Search
Search
London researchers collaborating on national dementia prevention program
Researchers at Lawson Health Research Institute are collaborating with Canada’s largest dementia research initiative, the Canadian Consortium on Neurodegeneration in Aging (CCNA), to study an innovative online program that offers older adults the opportunity to increase their knowledge of dementia and improve lifestyle risk factors. The program, Brain Health PRO (BHPro), offers interactive digital educational modules to empower older adults to improve their physical and mental health, and modify their risk factors for dementia.
“Using the BHPro modules participants will learn how to improve their physical and mental health and reduce their risk of cognitive impairment. It is particularly novel with the education modules being delivered remotely,” explains Dr. Michael Borrie, Scientist at Lawson and Medical Director for the Aging Brain and Memory Clinic at Parkwood Institute.
The bilingual program focuses on seven different modifiable dementia risk domains: exercise, nutrition, sleep, psychological and social health, cognitive engagement, heart health, and vision and hearing. For each, the program includes 10-minute educational videos, as well as interactive activities for users to complete. Participants will also be sent portable EEG headsets to measure their brain activity during sleep, and accelerometers to track their physical activity. With the rise of dementia anticipated to reach nearly one million Canadians over the next 12 years, dementia prevention is becoming an increasingly urgent national health priority.
“The launch of BHPro is part of a significant research effort to find concrete means of preventing dementia, with the ultimate goal of having tremendous benefits for the aging experience,” says Dr. Howard Chertkow, Scientific Director of the CCNA and Director of the Kimel Family Centre for Brain Health and Wellness at Baycrest.
“Alzheimer Society of Canada (ASC) is proud to support the launch of the BHPro through the CAN-THUMBS UP program,” adds Dr. Saskia Sivananthan, ASC’s Chief Research & KTE Officer.
BHPro is funded by the Canadian Institutes of Health Research and the ASC, and was created through the Canadian Therapeutic Platform Trial for Multidomain Interventions to Prevent Dementia (CAN-THUMBS UP) program, which is part of the CCNA. The study will support 350 older adults across Canada who have at least one risk factor for dementia, including up to 60 participants through Lawson, with the goal of seeing participants’ dementia risk reduced throughout the year-long study. Please note, there is limited space for research participants. To learn more, please visit canthumbsup.ca
About CCNA
CCNA is the national component of the CIHR dementia research strategy, bringing together over 340 researchers across Canada to collaboratively investigate the diagnosis, treatment and prevention of dementia and other age-related neurodegenerative diseases. For more information, visit ccna-ccnv.ca
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
London researchers discover novel method to diagnose long COVID
Study found unique blood biomarkers in patients with post-COVID-19 condition
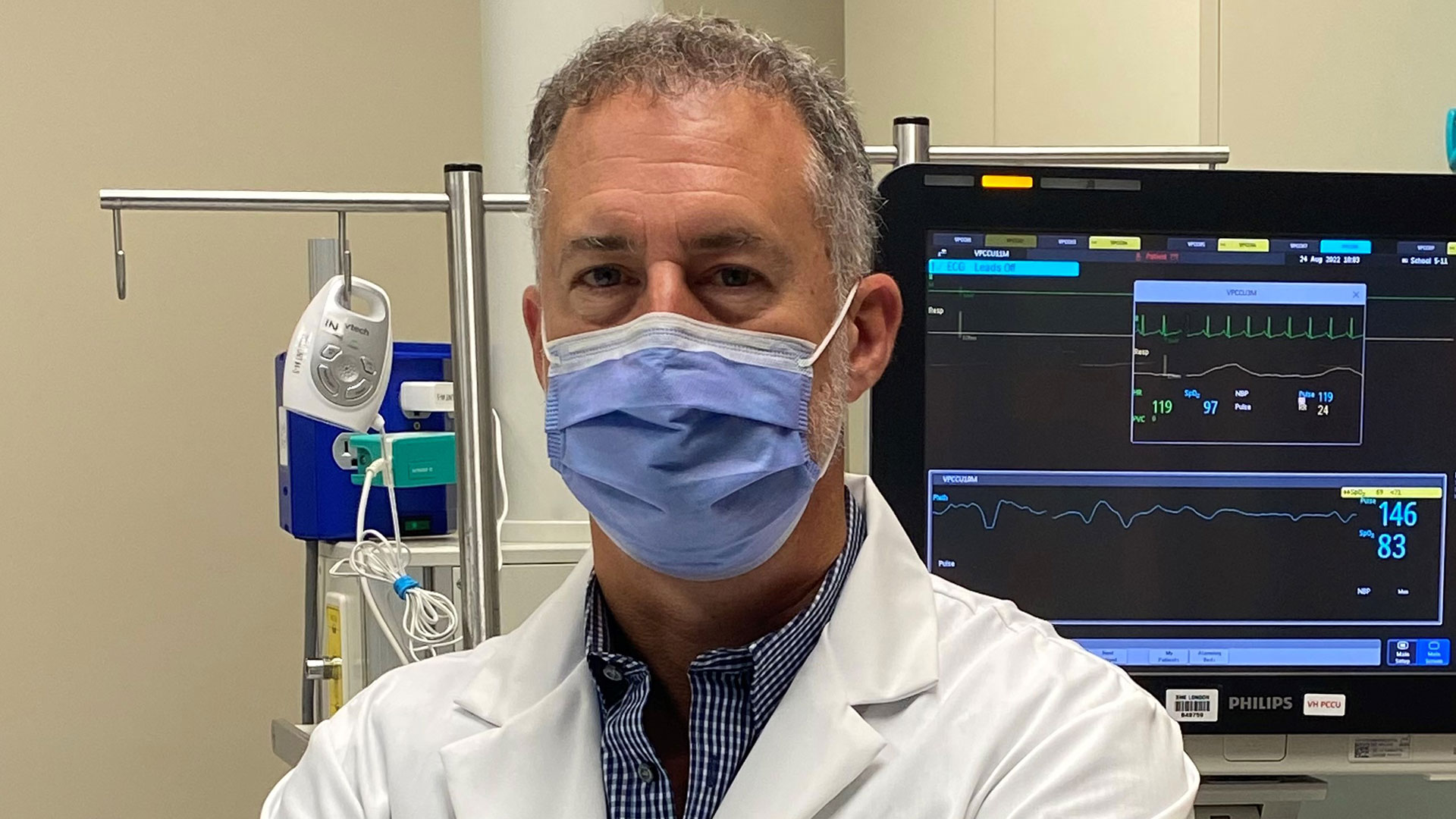
LONDON, ON – Published this week in Molecular Medicine, researchers at Lawson Health Research Institute have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition.
Long COVID occurs when someone experiences symptoms like fatigue, cognitive issues, shortness of breath and gastrointestinal issues after an initial COVID-19 diagnosis. It can sometimes take up to 12 months for the condition to occur.
“It’s estimated that 30 to 40 per cent of patients with COVID-19 will develop long COVID,” says Dr. Douglas Fraser, Lawson Scientist and Critical Care Physician at London Health Sciences Centre (LHSC). “Physicians currently rely on symptoms alone to diagnose the condition, but our research offers a unique profile of blood biomarkers that could be used in a clinical test.”
The researchers studied 140 blood samples from participants at LHSC and St. Joseph’s Health Care London, including St. Joseph’s Post-Acute COVID-19 Program. Participants were those with presumed long COVID, hospital inpatients with acute COVID-19 infection and healthy control subjects.
“We chose to study blood vessels that link all the body systems together to look for changes after an acute infection,” explains Dr. Fraser, who is also a Professor at Western University’s Schulich School of Medicine & Dentistry.
The team found that blood vessels of those with presumed long COVID were changing rapidly after a confirmed COVID-19 infection. They also found that patients with long COVID had 14 elevated blood biomarkers associate with blood vessels. With the help of machine learning, they discovered that two biomarkers called ANG-1 and P-SEL could be used to classify long COVID with 96 per cent accuracy.
“Long COVID is a relatively new condition and we have much to learn about it,” says Dr. Michael Nicholson, Associate Scientist at Lawson, Respirologist at St. Joseph’s and Associate Professor at Schulich Medicine & Dentistry. “This research advances our understanding of long COVID with the potential to improve diagnosis and patient care.”
The advantage of biomarkers is that they not only help diagnose a disease but also provide insight into potential treatments. The team is now focused on using their findings to create a clinical diagnostic test with a goal of also exploring therapeutics.
“With a point-of-care diagnostic test, we could confidently diagnose long COVID and eventually develop targeted therapeutics against these blood vessel changes that we have discovered,” says Dr. Fraser. “The ultimate goal is to improve patient outcomes following a long COVID diagnosis.”
This research was supported by funding from London Health Sciences Foundation, London Community Foundation and the AMOSO Innovation Fund. It builds on a growing body of COVID-19 research from scientists at Lawson Health Research Institute.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers discover novel method to diagnose long COVID
Study found unique blood biomarkers in patients with post-COVID-19 condition
Published this week in Molecular Medicine, researchers at Lawson Health Research Institute have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition.
Long COVID occurs when someone experiences symptoms like fatigue, cognitive issues, shortness of breath and gastrointestinal issues after an initial COVID-19 diagnosis. It can sometimes take up to 12 months for the condition to occur.
“It’s estimated that 30 to 40 per cent of patients with COVID-19 will develop long COVID,” says Dr. Douglas Fraser, Lawson Scientist and Critical Care Physician at London Health Sciences Centre (LHSC). “Physicians currently rely on symptoms alone to diagnose the condition, but our research offers a unique profile of blood biomarkers that could be used in a clinical test.”
The researchers studied 140 blood samples from participants at LHSC and St. Joseph’s Health Care London, including St. Joseph’s Post-Acute COVID-19 Program. Participants were those with presumed long COVID, hospital inpatients with acute COVID-19 infection and healthy control subjects.
“We chose to study blood vessels that link all the body systems together to look for changes after an acute infection,” explains Dr. Fraser, who is also a Professor at Western University’s Schulich School of Medicine & Dentistry.
The team found that blood vessels of those with presumed long COVID were changing rapidly after a confirmed COVID-19 infection. They also found that patients with long COVID had 14 elevated blood biomarkers associate with blood vessels. With the help of machine learning, they discovered that two biomarkers called ANG-1 and P-SEL could be used to classify long COVID with 96 per cent accuracy.
“Long COVID is a relatively new condition and we have much to learn about it,” says Dr. Michael Nicholson, Associate Scientist at Lawson, Respirologist at St. Joseph’s and Associate Professor at Schulich Medicine & Dentistry. “This research advances our understanding of long COVID with the potential to improve diagnosis and patient care.”

The advantage of biomarkers is that they not only help diagnose a disease but also provide insight into potential treatments. The team is now focused on using their findings to create a clinical diagnostic test with a goal of also exploring therapeutics.
“With a point-of-care diagnostic test, we could confidently diagnose long COVID and eventually develop targeted therapeutics against these blood vessel changes that we have discovered,” says Dr. Fraser. “The ultimate goal is to improve patient outcomes following a long COVID diagnosis.”
This research was supported by funding from London Health Sciences Foundation, London Community Foundation and the AMOSO Innovation Fund. It builds on a growing body of COVID-19 research from scientists at Lawson Health Research Institute.
The study’s first author Maitray Patel, is a MD/PhD candidate from Western’s Schulich Medicine & Dentistry. Patel worked on blood analysis under the supervision of Drs. Doug Fraser and Mark Daley.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers get $2.8 million in funding to support mental health and wellbeing of Canadian health care workers
The COVID-19 pandemic has had a tangible impact on the mental health and wellbeing of Canadian health care workers, who have faced challenges that include increased workloads, resource constraints and fears of exposure to COVID-19.

Announced today, researchers out of Lawson Health Research Institute's MacDonald Franklin OSI Research Centre, have received $2.8 million in funding from the Public Health Agency of Canada (PHAC) to launch a project that will support the mental health and wellbeing of Canadian health care workers. The project is titled “Promoting Resilience and Mental Health: Adapting Canada’s Department of National Defence Road to Mental Readiness (R2MR) Program to Support Canadian Health Care Workers.”
The project will adapt the current Road to Mental Readiness Program, created for the Canadian Military. The aim is to identify mental health and wellness barriers in health care institutions, and create a streamlined framework that will build and promote supportive environments within institutions across the nation.
“This program has been a personalized approach with the military, and we are now adapting it to focus on Canadian health care workers,” explains Dr. Anthony Nazarov, Associate Scientist at Lawson and the MacDonald Franklin OSI Research Centre at St. Joseph’s Health Care London. “We want to educate institutions to create an environment that supports wellness not just at the individual level, but at the institutional level as well.”
The project, which will span 14 months, will assist in the planning, adaptation and testing of the health care focused Road to Mental Readiness Program.
“One of the main reasons we felt this was necessary stems from a recent study our team conducted that focused on moral distress and the mental health of Canadian health care workers,” says Dr. Don Richardson, Lawson Scientist and Director of the MacDonald Franklin OSI Research Centre at St. Joseph’s. “Our preliminary study results found that many Canadian health care workers have been negatively impacted by the pandemic with conditions such as; posttraumatic stress disorder, stress and depression.”
Once the research team has adapted the current Road to Mental Readiness Program, they will test it with health care workers to confirm its efficacy.
“We hope to have this type of resiliency program adopted by health care organizations across the country,” explains Dr. Richardson. “If proven effective, this would provide additional tools to health care workers to help them cope, improve their resiliency and hopefully mitigate future staff shortages.”
The funding is part of the federal 2021 budget which has committed an investment of $50 million over two years to support projects that address posttraumatic stress disorder and trauma in frontline and essential workers, and others affected by the pandemic. The nine projects announced, totaling an investment of $28.2 million, is the first round of projects being supported through this Budget 2021 commitment.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers get $2.8 million in funding to support mental health and wellbeing of Canadian health care workers
LONDON, ON - The COVID-19 pandemic has had a tangible impact on the mental health and wellbeing of Canadian health care workers, who have faced challenges that include increased workloads, resource constraints and fears of exposure to COVID-19.
Announced today, researchers out of Lawson Health Research Institute's MacDonald Franklin OSI Research Centre, have received $2.8 million in funding from the Public Health Agency of Canada (PHAC) to launch a project that will support the mental health and wellbeing of Canadian health care workers. The project is titled “Promoting Resilience and Mental Health: Adapting Canada’s Department of National Defence Road to Mental Readiness (R2MR) Program to Support Canadian Health Care Workers.”
The project will adapt the current Road to Mental Readiness Program, created for the Canadian Military. The aim is to identify mental health and wellness barriers in health care institutions, and create a streamlined framework that will build and promote supportive environments within institutions across the nation.
“This program has been a personalized approach with the military, and we are now adapting it to focus on Canadian health care workers,” explains Dr. Anthony Nazarov, Associate Scientist at Lawson and the MacDonald Franklin OSI Research Centre at St. Joseph’s Health Care London. “We want to educate institutions to create an environment that supports wellness not just at the individual level, but at the institutional level as well.”
The project, which will span 14 months, will assist in the planning, adaptation and testing of the health care focused Road to Mental Readiness Program.
“One of the main reasons we felt this was necessary stems from a recent study our team conducted that focused on moral distress and the mental health of Canadian health care workers,” says Dr. Don Richardson, Lawson Scientist and Director of the MacDonald Franklin OSI Research Centre at St. Joseph’s. “Our preliminary study results found that many Canadian health care workers have been negatively impacted by the pandemic with conditions such as; posttraumatic stress disorder, stress and depression.”
Once the research team has adapted the current Road to Mental Readiness Program, they will test it with health care workers to confirm its efficacy.
“We hope to have this type of resiliency program adopted by health care organizations across the country,” explains Dr. Richardson. “If proven effective, this would provide additional tools to health care workers to help them cope, improve their resiliency and hopefully mitigate future staff shortages.”
The funding is part of the federal 2021 budget which has committed an investment of $50 million over two years to support projects that address posttraumatic stress disorder and trauma in frontline and essential workers, and others affected by the pandemic. The nine projects announced, totaling an investment of $28.2 million, is the first round of projects being supported through this Budget 2021 commitment.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers join global initiative to study loss of smell in COVID-19 patients
LONDON, ON – As part of an initiative called the Global Consortium for Chemosensory Research (GCCR), scientists at Lawson Health Research Institute and Western University are studying the sudden loss of smell in COVID-19 patients. They are asking individuals with confirmed or presumptive cases of COVID-19 worldwide to participate in a survey to better understand this symptom.
A sudden loss of smell, called anosmia, has been widely reported as a marker of COVID-19. More research is needed but emerging evidence suggests that more than 60 per cent of COVID-19 patients experience anosmia and that it is often the first symptom of the disease.
“While a sudden loss of smell is relatively rare, it is most commonly caused by an upper respiratory tract infection. It therefore stands to reason that COVID-19 could be causing anosmia,” says Dr. Leigh Sowerby, Associate Scientist at Lawson and Associate Professor at Western University’s Schulich School of Medicine & Dentistry. “Colleagues in the United Kingdom first made note of this with a surge of patients presenting with sudden loss of smell and many of these patients went on to develop COVID-19.”
In the new study, patients with loss of smell will answer questions through a publicly accessible survey. They will be asked about their experiences with COVID-19 and other respiratory illnesses. An immediate goal is to better understand the association between anosmia and COVID-19, and determine if loss of smell is the same in symptomatic and asymptomatic patients. The team also hopes to determine if loss of smell happens before other symptoms of COVID-19 as it could allow for earlier self-isolation advice.
“As a sinus surgeon, I see many patients who have lost their sense of smell. It really is the forgotten sense; we don’t appreciate smell until it’s gone,” explains Dr. Sowerby, who is also an Otolaryngologist at St. Joseph’s Health Care London. “Smell is a very important part of taste. Imagine if all food tasted like cardboard, and all you could do was make that cardboard taste spicy, salty, sweet or bitter. It can also be a safety concern if you cannot smell a gas leak, burning food or smoke.”
While there are existing therapies that can aid in regaining a sense of smell, it’s currently unknown whether they are effective for COVID-19 patients.
“We don’t yet know the long-term consequences of anosmia in COVID-19 patients and that’s why this research is important,” adds Dr. Sowerby. “I encourage anyone who has been diagnosed with COVID-19 or another respiratory illness to complete our survey if able.”
The GCCR survey is currently available in 10 languages at www.covidandsmell.com.
-30-
DOWNLOADABLE MEDIA

Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Global Consortium for Chemosensory Research (GCCR) is a group of global transdisciplinary scientists, clinicians, and patient advocates founded in response to the COVID-19 pandemic. With more than 500 members in 30 countries, the GCCR will harness their reach to conduct and analyze worldwide evidence-based research to combat the spread of COVID-19.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers join global initiative to study loss of smell in COVID-19 patients
As part of an initiative called the Global Consortium for Chemosensory Research (GCCR), scientists at Lawson Health Research Institute and Western University are studying the sudden loss of smell in COVID-19 patients. They are asking individuals with confirmed or presumptive cases of COVID-19 worldwide to participate in a survey to better understand this symptom.
A sudden loss of smell, called anosmia, has been widely reported as a marker of COVID-19. More research is needed but emerging evidence suggests that more than 60 per cent of COVID-19 patients experience anosmia and that it is often the first symptom of the disease.
“While a sudden loss of smell is relatively rare, it is most commonly caused by an upper respiratory tract infection. It therefore stands to reason that COVID-19 could be causing anosmia,” says Dr. Leigh Sowerby, Associate Scientist at Lawson and Associate Professor at Western University’s Schulich School of Medicine & Dentistry. “Colleagues in the United Kingdom first made note of this with a surge of patients presenting with sudden loss of smell and many of these patients went on to develop COVID-19.”
In the new study, patients with loss of smell will answer questions through a publicly accessible survey. They will be asked about their experiences with COVID-19 and other respiratory illnesses. An immediate goal is to better understand the association between anosmia and COVID-19, and determine if loss of smell is the same in symptomatic and asymptomatic patients. The team also hopes to determine if loss of smell happens before other symptoms of COVID-19 as it could allow for earlier self-isolation advice.
“As a sinus surgeon, I see many patients who have lost their sense of smell. It really is the forgotten sense; we don’t appreciate smell until it’s gone,” explains Dr. Sowerby, who is also an Otolaryngologist at St. Joseph’s Health Care London. “Smell is a very important part of taste. Imagine if all food tasted like cardboard, and all you could do was make that cardboard taste spicy, salty, sweet or bitter. It can also be a safety concern if you cannot smell a gas leak, burning food or smoke.”
While there are existing therapies that can aid in regaining a sense of smell, it’s currently unknown whether they are effective for COVID-19 patients.
“We don’t yet know the long-term consequences of anosmia in COVID-19 patients and that’s why this research is important,” adds Dr. Sowerby. “I encourage anyone who has been diagnosed with COVID-19 or another respiratory illness to complete our survey if able.”
The GCCR survey is currently available in 10 languages at www.covidandsmell.com.
London researchers part of a federal funding boost to enhance transition in care research
How can we improve health care for Canadians experiencing “transitions in care” to ensure they don’t fall through the cracks as they move through the health care system?
That’s the question two London researchers are aiming to answer, with the support of nearly $1.5 million in federal funding announced today at Western University's Schulich School of Medicine & Dentistry.
Peter Fragiskatos, MP for London North Centre, announced the funding boost on behalf of Federal Health Minister Jean-Yves Duclos, alongside Dr. Jane Rylett, Scientific Director of the Institute of Aging with the Canadian Institutes of Health Research (CIHR).

“When a person experiences a transition in care, whether moving from surgery to rehabilitation or aging out of pediatric care, the quality of their care and their health can be at risk,” said Bryan Neff, Western’s acting vice president of research, who hosted the funding announcement. “With federal investments like this, Western will continue to lead the way in identifying how to provide the best possible care for Canadians while improving efficiency in the health-care system.”
Transitions in care happen when responsibility for a person’s care shifts between providers, institutions or sectors. Some groups, such as patients with complex medical conditions, Indigenous peoples, and new immigrants, are particularly vulnerable to poor outcomes during transitions.
People with diabetes – a complex, typically life-long condition – fall into this category, which is why London’s Primary Care Diabetes Support Program (PCDSP) was developed. The clinic, which is part of the Centre for Diabetes, Endocrinology and Metabolism at St. Joseph’s Health Care London, is based at St. Joseph’s Family Medical and Dental Centre. The program provides diabetes support and management for individuals with type 2 diabetes who don’t have a family doctor or who may have additional medical and social issues that make diabetes management particularly challenging.
Maria Mathews, PhD, and her team at Schulich Medicine will evaluate the program to determine its impact on patient health, and on health-care providers, diabetes-related complications, and health system costs.
“While this program has already been shown to deliver high-quality care, my team is examining its overall impact to determine whether this model could be expanded to other sites and to support other chronic conditions,” said Mathews, a professor in the department of family medicine. With the $895,000 investment in her research, Mathews will determine “how we can best provide high- quality care for people with chronic conditions in a way that supports their health, eases strain on family doctors, and creates efficiencies in the health care system.”

Laura Brunton, PhD, an assistant professor at the School of Physical Therapy in Western’s Faculty of Health Sciences, received more than half a million dollars in CIHR funding.
Her team will examine a local program based at St. Joseph’s Parkwood Institute – called the Transitional and Lifelong Care Program (TLC) – that supports people with childhood-onset disabilities as they transition to adult care. This includes many patients with brain-based, neurodevelopmental conditions, such as cerebral palsy, spina bifida and developmental disabilities, as they move into adult care.
“Many of these patients have experienced severe health inequities because of the gaps in care when transitioning from pediatric care to the adult sector,” said Brunton, also a physiotherapist at St. Joseph’s Health Care London and affiliate scientist at Lawson Health Research Institute. “We’re going to evaluate the TLC model as an intervention that provides transitional, lifelong care and reduces the barriers experienced.”
Roy Butler, president of St. Joseph’s Health Care London, said today’s announcement highlights the synergy and collaboration among these organizations.
“We are happy to hear that work being done by both Laura Brunton and Maria Mathews to improve patient care is being recognized through this funding announcement. The two areas these talented researchers will be studying are innovative and ground-breaking with compassionate, forward-thinking teams who provide highly acclaimed care to vulnerable patients.”

Fragiskatos emphasized the vital importance of funding this field of research, given that most Canadians will experience a ‘transition in care’ at some point.
“People living in Canada routinely experience transitions in care as they navigate the health system. The important research that will be done here in London and at institutions across the country will help develop meaningful approaches to make these transitions easier for patients and caregivers,” he said.
Local researchers were among 14 groups across Canada that received approximately $12 million in federal funding to improve continuity of care for Canadians through the “Transitions in Care” initiative, which is provided in partnership with the Azrieli Foundation, Mitacs, and the Rossy Family Foundation.
London researchers team up with Diagnostics Biochem Canada to study COVID-19
LONDON, ON – Researchers at Lawson Health Research Institute (Lawson) and Western University have teamed up with local biotech company, Diagnostics Biochem Canada Inc. (DBC), to help us better understand COVID-19 and the body’s immune response to the infection.
A recently published study followed 28 critically ill patients at London Health Sciences Centre (LHSC); 14 who tested positive for COVID-19 and 14 who tested negative. They also followed 14 mildly ill non-hospitalized patients with COVID-19 and 14 healthy controls. The researchers tracked their body’s immune responses and found that all COVID-19 positive patients had a robust antibody response to the infection, even those with poorer outcomes.
“Our previous research showed that in severe cases of COVID-19, the body produces what’s called a cytokine storm, or an intense, initial immune response. However, in this new study, we observed that after a few days and weeks in critical care, the body produced a later, humoral antibody response that is equivalent to what we would expect with any similar infection,” explains Dr. Douglas Fraser, lead researcher and Critical Care Physician at LHSC.
Patients with COVID-19 reacted to the infection and produced ample anti-SARS-CoV-2 antibodies, including those who passed away. This finding suggests that blunted immune responses – when there is a lack of antibody production - did not contribute to mortality. Dr. Fraser says that based on their data, the focus of treatment should shift to combatting the viral load a person receives, and the body’s more immediate reaction to the infection.
This research was made possible through a collaboration between Lawson, Western and DBC, with DBC providing the serological testing kits.
“DBC was the first Canadian company to launch Health Canada-authorized serological tests for COVID-19 and we are happy that our scientists have been working with Lawson on this important study. We look forward to continuing this collaboration and supplying Canadian labs with much needed serological tests,” says Manon Hogue, CEO at DBC.
Analyzing serum antibody levels using a blood test could help improve patient outcomes by allowing early identification of who may require certain treatments, and guide decisions around patient cohorting. In addition, serological testing allows for viral surveillance and its immunity in the community.
London West MP, Kate Young adds, “London is once again showing the world that we are leading the way in scientific research into our most pressing health issues. It’s great to see a local business, Diagnostics Biochem Canada Inc., team up with the Lawson Health Research Institute to help better understand Covid-19. Working together they will help us unlock the keys to how Covid-19 impacts the body’s immune system.”
The study, “Critically Ill COVID-19 Patients Exhibit Anti-SARS-CoV-2 Serological Responses,” is published in the journal Pathophysiology.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
We have been exporting our products around the globe for over 47 years. As a leader in the industry, it has always been our goal to offer a wide range of test kits and continually introduce new and unique products to the marketplace. It is our strong commitment to research, development, and manufacture that has enabled us to offer our customers ongoing, unique, and quality products.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers working on a proactive approach to inclusiveness in the classroom
LONDON, ON – Researchers at Lawson Health Research Institute have launched a pilot study and pilot project called Queer in the Classroom, to examine the benefits of a proactive, inclusive approach within the education system for those who are part of the 2SLBTGQIA+ student community.
“The Queer in the Classroom initiative is so important because when we look at the data, youth in the 2SLGBTQIA+ community are 14 times more likely to die by suicide,” says Dr. Arlene MacDougall, Lawson Scientist, Director of MINDS and Psychiatrist at St. Joseph’s Health Care London. “We need to be focusing on this population who are also experiencing a higher degree of isolation, stigma and substance use.”
The pilot project focuses on professional development for teachers and staff to help create an environment that is tailored to best support 2SLGBTQIA+ students through the additional stress they face as a minority group.
“This project is about connecting with school boards and teachers to help develop the knowledge and skills to create spaces that go beyond tolerating differences,” explains MacDougall. “The focus is to create an environment that is more affirming, that is more responsive and more proactive rather than reactive.”
The foundation for the pilot project came from a scoping review of existing research on this topic conducted by the research team through the Mental Health INcubator for Disruptive Solutions (MINDS), that looked extensively at how teachers themselves can create a classroom that embraces all students.
“We further conducted our own research based on a series of interviews of 2SLGBTQIA+ students at both elementary and secondary schools in Ontario, and their parents and teachers. We focused on not only their safety in school, but also being celebrated for who they are,” says Iylah Neves, Lawson Research Assistant through MINDS. “We drew on all of this research to best inform the practices we are using with the Queer in the Classroom initiative.”
Currently the Queer in the Classroom project is being rolled out on a ‘by-request’ basis. However, the research team is working with a couple of school boards within Ontario to discuss the possibility of wider implementation.
“Queer in the Classroom has been driven by the voices of students with personal experiences who feel there is a deep need for this type of innovation,” says Neves. “It is our responsibility to make those changes so that students can access a safe, inclusive and nurturing environment.”
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London researchers working on a proactive approach to inclusiveness in the classroom
Researchers at Lawson Health Research Institute have launched a pilot study and pilot project called Queer in the Classroom, to examine the benefits of a proactive, inclusive approach within the education system for those who are part of the 2SLBTGQIA+ student community.
“The Queer in the Classroom initiative is so important because when we look at the data, youth in the 2SLGBTQIA+ community are 14 times more likely to die by suicide,” says Dr. Arlene MacDougall, Lawson Scientist, Director of MINDS and Psychiatrist at St. Joseph’s Health Care London. “We need to be focusing on this population who are also experiencing a higher degree of isolation, stigma and substance use.”
The pilot project focuses on professional development for teachers and staff to help create an environment that is tailored to best support 2SLGBTQIA+ students through the additional stress they face as a minority group.
“This project is about connecting with school boards and teachers to help develop the knowledge and skills to create spaces that go beyond tolerating differences,” explains MacDougall. “The focus is to create an environment that is more affirming, that is more responsive and more proactive rather than reactive.”
The foundation for the pilot project came from a scoping review of existing research on this topic conducted by the research team through the Mental Health INcubator for Disruptive Solutions (MINDS), that looked extensively at how teachers themselves can create a classroom that embraces all students.

“We further conducted our own research based on a series of interviews of 2SLGBTQIA+ students at both elementary and secondary schools in Ontario, and their parents and teachers. We focused on not only their safety in school, but also being celebrated for who they are,” says Iylah Neves, Lawson Research Assistant through MINDS. “We drew on all of this research to best inform the practices we are using with the Queer in the Classroom initiative.”
Currently the Queer in the Classroom project is being rolled out on a ‘by-request’ basis. However, the research team is working with a couple of school boards within Ontario to discuss the possibility of wider implementation.
“Queer in the Classroom has been driven by the voices of students with personal experiences who feel there is a deep need for this type of innovation,” says Neves. “It is our responsibility to make those changes so that students can access a safe, inclusive and nurturing environment.”
London scientists clinch $2 million in federal funding to develop better imaging tools for brain disease
LONDON, ON – Lawson Health Research Institute has been awarded over $2 million in federal funding for a project focusing on two unique medical imaging systems designed to give unparalleled insight into brain function and disease.
Today, the Right Honourable Justin Trudeau, Prime Minister of Canada, announced more than $518 million in research infrastructure support through the Canada Foundation for Innovation (CFI). In a live conversation today at 1 p.m., the Honourable François-Philippe Champagne, Minister of Innovation, Science and Industry, will share more about how the funding will support 102 state-of-the-art projects at 35 post-secondary institutions and research hospitals across the country - helping Canada remain at the forefront of exploration, innovation and discovery.
“Imaging technologies, such as MRI and PET scanners, have revolutionized our understanding and treatment of major neurological diseases, including dementia and mental illness, by allowing us to study disease mechanisms and their impact on brain health,” says Dr. Keith St. Lawrence, Lawson Scientist and project co-lead. “We are developing and testing two leading-edge systems that will enable imaging of key vascular, metabolic and molecular factors linked to disease.”
The first system is a head-only PET (positron emission tomography) insert that can be placed in any clinical MRI machine. Combining the molecular specificity of PET with the structural and functional capabilities of MRI, the possibilities for brain imaging will be greatly enhanced. The head-only PET insert being tested in London has been developed by Cubresa Inc., located in Winnipeg, Manitoba.
“Combined with deep-learning approaches, we could achieve a highly improved sensitivity of the PET insert and reduce the radiation dose by up to 50 times compared to whole-body imaging,” explains Dr. Jonathan Thiessen, Lawson Scientist and project co-lead. “This will be the first commercially available high-resolution brain PET/MRI installed in the world.”
For example, better diagnosis of different forms of dementias would be possible and researchers could closely compare protein abnormalities in the brain with cognitive function. The low radiation dose allows for long-term studies investigating changes in the brain and neuroinflammation that can lead to major psychiatric diseases and cognitive degeneration or disability.
The second system uses portable, state-of-the-art optical imaging to increase the reliability of bedside brain monitoring to provide rapid assessment of brain health in restrictive environments.
“We believe this technology will demonstrate how biomedical optics can improve neurological outcome for surgery and patients in intensive care, provide an accessible technology for assessing neurovascular health, and become a clinically relevant tool for monitoring changes in brain function,” says Dr. St. Lawrence.
With current systems, the type of data is limited and extremely vulnerable to signal contamination from the scalp which can overshadow signals from the brain. Using the team’s specialized detection approach, the scalp signal contributions could be greatly reduced to get more accurate information on markers of brain activity, such as cerebral blood flow and energy metabolism.
The team will study use of the system in surgical and intensive-care settings to monitor for cerebral ischemia and metabolic stress, which are the major causes of brain injury. They will also monitor treatment in patients with schizophrenia and study dysfunction in the brain associated with negative symptoms, as cognitive impairment deteriorates with age for some people with the disease. Another goal is to develop a brain-computer interface for patients who are incapable of physical communication.
“With this funding, we can develop a truly unique advancement that has the potential to test the limits of optics for brain applications,” adds Dr. Thiessen. These two imaging platforms build on previous investments in Lawson Imaging that now exceed over $40 million in research funds since the initial CFI support in hybrid imaging in 2007.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London scientists clinch $2 million in federal funding to develop better imaging tools for brain disease
Lawson Health Research Institute has been awarded over $2 million in federal funding for a project focusing on two unique medical imaging systems designed to give unparalleled insight into brain function and disease.
The Right Honourable Justin Trudeau, Prime Minister of Canada, announced more than $518 million in research infrastructure support through the Canada Foundation for Innovation (CFI).
“Canada's researchers and scientists are some of the brightest and most skilled in the world. These investments will ensure that they have the cutting-edge laboratories and equipment needed to help us build a Canada that is healthier, greener, and more competitive," says The Rt. Hon. Justin Trudeau, Prime Minister of Canada.
In a live conversation, the Honourable François-Philippe Champagne, Minister of Innovation, Science and Industry, shared more about how the funding will support 102 state-of-the-art projects at 35 post-secondary institutions and research hospitals across the country - helping Canada remain at the forefront of exploration, innovation and discovery.

The first system is a head-only PET (positron emission tomography) insert that can be placed in any clinical MRI machine. Combining the molecular specificity of PET with the structural and functional capabilities of MRI, the possibilities for brain imaging will be greatly enhanced. The head-only PET insert being tested in London has been developed by Cubresa Inc., located in Winnipeg, Manitoba.

For example, better diagnosis of different forms of dementias would be possible and researchers could closely compare protein abnormalities in the brain with cognitive function. The low radiation dose allows for long-term studies investigating changes in the brain and neuroinflammation that can lead to major psychiatric diseases and cognitive degeneration or disability.
The second system uses portable, state-of-the-art optical imaging to increase the reliability of bedside brain monitoring to provide rapid assessment of brain health in restrictive environments.
“We believe this technology will demonstrate how biomedical optics can improve neurological outcome for surgery and patients in intensive care, provide an accessible technology for assessing neurovascular health, and become a clinically relevant tool for monitoring changes in brain function,” says Dr. St. Lawrence.
With current systems, the type of data is limited and extremely vulnerable to signal contamination from the scalp which can overshadow signals from the brain. Using the team’s specialized detection approach, the scalp signal contributions could be greatly reduced to get more accurate information on markers of brain activity, such as cerebral blood flow and energy metabolism.
The team will study use of the system in surgical and intensive-care settings to monitor for cerebral ischemia and metabolic stress, which are the major causes of brain injury. They will also monitor treatment in patients with schizophrenia and study dysfunction in the brain associated with negative symptoms, as cognitive impairment deteriorates with age for some people with the disease. Another goal is to develop a brain-computer interface for patients who are incapable of physical communication.
“With this funding, we can develop a truly unique advancement that has the potential to test the limits of optics for brain applications,” adds Dr. Thiessen.
These two imaging platforms build on previous investments in Lawson Imaging that now exceed over $40 million in research funds since the initial CFI support in hybrid imaging in 2007. London is home to Canada’s first whole body PET/MRI scanner that was installed at St. Joseph’s Hospital, part of St. Joseph’s Health Care London.
London scientists key players in national dementia strategy
LONDON, ON – Researchers in London have been awarded $1.345 million over five years through the second phase of the Canadian Consortium on Neurodegeneration in Aging (CCNA), announced today as part of Canada’s national dementia strategy. CCNA is a collaborative research program tackling the challenge of dementia and other neurodegenerative illnesses.
Dr. Manuel Montero-Odasso, Scientist at Lawson Health Research Institute, is world renowned for his findings on the relationship between cognition and mobility in the elderly, and gait as a predictor of frailty and dementia. He leads the Mobility, Exercise and Cognition (MEC) Team in London, comprised of top researchers in the areas of mobility, exercise and brain health.
“Evidence from other countries with national dementia strategies shows that coordinated, targeted efforts at the national level improves results for all aspects of dementia care and also for research,” says Dr. Montero-Odasso, also a geriatrician and Director of the Gait and Brain Lab at Parkwood Institute, a part of St. Joseph’s Health Care London.
CCNA was purpose-built to synergize dementia research within the Canadian context. Phase I saw the creation of infrastructure fostering collaboration amongst Canadian researchers, and there are now 20 teams built around important research topics.
“This kind of effective national collaboration by scientists and clinicians from many disciplines gives the CCNA a cutting edge in research, prevention, treatment and management of all forms of dementia,” explains Dr. Montero-ODasso. “We created a national network of researchers form west to east coast with a high level of expertise to deliver lifestyle interventions to improve cognition and slow down progression to dementia. I feel privileged working with such excellent investigators and leading this important endeavour locally.”
The MEC team has several projects in the works, but the majority of the new funding is to complete the SYNERGIC Trial, SYNchronizing Exercises and Remedies on Gait and Cognition.
This first-in-the-world clinical study is testing a triple intervention aimed at treating Mild Cognitive Impairment (MCI) and delaying the onset of dementia. The SYNERGIC Trial incorporates physical exercises and cognitive training, along with vitamin D supplementation to determine the best treatment for improving mobility and cognition.
“We are looking at how interventions will work together and targeting cognitive decline at its earliest stage – individuals with MIC,” explains Dr. Montero-Odasso. “Both physical and cognitive exercises have shown promising effects for maintaining cognition, while vitamin D deficiency is associated with cognitive decline.”
A professor at Western University’s Schulich Medicine & Dentistry, Dr. Montero-Odasso partners with researchers from across the city including Dr. Rob Bartha, imaging scientist at Schulich Medicine & Dentistry and Robarts Research Institute at Western University, and Dr. Kevin Schoemaker who leads the Laboratory for Brain and Heart Health.
Study participants in the SYNERGIC Trial are asked to complete an individualized and progressive routine of exercises and cognitive training three times a week for six months, with one final assessment at 12 months. The main site for the study is Parkwood Institute with the physical exercises taking place at the Labatt Health Sciences Building on the Western campus.
“Our preliminary analysis is giving us a strong indication that a multimodal approach, combining physical exercise, cognitive training and supplementation, has a synergistic effect. It seems the whole is greater than the sum of its parts,” says Dr. Montero-Odasso.
To date, 138 research patients has been recruited across multiple sites in Canada. Individuals over 60 years old with mild cognitive impairment without dementia are eligible for this clinical trial. Those interested in participating are encouraged to contact a Lawson research coordinator at 519-685-4292 ext. 42910.
Dr. Montero-Odasso adds that “as our population ages, a comprehensive strategy is vital to ensure the growing number of those living with dementia receive the care and support they deserve. Over half a million Canadians are currently living with dementia. By 2031, this number is expected to nearly double.” More than one third of dementia cases might be preventable.
'In CCNA’s Phase II, researchers are working on analyzing the overall health of every patient in a large clinical cohort study, COMPASS-ND. This information will be used to enhance understanding of how changes in the brain affect dementia severity and ways to reduce and prevent this through lifestyle changes. Lawson is the leading recruitment site for COMPASS-ND and the London team will be instrumental in the larger lifestyle interventions moving forward.
CCNA is funded by the Government of Canada, Canadian Institutes of Health Research (CIHR) and other funding partners.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
London’s health community announces partnership with Canon Medical
Building on established excellence in medical imaging, Western University and London’s academic teaching hospitals, London Health Sciences Centre (LHSC), and St. Joseph’s Health Care London announced today a unique partnership with Canon Medical Systems Canada in advanced Computed Tomography (CT) that will advance patient care, research and teaching in Southwestern Ontario.
This new partnership includes the investment of a $4.5 million dedicated research CT, Angio Suite and portable ultrasound machine to be used for medical imaging research. London will also become home to the world’s largest installation of the most advanced CT platform from Canon Medical.
“London has an international reputation as a leader in medical imaging, and today we are celebrating a partnership that will build on that foundation of imaging excellence,” said Dr. Narinder Paul, Chair/Chief of the Department of Medical Imaging at Western’s Schulich School of Medicine & Dentistry, LHSC and St. Joseph’s. “Thanks to Canon’s investment, we will, for the first time, have the same CT equipment being used for patient care as we are using for research.”
CT is used to provide critical diagnostic information through combination of thousands of ultralow dose, high resolution X-ray images to create cross-sectional images of the brain, the heart, lungs, abdominal and pelvic organs, and of the blood vessels. CT provides essential imaging for most medical and surgical emergencies and is the standard of care for routine assessment and evaluation of patients with a wide range of conditions including many cancers. CT is also used to guide interventions for diagnosis through obtaining tissue biopsies, and is used to guide minimally invasive treatment.
Because the research CT will exactly mirror the equipment used clinically, it will allow researchers to more quickly and readily apply their research findings to patient care. The research in London will focus on improving patient safety by finding ways to lower radiation dose, developing faster and more detailed imaging techniques, and personalizing the patient experience.

This partnership includes the investment of a dedicated research CT, Angio Suite and portable ultrasound machine.
The partnership with Canon Medical also provides the opportunity to establish a training academy and a Canon Medical National Centre of Excellence in London. As new advanced CT protocols are developed and validated here, hands-on training will be provided for medical imaging teams from across the province, the country and the world.
“As Southwestern Ontario’s only medical school, we are very pleased that the partnership also provides for the establishment of a training academy,” said Dr. Davy Cheng, Acting Dean, Schulich School of Medicine & Dentistry, Western University. “We expect this training to attract interest from medical learners and professionals internationally, and we will welcome them to London to learn from our clinical and research leaders.”
In addition, LHSC and St. Joseph’s are acquiring six clinical CTs to be used for patient care, which will standardize all of the CT equipment at London’s hospitals. Two will be installed at University Hospital, three at Victoria Hospital and one at St. Joseph’s.
“The investment in these six new machines means a standardization of all CT equipment at London’s hospitals, and more importantly, ensures we will have the best available technology for patients – offering lower radiation doses with each scan, and producing higher resolution images enabling more precise detection and diagnosis,” said Dr. Paul Woods, President and CEO, London Health Sciences Centre.
“London is renowned for its excellence in imaging and has been at the forefront of significant advancements in technology, clinical translation and training over many years. We have been a city of numerous national firsts in imaging dating back decades. Today we take that excellence to a new level with an exciting and innovative partnership that will advance health care, teaching and research in our city,” said Dr. Gillian Kernaghan, President and CEO, St. Joseph’s Health Care London.
Following installation, further research to validate use and drive innovations can be done effectively and efficiently within the clinical setting, done by hospital-based researchers through Lawson Health Research Institute, the research institute of LHSC and St. Joseph’s.
“London’s integrated health care and research community is well-positioned to make the most of this opportunity, which ultimately means we can continually improve care for the patients and families that we serve,” said Dr. David Hill, Lawson Scientific Director and Integrated Vice President, Research for London’s hospitals.
LOVE YOUR BUGS! The female microbiome and prevention of disease
Women & their Microbes is proud to host a public event in collaboration with Junior League of Hamilton-Burlington on the female microbiome and prevention of disease on March 7 at 7 p.m. at the David Braley Health Sciences Centre in Hamilton. Let's celebrate women on the eve of International Women's Day!
Invited experts Dr. Vivien Brown, leading family physician, and Dr. Gregor Reid, world renowned microbiome scientist, will talk about the good bugs in your body and what they can do for you.
Not sure what is fact and what is fake? Bring your questions about the female microbiome and probiotics!
When: March 7, 2019 from 7 - 9 p.m., doors open at 6:30 p.m.
Where: David Braley Health Sciences Centre Auditorium, 100 Main Street West, Hamilton, Ontario
There is no fee or registration required, but space is limited.
For more information, please visit www.womenandtheirmicrobes.com or see the attached poster.
Machine learning could predict medication response in patients with complex mood disorders
Mood disorders like major depressive disorder (MDD) and bipolar disorder are often complex and hard to diagnose, especially among youth when the illness is just evolving. This can make decisions about medication difficult. In a collaborative study by Lawson Health Research Institute, The Mind Research Network and Brainnetome Center, researchers have developed an artificial intelligence (AI) algorithm that analyzes brain scans to better classify illness in patients with a complex mood disorder and help predict their response to medication.
The full study included 78 emerging adult patients from mental health programs at London Health Sciences Centre (LHSC), primarily from the First Episode Mood and Anxiety Program (FEMAP). The first part of the study involved 66 patients who had already completed treatment for a clear diagnosis of either MDD or bipolar type I (bipolar I), which is a form of bipolar disorder that features full manic episodes, as well as an additional 33 research participants with no history of mental illness. Each individual participated in scanning to examine different brain networks using Lawson’s functional magnetic resonance imaging (fMRI) capabilities at St. Joseph’s Health Care London.
The research team analyzed and compared the scans of those with MDD, bipolar I and no history of mental illness, and found the three groups differed in particular brain networks. These included regions in the default mode network, a set of regions thought to be important for self-reflection, as well as in the thalamus, a ‘gateway’ that connects multiple cortical regions and helps control arousal and alertness.
The data was used by researchers at The Mind Research Network to develop an AI algorithm that uses machine learning to examine fMRI scans to classify whether a patient has MDD or bipolar I. When tested against the research participants with a known diagnosis, the algorithm correctly classified their illness with 92.4 per cent accuracy.
The research team then performed imaging with 12 additional participants with complex mood disorders for whom a diagnosis was not clear. They used the algorithm to study a participant’s brain function to predict his or her diagnosis and, more importantly, examined the participant’s response to medication.
“Antidepressants are the gold standard pharmaceutical therapy for MDD while mood stabilizers are the gold standard for bipolar I,” says Dr. Elizabeth Osuch, a clinician-scientist at Lawson, medical director at FEMAP and co-lead investigator on the study. “But it becomes difficult to predict which medication will work in patients with complex mood disorders when a diagnosis is not clear. Will they respond better to an antidepressant or to a mood stabilizer?”
The research team hypothesized that participants classified by the algorithm as having MDD would respond to antidepressants while those classified as having bipolar I would respond to mood stabilizers. When tested with the complex patients, 11 out of 12 responded to the medication predicted by the algorithm.
“Machine learning is an approach that learns in a data-centric way, providing information that can be used to predict future data sets. In this case, that’s the prediction of MDD from bipolar I,” says Dr. Vince Calhoun, President of The Mind Research Network; Distinguished Professor, Departments of Electrical and Computer Engineering, Neurosciences, Computer Science, and Psychiatry at The University of New Mexico; and co-lead investigator on the study. “There are multiple layers of algorithms in this project. The first layer includes an approach that automatically extracts brain networks from the data provided and the second layer includes automatically identifying which combinations of networks are most sensitive or predictive of MDD and bipolar I.”

Above: Dr. Vince Calhoun
“This study takes a major step towards finding a biomarker of medication response in emerging adults with complex mood disorders,” says Dr. Osuch. “It also suggests that we may one day have an objective measure of psychiatric illness through brain imaging that would make diagnosis faster, more effective and more consistent across health care providers.”
Psychiatrists currently make a diagnosis based on the history and behavior of a patient. Medication decisions are based on that diagnosis. “This can be difficult with complex mood disorders and in the early course of an illness when symptoms may be less well-defined,” says Dr. Osuch. “Patients may also have more than one diagnosis, such as a combination of a mood disorder and a substance abuse disorder, further complicating diagnosis. Having a biological test or procedure to identify what class of medication a patient will respond to would significantly advance the field of psychiatry.”
The study, “Complexity in mood disorder diagnosis: fMRI connectivity networks predicted medication-class of response in complex patients,” is published online in Acta Psychiatrica Scandinavica. Local support included donor funding through London Health Sciences Foundation.
Learn more about this research:

Above: Drs. Elizabeth Osuch and Jean Théberge, Lawson scientists
Major Ronald Miller's story
“I just wasn’t myself,” says Major Ronald Miller when reflecting on his experience with post-traumatic stress disorder (PTSD). “I could see a significant change in my personality that just wasn’t me.”
Major Miller first joined the Canadian Armed Forces in 1971 as a young infantry private in the 1st Battalion, The Royal Canadian Regiment and later became an Officer in the Royal Canadian Artillery, which included a tour in Germany during the Cold War.
After the Cold War, he reoriented his career towards peacekeeping which saw him deployed to seven different conflict zones. “It was during the Civil War in El Salvador in 1991 that I experienced a number of incidents that first triggered my PTSD,” explains Major Miller. “From that time forward the PTSD was always there but I suppressed it.”
It wasn’t until 2016 that Major Miller’s PTSD resurfaced. After retiring from the Canadian Armed Forces in 2008, he started working a number of contracts in support of the military.
“Over the years, I was exposed to the kind of death and destruction that can be rather difficult from a psychological standpoint. The older I got, the less I was able to suppress those experiences. In fall 2016, I was supporting a NATO military exercise in the UK when I began experiencing horrible nightmares every night. I knew I needed to seek help.”
He reached out to Veteran Affairs Canada and was referred to the Operational Stress Injury (OSI) Clinic at Parkwood Institute, a part of St. Joseph’s Health Care London, where he was diagnosed with PTSD. It was there that he learned about PTSD research being conducted by Dr. Ruth Lanius, Scientist at Lawson Health Research Institute and Psychiatrist at London Health Sciences Centre.

“I saw the need to help by participating in research, not only for myself but for my friends who have succumbed to the illness.”
Major Miller participated in Dr. Lanius’ neuroimaging research which uses advanced imaging technologies like PET/MRI to study differences in brain activity and neural connections between healthy individuals and those with different subtypes of PTSD. Dr. Lanius hopes that patterns of brain activity can one day be used as an objective biomarker to accurately diagnosis different subtypes of PTSD and uncover new targets for therapy.
“The research experience was interesting. I was interviewed while in the MRI and had to talk about incidents that trigger my PTSD to study my brain waves,” explains Major Miller.
In one study, Dr. Lanius is studying patterns of brain activity for those with ‘moral injury,’ an intense feeling of shame or guilt that can sometimes affect veterans with PTSD.
“Sometimes you’re involved in situations that you don’t have control over but that you feel responsible for,” says Major Miller. “You wonder, ‘Could I have done something differently?’”
Major Miller was happy to participate in any study that might help. Today, he is managing his PTSD through a combination of therapies that work for him.
“My biggest fear was giving up the things I love. I’ve been a soldier since day one and I’m sure I will be until the day I die. It’s important we come up with solutions to ensure our veterans receive proper care. Through research, we can tailor treatment to the individual rather than looking for a broad brush solution that might not suit everyone.”
This story is also featured on Research Canada’s Patient Stories website.
Manuel Montero-Odasso
Manuel Montero-Odasso, MD; PhD
Professor, Schulich School of Medicine and Dentistry
Mobility, Cognitive and Brain Health
Dr. Manuel Montero-Odasso is a geriatrician at Parkwood Institute and Professor and Faculty Scholar in the Schulich School of Medicine and Dentistry at Western University. He is also the Director of the Gait & Brain Lab at Parkwood Institute, a clinician-scientist at the Lawson Health Research Institute and serves as team leader at the Canadian Consortium on Neurodegeneration in Aging and the Ontario Neurodegenerative Research Initiative.
Dr. Montero-Odasso leads the Gait and Brain Health Program goal of understanding mechanisms and treatments of mobility and cognitive decline in aging by focusing on the interaction between gait performance and cognition and how this increases the risk of falls. Through this work Dr. Montero-Odasso has established the use of “motor biomarkers”, like slowing of gait speed and dual-task effects on gait to predict frailty, falls, and dementia. He is also a co-PI of the Canadian Therapeutic Platform for Multidomain Interventions to Prevent Dementia, which focuses on multi-domain lifestyle interventions that include physical exercises, cognitive training, diet, self-management of cardiovascular factors and sleep, in order to reduce the risk or delay the onset of dementia in older adults.
Dr. Montero-Odasso has received more than $6 million of competitive peer-reviewed research funding, has published over 150 scientific articles, 14 books and book chapters, and has received several accolades, including the American Geriatrics Society New Investigator Award, the Schulich Clinician Scientist Award, the Premier of Ontario Excellence Research Award, and the CIHR New Investigator Award. In 2019, he was inducted as one of the Top 10 Hispanic Canadian for his contribution in Medicine and Science. He has been invited to give more than 100 international presentations as a guest speaker. He serves as associate editor for the Journal of Gerontology Medical Sciences, Geriatrics, and Journal of Alzheimer’s Disease, among others. He also serves as executive member and Vice-President of the Canadian Geriatrics Society.
