Search
Search
Exemplary leadership earns Ting-Yim Lee medical physics Gold Medal
Medical physicist Ting-Yim Lee still isn’t sure exactly what interviewers saw in him when they recruited him in 1988 to work in radiology research at St. Joseph’s Health Care London.
But he’s honoured they saw and cultivated that kernel of possibility.
Lee is now recognized as an innovative imaging scientist transforming research and patient care. In June, Lee will receive the Canadian Organization of Medical Physicists’ (COMP) Gold Medal Award for exemplary achievement. It is the organization’s most prestigious award.
“I was hired from Winnipeg to work here,” he says. “I had a thin CV, and very few publications. I was a nobody, I thought. But St. Joseph’s recognizes the potential in people and they saw potential in me. If not for St. Joseph’s nurturing environment, our imaging program would not be what it is today.”
Lee is director of PET/CT Research at Lawson Research Institute (Lawson) and medical physicist at St. Joseph’s Hospital. He is also a professor at Western University’s Schulich School of Medicine & Dentistry and a scientist at Robarts Research Institute.
At St. Joseph’s and Lawson, he has sparked the growth of the Molecular Imaging and Theranostics program. Recently it was chosen to be Canada’s first a GE Centre of Excellence in Molecular Imaging and Theranostics based on the past track record of the Lawson Imaging program of achieving a number of national and global firsts.
Mustard-seed growth
Lee says the Lawson Imaging Program’s development is symbolized by the mustard seed in the St. Joseph’s logo: “The mustard seed is the smallest of seeds and it grows into a strong and beautiful tree. When I started at St. Joseph’s, we’d installed a CT scanner one year earlier, and we were quite behind other hospitals. Then we started developing it bit by bit, piece by piece, leaf by leaf.”
Among his most celebrated achievements is developing CT Perfusion technology, a world-first in 2000 that has revolutionized stroke diagnosis and treatment by providing detailed images of blood flow in and to the brain.
The technology is used in more than 8,000 hospitals worldwide and more than 25,000 licences of the technology have been sold over the last 22 years– the royalties enabling the purchase of new, state-of-the-art CT and PET/CT equipment at St. Joseph’s to the benefit of researchers and patients alike.
Lee’s contribution helped secure a $30-million Canada Foundation for Innovation initiative in 2006, introducing hybrid imaging to Canada—including the nation’s first PET/MRI systems. His
expertise has turned contrast-enhanced CT into a powerful functional imaging tool with applications to oncology, cardiology, and neurology.
Excellence, multiplied
“It is no exaggeration to state that without Dr. Lee, the Lawson Imaging Research Program and the medical physics team would never have achieved the heights of success that it has,” says Frank Prato, PhD, founder of the program in 1982 and its leader until 2024.
Prato says Lee has had “a profound influence” on the careers of hundreds of medical physicists, including training and mentoring 60 graduate and postdoctoral students – many of whom are now training students of their own.
“These multipliers/amplifiers of Dr. Lee’s mentorship have had a profound effect on the excellence of the medical physicists we have in Canada and the excellence of the ones we train for the world,” Prato says.
Lee has published 290 research papers, which have been cited nearly 19,000 times – an indication of their impact in the medical community. He has been awarded the Meritorious Service Cross from the Governor General of Canada and received the Career Achievement Award as a WORLDiscoveries innovator.
The St. Joseph’s difference
More recently, Lee created, in partnership with St. Joseph’s Health Care Foundation and Western, two endowed chairs to research and translate liquid radiation therapy.
His considerable accomplishments are matched by his humility and his eagerness to deflect credit to his colleagues, St. Joseph’s, the St. Joseph’s Health Care Foundation and the broader imaging and research communities.
Excellent technology and research are an outgrowth of the people and culture of St. Joseph’s, Lee emphasizes. “I always feel that when I walk into St. Joseph’s, it immediately has that warm feeling that envelops you. It’s different. It’s a nurturing environment.”
The COMP Gold Medal is the highest award given by the Canadian Organization of Medical Physicists and is given to currently active or retired individuals to recognize medical physicists who have made outstanding contributions:
- A body of work fundamentally altering the knowledge base and practice of medical physics
- Leadership positions in medical physics organizations leading to improvements in the status and public image of medical physicists in Canada
- Significant influence on the professional development of the careers of medical physicists in Canada through educational activities or mentorship
Several London and Lawson-affiliated researchers have won the COMP Gold Medal, including Prato in 2024.
This year’s annual scientific meeting takes place in London on June 4 – 7.
Expanded No Fixed Address strategy houses half of those in danger of homelessness
At a community symposium on health care and homelessness attended by over 250 Londoners, a research team from Lawson Health Research Institute announced the results of a nine-month, federally funded project tackling the issue of homelessness from within hospital walls.
The No Fixed Address (NFA) strategy reaches and supports patients during the crucial transitional period when they are being discharged from the hospital and re-integrated into the community. The approach was initially tested with strong success for mental health patients across the city and the second ‘version’ of the project was extended to medical units at London Health Sciences Centre’s University Hospital and Victoria Hospital.

“Many of our patients with lived experience of homelessness were saying that their journey started with a hospital discharge,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and NFA project lead. “They were often experiencing major transitions in their lives and then experienced a hospital stay. Normally a relatively short visit, they aren’t able to gather the information and make a plan to be able to leave the hospital with somewhere to stay.”
Through partnerships between service providers and non-profit organizations, the NFA strategy helps prevent homelessness by providing timely and accessible supports to patients who would otherwise be discharged into homelessness. Staff from the Canadian Mental Health Association Middlesex, Salvation Army’s Housing Stability Bank, and Ontario Works in the City of London provided direct, on-site patient access to housing and income support databases
“Lawson’s No Fixed Address research project is the first evaluation anywhere of a strategy that aims to reduce the number of hospital patients being discharged into homelessness,” says Dr. Forchuk.
Over nine months, 74 people experiencing medical health issues accessed the NFA program. Of those, 54 per cent were also experiencing mental health challenges.
All of the study participants were in imminent danger of homelessness. Through the supports provided as part of this research study, half were able to arrange housing before being discharged.
“We were able to help a lot of people, with 50 per cent successfully securing housing,” shares Dr. Forchuk. “With the results and feedback we received, we learned a lot about how we can make the program even better.”
They found that there is a need for the supports to be extended as a transitional program in the community post-discharge, as the length of stay in the medical units tended to be short.
The project’s previous phase, involving acute and tertiary psychiatric care in the London region, prevented homelessness in 95 per cent of cases. “Going into the medical units, we found that people have highly complex needs that often involved mental health challenges.
By simply using the same approach that we did for those in psychiatric care, we helped half of the people find housing. To best serve the needs of everyone, we want to follow them after discharge.”
The team sees a solution in having a housing support worker provide transitional, wrap-around services that follow the person. They would continue to meet and work together after the hospital stay, helping to access community programs.
“This role would be embedded in both the health care system and the homeless serving system, supporting individuals who have complex physical and mental health issues as they are also navigating homeless resources.”
This project is funded by the Government of Canada's Homelessness Partnering Strategy’s (HPS) Innovative Solutions to Homelessness funding stream.
Overview and Numbers
Fast facts on homelessness and health care
- Stable housing after discharge is associated with higher quality of life, reduced substance abuse and fewer hospital admissions.
- Homeless clients are four times more likely to be readmitted to hospital within a month compared to low-income matched controls.
- Hospital care for homeless clients costs an average of $2,559 more per client.
- Finding appropriate housing or avoiding a potential eviction takes time – it is important to start as soon as possible during the discharge process.
Implementation of first phases of No Fixed Address
- Access on the unit to a housing advocate and income support staff.
- The initial intervention was accessed by 219 acute psychiatric clients, as well as 32 clients within a specialized tertiary care psychiatric hospital - only 3 became or remained homeless.
- Expanded to be an immediate wrap-around service with offices set up in the hospital mental health units.
- Staff from the Canadian Mental Health Association Middlesex (CMHA), Ontario Works (OW), and Salvation Army’s Housing Stability Bank (HSB) have on-site access to housing and income support databases.
- Clients can access service by drop-in or appointment.
- Services include assistance for finding housing, financial assistance, such as rent/utilities in arrears or first/last months’ rent for a new home, and access to high quality used furnishings, household supplies and a cleaning service.
Expanded second phase of No Fixed Address
- Program ran from July 2018 to March 2019 (9 months).
- 74 people accessed the program.
- Complex situations with both mental health and physical problems: 100% had medical issues and 54% had mental health issues.
- Lengths of stay were very short.
- People could not attend drop-in due to medical issues, so they relied on referral from staff.
- Although they were all in imminent danger of homelessness, 38 people (50%) were housed as a result of this program.
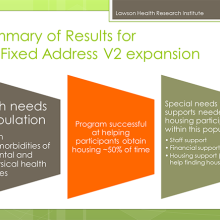
What were the main housing needs?
- Help finding a place to live
- Money for deposit
- Financial support
- Transportation support
- Help getting benefits
Recommendations and learnings for future models
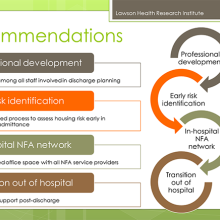
- Housing support worker needs to be a transitional support since work will be needed after discharge.
- Social work not the only key players (patient care facilitators, nursing staff, etc.).
- The transitional housing support role needs to be well embedded in the homeless serving system, as well as health care.
- People have physical and mental health issues and are also going to be navigating homeless resources.
- Despite the low success rate, many people were housed who would have otherwise been discharged to homelessness.
- We learned a lot about what was needed in an area where there was a knowledge vacuum.
- Future plans involve implementation with improvements to the model.
Expanding transitional support for young adults with diabetes
In 2012, researchers from across Ontario, led by a team at Lawson Health Research Institute, started the first multicenter randomized controlled trial to evaluate implementation of a transition coordinator for young adults with type 1 diabetes as they transferred from paediatric to adult care.
“There is a huge difference between the kind of care that they receive as children compared to adults, and that is consistent across Canada and most other countries,” explains Dr. Cheril Clarson, associate scientist at Children’s Health Research Institute, a program of Lawson, and a paediatric endocrinologist at Children’s Hospital, London Health Sciences Centre.
With children, patient visits involve a variety of specialists from different areas, such as the physician, nurse educator, dietitian and social worker. “The naturally build up a long-term relationship with the team, as some children might start the program when they are 2 or 3 years old as an example.” Dr. Clarson adds that the child’s caregivers are an integral part of the process and the care team also gets to know them very well.
Moving into the adult program means that the patient now has more responsibility and autonomy over their own care. They have to remember to go to appointments, fill prescriptions and maintain their daily diabetes care.
“During the emerging adulthood period, your attention is taken up by many other things – leaving home, starting post-secondary education, figuring out your identity and independence,” says Dr. Tamara Spaic, Lawson associate scientist and adult endocrinologist at St. Joseph’s Health Care London. “And on top of that they need to manage their diabetes every day. They are in a completely new system with a new care team – it’s a major transition. For many, they stop coming to appointments regularly and they don’t keep up with all of their own care.”
As young adults struggle to find their footing in a new system, there are significant short and long-term consequences when it comes to their health. Some will experience acute complications like high sugars leading to diabetic ketoacidosis and hospital admission or severe low blood sugars where they can lose consciousness and have a seizure.
“Different studies show between 30 to 60 per cent increased risk of complications like retinopathy, myocardial infraction, stroke and kidney disease in those who do not follow their care plan,” notes Dr. Spaic. “We see a bump in this young adult period where levels spike and their diabetes isn’t being controlled – this has impacts for both the individual and the system.”
The study enrolled 205 young adults with type 1 diabetes between the ages of 17 and 20. Patients were recruited from three paediatric centres and their care was transitioned to three adult centres. The multi-centre partnership included Children’s Hospital; St. Joseph’s; Children’s Hospital of Eastern Ontario; The Ottawa Hospital; and, Trillium Health Partners in Mississauga.
Participants were randomly assigned to two groups, with 104 patients in the structured transition program and 101 patients receiving standard care. Patients were seen in the paediatric care setting for six months and then transferred to adult care, where they continued with either the transition program or standard care for one year.
The core component of the program was a transition coordinator, a nurse who is a certified diabetes educator. The coordinator followed the young adults throughout the transition, interacting with the paediatric health care team to establish a base of support as they moved into adult care. They attended visits, established appropriate contacts for the patient, provided support for diabetic care, problem solved and helped navigate the system. In addition to face-to-face meetings, they were available via text messages, emails and phones calls.
“We had a high recruitment rate for the population and type of study, and a high number of participants followed the full program,” says Dr. Clarson. “Our results at the end of the intervention showed that the program worked very well. By providing additional support through a transitional coordinator, the results showed better outcomes all around.”
Compared to the baseline, study participants attended more care visits, were more satisfied with their care, suffered much less distress associated with diabetes, had better management on a daily basis and reported less emotional burden of diabetes.
The team then took it a step further and spent another year following the participants to see if they were able to sustain the behaviour and positive outcomes. They did not find a difference between the control and intervention groups.
“Unfortunately, we found no difference in the number of visits they attended, their satisfaction with care and management of their diabetes,” explains Dr. Spaic. “When they didn’t have the intervention, they essentially went back to baseline. Out hope is to see the program extended.”
Dr. Clarson adds that they developed the program so that it can be integrated in different ways, and also in difference areas of health care beyond diabetes. For example, they found that the preferred method of communication with the coordinator was text. This is an easy way to provide the fundamental support of a coordinator for longer, and it is cost-effective.
“Our patients really loved the intervention. By the end of the study, they felt more comfortable being able to navigate the adult health care system. They felt empowered and responded well. They wanted to continue the program.” The next step for the researchers is to evaluate support through a virtual transition coordinator.
“Closing the Gap: Results of the Multicenter Canadian Randomized Controlled Trial of Structured Transition in Young Adults With Type 1 Diabetes” was recently published in the journal Diabetes Care by the American Diabetes Association.
Learn more about the study and read about Nicole Pelcz, study participant, who found out at 13 years old that she had type 1 diabetes.
In the media:
Diabetic teens fall back to old habits after transition care, study says – London Free Press
Expert available to comment on COVID-19 in older adults
As the COVID-19 pandemic continues, data is showing that while illness and mortality occur across the lifespan, the death rate increases significantly for those over 65 years of age.
Dr. Manuel Montero-Odasso, Professor at Western University’s Schulich School of Medicine & Dentistry and Scientist at Lawson Health Research Institute is the co-chair of the Canadian Geriatrics Society COVID-19 Working Group. He is available to media for comment on the allocation of health care resources for older adults, and also on recommendations specific to this population to help prevent transmission.
“Particularly for older adults, they need to know that they are the most vulnerable but that there is no need to panic. They should follow evidence-based recommendations if they become sick. Importantly, we also stress the role of caregivers and family members, and we have specific recommendations for them on how to connect with their loved ones,” he said.
Dr. Montero-Odasso has also co-authored a position statement on behalf of the Canadian Geriatrics Society arguing that it is not acceptable to ration critical care admission or life-saving ventilation solely on the basis of age, as has been seen in other epicentres of COVID-19 when health care resource become scarce. They point out that while an established body of evidence supports that mechanical ventilation would likely be futile in some frail older adults with multiple comorbidities, there is a critical ethical difference between decisions made on the basis of futility versus those based on age alone.
“It is a concern not only because of ageism, but because it’s important to understand that age is not the only variable. It is also key to understand previous wishes of patients. You could have a 30-year-old with a chronic neurodegenerative condition who doesn’t want to be intubated and also an 80-year-old who has a high functionality and quality-of-life who does want to use all means possible to survive,” he said. “Age itself should not be the main driver of these decisions; important variables include previous functional capabilities, and levels of frailty. There needs to be a very thoughtful and thorough evaluation.”
Dr. Montero-Odasso says one example of how the COVID-19 Working Group has been involved in policy decisions is related to feedback on the Ontario Health Association Clinical Triage Protocol for Major Surge in COVID Pandemic.
“This important Ontario document does not use age alone in their recommendations and, moreover, it recommends to use proper geriatric tools, such as the Clinical Frailty Scale, in their triage algorithms to guide resources allocation,” he said.
Since COVID-19 was declared a pandemic, the first evidence that emerged was that the older adult population was being hit the hardest. As part of the Canadian Geriatrics Society COVID-19 Working Group, Dr. Montero-Odasso and colleagues have created resources and recommendations such as global recommendations for older adults, evidence-based position statements on ageism and healthcare resource utilization, and how to support health care workers on the front lines, such as the doctors and nurses in healthcare facilities.
Commentary reflects the perspective and scholarly interest of Western faculty members and is not an articulation of official university policy on issues being addressed.
-30-
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Exploring mobile software to better support youth mental health
Mental health services are rooted in relationships. When it comes to delivery, and specifically community-based and outpatient services, connection and communication between the individual and care provider need to be the focus.
When we think of youth in particular, technology is a regular form of communication for them.
“Our research team at Lawson is looking at how technology can assist in the delivery of mental health services for youth in a way that still supports the important components of treatment,” says Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson. “In our work with youth, they’ve talked about wanting the technology they are already using integrated into their care.”
In the health care sector, the use of technology needs to be carefully tested and implemented, to ensure it is not only meeting the needs of those using it but also that it complies with the standards for privacy and security.
On February 7, 2019, Lawson Health Research Institute and InputHealth welcomed community members and stakeholders for the announcement of a new health care technology solution that is being researched by Dr. Forchuk and her team, with generous contributions from the provincial government.
TELEPROM-Y is a mobile-based TELEMedicine and Patient-Reported Outcome Measurement Youth study aiming to improve access to specialized services and reduce inpatient mental health admissions for youth. The initiative is one of 11 that received funding from Ontario’s second round of the Health Technologies Fund (HTF), a program of the Ontario Ministry of Health and Long-Term Care administered by Ontario Centres of Excellence.
TELEPROM-Y received $395,109 in provincial funding with $494,630 in matching contributions for a total investment of $889,739.
InputHealth’s CEO Damon Ramsay and Chief Medical Officer Puneet Seth, along with Jennifer Moles from the Ontario Centres of Excellence were on hand with Dr. Cheryl Forchuk to hear more about how the technology and funding will help support youth. Project contributors Woodstock General Hospital and Youth Opportunities Unlimited (Y.O.U.) also attended the announcement.
This project is taking a unique approach to creating connections with youth. Researchers will use an electronic Collaborative Health Record (CHR) developed by InputHealth, an innovative Canadian digital health software company, which allows for secure communication. Patients will have access to virtual visits, prompts and reminders, text or email messages, and educational materials delivered by phone.

InputHealth's Puneet Seth and Damon Ramsay provided a demonstration of the software being used in the study.
Dr. Forchuk explains that “the study is focusing on an important transitional period. The majority of mental illnesses occur between the ages of 16 to 25 years old.” The research team is recruiting participants between these ages who have symptoms of anxiety and/or depression, and are receiving outpatient services from a hospital-based mental health care program at London Health Sciences Centre, St. Joseph’s Health Care London and Woodstock General Hospital, or community-based services from partner organizations.
A key aspect is to assess whether the technology is effective and efficient, while acceptable to both the staff and youth using the app.
“Careful evaluation is essential to make sure we are doing the right things for the people we serve,” adds Dr. Forchuk, who is also the Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery.
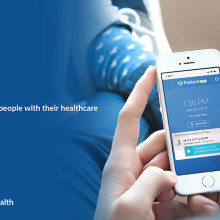
The mobile software will also be evaluated on its ability to improve the ease of access to care; monitor mood and behaviour changes for earlier intervention; enhance information exchange between patient and health care provider; and, support the overall experience for the youth.
Other project contributors include St. Michael’s Hospital Centre for Excellence in Economic Analysis Research, The Forge (McMaster University), Thunder Bay Regional Health Sciences Centre and Western University.
The study extends previous findings from the Youth Mental Health Engagement Network study (Y-MHEN), which developed, delivered and evaluated an interactive web-based personal health record, the Lawson SMART Record (LSR), to assist mental health patients in managing their care and connecting with care providers.
The Health Technologies Fund is a program of the Ontario Ministry of Health and Long-term Care and is administered by the Ontario Centres of Excellence. Program supports the development of made in Ontario health technologies by accelerating evaluating, procurement, adoption and diffusion within the Ontario health system.
Family environment influences emotional well-being of children with epilepsy
LONDON, ON – Children with epilepsy have a higher risk of developing emotional and behavioural disorders, including depression, anxiety and poor self-esteem, yet it has been difficult for researchers to pinpoint why this occurs. In a new study, researchers at Children’s Health Research Institute (CHRI), a program of Lawson Health Research Institute, have found that family environment influences the relationship between clinical characteristics of epilepsy at diagnosis and children's emotional well-being two years later.
Emotional well-being is a broad measure of emotional functioning that includes multiple aspects of mental health, such as depression, anxiety, anger, happiness, or confidence. The researchers studied a group of children aged four to 12 with new-onset epilepsy, investigating factors at the time of diagnosis and their impact on the emotional well-being of the children two years later. The study focused on the role of the family environment, an area that has not been well-studied.
Results showed that clinical factors related directly to the children’s epilepsy, such as the type of epilepsy and frequency of seizures, were not associated with emotional well-being. Instead, several family characteristics, including family stresses, functioning and resources, were strongly associated with emotional well-being.
“This is important for how we think about patient care,” says Dr. Kathy Speechley, principal investigator on the study, Chair of the Children’s Health & Therapeutics Division at CHRI and a professor at Western University’s Schulich School of Medicine & Dentistry. “Treating the physical symptoms of chronic disease alone often does not result in significant improvements in quality of life. We need to examine other avenues for care.”
“From the time of diagnosis forward, it’s important for the health care team to take a broader, family-centred approach beyond controlling a child’s seizures. This means developing a better understanding of what day-to-day life is like for families living with childhood epilepsy, including their stressors, how well they are functioning and the resources they have to aid their adaptation to stressful life events,” says Dr. Shane Goodwin, first author on the study, which was conducted while he was a PhD candidate in the Department of Epidemiology & Biostatistics at Schulich Medicine & Dentistry and a trainee at CHRI. He is currently a postdoctoral fellow at the University of Waterloo.
One example of a family-centered approach to care the researchers point to is referring patients and their families to support programs, such as Clinic to Community in Southwestern Ontario. The Clinic to Community program is funded by the Ontario Brain Institute, and provides information about epilepsy and a network of support services.
The researchers completed the study using data from the Health-Related Quality of Life in Children with Epilepsy Study (HERQULES), a multicenter prospective cohort study based in Children’s Hospital at London Health Sciences Centre.
They will now continue to analyze data from the same group of patients as they progress toward adulthood and will develop intervention trials aimed at supporting families’ successful adaptation to life with epilepsy.
The study received funding from the Canadian Institutes of Health Research and the Children’s Health Foundation.
Drs. Kathy Speechley and Shane Goodwin will be available for interviews and photos on Wednesday, January 24 between 1:30 p.m. and 5:00 p.m.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Fecal transplants show promise as treatment for non-alcoholic fatty liver disease
LONDON, ON – A new study from Lawson Health Research Institute and Western University suggests that fecal transplants could be used as a treatment for non-alcoholic fatty liver disease (NAFLD). The randomized controlled trial published in The American Journal of Gastroenterology found that fecal transplants in patients with NAFLD result in a reduction in how easily pathogens and other unwanted molecules pass through the human gut and into circulation, known as intestinal permeability. The results could have implications for the treatment of numerous conditions including metabolic syndrome and autoimmune diseases.

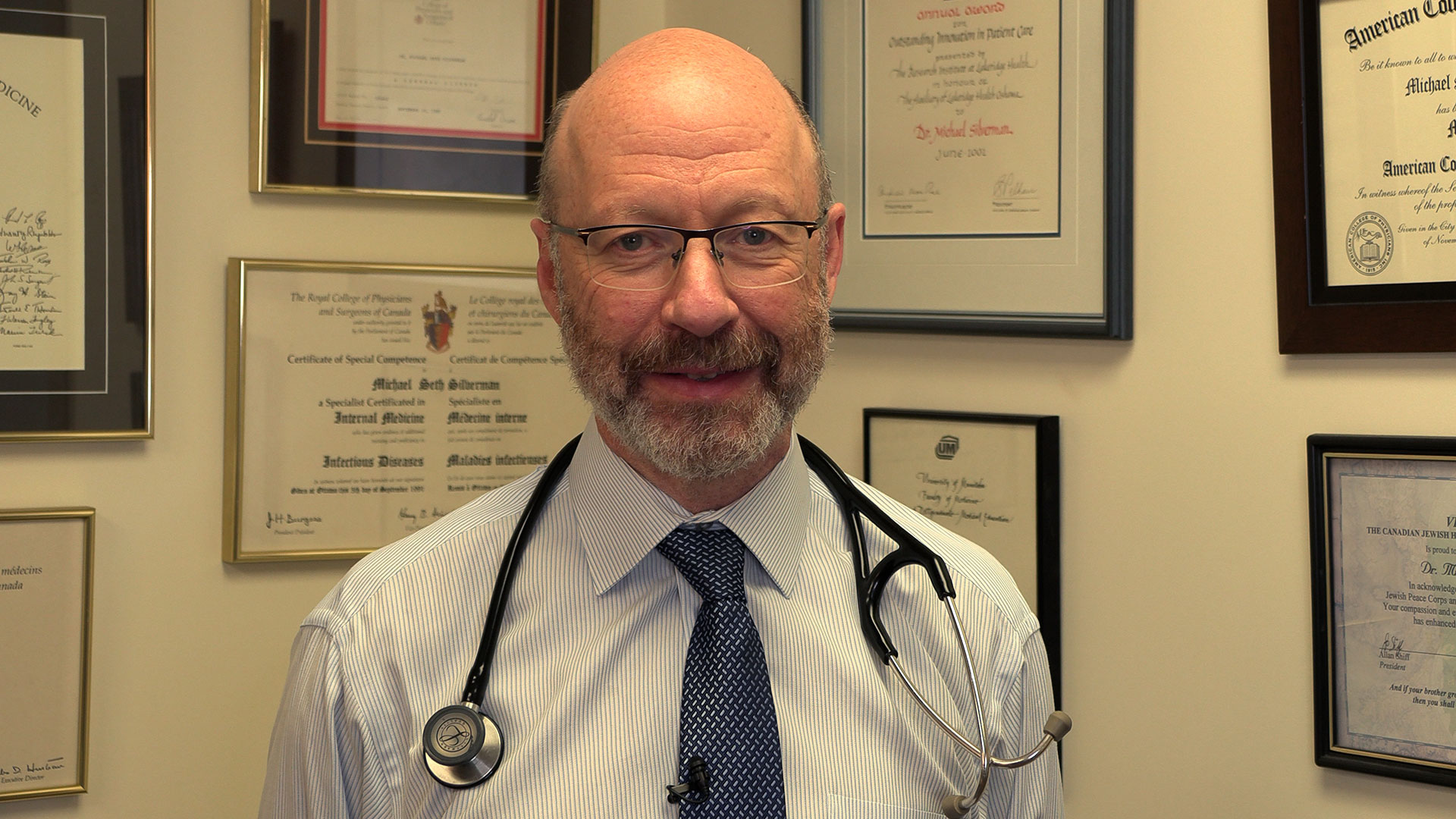
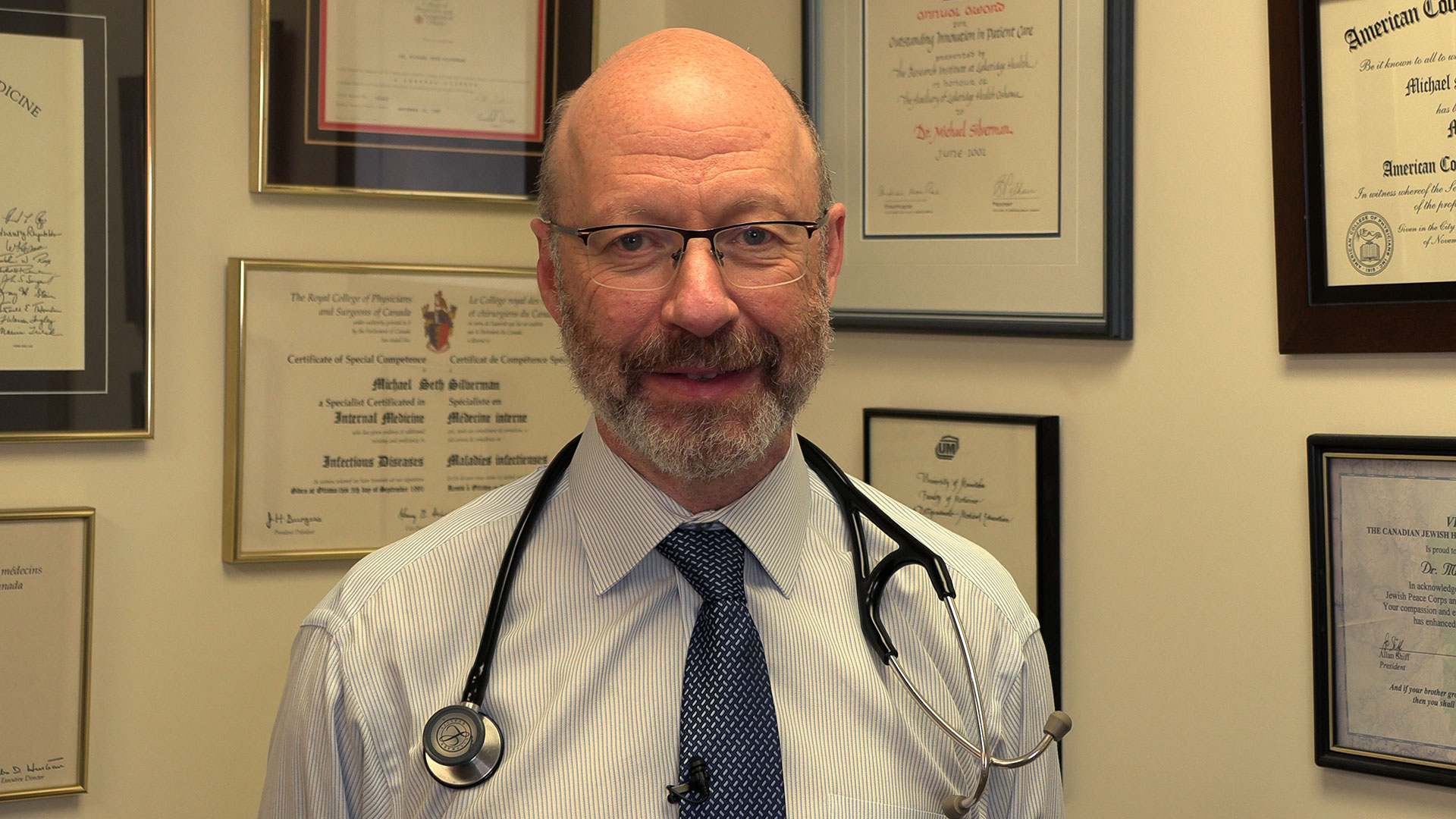
“Intestinal permeability plays a role in the development of metabolic syndrome which is a major cause of coronary and cerebrovascular disease. It has also been associated with autoimmune diseases like multiple sclerosis (MS), rheumatoid arthritis, systemic lupus and type 1 diabetes,” explains Dr. Michael Silverman, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry.
Many NAFLD patients have increased intestinal permeability which triggers inflammation, increased fat in the liver, insulin resistance and elevated levels of triglycerides in the blood. The human microbiome – the diverse collection of microbes in our body – is thought to play a role. Previous studies have shown differences between the gut microbiome of NAFLD patients compared to healthy individuals.
“Our team wondered whether we could change the gut microbiome of NAFLD patients to reduce intestinal permeability,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The trial included 21 NAFLD patients from London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. Patients were randomized to receive a fecal transplant using stool from a healthy donor or a placebo (the patient’s own stool). Fecal material was delivered to the small intestine using endoscopy. Patients were followed for six months to assess changes to their gut microbiome, intestinal permeability, percentage of liver fat and insulin resistance.
While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Our study demonstrates that intestinal permeability can be improved through fecal transplant from a healthy donor,” says Dr. Laura Craven, a recent PhD graduate from Schulich Medicine & Dentistry and first author on the published study. “This suggests that fecal transplant could be used as an early intervention in the treatment of NAFLD to reduce intestinal permeability and prevent inflammation”
“Our findings have implications for other conditions too,” adds Dr. Silverman, who is also Chair/Chief of Infectious Diseases at Western, LHSC and St. Joseph’s. “Changing the gut microbiome could hold promise in preventing and treating metabolic syndrome and autoimmune diseases associated with increased gut permeability.”
The team hopes to next conduct a large multi-centre trial to further investigate FMT as an intervention for NAFLD and as a therapy to reduce intestinal permeability.
NAFLD is an obesity-related disorder and is the second-leading cause of liver transplant in North America. While reversible if treated early, its progression can lead to liver failure or cancer. Current therapies are not overly effective and the prevalence of NAFLD is increasing.
Dr. Silverman is a pioneer in the field of fecal transplants, including their use as a treatment for Clostridioides difficile (C. diff). He is involved in multiple studies examining the potential of fecal transplants as treatments or supportive therapies for numerous conditions including multiple sclerosis (MS) and different types of cancer.
“In order to conduct this research, we need stool donors,” notes Dr. Silverman. “By donating your poop, you can help us assess the value of fecal transplants to treat a variety of diseases.”
The team is in need of young, healthy stool donors for fecal transplants. All donors are required to go through a screening process. Those interested in becoming a stool donor can contact Dr. Seema Nair Parvathy, Research Coordinator, Fecal Transplant Program, at 519-646-6100 ext. 61726.
-30-
DOWNLOADABLE MEDIA
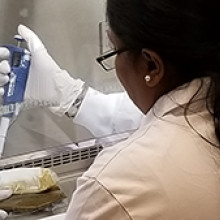
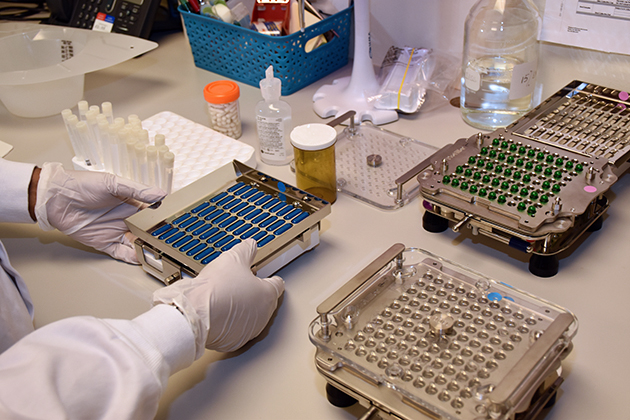
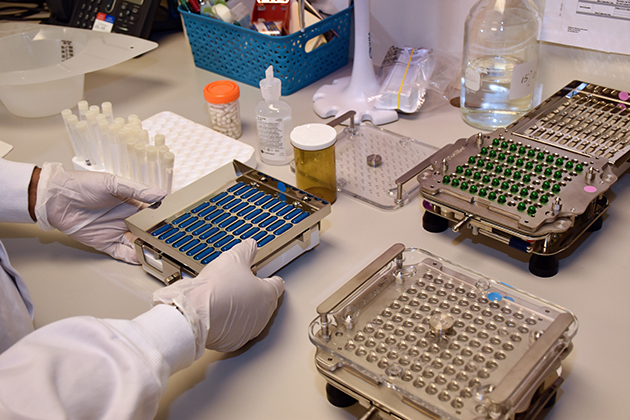
Stool samples being prepared in the lab.

Dr. Michael Silverman (left) and Dr. Jeremy Burton (right)

Dr. Laura Craven
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Fecal transplants show promise as treatment for non-alcoholic fatty liver disease
A new study from Lawson Health Research Institute and Western University suggests that fecal transplants could be used as a treatment for non-alcoholic fatty liver disease (NAFLD). The randomized controlled trial published in The American Journal of Gastroenterology found that fecal transplants in patients with NAFLD result in a reduction in how easily pathogens and other unwanted molecules pass through the human gut and into circulation, known as intestinal permeability. The results could have implications for the treatment of numerous conditions including metabolic syndrome and autoimmune diseases.
“Intestinal permeability plays a role in the development of metabolic syndrome which is a major cause of coronary and cerebrovascular disease. It has also been associated with autoimmune diseases like multiple sclerosis (MS), rheumatoid arthritis, systemic lupus and type 1 diabetes,” explains Dr. Michael Silverman, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry.
Many NAFLD patients have increased intestinal permeability which triggers inflammation, increased fat in the liver, insulin resistance and elevated levels of triglycerides in the blood. The human microbiome – the diverse collection of microbes in our body – is thought to play a role. Previous studies have shown differences between the gut microbiome of NAFLD patients compared to healthy individuals.

“Our team wondered whether we could change the gut microbiome of NAFLD patients to reduce intestinal permeability,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The trial included 21 NAFLD patients from London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. Patients were randomized to receive a fecal transplant using stool from a healthy donor or a placebo (the patient’s own stool). Fecal material was delivered to the small intestine using endoscopy. Patients were followed for six months to assess changes to their gut microbiome, intestinal permeability, percentage of liver fat and insulin resistance.
While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Our study demonstrates that intestinal permeability can be improved through fecal transplant from a healthy donor,” says Dr. Laura Craven, a recent PhD graduate from Schulich Medicine & Dentistry and first author on the published study. “This suggests that fecal transplant could be used as an early intervention in the treatment of NAFLD to reduce intestinal permeability and prevent inflammation”

Dr. Laura Craven
“Our findings have implications for other conditions too,” adds Dr. Silverman, who is also Chair/Chief of Infectious Diseases at Western, LHSC and St. Joseph’s. “Changing the gut microbiome could hold promise in preventing and treating metabolic syndrome and autoimmune diseases associated with increased gut permeability.”
The team hopes to next conduct a large multi-centre trial to further investigate FMT as an intervention for NAFLD and as a therapy to reduce intestinal permeability.
NAFLD is an obesity-related disorder and is the second-leading cause of liver transplant in North America. While reversible if treated early, its progression can lead to liver failure or cancer. Current therapies are not overly effective and the prevalence of NAFLD is increasing.
Dr. Silverman is a pioneer in the field of fecal transplants, including their use as a treatment for Clostridioides difficile (C. diff). He is involved in multiple studies examining the potential of fecal transplants as treatments or supportive therapies for numerous conditions including multiple sclerosis (MS) and different types of cancer.
“In order to conduct this research, we need stool donors,” notes Dr. Silverman. “By donating your poop, you can help us assess the value of fecal transplants to treat a variety of diseases.”
The team is in need of young, healthy stool donors for fecal transplants. All donors are required to go through a screening process. Those interested in becoming a stool donor can contact Dr. Seema Nair Parvathy, Research Coordinator, Fecal Transplant Program, at 519-646-6100 ext. 61726.

Drs. Michael Silverman (left) and Jeremy Burton (right)
Fecal transplants show promise in improving melanoma treatment
LONDON, ON – In a world-first clinical trial published in the journal Nature Medicine, a multi-centre study from Lawson Health Research Institute, the Centre hospitalier de l’Université de Montréal (CHUM) and the Jewish General Hospital (JGH) has found fecal microbiota transplants (FMT) from healthy donors are safe and show promise in improving response to immunotherapy in patients with advanced melanoma.
Immunotherapy drugs stimulate a person’s immune system to attack and destroy cancer. While they can significantly improve survival outcomes in those with melanoma, they are only effective in 40 to 50 per cent of patients. Preliminary research has suggested that the human microbiome – the diverse collection of microbes in our body – may play a role in whether or not a patient responds.
“In this study, we aimed to improve melanoma patients’ response to immunotherapy by improving the health of their microbiome through fecal transplants,” says Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Associate Scientist at Lawson and Associate Professor in the Department of Oncology at Western University’s Schulich School of Medicine & Dentistry.
A fecal transplant involves collecting stool from a healthy donor, screening and preparing it in a lab, and transplanting it to the patient. The goal is to transplant the donor’s microbiome so that healthy bacteria will prosper in the patient’s gut.
“The connection between the microbiome, the immune system and cancer treatment is a growing field in science,” explains Dr. Saman Maleki, Scientist at Lawson and LHSC’s LRCP, Assistant Professor in Schulich Medicine’s Departments of Oncology, Pathology and Laboratory Medicine, and Medical Biophysics, and senior investigator on the study. “This study aimed to harness microbes to improve outcomes for patients with melanoma.”
The phase I trial included 20 melanoma patients recruited from LHSC, CHUM and JGH. Patients were administered approximately 40 fecal transplant capsules orally during a single session, one week before they started immunotherapy treatment.
The study found that combining fecal transplants with immunotherapy is safe for patients – which is the primary objective of a phase I trial (also called ‘safety trials’). The study also found 65 per cent of patients who retained the donors’ microbiome had a clinical response to the combination treatment. Five patients experienced adverse events sometimes associated with immunotherapy and had their treatment discontinued.
“We have reached a plateau in treating melanoma with immunotherapy, but the microbiome has the potential to be a paradigm shift,” says Dr. Bertrand Routy, Oncologist and Director of CHUM’s Microbiome Center. “This study puts Canada at the forefront of microbiome research by showing we can safely improve patients’ response to immunotherapy through fecal transplants.”
“These exciting results add to a rapidly growing list of publications suggesting that targeting the microbiome may provide a major advance in the use of immunotherapy for our patients with cancer,” adds Dr. Wilson H. Miller Jr. of the JGH and Professor in the Departments of Medicine and Oncology at McGill University.
The study is unique due to its administration of fecal transplants (from healthy donors) in capsule form to cancer patients – a technique pioneered in London by Dr. Michael Silverman, Lawson Scientist, Chair of Infectious Diseases at Schulich Medicine and Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London.
“Our group has been doing fecal transplants for 20 years, initially finding success treating C. difficile infections. This has enabled us to refine our methods and provide an exceptionally high rate of the donor microbes surviving in the recipient’s gut with just a single dose,” says Dr. Silverman. “Our data suggests at least some of the success we are seeing in melanoma patients is related to the efficacy of the capsules."
The team has already started a larger phase II trial involving centres in Ontario and Quebec. Lawson researchers are also studying the potential of fecal transplants in the treatment of other cancers, including renal cell carcinoma, pancreatic cancer and lung cancer, as well as HIV and rheumatoid arthritis.
This research is supported in part through donor funding from London Health Sciences Foundation, Western University, the Lotte and John Hecht Memorial Foundation, the JGH Foundation, Canadian Cancer Society’s Impact Grant program and The Terry Fox Foundation.
-30-
ADDITIONAL DOWNLOADABLE MEDIA

About the CRCHUM
The CHUM Research Centre (CRCHUM) is one of North America’s leading hospital research centres. It strives to improve the health of adults through a continuum of research spanning disciplines such as basic science, clinical research and population health. More than 2,150 people work at the CRCHUM, including nearly 500 researchers and nearly 650 students and postdoctoral fellows. crchum.com
About the Jewish General Hospital
Part of the Integrated Health and Social Services University Network for West-Central Montreal (CIUSSS), the Jewish General Hospital has served patients from Montreal, elsewhere in Quebec, and beyond, since 1934. This McGill University teaching hospital, with approximately 600 beds, is one of the province's largest acute-care hospitals. It admits more than 22,000 patients per year, while handling approximately 578,000 outpatient visits, more than 84,000 emergency visits and more than 3,600 births. Treatment is provided by approximately 800 affiliated doctors, many of whom have teaching appointments at McGill University, as well as more than 300 medical residents per year, together with nursing and a wide range of allied health services.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Fecal transplants show promise in improving melanoma treatment
In a world-first clinical trial published in the journal Nature Medicine, a multi-centre study from Lawson Health Research Institute, the Centre hospitalier de l’Université de Montréal (CHUM) and the Jewish General Hospital (JGH) has found fecal microbiota transplants (FMT) from healthy donors are safe and show promise in improving response to immunotherapy in patients with advanced melanoma.
Immunotherapy drugs stimulate a person’s immune system to attack and destroy cancer. While they can significantly improve survival outcomes in those with melanoma, they are only effective in 40 to 50 per cent of patients. Preliminary research has suggested that the human microbiome – the diverse collection of microbes in our body – may play a role in whether or not a patient responds.
“In this study, we aimed to improve melanoma patients’ response to immunotherapy by improving the health of their microbiome through fecal transplants,” says Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Associate Scientist at Lawson and Associate Professor in the Department of Oncology at Western University’s Schulich School of Medicine & Dentistry.
A fecal transplant involves collecting stool from a healthy donor, screening and preparing it in a lab, and transplanting it to the patient. The goal is to transplant the donor’s microbiome so that healthy bacteria will prosper in the patient’s gut.
“The connection between the microbiome, the immune system and cancer treatment is a growing field in science,” explains Dr. Saman Maleki, Scientist at Lawson and LHSC’s LRCP, Assistant Professor in Schulich Medicine’s Departments of Oncology, Pathology and Laboratory Medicine, and Medical Biophysics, and senior investigator on the study. “This study aimed to harness microbes to improve outcomes for patients with melanoma.”
The phase I trial included 20 melanoma patients recruited from LHSC, CHUM and Jewish General Hospital. Patients were administered approximately 40 fecal transplant capsules orally during a single session, one week before they started immunotherapy treatment.
The study found that combining fecal transplants with immunotherapy is safe for patients – which is the primary objective of a phase I trial (also called ‘safety trials’). The study also found 65 per cent of patients who retained the donors’ microbiome had a clinical response to the combination treatment. Five patients experienced adverse events sometimes associated with immunotherapy and had their treatment discontinued.
“We have reached a plateau in treating melanoma with immunotherapy, but the microbiome has the potential to be a paradigm shift,” says Dr. Bertrand Routy, Oncologist and Director of CHUM’s Microbiome Center. “This study puts Canada at the forefront of microbiome research by showing we can safely improve patients’ response to immunotherapy through fecal transplants.”
“These exciting results add to a rapidly growing list of publications suggesting that targeting the microbiome may provide a major advance in the use of immunotherapy for our patients with cancer,” adds Dr. Wilson H. Miller Jr. of the JGH and Professor in the Departments of Medicine and Oncology at McGill University.
Previous studies looking at patients receiving immunotherapy who do not respond have found many had an unhealthy microbiome, explains Dr. Lenehan.
“There's a portion of people who don't respond or the treatment just doesn't work,” says Dr. Lenehan. “The hope with the fecal transplant is to make more people respond to treatment.”
These results have also led to a closer examination of the role of the microbiome in regulating how the body responds to disease and how the drugs themselves interact with the microbiome.

“The microbes on and in us - and there's actually a huge amount of those – play a critical role, including modulating some of our immune responses,” explains Dr. Jeremy Burton, Research Chair of Human Microbiome and Probiotics, Scientist at Lawson and St. Joseph’s Health Care London and Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine.
The study is unique due to its administration of fecal transplants (from healthy donors) in capsule form to cancer patients – a technique pioneered in London by Dr. Michael Silverman, Lawson Scientist, Chair of Infectious Diseases at Schulich Medicine and Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London.
“Our group has been doing fecal transplants for 20 years, initially finding success treating C. difficile infections. This has enabled us to refine our methods and provide an exceptionally high rate of the donor microbes surviving in the recipient’s gut with just a single dose,” says Dr. Silverman. “Our data suggests at least some of the success we are seeing in melanoma patients is related to the efficacy of the capsules."
The team has already started a larger phase II trial involving centres in Ontario and Quebec. Lawson researchers are also studying the potential of fecal transplants in the treatment of other cancers, including renal cell carcinoma, pancreatic cancer and lung cancer, as well as HIV and rheumatoid arthritis.
This work is not possible without poop donors, and there is a critical need for more. Donors must be between the ages of 18 to 50 and reside in the London, Ont. area. To learn more about eligibility and donating, call the 519 646-6100, ext. 61726 or email Dr. Seema Nair Parvathy, Research Scientist, at SeemaNair.Parvathy@sjhc.london.on.ca.
This research is supported in part through donor funding from London Health Sciences Foundation, Western University, the Lotte and John Hecht Memorial Foundation, the JGH Foundation, Canadian Cancer Society’s Impact Grant program and The Terry Fox Foundation.
Fifth annual Lawson Impact Awards honours research excellence
Over 300 guests attended the fifth annual Lawson Impact Awards on Wednesday, April 18 at the London Convention Centre to honour research making a difference and to recognize the accomplishments of our scientists, staff, trainees and partners.
“There are many individuals, groups and partners at Lawson who regularly go above and beyond to drive innovative new discoveries. For the past five years, the Lawson Impact Awards have given us the opportunity to step back and reflect on the importance of the work we do here and how these contributions ultimately improve patient care,” says Dr. David Hill, Scientific Director, Lawson Health Research Institute.
This year’s Lawson Impact Award winners include:
- Dr. Robert Teasell – Scientist of the Year Award
- Dr. Mandar Jog – Innovation Award
- Dr. Manuel Montero-Odasso – Dr. Joseph Gilbert Research Contribution of the Year Award
- London X-Ray Associates – Industry Partner of the Year Awards
- CAISA Fashion Show; London Run for Ovarian Cancer; and Kyle MacDonald and John Franklin – Community Partner of the Year Award
- Sarah Best – Staff Award of Excellence
- Sheila Fleming – Staff Award of Excellence
- Amanda McIntyre – Leadership Award for Fellows & Students
The recipients of Lawson’s 2018 Strategic Research Fund (SRF) were also revealed at the Lawson Impact Awards. The Lawson SRF is an annual competition that supports projects that will advance science in alignment with Lawson’s strategic research goals, as outlined in the Lawson Strategic Plan 2014-2018. This year’s competition was open to all areas of research. The following two projects were awarded $50,000 over a two-year period:
- “Mindfulness group intervention for newly diagnosed persons with Multiple Sclerosis: A pilot study” – Drs. Sarah A. Morrow and Arlene MacDougall
- “Extending routinely collected data research at Western: Does enhanced medical reconciliation improve care at London hospitals?” – Drs. Blayne Welk and Amit Garg
In addition to the Lawson Impact Award and SRF recipients, two Children’s Health Research Institute (CHRI) award recipients were recognized at the event. CHRI is a program of Lawson and awards a Scientist and Trainee of the Year annually. These awards are sponsored by the Children’s Health Foundation. CHRI’s 2017 award recipients were honoured at the Lawson Impact Awards: Dr. Lina Dagnino (CHRI Scientist of the Year) and Dr. Amer Youssef (CHRI Deb Comuzzi Trainee of the Year).
A highlight of the event was a keynote presentation from physician-scientist and 3D innovator, Dr. Julielynn Wong, titled “How Technology is Enhancing Our Future.” Dr. Wong delivered an engaging talk on how technology trends such as 3D printing and drones can improve health care accessibility. Her presentation included a 3D printing demonstration and guests were given the opportunity to examine samples of 3D printed medical supplies.
To view videos of each award winner, visit the Lawson YouTube page. To see more photos from the event, visit Lawson’s Facebook page.
First clinical guidelines in Canada for pain following spinal cord injury
Researchers at Lawson Health Research Institute are the first in Canada to develop clinical practice guidelines for managing neuropathic pain with patients who have experienced a spinal cord injury (SCI).
Neuropathic pain is complex and chronic, and is the most common complication reported by people following SCI. The research team worked with care providers at Parkwood Institute, part of the St. Joseph’s Health Care London family, and an international panel to address the complex and unique challenges for managing pain during recovery and rehabilitation.
In 2003, Dan Harvey sustained a spinal injury after falling off a trampoline. Using his personal experience, as well as his experiences meeting with newly injured people, Harvey contributed to the development of the new guidelines.
“Neuropathic pain – and pain in general – affects every person with a spinal cord injury very differently. Some people have it, some people don’t. But for those who do have it, it can make rehabilitation and recovery much more difficult,” explains Harvey.
“On top of just learning how to use your body again, you also have to deal with various forms of physical pains, which can make it challenging to mentally adapt to an injury.”
For those with chronic pain, it may be hard to just get out of bed in the morning, feel well enough to leave the house, or even fall asleep. “I have fairly extensive neuropathic pain, so I’m well aware of how difficult it can be to get a full night’s sleep, or show attentiveness at work or at school when it literally feels like your legs are on fire,” says Harvey.

Dan Harvey with Lawson researchers Stacey Guy, Swati Mehta and Dr. Eldon Loh.
Dr. Eldon Loh, Lawson Researcher and Physical Medicine and Rehabilitation Specialist at St. Joseph’s, and his team recognized that pain can be an overlooked part of a spinal cord injury and plays a major factor in the success of rehabilitation. It’s difficult for someone in pain to participate fully in their own recovery, and so long-term disability becomes more likely. Pain is difficult to manage and it often takes multiple approaches to find something that works for each person.
“This is a starting point for us to standardize how we approach pain in the clinic. We have identified gaps and offered recommendations to not only manage the pain, but also ensure that our patients can fully benefit from rehabilitation,” says Dr. Loh.
The results of the three-year process led to recommendations for screening and diagnosis, treatment and models of care. Important clinical considerations accompany each recommendation.
“For those in hospital following an injury, it’s about making sure they can be as independent as possible before discharge. Over time, we want to keep pain levels under control so that they are able to live life to the fullest,” adds Dr. Loh.
The research will inform new tools and resources for care providers and patients.
Harvey believes the guidelines will have a tremendous impact for patients whose pain may have been overlooked. “Pain can be created through many different avenues and the effects can snowball after a person is discharged and sent home. If you don’t check all of the boxes, you might be missing a very important item.”
The new guidelines have been published in the international journal Spinal Cord. The Ontario Neurotrauma Foundation and Rick Hansen Institute provided funding for the research study.
A special thanks to individuals from St. Joseph's who were involved in the project: Steve Orenczuk, Patrick Potter, Keith Sequiera, Lindsey Guilbault, Robert Teasell, Anna Kras-Dupuis, Dalton Wolfe, Alba Casalino and Dwight Moulin.

Additional members of the panel that developed the new clinical practice guidelines.
