Should men be screened for prostate cancer?
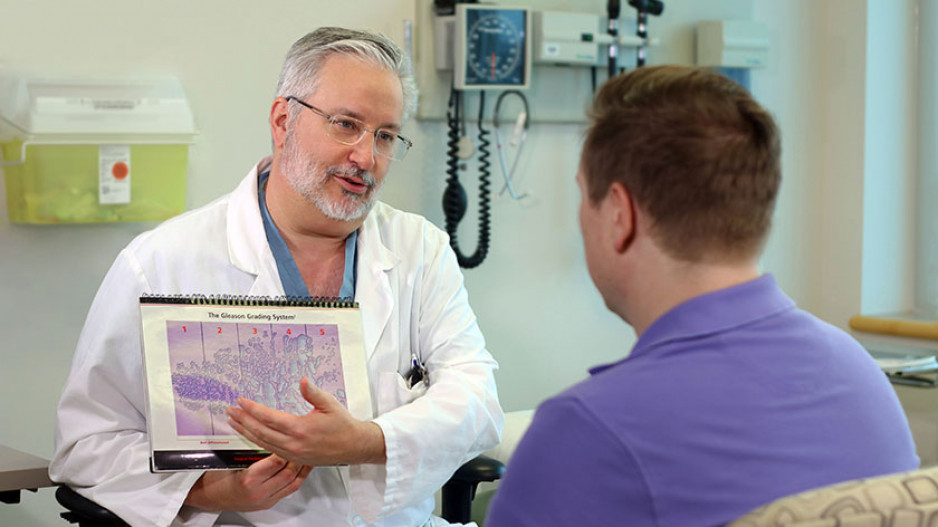
Poised over a medical model of a detachable penis in his office at St. Joseph’s Hospital, Dr. Stephen Pautler quips, “to screen or not to screen, that’s really the question.” Shakespeare he’s not, but as a urologist for almost 20 years, Dr. Pautler knows a thing or two about prostate care. “There are a lot of misconceptions out there. I call it coffee shop talk – where men share the worst stories they’ve heard, leading to misinformation and potentially dangerous consequences,” says Dr. Pautler.
Why is it important to screen for prostate cancer?
According to the Canadian Cancer Society one in seven men will have prostate cancer in their lifetime and in 2022 alone:
-
24,600 men will be diagnosed with prostate cancer
-
67 will be diagnosed every day
-
13 will die from prostate cancer every day
Flawed prostate cancer study causes dip in screening
“The rate of men getting screened is decreasing, resulting in missed diagnoses,” adds Dr. Pautler. “It’s a bit complex, but basically a study came out from the United States in 2011 saying screening doesn’t save lives. But that study was flawed.” Subsequently, a Canadian panel recommended against screening based on this work. Years later, a second study from Europe is back-tracking on the original findings, saying screening does in fact reduce mortality.
“Sadly, there weren’t any urologists on the first study panel. In the end, the recommendation that infiltrated family doctor offices was `don’t bother offering prostate screening, it doesn’t help’. Now we are stuck with this false information in the community that we need to combat.”
An associate professor of surgery and oncology at Western University, lead for Southwest Regional Surgical Oncology at Cancer Care Ontario, a Canadian pioneer in surgical robotics, and an all-around cool guy, Dr. Pautler is an internationally-acclaimed and highly respected leader in prostate care. He has been watching the changing tide of screening opinions over many years.
“Canada and the United States have come to the decision that not screening is a grave mistake, and that options should always be discussed with the appropriate men,” says Dr. Pautler. “If a man is 50 to 70 years old with a minimum 10 years of life left, it’s time to talk about options.”
Prostate screening – nothing to shy away from
Prostate screening happens in two steps starting with a PSA test.
Prostate screening happens in two steps starting with a PSA test. “PSA is a simple blood test that looks for levels of a protein in the blood,” explains Dr. Pautler. “PSA is made by the prostate, and high levels mean a higher risk cancer is present. But this test isn't perfect, as it can sometimes come back with inconclusive results or false positives.” The second part of the screening is a rectal exam.
“In my experience, men tend to build up this little exam in their heads. We are simply looking for lumps and bumps, which is a key indicator and an important thing to check. I’ve been in this field a long time, and the hype men give this is way worse than the exam. Men really need to move past the perceived awkwardness – because it’s important.”
Want to learn more? Subscribe to the DocTalks Podcast to receive an alert for an upcoming episode on prostate cancer with Dr. Pautler.