Search
Search
Hospital-based research delivers high quality and efficient patient care
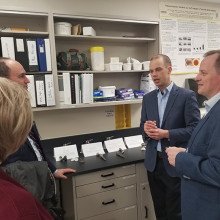
On January 10, 2020, the Honourable Jeff Yurek, Minister of Environment, Conservation and Parks and MPP for Elgin-Middlesex-London, joined London Health Sciences Centre (LHSC), Lawson Health Research Institute and the Ontario Hospital Association for a research tour at LHSC’s University Hospital.
This tour was organized to afford the Minister the ability to see first-hand how research-intensive hospitals like those in London are helping to deliver high quality and efficient patient care to people across the province and beyond.
At University Hospital, Drs. Matthew Teeter and Brent Lanting are leading clinical research in hip and knee replacement that is reducing the time patients are in hospital following surgery. They are utilizing wearable technology to better assess how patients are doing, flag issues and predict outcomes, while partnering with industry to develop the next generation of implants.
Dr. Teeter leads one of Canada’s only Implant Retrieval Labs, which stores thousands of failed hip, knee and shoulder implants retrieved from patients. Surgeons and scientists from all over the world send implant specimens to London to be imaged and studied.
As the research institute of LHSC and St. Joseph’s Health Care London, Lawson’s researchers and their teams are helping people live their life to the fullest by minimizing the effects of injury, disease and disability. Research is done within hospital walls and can be directly implemented into patient care.
This includes ground breaking work in minimally invasive and robotic cardiac surgeries let by Dr. Michael Chu and the cardiac surgery team. They have helped patients like Maria Bruno who shared her experience as a patient, and the impact on her own life and that of her family.

“Today, my heart is in perfect condition,” shares Maria. “The ability to perform this procedure is unique in Canada. I’m forever grateful to this hospital and Dr. Chu for being able to repair it. I’m a huge advocate for continued research because there are many, many patients who could benefit.”
As an active clinician researcher, Dr. Chu also investigates augmented reality image guidance in minimally invasive valve surgery, experimental transcatheter technology and complex aortic reconstruction. In 2019, Dr. Chu along with colleagues from University Health Network published a high-impact finding that women are more likely to experience poorer outcomes following aortic surgery.
Dr. Mandar Jog is a world leader in his field, revolutionizing treatment for people with movement disorders including Parkinson’s disease and essential tremor. Last year, his work on spinal cord stimulation was covered by BBC World News.
Patients Real Beaulieu and Guy Alden who have been involved with the team’s clinical trials told the Minister about the dramatic improvements in their quality of life

“With the tremor, I was at the point where I couldn’t write, I couldn’t get a key in the key hole. I couldn’t function normally in life and it was embarrassing for me,” remembers Real. “After the treatment with Dr. Jog, it was a huge turnaround for me and how I could live my life.”
Hospital-based research is critical to supporting health care in Ontario. “Health research is a necessity in order to provide the best care for patients and ensure the health system is sustainable. Researchers, clinicians, staff and trainees working at hospital sites across the city are driving important discoveries that continually improve patient care,” says Dr. David Hill, Lawson Scientific Director and Integrated VP, Research for LHSC and St. Joseph’s Health Care London.
Hospital-based research in London ranked in the top 10 for Canada
Lawson Health Research Institute is ranked eighth in the country according to the 2018 edition of “Canada’s Top 40 Research Hospitals List” by Re$earch Infosource. This strong position has been maintained by Lawson for the past five years and also keeps the institute within the top five institutions in Ontario.
The research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s), Lawson has also maintained the top ranking for research intensity among the large tier institutions, with $616,300 of research spending per researcher.
“As a hospital-based research institute, our innovation happens where care is delivered,” says Dr. David Hill, Lawson Scientific Director. “Every day, teams of researchers are working directly with clinicians and patients to improve treatments, or create entirely new ones. They find innovative methods of delivering services that drive efficiency and reduce costs.”
The top 40 list analyzes hospital-based research institutes from across the country on several metrics, including total research income from the previous fiscal year. The ranking looks at funds received from all sources, including both internal and external, to support research at the organization. According to the report, Lawson received $123,255 million in research income in 2017, which was a 0.8 per cent drop from the previous fiscal year.
Dr. David Hill advocates for increased scientific funding nationally. “We held our position despite the modest decrease in funding. Canada as a whole requires significant investment in scientific discovery to increase the well-being of Canadians and build a robust economy.”
This year, a special spotlight on intellectual property (IP) is showcasing the top Canadian organizations – universities, corporations, hospitals and government departments/agencies – patenting at the US Patent and Trademark Office.
Lawson, as the research institute of LHSC and St. Joseph’s, is featured in the top 10 list for Hospital Patent Leaders as measured by ownership of patents granted between 2013-2017. Lawson has ranked in the sixth spot with 13 patents owned.
Commercialization opportunities are managed through WORLDiscoveries®, the business development arm of London’s extensive research network. Born out of a partnership between Lawson, Robarts Research Institute and Western University, WORLDiscoveries® draws upon a mix of industry connections, sector-specific market knowledge, and business development expertise to help researchers and local inventors commercialize their discoveries through licensing and new company spin-offs.
“We support technology development and licensing agreements by taking local knowledge and discoveries to industry partners worldwide,” explains Dr. Hill. “Research-intensive hospitals are improving health care, creating jobs and contributing to the country’s growing knowledge economy.”
Featured Innovations
A Stroke of Genius

Based at St. Joseph’s Hospital in London, Dr. Ting-Yim Lee specializes in computed tomography (CT) imaging, a type of x-ray technology that captures images of slices of the body. As a young scientist, he dreamed of using CT imaging to measure how blood flows in the human body. The idea was to develop software that could be installed on existing CT scanners to make quick, easy work of a very complex algorithm. If a patient came to the emergency room suffering from a stroke, it would allow the doctor to quickly analyze and address the damage.
Thanks to decades of public and private sector support, Dr. Lee’s idea has evolved from concept to prototype to clinically-approved product. Through a licensing deal with GE Healthcare, his software is now installed on 70 per cent of the company’s new CT scanners on the market. It’s currently in use in more than 8,000 hospital imaging departments around the world.
Stroke is a situation where every minute of delay in treatment has grave consequences on the recovery of the patient, and this software allows physicians to quickly decide on the best treatment for the patient. Dr. Lee is extending his technology to measure blood flow in whole organs, including predicting and monitoring how cancer and heart attacks respond to treatment. The royalties from the licenses enabled Lawson to install Canada’s first PET/CT scanner to complement CT Perfusion with metabolic information from PET scanning.
Novel discovery in the field of Parkinson’s Disease

In addition to a busy neurosurgery practice, Dr. Matthew Hebb maintains a highly productive research program. Dr. Hebb is creating tools to advance Parkinson’s Disease research and therapeutics across the globe. Parkinson’s Disease is characterized by progressive neurological impairment caused by the death of cells in the nervous system. Dr. Hebb’s team provided a novel description of brain-derived progenitor cells (BDPCs) that could protect and stimulate re-growth of disease-affected neurons. This discovery may offer critical insight into the disease process and provide a new personalized source of brain-derived cells for delivering therapy back into the same individual.
By using a patient’s own BDPCs, Dr. Hebb hopes to slow or halt disease progression and stimulate regeneration of damaged brain circuitry. BDPCs may further advance drug, genetic and functional screening across broad patient populations. This work also resulted in a patent and partnership with STEMCELL Technologies to develop innovative research tools for Parkinson’s Disease and other incurable neurological diseases.
Computer assisted surgical techniques and technologies

Dr. Christopher Schlachta is Medical Director of CSTAR, the Canadian Surgical Technologies & Advanced Robotics, at LHSC. His current research interests are focused on development of computer-assisted surgical techniques and technologies to enhance care and training. Along with his team, he has demonstrated how computer-assisted technologies in the operating room can enhance communication among surgeons and trainees to produce better outcomes for patients. He is currently partnering with industry to commercialize operating room technology developed with engineers at CSTAR.
His Wireless Hands-free Surgical Pointer system incorporates infrared and inertial tracking technologies to address the need for hands-free pointing during minimally invasive surgery. The combination of these technologies allows for optimal movement of the pointer and excellent accuracy while the user is located at a realistic distance from the surgical monitor.
Smart tech, smart treatment for movement disorders

Dr. Mandar Jog operates the London Movement Disorders Centre and has driven the development of TremorTek, a wearable sensor technology that has already successfully treated hundreds of research patients who suffer from tremors in their arms and hands. These tremors, typically caused by Parkinson’s disease or essential tremor, are a common movement disorder symptom yet there is no effective treatment. Neurotoxin therapy has been identified as a possible treatment for tremors; however, an injection in the wrong place or at the wrong dose can cause negative side effects. Everyone experiences tremors in different ways – the location and strength of the movements, and how often they occur varies widely.
Using commercially available sensor technology, Dr. Jog and his team were able to isolate independent muscle movements. They created a system that matched the muscle activity pinpointed by the sensors with the correct amount of toxin to administer. This kinematic technology can be applied to the pre-treatment assessment of patients and the information generated can guide the placement of botulinum toxin. The technology has been taken by a spinoff company MDDT Inc. that has been working with numerous stakeholders interested in its applications.
How changes in the brain affect walking while talking in older adults
Dr. Manuel Montero-Odasso’s research demonstrates that gait testing, such as walking while performing a cognitively demanding task like counting backwards (dual-task gait),can be an effective predictor of progression to dementia. In a new study, a team at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry has discovered changes to the brain that correspond to these findings.
These changes identify a brain mechanism that corresponds with slow dual-task gait among older adults with mild cognitive impairment (MCI), an intermediate stage between the expected cognitive decline of normal aging and the more serious decline of dementia. Through their work Dr. Montero-Odasso and his team have found that a high dual-task gait cost, or a significant slowdown in walking speed when dual-tasking, is associated with a two- to three-fold increased risk of progression to dementia. However, the brain mechanism underlying this association was unclear.
To address this research question, Dr. Montero-Odasso partnered with Robert Bartha, PhD, an imaging scientist at Schulich Medicine & Dentistry and Robarts Research Institute at Western University. The team used magnetic resonance imaging (MRI) to examine the medial temporal areas of the brain, particularly the hippocampus, the parahippocampal gyrus, and the entorhinal cortex, which are regions particularly vulnerable to degeneration in Alzheimer’s disease. Participants were 40 older adults with MCI taking part in Dr. Montero-Odasso’s “Gait and Brain Study” at St. Joseph’s Health Care London’s Parkwood Institute.
The researchers found that participants with higher dual-task gait costs had a smaller grey matter volume in the left entorhinal cortex. Although grey matter volume loss is a common finding in people with Alzheimer’s disease, it is still unclear which areas of the brain are first affected by neurodegeneration. This finding points to the entorhinal cortex as a susceptible brain region in early stages of cognitive decline. This is in line with previous studies reporting that progression to Alzheimer’s disease is associated with volume loss in the entorhinal cortex.
The study therefore suggests that cognitive and motor dysfunction in older adults with MCI share common changes to the brain. This further supports that dual-task gait changes may be a measurable motor marker for neurological degeneration happening in Alzheimer’s disease.
“These novel results show that early brain changes common to pre-dementia states can be manifested by the way patients walk,” says Dr. Montero-Odasso, scientist at Lawson, geriatrician at St. Joseph’s Health Care London, and professor at Schulich Medicine & Dentistry. “This evidence supports walking while performing a cognitively demanding task as an important way to help predict dementia.”
The study, “Entorhinal Cortex Volume Is Associated With Dual-Task Gait Cost Among Older Adults With MCI: Results From the Gait and Brain Study,” is published in The Journals of Gerontology: Series A.
HRI Talks: Trauma and Moral Injury: Making the Invisible Wound Visible
Event page: https://hriresearch.com/news/hri-talks/trauma-and-moral-injury-making-the-invisible-wound-visible/
Registration link: https://us02web.zoom.us/webinar/register/8016712243425/WN_8XVEiG6dQGKycm9wfoLLqQ
Event description:
This is a free, public Zoom event. A moderated discussion will be followed by a live Q&A with audience members. A recording will be available following the event.
The people our society sends to the front lines of catastrophe – the disasters, the conflicts, the pandemics – do invaluable, selfless work. Too often, they pay a price for their efforts. Increasingly, one of the tolls they pay is living with a form of trauma called moral injury.
In this HRI Talk, Dr. Ruth Lanius will lead a discussion on moral injury/distress and explore the emerging science that enables us to understand what’s happening in the brain and how to better treat individuals suffering from moral injury.

ICES launches call for applications to its next faculty training cycle
The ICES Faculty Scholars Program has officially launched the call for applications to its fourth training cycle (2019-2021).
This two-year, part-time learning opportunity is open to Ontario-based academic researchers who are passionate about population health and health services research, and wish to obtain an appointment as an ICES Scientist,
The program was established at ICES Western in 2013 as part of its strong focus on supporting trainees and new investigators. By leveraging partnerships with other ICES sites and in conjunction with an interactive e-learning environment, faculty from different regions are able to fully participate in the ICES Faculty Scholars program.
Scholars will have access to:
- Training in the use of Ontario’s health administrative databases for research.
- Seminars on advanced methods relevant to population health research.
- Opportunities for collaboration with experts across the ICES network.
- Individual project mentorship and data analytic support to develop and complete one or more research studies using Ontario’s health administrative databases.
Hear from successful ICES Faculty Scholars:
“The methods of planning and completing an ICES project are unique. This program is the best possible way to demystify the process and produce high quality work from the outset. The amount of support is outstanding, so you have confidence that your work will be successful.”
Dr. Andrew Appleton, Assistant Professor, General Internal Medicine, Western University
“The Faculty Scholars Program is extremely well structured and run. The Program provides a positive and open learning environment for Scholars to ask questions and learn about the administrative and practical aspects pertaining to conducting research at ICES.”
Dr. James Crispo, Researcher, Health Sciences North Research Institute
Applications for the 2019–2021 program will be accepted until January 18, 2019. Any questions regarding the program, applications or eligibility can be directed to @email.
Go to the ICES website for more information on the ICES Faculty Scholars Program.
ICES is a not-for-profit research institute encompassing a community of research, data and clinical experts. With its growing network across the province, ICES researchers are able to access a vast and secure array of health-related data to evaluate health care delivery and outcomes. Learn more about ICES Western.
ICU patients with non-brain-related injuries may suffer undetected cognitive dysfunction
LONDON, ON - A new study led by Western University and Lawson Health Research Institute has found that most patients entering hospital intensive care units (ICU) for non-brain-related injuries or ailments also suffer from some level of related cognitive dysfunction that currently goes undetected in most cases.
The findings were published today in the influential scientific journal, PLOS One.
Many patients spend time in the ICU for reasons that have nothing to do with a known brain injury, and most health care providers and caregivers don’t have any evidence to believe there is an issue with the brain. For example, a patient may have had a traumatic injury that does not involve the brain, yet still requires breathing support to enable surgeons to fix damaged organs, they may have issues with their heart or lungs, they may contract a serious infection, or they may simply be recovering from a surgical procedure like an organ transplant that has nothing directly to do with their brain.
For the study, Western researchers from the Schulich School of Medicine & Dentistry and the Brain and Mind Institute and researchers from Lawson assessed 20 such patients as they left the ICU and every single patient had detectible cognitive deficits in two or more cognitive areas of investigation, including memory, attention, decision-making and reasoning. Again, this is in spite of the fact that, on the face of it, they had no clear brain injury.
The discovery was made using online tests, developed by renowned Western neuroscientist Adrian Owen and his teams at the Brain and Mind Institute and BrainsCAN, which were originally designed to examine cognitive ability in patients following brain injuries but for this purpose, are being used to detect cognitive deficits in people who have spent time in an intensive care unit without a diagnosed brain injury.
“Many people spend time in an intensive care unit following a brain injury and, of course, they often experience deficits in memory, attention, decision-making and other cognitive functions as a result,” explains Owen, a professor at Schulich Medicine & Dentistry. “In this study, we were interested to see how patients without a specific brain injury fair after leaving the ICU. The results were astonishing.”
Why cognitive ability declines even in non-brain related visits to the ICU likely varies from patient to patient, but Dr. Kimia Honarmand from Schulich Medicine & Dentistry says the lesson to be learned is that many conditions affect brain function, even though they might not directly involve the brain.
“If you are having trouble breathing, your brain may be starved of oxygen. If you have a serious infection, the inflammation that occurs as a result of infection may affect brain function. If you are undergoing major surgery, you might be given drugs and have procedures that may affect your breathing, which in turn may affect the flow of oxygen to the brain,” explains Dr. Honarmand. “What we have shown here is that all or any of these events can lead to deficits in brain function that manifest as impairments in cognition. And healthy cognition is a vital determinant of functional recovery.”
Dr. Marat Slessarev, Lawson Scientist, says these findings can shift how the medical community treats incoming patients and more importantly, outpatients following ICU visits.
“Historically, the clinical focus has been on just survival. But now we can begin to focus on good survival,” says Dr. Slessarev, also an associate member at the Brain and Mind Institute and an assistant professor at Schulich Medicine & Dentistry. “These sensitive tests will enable doctors to both detect cognitive impairment and track cognitive performance over time, which is the first step in developing processes for optimizing brain recovery.”
-30-
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Imaging “hidden” regions of the heart
After suffering a heart attack, some patients develop a microvascular obstruction, an area of the injured heart with extremely poor blood flow. These patients are at an increased risk of developing heart failure in the future.
Medical imaging technologies such as magnetic resonance imaging (MRI) and positron emission tomography (PET) can be used to study the remodeling process after a heart attack that can lead to a microvascular obstruction. However, poor blood flow makes it difficult to get contrast agents into the obstruction. Contrast agents are used in medical imaging to show contrast between different types of tissue, such as damaged and healthy tissue.
Benjamin Wilk, a PhD candidate at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry, will investigate whether a hybrid PET/MRI system and a new method of administering contrast agents can allow researchers to image microvascular obstructions and study these “hidden” regions in the heart.
Contrast agents are usually injected as a bolus, meaning the entire injection is administered immediately. In this study, participants will instead receive a constant infusion of an MRI contrast agent and PET tracer, which means the injection will be delivered over the course of an hour. The MRI contrast agent they are using is sensitive to blood flow and scar tissue, and the PET tracer is sensitive to inflammatory cells.
This will allow researchers to study the anatomy, blood flow and inflammatory processes in microvascular obstructions a week after heart attack. Participants will then be imaged again after six weeks to study the long-term effects on heart function.
“Studying the heart after a heart attack using novel contrast agent injection strategies with simultaneous PET/MRI could provide crucial information for treatment planning, helping us reduce the number of people affected by heart failure in the future,” says Wilk. “This project could also lead to further research into finding better ways to administer PET tracers and MRI contrast agents. These methods could be applied to different diseases as well.”
Wilk received a Lawson Internal Research Fund (IRF) Studentship to conduct the study, which will be supervised by Dr. Frank Prato, Assistant Director, Lawson and leader of the Lawson Imaging research program at St. Joseph’s Health Care London.
“Lawson's IRF is valuable for students for many reasons. It not only allows us to conduct further research, it also enriches our experience by giving us opportunities to write grants and attend conferences,” adds Wilk.
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Imaging the microbiome
Normally samples of bacteria must be removed from their microbiome environment for analysis, which can lead to changes in their metabolic activity and other behaviors, hindering our ability to accurately study the gut or urogenital microbiome.
“This could be avoided if we are able to observe the bacteria in the body using Magnetic Resonance Imaging (MRI),” says Sarah Donnelly, MSc student at Lawson Health Research Institute and the Department of Microbiology and Immunology and collaborative Molecular Imaging program at Western University’s Schulich School of Medicine & Dentistry.
She is investigating the possibility of using magnetically-labelled bacteria with MRI to more directly study microbial interactions in urological and other conditions.
“The hope is that in the future we can use imaging technologies to visualize aspects of the microbiome in its healthy state compared to diseased states to see the early signs of disease and take preventative measures or allow for early intervention,” she says.
Donnelly has received a Lawson Internal Research Fund (IRF) Studentship to conduct the study, which will be supervised by Dr. Jeremy Burton, scientist in Lawson’s Human Microbiome and Probiotics research program at St. Joseph’s Health Care London (St. Joseph’s) and appointed to the Departments of Surgery and Microbiology & Immunology at Schulich Medicine & Dentistry; and Dr. Donna Goldhawk, scientist in Lawson’s Imaging research program at St. Joseph’s and assistant professor in the Department of Medical Biophysics at Schulich Medicine & Dentistry.
Escherichia coli (E. coli) are a common bacterium found in the human gut microbiome and frequently cause non-intestinal conditions like urinary tract infections. The researchers will program E. coli to express an iron uptake gene, magA. This gene is taken from another type of bacteria called magnetotactic because of their response to Earth’s magnetic field. The researchers will study whether the increase in iron uptake caused by magA expression will allow MRI to detect the magnetic signal more clearly than it would in images of untransformed E.coli. This would make it possible to see the bacteria’s behavior in living subjects without removing the bacteria cells from the microbiome environment.
They will then use this technique to study how magA labelled bacteria affect biofilm on medical devices. A biofilm is a structure produced when certain bacteria adhere to a surface and then stick together.
They will also analyze how lithotripsy affects the bacteria’s spatial distribution and interactions in three-dimensional models of kidney stones. Lithotripsy uses shockwaves to break up kidney stones into smaller pieces that are able to pass naturally out of the body. However, these shockwaves not only affect kidney stones. The waves are sent throughout the tissue, and the bacteria living on these tissues may also be affected.
“While lithotripsy is effective in treating kidney stones, we don’t know the side effects of lithotripsy on the microbiome. The shockwaves could disturb the bacteria, potentially leading to diseases caused by an imbalance between helpful and harmful bacteria,” says Donnelly.
These laboratory models will allow the researchers to perform studies in vivo (in animal models) in the future.
“Health research is very important for the development of new technologies and treatments but it is often difficult to secure funding. The IRF program allows students to pursue research that would not otherwise be possible,” explains Donnelly.
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Improved imaging for prostate cancer
Prostate cancer is the most commonly diagnosed cancer among Canadian men. However, with improved testing and better treatment options, the number of deaths from the disease has been declining over the last several years.
Scientists at Lawson Health Research Institute are working to continue this trend by testing improved prostate cancer imaging using a new molecule. Known as a Prostate Specific Membrane Antigen (PSMA) probe, the new molecule is used in Positron Emissions Tomography (PET) scans. The probe targets PSMA, a unique molecule on prostate cancer cells, to provide highly specific images for better diagnosis and management of patient disease.
PET probes are used in imaging to correctly diagnose cancer. The probes are injected into a patient where they spread to identify sites of disease. The most common PET probes are suitable for many types of cancer, but are not as sensitive in identifying prostate cancer. PSMA probes provide higher accuracy by targeting PSMA molecules, which are highly over-expressed on prostate cancer cells.
PSMA probes are gaining popularity across the globe. This specific probe is a molecule called 18F-DCFPyL and was developed by Dr. Martin Pomper at the John Hopkins Hospital in Baltimore. Dr. Pomper, also a Scientific Advisor to Lawson’s prostate imaging team, worked in collaboration with Canada’s Centre for Probe Development and Commercialization (CPDC) to bring the probe to our nation.
Lawson’s Canadian Institutes of Health Research (CIHR) Team in Image Guidance for Prostate Cancer gained early access to the PSMA probe due to a history of close collaboration with Dr. Pomper and the CPDC. Marking the first time a PSMA probe has been used in Canada, the team captured PET/MRI and PET/CT images from a 64-year-old prostate cancer patient on March 18, 2016 at St. Joseph’s Hospital.
“This is a tremendous step forward in the management of prostate cancer,” said Dr. Glenn Bauman, a Lawson scientist and Radiation Oncologist at London Health Sciences Centre. “PSMA probes have the potential to provide increased accuracy and detection which leads to better, personalized treatment.”
Lawson plans to study the probe with an additional 20 men over the next two years as part of an ongoing clinical trial funded by the Ontario Institute for Cancer Research (OICR). Lawson scientists are working with researchers across Ontario to develop other clinical trial protocols that will use 18F-DCFPyL to measure responses to drug treatments and to evaluate men with suspected recurrence of prostate cancer after radiotherapy.
“The goal of these studies it to establish the value of PSMA probes, particularly18F-DCFPyL, and provide evidence to support the use of these probes in routine clinical care,” said Dr. Bauman.
Donor funding through London Health Sciences Foundation was one catalyst in this research, providing initial funding to hire Research Associate, Catherine Hildebrand, who set up citywide cancer imaging workshops and helped the team prepare successful grant applications to secure key funding from CIHR and OICR.
Improving mental health treatments for stroke patients is the focus of a new study
LONDON, ON- Strokes affect approximately 400,000 Canadians each year and can be debilitating. They can negatively affect a person’s cognition and mobility, and severely impact mental health and wellbeing.
A team at Lawson Health Research Institute are looking to improve mental health treatments and resources for patients who have experienced a stroke. The team will recruit 100 stroke patients to assess whether the completion of a guided therapy program can improve mental health and quality of life.
“More than sixty per cent of patients experience depression after stroke,” says Dr. Robert Teasell, Lawson Scientist and Physiatrist at St. Joseph’s Health Care London’s Parkwood Institute. “Having a stroke itself makes people more vulnerable and makes people feel their lives have changed negatively.”
During stroke rehabilitation, patients are typically offered mental health treatments, but the research team say it is post rehabilitation that stroke patients tend to experience worsening depression.
“Publicly funded allied health care services are available at inpatient and outpatient care; however, psychology is often limited across the rehabilitation continuum from acute to community care,” says Dr. Swati Mehta, Lawson Scientist. “We are looking at how we can provide a program that is cost effective to help those who have these barriers to access mental health services.”
“Patients have described to me that they feel like they have been dropped off a cliff because of the lack of resources once their programs have ended,” adds Dr. Teasell.
The study will examine the use of cognitive behavioral therapy (CBT), which is an evidence based psychological intervention that aims to provide people with increased coping ability and self-efficacy. Participants will complete a 10-week guided program with specific targeted lessons, tailored to the needs of those post stroke, delivered virtually through a trained clinician. They will then complete a questionnaire to see if there have been any improvements to self-efficacy and emotional wellbeing.
“We have found this form of therapy (CBT) has been very effective and feasible for spinal cord injury patients with mild traumatic brain injury and we want to see how a modified version could potentially help those with stroke and depression,” says Randy Upper, Clinical Research Associate at Lawson.
If CBT is proven effective through this study, Dr. Mehta hopes it will encourage similar programming that would be available to stroke patients after rehab.
“We are hoping we can connect with community organizations and work with them to implement this program in a service delivery model that would be easily accessible for stroke patients living in the community.”
Recruitment for this study is currently underway, those interested in taking part can email Dr. Swati Mehta at: @email
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Improving palliative cancer treatment with existing diagnostic scans: Study reveals promising results
A recent study from London Health Sciences Centre and Lawson Health Research Institute suggests that using existing diagnostic CT scans in planning simple palliative radiation treatments can significantly cut down the waiting time for urgent treatment, resulting in a better experience for cancer patients.
“Reducing the time patients spend in a cancer centre has far-reaching benefits,” said lead study author Melissa O’Neil an Advanced Practice Radiation Therapist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP). “Faster treatment initiation means quicker relief from symptoms for patients. Utilizing existing scans is also cost-effective and frees up appointment slots or staff, allowing us to accommodate and assist more patients in need.”

Palliative radiation therapy is used to relieve symptoms in patients whose cancers cannot be cured. It’s often used when tumours cause pain, neurological issues or breathing problems such as blocked airways.
In the current standard practice, patients referred for palliative radiation typically require a CT simulation scan before starting their treatment. This scan creates 3D images that the patient's health care team uses to develop a customized radiation treatment plan. Unfortunately, this process often takes several hours, even with efforts to speed it up.
However, many of these patients have undergone previous diagnostic CT scans as part of their routine medical care. Previous research has shown that radiation oncology teams can create suitable palliative treatment plans for patients with bone and soft tissue metastases using these existing scans. This approach is less time-consuming than the more intensive simulation scans.
In the current study, O’Neil and her colleagues explored whether using existing CT scans to plan treatment before a patient arrives at the cancer centre could reduce their wait time while still ensuring appropriate care. They randomly assigned 33 patients who needed palliative radiation for tumours in their chest, abdomen or pelvis to either the standard treatment planning with on-site CT simulation scans or to treatment planning using diagnostic CT scans taken within the previous 28 days.
The study found that patients who didn't need the extra CT simulation scan spent much less time at the cancer centre on the day of their treatment – just under 30 minutes compared to nearly five hours for the others. Treatments were delivered successfully, and patient perception on time spent at the cancer centre was improved for those whose treatment planning used diagnostic CT scans taken without the previous 28 days.
"For patients who need radiation to help treat symptoms of cancer, it's important for us to get them treated quickly and to minimize the time they spend waiting for medical appointments,” said Dr. David Palma, Radiation Oncologist at LHSC and Associate Scientist at Lawson. “This trial shows that this new approach not only saves resources by reducing the number of scans we do, but also substantially reduces the time patients spend waiting for urgent radiation.”
"These findings are incredibly promising, especially in light of the nationwide shortage of radiation therapists," said Dr. Michael Ott, Physician Department Executive for Oncology at LHSC. “Work like this has benefits that can reach far beyond London, offering more relief for patients across the country."
The findings were presented at the American Society for Radiation Oncology’s Annual Meeting on Oct. 3, 2023. This meeting is recognized globally as the leading radiation oncology scientific event, drawing more than 8,500 attendees each year.
While the study shows promise, the research team said it's important to note that using prior diagnostic scans may not be suitable for every type of cancer or patient. It depends on the specific area being treated and the technique used.
For more information, please contact:
Jessica Rabaey
Communications Consultant
London Health Sciences Centre
T: 519-685-8500 ext. 77728
Jessica.rabaey@lhsc.on.ca
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Improving recovery and rehabilitation for patients with mental illness
Over 130 hospital-based clinical, administrative and research staff members, persons with lived experience of mental illness, family caregivers, peer and community supporters, and staff from local community mental health agencies attended the 18th Annual Mental Health Research & Innovation Half Day on November 1, 2017. The event provided an opportunity to learn more about mental health research at Parkwood Institute and the Southwest Centre for Forensic Mental Health Care (Southwest Centre), part of the St. Joseph’s Health Care London (St. Joseph’s) family.
“This year’s Mental Health Research and Innovation Half Day was one of the best attended in our history of hosting the event. We had a very diverse and engaged audience with great energy and a lot of enthusiasm,” says Dr. Arlene MacDougall, Director of Research and Innovation for mental health care at St. Joseph’s and Lawson Health Research Institute (Lawson).
Exciting recent projects were showcased though talks highlighting excellence in recovery and rehabilitation research, the theme of this year’s event; poster presentations; the 13th Annual Tony Cerenzia Research Lecture delivered by Dr. Sean Kidd; and interactive workshop sessions.

“We chose ‘recovery and rehabilitation’ as the theme for the event because it is so important in our clinical care and research programs to have this focus. We need to prioritize the development, implementation and evaluation of practices and interventions that foster recovery of the whole person experiencing mental illness, which includes their psychological, social and other needs that go beyond traditional notions of healthcare,” Dr. MacDougall adds.
13th Annual Tony Cerenzia Research Lecture
Guest speaker Dr. Kidd’s talk – “From clinical trials to the clinic: A story about making Cognitive Adaptation Training for schizophrenia more accessible” – focused on how to implement interventions proven in clinical trials. Dr. Kidd is a clinical psychologist, senior scientist and psychology division chief at the Centre for Addiction and Mental Health (CAMH) in Toronto. He is also an associate professor in the Department of Psychiatry at the University of Toronto.

Above: Dr. Sean Kidd's lecture focused on implementing interventions proven in clinical trials.
Workshop Sessions
Following Dr. Kidd’s lecture, attendees had the opportunity to participate in one of six workshops on a variety of topics related to recovery and rehabilitation focused mental health research:
“Implementing Interventions: A facilitated conversation attending to evidence, strategy, and recovery oriented care”
Led by Dr. Sean Kidd
Participants shared successful strategies for implementing novel approaches to care and discussed the challenges involved. They also looked at ways to leverage technology and education materials.
“Spirituality in Mental Health Care: Practically Supporting Recovery and Wellness”
Led by Stephen Yeo, Lawson allied scientist and chaplain, Southwest Centre; and Dr. Clark Heard and Jared Scott, Lawson associate scientists and occupational therapists, Southwest Centre
This workshop focused on the practical application of spirituality within the clinical setting, including the use of labyrinths, which contribute to recovery by promoting spiritual self-care, insight development and personal meaning-making reflection. Attendees had the opportunity to participate in a labyrinth walk and a related spiritual reflection. Read more about the labyrinths at Parkwood Institute and the Southwest Centre or watch the following video featuring highlights from the workshop:
“Indigenous Men’s Health and Wellbeing: Connection with Culture as a Rehabilitation and Recovery Tool”
Led by Bill Hill, social worker, Parkwood Institute and Dr. Vicki Smye, associate professor, director of nursing at Western University
Through the sharing of practitioner experience and Indigenous men’s voices, the workshop focused on understanding the powerful links between connection to culture and mental health and well-being (pictured below).

“Engaging Service Users and their Families in Research”
Led by Dr. Cheryl Forchuk, The Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery, Lawson; and Deborrah Sherman, executive director, Ontario Peer Development Initiative
Participants in this workshop discussed the benefits of patient and family involvement in mental health research and identified strategies to support patient and family engagement (pictured below).

“Innovation in Mental Health Care: Moving Ideas to Impact”
Led by Kaitlin Saxton, research and innovation facilitator, Parkwood Institute; and Lisa Bitcola, centre manager of projects and operations, Ivey International Centre for Health Innovation
This workshop focused on how innovation relates to research and quality improvement initiatives within St. Joseph’s Mental Health Care facilities. Participants discussed innovative approaches that could be implemented within their own clinical practice, research and quality improvement initiatives (pictured below).

“My Professional Practice: Where's the Research?”
Led by Amanda Thibeault, director, professional practice, St. Joseph’s
In this session, participants discussed how they can incorporate research into their clinical practice (pictured below).

Improving surgery for wrist arthritis
Wrist arthritis can cause debilitating pain, weakness and decreased range of motion. When patients are first diagnosed, the condition can often be managed with activity modification and pain medication. However, as symptoms progress, patients eventually require surgery.
Surgeons typically perform a procedure called four-corner fusion to preserve wrist motion and provide pain relief. This surgery involves removing one of the carpal bones and fusing four of the remaining carpal bones. Although this procedure is one of the most common treatments for wrist arthritis, it is not known how the position of the fusion of the wrist bones affects range of motion and joint contact.
Lawson associate scientist Dr. Nina Suh is leading a study with the goal of improving the surgical technique for four-corner fusion to maximize wrist function and symptom relief, and delay wrist arthritis progression.
Dr. Suh and her team will use a customized active-motion wrist simulator to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
“We hope this research will lead to new surgical techniques that will help us to more effectively manage wrist arthritis with four-corner fusion,” says Dr. Suh, who is also an orthopaedic surgeon at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London and an assistant professor at Western University’s Schulich School of Medicine & Dentistry. “The project will also advance our understanding of wrist biomechanics, providing a foundation for the development of enhanced patient-specific surgical tools, such as custom wrist fusion devices and implants.”
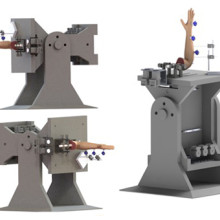
Image of the customized active-motion wrist simulator Dr. Nina Suh and her team are using to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
The study is being funded through the Lawson Internal Research Fund (IRF), designed to allow scientists the opportunity to obtain start-up funds for new projects with exciting potential.
“The IRF program is valuable for scientists as external funding sources routinely require preliminary data to strengthen applications,” says Dr. Suh. “Particularly for new scientists such as myself, these grants provide seed funding that allows us to demonstrate the validity of our methodology and the clinical usefulness of our results.”
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Injection of opioids linked to significant increase in bacterial heart infections
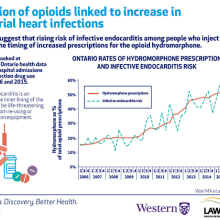
People who inject drugs are at a high risk for a number of health issues. In a new study from ICES, Lawson Health Research Institute and Western University, researchers discovered a significant rise in the risk of infective endocarditis, a serious heart infection, among Ontarians who inject drugs. When examining opioid prescriptions in the province, the research team discovered the increased risk of infective endocarditis may be related to the growing use of a specific opioid, hydromorphone.
The researchers looked at de-identified Ontario health data for 60,529 hospital admissions related to injection drug use between 2006 and 2015. Of the 60,529 admissions, 733 patients had infective endocarditis. Although hospital admission rates in people who inject drugs were stable over the study period, the risk of infective endocarditis increased from 13.4 admissions to 35.1 admissions every three months.
“Rates of infective endocarditis in people who inject drugs have been increasing around the world and our study shows this is true in Ontario,” says Dr. Matthew Weir, adjunct scientist at ICES, associate scientist at Lawson and assistant professor at Schulich School of Medicine & Dentistry, Western University. “We wondered if a change in the types of drugs people inject was responsible for this higher risk.”
Through further analysis of Ontario health data, the team discovered the increasing risk of infective endocarditis may be linked to a rise in prescriptions of the opioid hydromorphone. The number of hydromorphone prescriptions in Ontario increased from 16 per cent of all opioid prescriptions in 2006 to 53 per cent by 2015. This parallels the timing for increased risk of infective endocarditis among people who inject drugs.
The researchers initially suspected the increased risk for infective endocarditis would begin when controlled-release oxycodone was removed from the market in 2011.
“We thought hydromorphone prescriptions would increase when controlled-release oxycodone was removed from the market, leading to increased risk of heart infection,” says Dr. Michael Silverman, associate scientist at Lawson and associate professor at Schulich Medicine & Dentistry. “However, while the study did show a substantial increase in risk for infective endocarditis, it began in 2010.”
Traditional controlled-release oxycodone was easily dissolvable and people who inject drugs did not save or reuse their injection equipment. Controlled-release hydromorphone, the more common form of the drug, is more difficult to dissolve. Since residue of the drug gets left in injection equipment, injection drug users save the equipment for future use or to share with others. Reusing injection equipment allows multiple opportunities for bacterial contamination, increasing the chances that bacteria will be injected when the equipment is next used.
Infective endocarditis occurs when the inner lining of the heart becomes infected. It can be a life-threatening illness and research suggests it can be caused by sharing or re-using injection equipment, possibly through the injection of bacteria.
“While the timing was not what we expected, we did find a correlation between the rise in infective endocarditis and hydromorphone prescriptions,” says Dr. Sharon Koivu, Lawson scientist and associate professor at Schulich Medicine & Dentistry. “Our research is now focused on better understanding the potential relationship between the injection of hydromorphone and risk of infective endocarditis.”
The team is conducting ongoing studies that are looking at whether bacteria that cause infective endocarditis are more likely to survive in equipment used to prepare hydromorphone compared to other drugs.
“The opioid crisis is one of the most pressing health issues of our time. Our findings not only confirm an increasing risk of infective endocarditis in persons who inject drugs but also offer the first evidence for why it might be happening,” says Dr. Weir. “Through research and collaboration, we hope to further collect the evidence needed to address this global problem.”
The study, “The risk of infective endocarditis among people who inject drugs: A retrospective, population-based time series analysis,” is published today in CMAJ (Canadian Medical Association Journal).
insideLHSC: Diagnosing concussion
With a drop of blood, Dr. Douglas Fraser and a team of Lawson and Western University researchers are changing the way we diagnose concussion.
In the past decade, rates of reported head injury have increased by more than 40 per cent in children and youth playing football, soccer and hockey. In that same time our understanding of the impacts of concussions has significantly increased. Concussions can often result in severe symptoms and, in some individuals, long-term neurological dysfunction. When ignored, these injuries can have lasting consequences. As a result, concussions are a growing public health concern.
The diagnosis of a concussion can be difficult. Current tests rely on a patient’s description of their symptoms and the judgment of his or her physician. Concussions are sometimes misdiagnosed and some athletes with concussion return to sports too soon, putting them at risk of further injury.
By eliminating the guesswork in diagnosis, London researchers hope to improve patient outcomes.
International Women's Day 2020
International Women’s Day, taking place on March 8, 2020, is a day to celebrate the various achievements of women around the world and is a call to action for gender parity. This year’s theme is “Each for Equal” to emphasize that each individual has a significant part in working towards a gender equal world.
This year, Lawson is highlighting the different paths for women who are working towards a career in the health sciences. Below are the perspectives from students, physicians and researchers on their contributions to science and medicine.

High school student, Nimrit Aulakh, is completing her co-op placement with Lawson Scientist, Dr. Cheryl Forchuk. Her research focuses on improving mental health care for youth.
“Science has always been of interest to me and has now become significant within my academic endeavours. Part of my desire to become involved in the sciences stemmed from my older sister, who exposed me initially to the research side of science. It is with the help of rationale and logic in science that I can enrich my academic experience. Specifically, I have been working as a co-op student alongside the Mental Health Nursing Research Alliance and learning what it means to be a researcher. During my time, I conducted preliminary analyses on one of their studies, which focuses on improving mental health care for youth through virtual models of care. I will be presenting my findings at the Thames Valley Science and Engineering Fair later this month and if successful, will advance to the Canada Wide Science Fair. This experience has shown me a new side of science, one that I hope that I can continue to be a part of. I realized that through science and research, I can contribute to advancing society. To continue my journey through post-secondary education, I have applied to get my Bachelor’s in Health Sciences. Both within and beyond my four years of undergraduate studies, I hope to continue my contributions in serving the public through scientific research, as well as create an image for girls with the same interests as me, everywhere.”

Romaisa Pervez is a Research Assistant working with Lawson Scientist, Dr. Arlene MacDougall. She recently completed her Master of Science in Epidemiology and Biostatistics at Western University.
“I’m the student lead on a project that’s titled “Building a Sustainable Model and Evaluation for Psychological Rehabilitation in Kenya: An Implementation Study.” I’m working with the CREATE (Community Recovery Achieved Through Entrepreneurism) Kenya team to conduct a study to improve how we deliver, evaluate, and train persons with lived experience or community members to facilitate the Psychosocial Rehabilitation (PSR) Toolkit so it can be locally sustained in Kenya. I’ve travelled to Kenya twice during my Master’s to build relationships with stakeholders and conduct focus groups/interviews. My passion lies in understanding how we can implement upstream initiatives for mental health that are both sustainable and effective. Furthermore, I want to explore how we can find leverage points within the current mental health system in low to middle income countries and create innovative solutions. In the near future, I want to pursue medicine and further my knowledge and build stronger skills in this field.”

Dr. Kelly Anderson is an Associate Scientist at Children’s Health Research Institute, a program of Lawson. She is also Assistant Professor in the Department of Epidemiology & Biostatistics at the Schulich School of Medicine & Dentistry, Western University.
“I lead a research program in public mental health research, with a primary focus on young people experiencing a first onset of psychotic disorder. Together with my team, we are investigating the distribution and risk factors for psychotic disorders, prevention in early psychosis, and access to care and utilization of services in first-episode psychosis. My research program is centered around mentorship and training of students from all levels, and I work with trainees to foster high-level skills in the design and analysis of epidemiologic studies using large complex datasets. I am committed to fostering a culture of equity, diversity, and inclusion within my research team, and I advocate strongly for gender and early career representation for awards, scientific symposia, and other career opportunities. As a female scientist, I regularly mentor young women, both formally and informally, and due to the focus of my research, I also regularly work with trainees with lived experience of mental disorders. The diverse experiences and perspectives of these students both inspire and inform our work together.”

Dr. Michelle Barton-Forbes is an Associate Scientist at Lawson and a Physician at London Health Sciences Centre (LHSC) specializing in paediatric infectious diseases. She is also an Assistant Professor at the Schulich School of Medicine & Dentistry, Western University.
“My research program is focused on the clinical epidemiology of infectious diseases in children, particularly in vulnerable paediatric populations such as neonates and young infants. A secondary area of interest is in bacterial resistance and antimicrobial stewardship. Through engagement in multicentre research and contribution to national guideline development, I am able to make a difference in the management and prevention of common childhood infections nationally. The combination of intense passion for my subspecialty, inquisitive curiosity and a drive to better understand common childhood illnesses is infectious to my students. I motivate my students to excellence by inspiring them to believe in themselves and their ability to make a difference. My students are encouraged and challenged to find answers to unanswered questions and unexplained trends through research. As a proud Canadian and an immigrant from a nation that prides itself in its diversity, I believe that diversity is our strength. The Jamaican national motto “out of many one people” has framed my worldview and has influenced my practice.”

Dr. Eileen Crowley is a Scientist at Lawson and a Pediatric Gastroenterologist at LHSC. She is also an Assistant Professor at the Schulich School of Medicine & Dentistry, Western University.
“My research interests include pediatric inflammatory bowel disease (IBD), the genetics of IBD, big datasets, therapeutic drug monitoring clinical trial endpoints and precision medicine. My work has served to be better delineate the genetic phenotype of children with IBD as well as optimizing response to therapy in this age group. I engage students and motivate them to work with enthusiasm! My aim is to create learning opportunities that are active, collaborative and promote learning relationships. Once I have identified a student’s goal, it is easier to share and attain that goal. Within the research setting, I aim to maintain an environment where every student feels accepted, valued and safe. Sharing of ideas creates opportunities whilst also fostering a sense of personal belonging and achievement.”
To learn more about International Women’s Day, visit https://www.internationalwomensday.com/.