community. TMIC’s unique combination of infrastructure and scientific expertise allow for a wide range of tools for comprehensive and targeted metabolomics studies. For more information, visit www.metabolomicscentre.ca.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
The University of Alberta in Edmonton is one of Canada's top teaching and research universities, with an international reputation for excellence across the humanities, sciences, creative arts, business, engineering and health sciences. Great ideas change the world, but ideas need a push forward. At the University of Alberta, we know that push has never been more important as we do our part to keep doors of opportunity open to all. We're making research discoveries. We’re cultivating entrepreneurs. And we’re giving our students the knowledge and skills they need to turn today's ideas into tomorrow's innovations.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study is first to identify potential therapeutic targets for COVID-19
LONDON, ONTARIO - A team from Lawson Health Research Institute and Western University are the first in the world to profile the body’s immune response to COVID-19. By studying blood samples from critically ill patients at London Health Sciences Centre (LHSC), the research team identified a unique pattern of six molecules that could be used as therapeutic targets to treat the virus. The study is published this week in Critical Care Explorations.
Since the pandemic’s start there have been reports that the immune system can overreact to the virus and cause a cytokine storm – elevated levels of inflammatory molecules that damage healthy cells.
“Clinicians have been trying to address this hyperinflammation but without evidence of what to target,” explains Dr. Douglas Fraser, lead researcher from Lawson and Western’s Schulich School of Medicine & Dentistry and Critical Care Physician at LHSC. “Our study takes away the guessing by identifying potential therapeutic targets for the first time.”
The study included 30 participants: 10 COVID-19 patients and 10 patients with other infections admitted to LHSC’s intensive care unit (ICU), as well as 10 healthy control participants. Blood was drawn daily for the first seven days of ICU admission, processed in a lab and then analyzed using statistical methods and artificial intelligence (AI).
The research team studied 57 inflammatory molecules. They found that six molecules were uniquely elevated in COVID-19 ICU patients (tumor necrosis factor, granzyme B, heat shock protein 70, interleukin-18, interferon-gamma-inducible protein 10 and elastase 2).
The team also used AI to validate their results. They found that inflammation profiling was able to predict the presence of COVID-19 in critically ill patients with 98 per cent accuracy. They also found that one of the molecules (heat shock protein 70) was strongly associated with an increased risk of death when measured in the blood early during the illness.
“Understanding the immune response is paramount to finding the best treatments,” says Dr. Fraser “Our next step is to test drugs that block the harmful effects of several of these molecules while still allowing the immune system to fight the virus.”
The study was made possible with donor support to London Health Sciences Foundation. It also received additional funding from Lawson, Western and the AMOSO Innovation Fund.
-30-
DOWNLOADABLE MEDIA

Above: Blood samples from critically ill COVID-19 patients.

Above: A blood sample from a critically ill COVID-19 patient is collected at London Health Sciences Centre.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study offers hope for hard-to-treat type 2 diabetes
A landmark international study involving patients and researchers at St. Joseph’s Health Care London shows automated insulin pump delivery can be ‘life-changing’ for people with type 2 diabetes
Lisa Mercer had tried just about everything to regulate the ups and downs of her blood sugars, from a strict diet to medication to four-a-day-day insulin shots.
But her busy life with type 2 diabetes finally started to feel better when she enrolled in a clinical trial at St. Joseph’s Health Care London to test the effectiveness of a system that combined glucose monitoring with an automated insulin pump.
“It was life-changing for me. I was diagnosed with type 2 diabetes 25 years ago and my blood sugars have always been all over the map. I felt sort of helpless. I said yes to this clinical trial because I hoped it would return some normalcy to my life,” she says. Now that study, with results newly published in the prestigious New England Journal of Medicine, is being heralded as a big step forward for patients with hard-to-treat type 2 diabetes.
“This is an exciting finding because it shows we can improve patients’ blood sugars and hopefully prevent long-term negative consequences of high sugars while at the same time making it easier for patients to manage the disease,” says Dr. Tamara Spaic, Medical Director of St. Joseph’s Diabetes Education Centre and the lead Canadian researcher for the multi-site international study based at the Jaeb Center for Health Research in Tampa, Fla.
Study participants were placed either in a group testing the effectiveness of a new system called Control IQ+ or a control group continuing their existing diabetes management regimen.
The intervention group wore glucose monitors that electronically talked with high-tech pumps that delivered insulin – automatically, in the right dose and at the right time – with minimal patient input.
While the device was approved about five years ago for people with type 1 diabetes, this is the first examination of its effectiveness managing the complexities of type 2 diabetes.
“The biggest burden in diabetes control is that it’s 24/7 vigilance: did I eat or not; what did I eat and how much; did I exercise; do I need to wake up for an insulin shot in the middle of the night? This system largely removes those variables to bring blood sugars to target levels,” says Spaic, who is also a Lawson Research Institute scientist and professor of endocrinology and metabolism at Western University’s Schulich School of Medicine & Dentistry.
“What surprised us was that this worked so well across all populations regardless of duration of the disease, amount of insulin needed, whether they used other medications or not, whether they were tech-savvy or not. It worked for everyone regardless of their ethnicity, socioeconomics, and whether they were male or female, old or young,” she adds.
Researchers even asked participants in the intervention group to skip insulin with meals on occasion – generally a no-no in the highly regimented life of someone with insulin-managed diabetes – and the automated system responded appropriately and quickly to adjust blood sugars.
Mercer found improvement within a couple of weeks: “Before the pump, I felt awful. When my sugars were too low, I got the shakes, I had trouble communicating and thinking clearly and I got extremely tired. When my sugars were too high, I was exhausted. It dominated every day and was tough on my job as a police officer. Now I feel better. I feel more in control.
“Is it perfect? No. But my sugars are stable and consistent more often than not.”
Not yet approved in Canada
In February, the US Food and Drug Administration cleared the use of the Control IQ+ system in adults with type 2 diabetes – approval that also meant the expense could be covered through health insurance.
However, it has not yet been brought to Health Canada regulators for approval, Spaic says.
Even so, several of her patients, including Foster, decided to continue using the system after the 13-week trial, paying out-of-pocket or through private insurance.
Spaic and St. Joseph’s colleagues, endocrinologist Dr. Selina Liu and nurse coordinator Marsha Driscoll, were extensively involved in the design of the study, recruiting and monitoring participants and reporting results.
Diabetes type 2 usually develops in adulthood and is a condition in which body cannot make enough insulin or does not properly use the insulin it makes to regulate the amount of glucose (sugar) in the blood.
While most people with type 2 diabetes can control their blood sugars through lifestyle changes or with new treatments such as non-insulin glucose-lowering medications, the sub-set of North Americans who require insulin still numbers in the millions.
THE STUDY:
What: 13-week, large-scale clinical trial to test the effectiveness of a system combining automated insulin delivery with continuous glucose monitoring for people with type 2 diabetes.
Who: 319 study participants – including 13 at Lawson Research Institute of St. Joseph’s Health Care London – all needing multiple daily insulin doses. Age range 19 to 87, from 21 centres across the U.S. and Canada. Study led by Jaeb Centre for Health Research in Tampa, Fla., and funded by Tandem Diabetes Care, which also provided the automated insulin-delivery systems
How: Two-thirds of patients received an automated insulin pump, continuous glucose monitor and transmitter to track and automatically administer insulin to regulate their blood sugars. A control group continued their existing insulin-delivery method and also received glucose monitors.
Results: The intervention group had more stable blood sugar levels – with 3.4 more hours per day in the target glucose range – than the control group. Use of automated insulin devices was successful and safe even for patients without previous experience with an insulin pump
Why it matters: Automated insulin delivery can help insulin-dependent patients manage their type 2 diabetes better than before. Better management means improved quality of life and may result in fewer diabetes complications such as heart disease and damage to the eyes, kidneys and nerves.
Study testing benefit of antibodies from people recovered from COVID-19 on severe cases of infection
LONDON, ON – Researchers at Lawson Health Research Institute are taking part in a large, multi-centre study examining the use of convalescent plasma transfusions from people who have recovered from COVID-19 as a possible treatment for infected patients.
When a person is infected with a virus, their immune system produces protein antibodies, specific to that virus, that help the body fight the infection. These antibodies stay in the bloodstream after the person has recovered, and provide a degree of long-term immunity. Convalescent plasma is a term that describes plasma from a person who has recovered from illness. The hope is that naturally derived antibodies for COVID-19 will help fight serious infection in other individuals.
The CONCOR-1 Trial, led by Canadian researchers, will recruit 1,200 participants from Canada and New York. Researchers are collecting blood plasma from recovered COVID-19 patients and transfusing it into seriously ill patients. Measurable outcomes include the rate of intubation and mortality rate after 30 days of enrollment in the trial.
Convalescent plasma donation is being coordinated through Canadian Blood Services. For this study, they are currently collecting plasma from eligible donors under the age of 67 who have fully recovered from COVID-19 and have been symptom free for at least 28 days. Those who are interested in donating can find more information on the Canadian Blood Services website.
Dr. Ziad Solh, Lawson Associate Scientist, and Hematologist and Transfusion Medicine Specialist at London Health Sciences Centre explains, “this is an experiment; we don’t yet know if this treatment will show benefit, but it does show promise as similar treatments have had some success in studies of other viral infections such as SARS.”
Trial participants must be over 16 years of age, requiring oxygen, have been sick for less than 12 days, and their plasma must be compatible with donor plasma.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study to examine inflammatory response in patients with COVID-19
LONDON, ON – Researchers at Lawson Health Research Institute and Western University have launched a new study to help us better understand how the body’s immune system responds to COVID-19.
Any time there is a threat to the body, the immune system is activated. Some early reports from scientists and physicians working with COVID-19 patients indicate that this virus may cause a cytokine storm, or a heightened immune response, in some patients.
“Some researchers are suggesting that mortality could be improved with immunosuppressive therapies, however, evidence to support this is severely lacking at this time,” explains Dr. Douglas Fraser, lead researcher and Paediatric Critical Care Physician at London Health Sciences Centre (LHSC).
Daily blood samples are being taken from patients at LHSC who are presumed to have COVID-19. The samples are tested for inflammatory biomarkers and this information is recorded to track the changing immune response over time. The immune response in COVID-19 positive patients will also be compared to the immune response in patients with other infections, as well as in healthy controls. Clinical data of enrolled patients is also being recorded, and can be used in future studies.
Dr. Fraser, also a Lawson Scientist and Professor at Western’s Schulich School of Medicine & Dentistry, explains, “if a hyperinflammatory response is found to contribute to greater adverse outcomes from COVID-19, there are current therapies available to help these cases. This study could also inform why some people become critically ill and others do not, and help determine who will respond to certain therapies.”
This research will help provide an overall understanding of how the immune system reacts to COVID-19. As a hospital-based research institute, laboratories at Lawson are uniquely positioned to handle these types of studies, as close proximity to patients and sample collection is essential.
COVID-19, also referred to as the 2019 Novel Coronavirus, is a new respiratory virus first identified in Wuhan, China. On March 12, 2020, the World Health Organization declared COVID-19 a global pandemic. As of March 26, 2020, there are over 510,000 confirmed cases and over 22,000 recorded deaths world-wide.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study to examine inflammatory response in patients with COVID-19
Researchers at Lawson Health Research Institute and Western University have launched a new study to help us better understand how the body’s immune system responds to COVID-19.
Any time there is a threat to the body, the immune system is activated. Some early reports from scientists and physicians working with COVID-19 patients indicate that this virus may cause a cytokine storm, or a heightened immune response, in some patients.
A cytokine storm, or a heightened immune response results when excessive levels of cytokines, the activating compounds of immune cells, are released into the bloodstream to attack the virus. This can lead to lung inflammation and respiratory distress. The leading cause of death for patients with COVID-19 is respiratory failure with or without multiorgan dysfunction.
“Some researchers are suggesting that mortality could be improved with immunosuppressive therapies, however, evidence to support this is severely lacking at this time,” explains Dr. Douglas Fraser, lead researcher and Paediatric Critical Care Physician at London Health Sciences Centre (LHSC).
Daily blood samples are being taken from patients at LHSC who are presumed to have COVID-19. The samples are tested for inflammatory biomarkers and this information is recorded to track the changing immune response over time. The immune response in COVID-19 positive patients will also be compared to the immune response in patients with other infections, as well as in healthy controls. Clinical data of enrolled patients is also being recorded, and can be used in future studies.
Dr. Fraser, also a Lawson Scientist and Professor at Western’s Schulich School of Medicine & Dentistry, explains, “if a hyperinflammatory response is found to contribute to greater adverse outcomes from COVID-19, there are current therapies available to help these cases. This study could also inform why some people become critically ill and others do not, and help determine who will respond to certain therapies.”
This research will help provide an overall understanding of how the immune system reacts to COVID-19. With this understanding, targeted therapies can be developed to improve patient outcome and reduce Intensive Care Unit (ICU) demand. As a hospital-based research institute, laboratories at Lawson are uniquely positioned to handle these types of studies, as close proximity to patients and sample collection is essential.
COVID-19, also referred to as the 2019 Novel Coronavirus, is a new respiratory virus first identified in Wuhan, China. On March 12, 2020, the World Health Organization declared COVID-19 a global pandemic. As of March 26, 2020, there are over 510,000 confirmed cases and over 22,000 recorded deaths world-wide.
Study validates methods for tracking prevalence and service use of people who experience homelessness
A new population-based retrospective validation study, using ICES data collected between 2007 and 2014 in Ontario, has found that health records can be used to track service use as well as the needs of individuals experiencing homelessness. Researchers found that the algorithms tested were able to accurately identify up to 35 per cent of individuals who experience homelessness in a given year.
The best performing algorithm estimated a large increase in homelessness prevalence between 2007 and 2016, with approximately one in 200 adults in Ontario experiencing homelessness in 2016.
“We do not know how many people experience homelessness yearly in Ontario, or in the country as a whole. Current methods rely on shelter data, or large point-in-time counts that require large investments, and are only done in specific communities,” explains Lucie Richard, Lawson researcher and lead author of the study. “Also, not all people who are homeless use shelters. This approach gives us an alternative that can include a wide range of communities and different types of homelessness over time.”
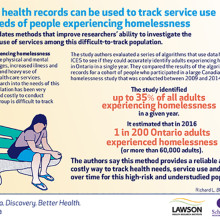
While numerous computer algorithms are already used to analyze administrative databases and identify disease populations to measure the burden of chronic diseases in Canada, this study, conducted by researchers at Lawson Health Research Institute and Western University, is one of the first to validate and track a social determinant of health with good accuracy.
People who experience homelessness often face mental and physical health challenges, have an increased risk of illness and death, and are among the highest users of emergency and other health care services. Homelessness is an important health issue for Canadians.
This ability to track individuals experiencing homelessness over time using administrative databases provides inexpensive, long-term monitoring, which will inform efforts to improve housing and health status in the community and across the country. Researchers and health care providers can now track health status and health care usage of individuals experiencing homelessness.
Understanding how many people experience homelessness and what demographics correlate with homelessness will allow for better service planning, and providers will have the information needed to more appropriately meet the needs of this vulnerable population.
The study, “Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada” is published in BMJ Open.
Study validates methods for tracking prevalence and service use of people who experience homelessness
LONDON, ON – A new population-based retrospective validation study, using ICES data collected between 2007 and 2014 in Ontario, has found that health records can be used to track service use as well as the needs of individuals experiencing homelessness. Researchers found that the algorithms tested were able to accurately identify up to 35 per cent of individuals who experience homelessness in a given year.
The best performing algorithm estimated a large increase in homelessness prevalence between 2007 and 2016, with approximately one in 200 adults in Ontario experiencing homelessness in 2016.
“We do not know how many people experience homelessness yearly in Ontario, or in the country as a whole. Current methods rely on shelter data, or large point-in-time counts that require large investments, and are only done in specific communities,” explains Lucie Richard, Lawson researcher and lead author of the study. “Also, not all people who are homeless use shelters. This approach gives us an alternative that can include a wide range of communities and different types of homelessness over time.”
While numerous computer algorithms are already used to analyze administrative databases and identify disease populations to measure the burden of chronic diseases in Canada, this study, conducted by researchers at Lawson Health Research Institute and Western University, is one of the first to validate and track a social determinant of health with good accuracy.
People who experience homelessness often face mental and physical health challenges, have an increased risk of illness and death, and are among the highest users of emergency and other health care services. Homelessness is an important health issue for Canadians.
This ability to track individuals experiencing homelessness over time using administrative databases provides inexpensive, long-term monitoring, which will inform efforts to improve housing and health status in the community and across the country. Researchers and health care providers can now track health status and health care usage of individuals experiencing homelessness.
Understanding how many people experience homelessness and what demographics correlate with homelessness will allow for better service planning, and providers will have the information needed to more appropriately meet the needs of this vulnerable population.
The study, “Validation study of health administrative data algorithms to identify individuals experiencing homelessness and estimate population prevalence of homelessness in Ontario, Canada” is published in BMJ Open.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western University’s Faculty of Health Sciences (FHS) is committed to bettering the human condition through outstanding training of health professionals, the education of students in the fundamentals of health, disability, and sport, and through the actions of our graduates who integrate the art and science of their disciplines.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study will use 3D bio-artificial tissue model to improve understanding of wound healing after glaucoma surgery
James Armstrong, an MD/PhD student at Western University’s Schulich School of Medicine & Dentistry conducting research at Lawson Health Research Institute, is creating a 3D bio-artificial tissue model to study wound healing following glaucoma surgery.
There are currently no curative treatments for glaucoma, the leading cause of irreversible blindness world-wide. The only therapy that can delay the progression of the disease is the reduction of intra-ocular pressure, which can be accomplished by taking drugs or undergoing surgery. Surgery is usually a last resort if pharmacological treatment is unsuccessful as many of these surgeries fail due to excessive healing of the surgical wound. A dense, scar-like tissue can develop at the surgical site, which blocks the pressure-lowering effect and leads to surgical failure, revision and even blindness.
Armstrong will identify risk factors for fibrotic glaucoma surgery failure through reviews of electronic patient records and literature. Using the constructed model of the ocular tissue involved in glaucoma surgery, he will simulate the surgical wound to study the physiology of how the tissue heals and test potential drugs designed to modulate the wound healing process.
The project has been awarded a Lawson Internal Research Fund (IRF) Studentship, and is supervised by Lawson scientist and St. Joseph’s Health Care London physician Dr. Cindy Hutnik.
“Right now there is a shift happening towards earlier surgical interventions for glaucoma so an understanding of the wound healing response is critical to ensure safe and successful outcomes for patients,” Armstrong says. “Future work in this area could include developing a diagnostic test to inform physicians of a patients’ likelihood of excessive healing before the patient even sets foot in the operating room. This will allow surgeons to ‘customize’ how they pre-treat each individual patient with wound healing modulating drugs.”
Although this study is focused on wound healing within the eye, the same processes are at work in many other diseases. Understanding and having the ability to manipulate wound healing mechanisms could have widespread applicability, not only for glaucoma, but also for other diseases such as atherosclerosis, interstitial pulmonary fibrosis, hepatic fibrosis, systemic sclerosis or muscular dystrophy, as well as heart, kidney or liver failure.
“The IRF has given me the opportunity to pursue research in an area where any progress could impact a significant portion of the population,” Armstrong says. “It’s a great way for researchers who are early in their career to get a foot in the door. It allows them to collect the amount of data necessary to receive funding from larger granting agencies.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).

Supporting a rapid research response during the pandemic
LONDON, ON – Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Supporting a rapid research response during the pandemic
Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
Congratulations to all of the researchers and their teams who have been awarded funding:
- Dr. Ian Ball - Predictors of clinical deterioration in hospitalized patients with COVID-19: The CORAL study
- Dr. Doug Fraser - Translational Research Centre: Repository of biological specimens from patients
- Dr. Sean Gill - Rapid identification of therapeutic targets mediating pulmonary microvascular endothelial cell dysfunction in COVID-19 patients
- Dr. Marnin Heisel - Testing Online Meaning-Centered Men’s Groups to Promote Psychological Well-Being and Reduce Despair in the Face of the COVID-19 Pandemic
- Dr. Kimia Honarmand - The impact of the COVID-19 pandemic on frontline healthcare workers: A Southwest Ontario survey
- Dr. Michael Knauer - Improving diagnostic and epidemiologic detection of SARS-CoV-2
- Dr. Jim Koropatnick - Targeting the SARS-CoV-2 receptor with candidate antisense drugs to prevent infection and disease progression
- Dr. Eldon Loh - COVID-19 and Disability: The Impact of a Societal Lockdown on those with Spinal Cord and Brain Injuries
- Dr. Len Luyt - Stapled Peptides as SARS-CoV-2 Fusion Inhibitors
- Dr. Claudio Martin - COVIDOPATHY – An observational study of coagulation abnormalities in patients with COVID-19
- Dr. Tianqing Peng - Developing new ssDNA aptamers targeting S protein receptor binding domain of SARS-CoV-2 to disrupt virus infection cycle as a potential therapy
- Dr. Eva Turley - Hyaluronan signaling through the inflammasome is a target for blunting acute respiratory distress syndrome (ARDS) in COVID-19 patients
- Dr. Ruud Veldhuizen - Next generation exogenous surfactants for COVID-19 and future respiratory pandemics
- Dr. Blayne Welk - Characterizing the burden of surgical care in COVID-19 positive patients
Synthetic surfactant could ease breathing for patients with lung disease and injury
Human lungs are coated with a substance called surfactant which allows us to breathe easily. When lung surfactant is missing or depleted, which can happen with premature birth or lung injury, breathing becomes difficult. In a collaborative study between Lawson Health Research Institute and Stanford University, scientists have developed and tested a new synthetic surfactant that could lead to improved treatments for lung disease and injury.
Lung surfactant is made up of lipids and proteins which help lower tension on the lung’s surface, reducing the amount of effort needed to take a breath. The proteins, called surfactant-associated proteins, are very difficult to create in a laboratory and so the surfactant most commonly used in medicine is obtained from animal lungs.
London, Ontario has a rich legacy in surfactant research and innovation. Dr. Fred Possmayer, a scientist at Lawson and Western University, pioneered the technique used to purify and sterilize lung surfactant extracted from cows. Called bovine lipid extract surfactant (BLES), the therapeutic is made in London, Ontario and used by nearly all neonatal intensive care units in Canada to treat premature babies with respiratory distress.
“When we look at treating adults, surfactant therapy is more difficult. For example, their lungs are 20 times bigger than those of babies and so we need much higher doses of surfactant,” explains Dr. Ruud Veldhuizen, a scientist at Lawson and an associate professor at Western University’s Schulich School of Medicine & Dentistry. “We therefore need to find novel approaches to surfactant therapy for adult patients.”
In this collaborative study, the research team took a new approach to creating synthetic surfactant. Rather than trying to recreate surfactant-associated proteins in the lab, scientists at Stanford created protein mimics. Pioneered by Dr. Annelise Barron, associate professor at Stanford, these protein mimics look like surfactant-associated proteins and have similar properties but are easier to create and more stable. As a result, the team was able to create a new synthetic surfactant.
Collaborating with the Stanford team, Dr. Veldhuizen evaluated the synthetic surfactant in animal models in his research lab at St. Joseph’s Health Care London. The study showed that, unlike other synthetic surfactants currently on the market, the new surfactant equaled or outperformed the animal-derived surfactant in every outcome. This included outperforming animal-derived surfactant in oxygenating blood, which is the lungs’ main purpose.
“The unique ability of the Veldhuizen lab to perform these rigorous and sophisticated studies was a critical aspect of the success of this project,” says Dr. Barron.
“These are very promising results,” says Dr. Veldhuizen. “For the first time, a synthetic surfactant has been developed which appears to be just as effective, if not more so, as that taken from the lungs of animals.”
The team estimates that the synthetic surfactant could be produced at as low as one quarter of the cost of the animal-derived surfactant. With a lower cost the synthetic surfactant could be tested with more lung diseases and injuries in adults and made available in more developing countries.
The team hopes to continue their research with further testing of the synthetic surfactant, including its long term effects. The team also hopes to test its ability to be customized for specific diseases. “Since it is made in the lab, we could combine the surfactant with other drugs like antibacterial agents and deliver it to specific areas of the lung, such as those where an infection is located,” explains Dr. Veldhuizen.
One disease the scientists would like to further study is acute respiratory distress syndrome (ARDS). ARDS is characterized by a low amount of oxygen in the blood due to difficulty breathing. While current surfactants have been tested with ARDS patients, they have not been effective. Dr. Veldhuizen wants to combine this new synthetic surfactant with anti-inflammatory agents and antibacterial agents to test whether patient outcomes are improved.
The study, “Effective in vivo treatment of acute lung injury with helical, amphipathic peptoid mimics of pulmonary surfactant proteins,” is published in Scientific Reports.




