It's okay to ask for help
The Zero Suicide initiative at St. Joseph’s Health Care London is helping to close systemic gaps in care
Struggling with persistent thoughts of suicide, a young woman in the care of Dr. Sandra Northcott was at risk of harming herself. She had been hospitalized multiple times for prolonged periods due to mental illness and was struggling to cope.
“We will keep you safe,” Dr. Northcott told her.
“I realize that today, you’re not able to keep yourself safe, that is our job. We will look after you until you are able to look after yourself. I know you’re not feeling strong right now and that is okay. I just need you to be brave.”
Those who have lost a loved one to suicide know the catastrophic and lasting impact the devastating act has on individuals, families and communities. One of the top 10 leading causes of death in Canada, suicide is often intertwined with mental illness. It is estimated that nearly 90 per cent of people who died by suicide were dealing with a mental health issue or illness.
What is less known is that many individuals who are struggling with suicidal thoughts often reach out for help through the health care system before ultimately deciding to end their lives. That realization was the driving force behind the decision to implement the Zero Suicide initiative within the mental health care program of St. Joseph’s Health Care London.
“About 30 per cent of individuals who have died by suicide had seen a mental health care provider prior to their death,” says Dr. Northcott, psychiatrist at St. Joseph’s Health Care London’s mental health care program. “That tells us there are gaps we need to fill across our health care system. We had to become part of the solution. We saw an opportunity for system improvement.”
The first of its kind within Canada, the program has transformed suicide rates in health systems across the Unites States and the UK. Phase one of the Zero Suicide program was launched at St. Joseph’s in 2016 within the Adult Ambulatory Care (outpatient) and Concurrent Disorders programs at Parkwood Institute, funded entirely through generous donations to St. Joseph’s Health Care Foundation.
“Conversations around suicide can be complex and challenging, both for the health care provider and the patient,” adds Dr. Northcott, who is also the physician lead for the project. “Zero Suicide provided the opportunity to standardize how often we ask patients about suicide ideation. It also allowed us to re-educate staff on how to have more meaningful conversations, and provide them with new tools and resources to support those conversations, ultimately helping patients feel comfortable sharing thoughts and feelings.”
The initiative is now in phase two, which involves implementation across the majority of mental health inpatient units at Parkwood Institute and Southwest Centre for Forensic Mental Health Care. All outpatients and inpatients will be included in this program for improved suicide prevention care, regardless of risk level.
“The Zero Suicide Initiative is about bringing people together, providing standardized training, making plans to support safety, and creating bridges in care transitions,” says Jodi Younger, Vice President of patient care and quality at St. Joseph’s. “This systematic, quality improvement approach sets a bold goal of reducing suicide to a never-event by wrapping care around the individual so that fewer people fall through gaps in their care journey.”
Through Zero Suicide, every individual is offered tailored suicide prevention strategies, risk assessment –including a full deep-dive lifetime history of any suicidal thoughts or actions – and, if needed, a safety plan. Each patient, together with their health care provider, will also develop an individualized coping plan to identify what types of situations might cause stress and healthy behaviours to help them cope. It is also an action plan to determine who they can call or where to go when in need of support. In addition, within 24 hours of discharge from an inpatient stay, each patient receives a caring call from the outpatient team to schedule a follow-up appointment and every outpatient is asked about their current risk of suicide at every visit.
The most impressive part of the planning and implementation stages, says Dr. Northcott, was how fully staff embraced the initiative and how integral patients and families were to informing the Zero Suicide process and tools.
“We wanted to ensure the program was tailored to meet the needs of our specialized mental health care program. It was important that our staff, patients and families were full partners in the design of this model.”
The initiative has been a true example of patients and families being fully integrated into the process and helping to drive the work, adds Jodi. “They were instrumental in providing valuable feedback from the perspective of those we serve.”
Today, the same young woman Dr. Northcott cared for during a difficult phase of her life is at a much better place in her recovery journey. She is living well in the community and managing her mental illness one day at a time.
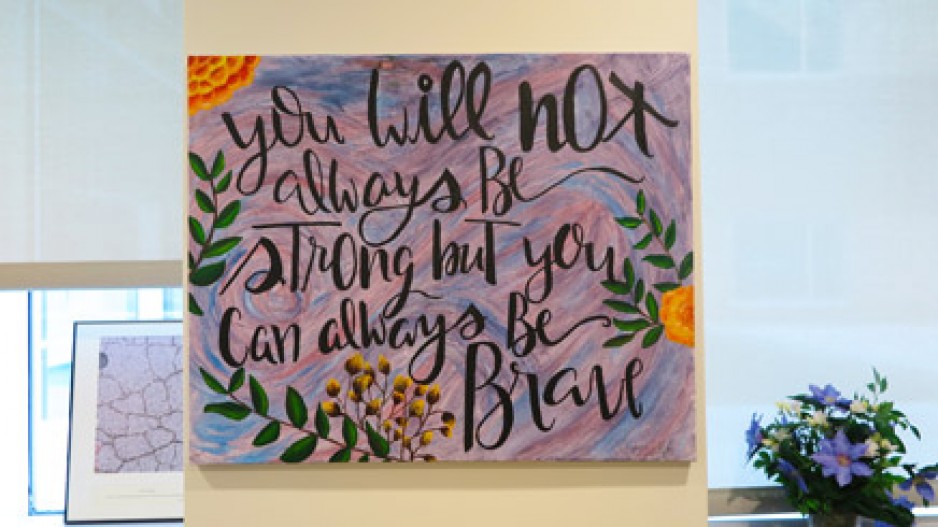
As a gesture of appreciation, and in realizing so many others have and will continue to struggle with the difficult depths of a mental illness, the grateful patient painted two pieces of artwork and gifted them to Dr. Northcott. They hang in the physician’s treatment office at Parkwood Institute to provide a glimpse of hope and assurance to other patients. Both paintings reflect the words of support and encouragement spoken to her by Dr. Northcott when she needed them most. “You will not always be strong, but you can always be brave,” and “It’s okay to ask for help.”
“Those were the two messages she took from her care,” reflected Dr. Northcott. “I needed her to believe that.”
For mental health crisis support in London-Middlesex: