Search
Search
National award honours innovator Frank Prato’s excellence in medical physics
Dr. Frank Prato is a man of many firsts:
First in Canada to conduct magnetic resonance brain imaging. A pioneer in magnetic resonance cardiac imaging. Driving force behind the installation of Canada’s first PET/MR scanner. Founder of the Canadian Organization of Medical Physicists (COMP) while president of the Canadian College of Medical Physicists.
And while Dr. Prato admits to a competitive streak that constantly propels him to break new ground in medical physics, the renowned, prolific researcher is keen to note these innovations have been part of a larger team effort.
“My career has been filled with opportunities to work with and train some spectacular scientists who have made major contributions across Canada and around the world,” he says. “I’m proud of the whole group that has developed over the years and the support St. Joseph’s has provided.”
Chief Medical Physicist at St. Joseph’s Health Care London (St. Joseph’s), Dr. Prato has been awarded the 2024 COMP Gold Medal, the organization’s highest award for outstanding career achievement.
“Dr. Prato’s ground-breaking work in the field of medical physics has not only advanced the scientific community but also significantly impacted patient care in Canada and beyond,” says COMP President Boyd McCurdy, “His pursuit of innovation and excellence exemplifies the highest standards of our profession, and we celebrate his outstanding contributions to medical physics with admiration and gratitude.”

Dr. Prato is also Assistant Scientific Director and Imaging Program Leader at Lawson Health Research Institute (Lawson) and professor of medical imaging and medical biophysics at Western University.
“I have worked with Frank for 36 years now and have come to recognize him as one of the finest people I know,” says Dr. Ting-Yim Lee, Director of PET/CT Research at Lawson, medical physicist at St. Joseph’s Hospital, and one of the nominators of Dr. Prato for the award.
“Frank is unfailingly helpful and authentic, a great listener and a tenacious problem-solver. He demonstrates excellence and professionalism in medical physics locally, nationally and internationally.”
Dr. Lee cites Dr. Prato’s leadership in being “at the forefront of numerous international innovations in nuclear medicine and diagnostic radiology.”
Throughout his 48 years as a medical physicist, Dr. Prato has been inspired by the potential of technology’s reach into human health.
“I’ve always wanted to work in an area where we can do research, with a vision of what’s going to be important in patient health. I get excited about being on the leading edge of discovery that’s embedded in patient care.”
Critical advancements in nuclear medicine and diagnostic radiology, thanks to the work of Dr. Prato and his St. Joseph’s/Lawson team, have included:
- Introducing the first bone mineral density imaging procedure on a patient in Canada, a tool now essential for managing osteoporosis.
- Performing the first magnetic resonance brain imaging in Canada, setting a national standard.
- Pioneering magnetic resonance cardiac imaging techniques, enhancing the understanding of myocardial scarring and blood flow assessment.
- Introducing the first PET/CT and PET/MR scanners in Canada, revolutionizing molecular imaging and proving the economic value of advanced imaging technologies.
- Imaging the brains of premature infants, a world first.
- Developing Canada’s first self-sustaining cyclotron infrastructure.
- Conducting the world’s first MRI-compatible, high-resolution brain PET scan.
- Early diagnosis and treatment of dementia, mental illness and prostate cancer.
Dr. Prato’s leadership extends beyond his technical achievements. As the founder of COMP, an organization that now includes more than 800 professionals, he played a crucial role in establishing the organization, advocating for medical physicists' independent voice and professional growth.
His tenure as President and board member of the Canadian College of Physicists in Medicine (CCPM) was marked by significant advancements, including enhancing certification processes and establishing reciprocity with the American Board of Medical Physics. Dr. Prato also received the Valuable Service Award from CCPM in 2002 and was named a Fellow of COMP in 2013.
Earlier this spring, Dr. Prato received a Dean’s Award of Excellence for Research Faculty from Western University’s Schulich School of Medicine & Dentistry. He is also the sole Canadian to have won the d'Arsonval Award, an international honour from the Bioelectromagnetics Society.
A dedicated mentor, Dr. Prato has guided more than 60 Masters of Science students, PhD students and Post-Doctoral Fellows, many of whom have won awards and secured prominent positions in the field. His mentorship has been instrumental in the success of numerous scientists within the Imaging Program at Lawson, contributing to a legacy of innovation for years to come.
“At 78 years old,” he says, “I am pleased to say I have achieved things at St. Joseph’s that will far outlast me.”
National research collaboration leads to Health Canada approval of life-saving radioisotope production
A Canadian consortium, which includes Lawson Health Research Institute (Lawson), TRIUMF, BC Cancer and Centre for Probe Development and Commercialization, is the first in the world to receive regulatory approval to produce the world’s most commonly used medical isotope, technetium-99m (Tc-99m), using small particle accelerators known as cyclotrons.
Tc-99m is used in tens of millions of nuclear medicine procedures globally each year. These include cancer scans, cardiac tests, as well as several other diagnostic procedures. As the world moves away from uranium-based nuclear reactors, there has been growing concern in the medical community of a global shortage of these life-saving compounds. This development helps secure a domestic supply of Tc-99m for Canadian patients.
For over a decade, Dr. Michael Kovacs, Director, Lawson Cyclotron & PET Radiochemistry Facility, and Steven Foster, Business Manager, Lawson Imaging, have been working on research that has contributed significantly to this major development. They have demonstrated the successful production of Tc-99m on a standard hospital-based cyclotron at Lawson, confirming that this technology can be used by almost half of the world’s already installed cyclotrons. Clinical trials were conducted across Canada and locally at St. Joseph’s Health Care London.
“In 2011, we received federal funding to see if we could develop a technology to produce Tc-99m in hospital cyclotrons,” explains Dr. Kovacs. “Canada’s Chalk River nuclear reactor was one of the world’s largest suppliers, and it was set to close in 2016. Cyclotron facilities offer a greener, safer, more sustainable approach for producing critical medical isotopes. Our goal was to find an alternative to the traditional means of producing this isotope, and we have been successful.”
Nuclear medicine is a functional imaging technique, meaning that it images biological function. Medical isotopes are converted to radiopharmaceuticals which get injected into the patient during a procedure. According to the specific biological properties of the isotope, they move throughout the body, rendering a 3D map of where the isotope has gone. This gives researchers and medical professionals valuable information of how various physiological processes are performing.
“Canada is a global leader in nuclear imaging technology. With the help of our collaborators across the country, we have home-grown technology to produce commercial quantities of Tc-99m on common cyclotrons,” adds Mr. Foster. “This technology has been patented and licensed to ARTMS Inc., a spin-off from the consortium, and is now being commercialized and sold throughout the world.”
The process was approved by Health Canada in November, 2020, and is expected to be deployed in British Columbia by 2022.
Navigating the Road Ahead - Dementia: Reshaping Attitudes
Research and Clinical Care Panel
Featuring the latest in dementia research from a practical perspective
Moderated by Dr. Scott McKay, Family Physician
- Dr. Elizabeth Finger, Cognitive Neurologist
- Dr. Micheal Borrie, Geriatrician
- Dr. Lisa Van Bussel, Geriatric Psychiatrist
Morning Keynote
Sylvia Davidson
BScOT, MSc - Baycrest
Improving Quality of Life through Technology and Care
Afternoon Keynote
Rebecca Brown
MSW, RSW - Western University
Compassion Fatigue and the Impact on Carers
Designing for Dementia Panel
A discussion on the importance of 'designing for dementia' in both community and institutional settings
Moderated by Brad Lohman, The Manor Village Life Centres
- Natalie Rowe - Faculty, School of Design, Fanshawe College
- Ron Koudys - Principal, Ron Koudys Landscape Architects INC
- Heather Brinker - Occupational Therapist, VHA Home HealthCare
For more information, see the event poster or visit www.alzheimerlondon.ca.
New Alzheimer’s research aims to improve treatment and support for patients with agitation
Two new interventional studies have been brought to London, focused on improving quality of life for patients with Alzheimer’s disease and their caregivers. Both hope to improve upon standard approaches to treating agitation, a core symptom of Alzheimer’s.
Agitation is a significant source of stress for patients and caregivers. It is complex and difficult to treat. Often, families do not know about this particular symptom of Alzheimer’s and are not properly trained on how to manage care while dealing with agitation.
“These studies are designed to have a direct impact on patients, families and care providers, to improve quality of life and function in those suffering from agitation due to Alzheimer’s,” says Dr. Amer Burhan, Associate Scientist at Lawson Health Research Institute (Lawson) and Geriatric Neuropsychiatrist, St. Joseph’s Health Care London (St. Joseph’s).
Parkwood Institute, a part of St. Joseph’s, is one of multiple sites participating in these studies across Canada and the United States.
One study aims to identify patients early in their diagnosis, while they are living at home or in the community, and apply a comprehensive psychosocial approach, with or without medication, to help with the management of agitation. “We hope to identify participants and have them participating in our program before they experience a crisis due to agitation,” explains Dr. Burhan.
Psychosocial intervention is a way of helping patients and caregivers understand the reasons for agitation. Agitation can develop due to a wide range of causes. For example, patients may just be bored and need help to find something meaningful to occupy their time, they could be upset about something in their current environment, or may be suffering from physical discomfort or pain.
Interventions can include communicating with patients in a manner that creates calm, scheduling meaningful activities, and maintaining routine and rhythm in life. The research team will connect with families early after diagnosis to give them the tools and support they need.
Initially, participants will be treated using structured psychosocial intervention to help reduce and manage their agitation. After three weeks, they will be reassessed and if significant agitation continues to persist, the patient will be randomly selected to receive either a placebo, or medication known as S-Citalopram to treat agitation while they continue to receive psychosocial care.
Sylvia Wilson is the wife of one of the study participants. By enrolling in this trial, she feels she has gained a much better understanding of her husband’s disease, and is grateful for the support that study participants receive.
“My husband typically does not like going to visit doctors, but Dr. Burhan and his team are great,” says Wilson. “They understand agitation, and other symptoms of the disease very well, and I notice a difference in his mood with the treatment he receives through the study.”
Participants are still able to receive care from their primary physician and care teams, with the study providing an added layer of support.
Another study is focused on Alzheimer’s patients who are admitted to hospital or living in long-term care. The aim is to standardize the approach to care for agitation related to Alzheimer’s. After baseline assessment, participants will be randomized to receive the current treatment as per usual, or an integrated care pathway derived from evidence-informed treatment guidelines. These include washing out medications that have not helped, adding individualized behavioral and environmental support, and if medications are needed, use a specific set of medications and dosages based on best evidence.
“Better understanding agitation is a growing area of interest in geriatric research. The work being done locally is part of an international effort to create a paradigm shift in treating patients with Alzheimer’s disease and agitation,” explains Dr. Burhan.
Researchers are ready to offer these studies to patients and their families, hoping to make these treatment protocols an integral part of care for patients with agitation due to Alzheimer’s disease. Those interested in learning more about these studies can contact Dr. Burhan at @email or call 519-646-6100 x. 48170.
In the media: Study on 'agitation' in Alzheimer's patients seeks participants
New biomarker speeds identification of lung disease
LONDON, ON- A new diagnostic method could help identify one of the deadliest types of interstitial lung disease (ILD) sooner, allowing for faster treatment and improved patient outcomes.
Idiopathic pulmonary fibrosis (IPF) is one of the most serious and common types of ILD, occurring most often in patients 60 and older with an average survival time of three to five years. At any given time roughly 300 patients are being treated for IPF in London, Ontario. Globally, it is the number one reason for lung transplants.
A new study published in Respiratory Research has found that testing for a protein called cyclin-dependent kinase inhibitor protein (p16) in biopsy tissue may help more accurately identify IPF.
Dr. Marco Mura, Associate Scientist at Lawson and Respirologist at London Health Sciences Centre (LHSC), together with Dr. Matthew J. Cecchini, Pathologist at LHSC, led the study. Dr. Mura says the test could mean knowing years sooner if a lung transplant might be needed.
“We developed a method that is actually quite inexpensive to increase the diagnostic accuracy of the biopsy and help to avoid unclassifiable cases. The method has a prognostic value, so it helps predict survival of these patients at the time of biopsy,” says Dr. Mura, who is also an Associate Professor of Medicine at Western University.
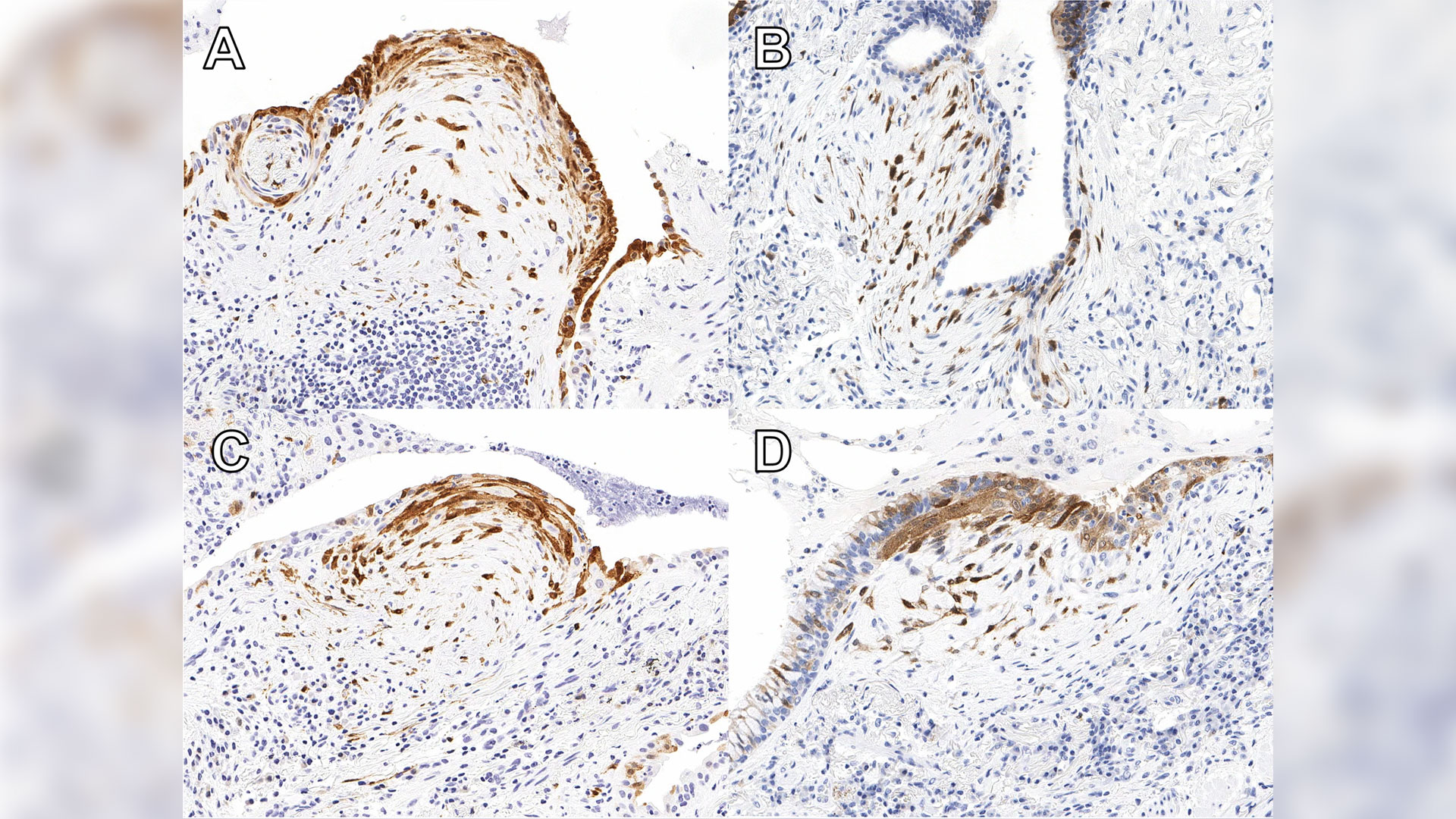
Patients with high expression of p16 were shown to experience worse outcomes than others with ILD, indicating that it is essential for these patients to start necessary treatment without delay. The protein is already widely used in ovarian cancer diagnosis. Now additional ongoing studies will help reinforce the value of the test for IPF diagnosis.
“We have no tests that we can apply to the (lung) biopsy other than the pathologist looking at it and saying ‘OK, this biopsy shows this pattern,’” Dr. Mura says. “There were absolutely zero additional biomarker tests to reinforce, validate or support the diagnosis. So, this will be the first time that we implement such test biomarkers in clinical practice.”
With this type of test that looks at the quantity of the biomarker, there is also the possibility of applying artificial intelligence to advance diagnosis in the future.
The research was supported by a 2018 Internal Research Fund grant from Lawson.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New clinical protocol after general surgery cuts opioid prescribing in half
In recent years deaths from opioid overdoses have become one of the most common injury-related deaths in North America. The continent also has the highest per capita rate of opioid prescription in the world.
Recognizing the role that opioid prescribing plays in the national opioid crisis, a team of researchers at Lawson Health Research Institute and Western University have developed a new clinical protocol called STOP Narcotics. A study demonstrating the efficacy of their protocol was presented at the American College of Surgeons Clinical Congress in Boston, Massachusetts on October 24.
The protocol includes a combination of patient and health care provider education and an emphasis on non-opioid pain control. The study found that they were able to reduce the overall amount of opioids being prescribed after general surgery by 50 per cent while still adequately treating a patient’s post-operative pain.
“By significantly reducing the amount of opioids prescribed, this decreases the exposure risk and potential for misuse of narcotic medication,” said Dr. Luke Hartford, a resident in general surgery at Western’s Schulich School of Medicine & Dentistry and first author on the study. “This also decreases excess medication available to be diverted to individuals for whom it was not intended.”
The study involved 416 patients at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London who underwent laparoscopic cholecystectomy or open hernia repair. They received medication for post-operative pain through the standardized protocol, specifically acetaminophen (Tylenol) and a non-steroidal anti-inflammatory drug (Naproxen) for the first 72 hours post-surgery.
The protocol instructs physicians to write a limited prescription of ten pills of opioids (Tramadol), with an expiry date of seven days after surgery, with instructions for the patient to fill this prescription only if adequate pain control was not otherwise achieved. There are also instructions on proper disposal of unused medication for the patient.
Dr. Ken Leslie, scientist at Lawson, associate professor in the Department of Surgery at Schulich Medicine & Dentistry, and Chair/Chief of the Division of General Surgery at London Health Sciences Centre led the implementation of the new protocol.
“We recognized that before STOP Narcotics, every surgeon had a different approach to pain control, and that most surgeons were prescribing more narcotics than are actually needed,” said Dr. Leslie. “When we looked at the data from this new protocol, we saw that the patient’s pain-control was just as good with this pathway, without a huge prescription for narcotics.”
The results showed that in the STOP narcotics group, compared to a control group, there was a 50 per cent reduction in the number of opioids being prescribed. They also demonstrated that only 45 per cent of patients actually filled their opioid prescription, compared to 95 per cent in the control group, and they were also able to increase appropriate disposal of excess opioid medication from 7 per cent in the control group to 23 per cent in the STOP Narcotics group. The levels of reported post-operative pain were the same in both groups.
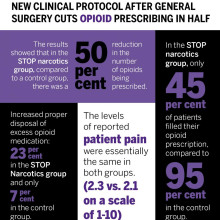
The group now hopes to expand the protocol for applications beyond general surgery.
“If we can decrease the opioid exposure risk in our patients, and decrease the amount of excess medication available for diversion, and spread this to other institutions and surgical procedures and specialties, this has the potential to significantly impact the opioid crisis,” said Dr. Patrick Murphy, a resident in general surgery at Schulich Medicine & Dentistry and co-author on the study.
The study, “The Standardization of Outpatient Procedure (STOP) Narcotics: A Prospective Noninferiority Study to Reduce Opioid Use in Outpatient General Surgical Procedures,” is published in the Journal of the American College of Surgeons.
| Dr. Ken Leslie | Dr. Luke Hartford | Dr. Patrick Murphy |
Image

|
Image

|
Image
|
New device could reduce COVID-19 infection risk and demand for invasive ventilators
LONDON, ON – Led by Lawson Health Research Institute, London Health Sciences Centre (LHSC), University Health Network (UHN) and General Dynamics Land Systems-Canada (GDLS-Canada), researchers have designed a non-invasive ventilation mask that could significantly reduce aerosolization – the production of airborne respiratory droplets that may contain viruses or bacteria – when treating patients with COVID-19. The new device aims to reduce infection risks associated with non-invasive ventilation and lessen the demand for invasive ventilators. It is currently being tested through a clinical trial with patients at LHSC.
“Since the beginning of this pandemic, there have been global concerns about a shortage of ventilators,” says Dr. Tarek Loubani, Lawson Associate Scientist and Emergency Department Physician at LHSC. “Non-invasive ventilators like CPAP (continuous positive airway pressure) and BiPAP (bi-level positive airway pressure) machines are associated with an increased risk of COVID-19 transmission and so many hospitals have moved directly to invasive ventilation.”
COVID-19 is primarily spread through inhalation of respiratory droplets and the most severely ill patients require a ventilator to help them breathe. Unlike invasive ventilators, which require intubation, non-invasive ventilators help patients breathe through a mask that provides positive pressure to keep the lungs open and functioning. While non-invasive ventilators may be effective for some COVID-19 patients, their use comes with a much higher risk of spreading infection through aerosolization of respiratory droplets.
The team’s non-invasive ventilation mask aims to eliminate this risk. The novel device is customized from a standard firefighter’s mask using 3D printing and can be attached to any CPAP or BiPAP machine. Unlike traditional masks, it creates two tight seals – one around the patient’s nose and mouth and another around the face. Patients breathe in and out of a filter that captures any viral particles before they are released to the air.
“There are countless CPAP and BiPAP machines idling around the world while all resources go towards invasive ventilation,” explains Dr. Azad Mashari, Anesthesiologist at UHN’s Peter Munk Cardiac Centre. “Our mask aims to put these machines back into the clinician’s toolkit. By eliminating air leaks, we can improve patient safety and significantly reduce the risk of contracting COVID-19 for health-care workers and other patients.”
Drs. Loubani, Mashari and Benjamin Thomson, Nephrologist at Mackenzie Health, were part of a clinical research team that worked with engineers from GDLS-Canada to develop the device within six days.
“GDLS-Canada responded quickly to the urgent need to support those on the COVID-19 healthcare frontlines during this global health emergency,” says Doug Wilson-Hodge, GDLS-Canada’s Manager of Communications, Community and Government Relations. “The innovative design was very much a collaborative effort between all parties to contribute solutions to the COVID-19 pandemic.”
The initial clinical trial will test the device with up to 50 patients at LHSC’s Victoria Hospital and University Hospital with plans to expand to UHN. In addition to patients with COVID-19, participants will include those with asthma, chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF).
The research team anticipates other hospitals in Ontario and across Canada will join the study to create a multi-centre clinical trial. The device will be used in emergency departments and has potential to be used in intensive care units, remote nursing stations and during pre-hospital transport. It has also been designed for easy production in resource-strained locations.
“This problem affects everyone and it’s critical that we all do what we can to help,” adds Dr. Loubani. “We hope it will help not only those in urban centres like Toronto and London, but people in remote communities around the world.”
The trial is being supported with funding from Glia, an organization internationally recognized for producing medical supplies that are easily accessible and can be manufactured in low-resource settings.
-30-
DOWNLOADABLE MEDIA
Images




Video



Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
London Health Sciences Centre has been at the forefront of medicine in Canada for 145 years and offers the broadest range of specialized clinical services in Ontario. Building on the traditions of its founding hospitals to provide compassionate care in an academic teaching setting, London Health Sciences Centre is home to Children’s Hospital, University Hospital, Victoria Hospital, the Kidney Care Centre, two family medical centres, and two research institutes – Children’s Health Research Institute and Lawson Health Research Institute. As a leader in medical discovery and health research, London Health Sciences Centre has a history of over 70 international and national firsts and attracts top clinicians and researchers from around the world. As a regional referral centre, London Health Sciences Centre cares for the most medically complex patients including critically injured adults and children in southwestern Ontario and beyond. The hospital’s nearly 15,000 staff, physicians, students and volunteers provide care for more than one million patient visits a year. For more information, visit www.lhsc.on.ca.
University Health Network consists of Toronto General, recently voted one of the Top 5 Hospitals in the World according to Newsweek Magazine, and Toronto Western Hospital, the Princess Margaret Cancer Centre, Toronto Rehabilitation Institute, and the Michener Institute of Education at UHN. The scope of research and complexity of cases at University Health Network has made it a national and international source of discovery, education and patient care. It has the largest hospital-based research program in Canada, with major research in cardiology, transplantation, neurosciences, oncology, surgical innovation, infectious diseases, genomic medicine and rehabilitation medicine. University Health Network is a research hospital affiliated with the University of Toronto. www.uhn.ca
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New form of expanded dialysis improves quality of life, study finds
LONDON, ON – In a published study, a hospital research team from Lawson Health Research Institute has found that expanded dialysis, a new method that removes a broader range of toxins from the body, can improve quality of life in chronic kidney disease patients who struggle with the side effects of traditional dialysis.
In a clinical trial led by Dr.Chris McIntyre, Nephrologist at London Health Sciences Centre (LHSC) and Scientist at Lawson, dialysis patients at LHSC were administered expanded dialysis through a new dialyzer made by Baxter International Inc.
The dialyzer, called THERANOVA, has precisely-made pores that allow larger sized toxic chemicals to be filtered from the blood while retaining essential molecules such as albumin. “The chemicals that can now be filtered out can cause inflammation, malnutrition and the buildup of waste,” explains Dr. McIntyre. “With traditional dialysis treatments, we haven’t been as successful at removing those chemicals and some patients experienced significant side effects.”
These larger molecules that the THERANOVA dialyzer is able to filter out are believed to be associated with inflammation, cardiovascular disease and chronic symptoms like fatigue. Study participant Robert Wahby has chronic kidney disease and has been on dialysis for about five years. He is no stranger to these symptoms. “I was hoping that trying this new dialyzer would help get rid of some of my symptoms. My appetite was down, I was a little weak and I was hoping I would sleep better.”
As part of the clinical trial, Wahby started to immediately notice a positive difference when administered dialysis through the THERANOVA dialyzer. “I felt better, I was eating more and I had a better night’s sleep.”
His wife, Marlene Wahby, also noticed promising changes. “His sleeping patterns have gotten better and he feels better when he comes home. When he was on the traditional dialysis, he got very jumpy and didn’t feel well at all after treatments.”
This study was conducted for three months with 28 patients. Along with receiving the expanded dialysis treatment, the research participants were monitored through the London Evaluation of Illness (LEVIL) app, developed by Dr. McIntyre with the help of patient input.
“One of our big research challenges is measuring the quality of life on dialysis,” says Dr. McIntyre. “Conventional measures take time and may not be as accurate, so by asking questions through the app every day we were able to get a true idea of how patients were feeling.”
By using the LEVIL app, the team was able to determine that patients that had a poorer quality of life at the start of the study significantly improved in the areas of general wellbeing, energy and sleep after approximately four to eight weeks of expanded dialysis.
Now that the first phase of this study has been completed and published in Kidney Medicine, the next phase will include 60 dialysis patients for up to six months of treatments using the THERANOVA dialyzer. This second phase will be a multicentered clinical study led by Lawson, University of Toronto and Humber River Hospital.
-30-
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New imaging solution could help improve survival for patients with recurring prostate cancer
London, ON - A multicentre study led by London Health Sciences Centre Research Institute (LHSCRI), Lawson Research Institute of St. Joseph’s Health Care London (Lawson), and University Health Network (UHN) has found a novel imaging solution, called prostate-specific membrane antigen (PSMA) positron emission tomography (PET) scanning, can more effectively detect the recurrence of prostate cancer compared to standard imaging methods, and is associated with improved survival outcomes. The study, carried out over seven years, is published in The Journal of Nuclear Medicine.
During a PSMA PET scan, a radioactive molecule designed to target a protein in prostate cancer cells is injected into the bloodstream of a patient prior to the scan. The study uncovered that the molecule is effective in binding to prostate cancer cells, helping to detect recurring prostate cancer earlier and more effectively than standard imaging methods.
“This new technique gives physicians the information needed to determine the best treatment,” says Dr. Glenn Bauman, Scientist at LHSCRI and Radiation Oncologist at London Health Sciences Centre (LHSC). “When a blood test shows cancer has returned but standard imaging can’t find it, physicians may need to use less precise therapies like whole-body drug therapy. With this new imaging technique, we can locate the cancer and target it directly.”
The research team found that the overall detection rate was 70 per cent, much higher than the historical rates of detection of 10-20 per cent with conventional bone scan and CT scans. About half of all patients had their management of the disease changed based on the results of the scans. Almost 90 per cent of men with cancer detected by PSMA PET had a change in management of their recurring prostate cancer following the scan. They also found that patients who had their treatments modified based on results from the PET scan had a better overall survival rate than those who received standard imaging.
“We’re encouraged by how this imaging approach is already changing cancer care,” says Dr. Ur Metser, Division Head of Molecular Imaging at UHN and Clinician Scientist at UHN’s Princess Margaret Cancer Centre. “Our study showed that PET scans using this technique led to more personalized treatment decisions and those changes are linked to longer survival. That’s a meaningful step forward for patients and their care teams.”
Dr. Bauman and his colleagues from Lawson and LHSCRI were the first in Canada to image a patient using PSMA PET imaging in 2016. Since then, this study has enrolled thousands of men across six hospitals in Ontario through funding from Ontario Health - Cancer Care Ontario. Based on promising results from this and other research, PSMA PET scans are now funded as a standard of care test for men with advanced prostate cancer.
For more information, please contact: Deb Flaherty, Consultant, Communications & Public Affairs, St. Joseph's Health Care London.
519-646-6100 ext. 47560
ABOUT LAWSON RESEARCH INSTITUTE
Lawson Research Institute, the health innovation arm of St. Joseph's Health Care London, is committed to making and sharing discoveries that improve lives locally and internationally. Every day, Lawson researchers work to transform imagination to innovation to patient impact. Lawson leads health-care research. Find us at LawsonResearch.ca and @stjosephslondon on social media.
ABOUT LONDON HEALTH SCIENCES CENTRE RESEARCH INSTITUTE
At London Health Sciences Centre Research Institute (LHSCRI), our teams pioneer discoveries that transform the health of adult and paediatric patients around the world. As the research institute of London Health Sciences Centre (LHSC), we conduct research where patient care is delivered, working alongside patients, families, health-care providers and academic partners like Western University. We are leaders in advancing the understanding, diagnosis, treatment and management of diseases and health conditions through a diverse research program that ranges from laboratory-based science to clinical trials. Our research has a global impact as we build on LHSC’s 150-year legacy of health innovation and drive forward medical breakthroughs that
make a difference in the lives of patients and their families. Find us online at WWW.LHSCRI.CA and on social media @LHSCRI.
New imaging tool for diagnosing heart disease
An international team led by scientists from Lawson Health Research Institute and Cedars-Sinai Medical Center are the first to show that Magnetic Resonance Imaging (MRI) can be used to measure how the heart uses oxygen for both healthy patients and those with heart disease.
Reduced blood flow to the heart muscle is the leading cause of death in the Western world. Currently, the diagnostic tests available to measure blood flow to the heart require injection of radioactive chemicals or contrast agents that change the MRI signal and detect the presence of disease. There are small but finite associated risks and it is not recommended for a variety of patients including those with poor kidney function.
Standard methods
More than 500,000 of these tests are performed each year in Canada. A patient suspected of coronary heart disease for example may have reasonably normal blood flow at rest but as soon as they exercise they have pain or feel out of breath. They need more oxygen delivered to the heart tissue but due to vessels being compromised that doesn’t happen.
The standard technique is usually done in two days with the goal of seeing if the heart can increase blood flow when more oxygen is needed. The first test studies the patient at rest to see what the blood flow is like in the heart. This is a nuclear medicine imaging test that requires radioactive material to be injected and takes about an hour or more to complete.
They next day, they come for the same test but with the introduction of a stressor. That can be physical exercise but more often they are given an injection of a chemical drug which stimulates the heart and increases blood flow. This is in addition to a second injection of the radioactive material. The heart is imaged to see the level of oxygen getting to different parts of the heart and whether there are obstructions or reduction in size of the surrounding arteries.
A new stress test
“We wanted a non-invasive way to image the heart and replace the stress stimulus, and drastically reduce the amount of time needed for testing,” says Dr. Frank Prato, Lawson Assistant Director for Imaging. “This new method, cardiac functional MRI (cfMRI), does not require needles or chemicals being injected into the body. It eliminates the existing risks and can be used on all patients."
The team included researchers from Lawson; Cedars-Sinai Medical Center and University of California; King’s College in the United Kingdom; University Health Network and the University of Toronto; Siemens Healthineers; and, University of Edinburgh in the United Kingdom.
“Our discovery shows that we can use MRI to study heart muscle activity,” explains Dr. Prato. “We’ve been successful in using a pre-clinical model and now we are preparing to show this can be used to accurately detect heart disease in patients.”
To replace the stress test, this new technique uses repeat exposure to carbon dioxide to test how well the heart’s blood vessels are working to deliver oxygen to the muscle. A breathing machine changes the concentration of carbon dioxide in the blood. Levels are brought up for three minutes and then back down to normal four times. These changes should result in a change in blood flow to the heart, but does not happen when disease is present.
The cfMRI method reliably detects whether these changes are present and is comparable to the information gathered from the current two-day technique – in much less time and without injections. Dr. Prato notes that “we don’t want to stress the heart. We want to see whether there is capacity in the heart to increase blood flow if the heart needs to work harder.”
A brilliant discovery
Other researchers have explored oxygenation-sensitive MRI but initial results contained a high level of ‘noise’ with blurry images. Project leader and partner Dr. Rohan Dharmakumar, Associate Director of the Biomedical Imaging Research Institute at Cedars-Sinai Medical Center, believed that the noise was actually variation in the heart’s processing of oxygen. He engineered a way to average this variation and through testing at Lawson the team discovered that the noise is actually a new way to study how the heart works.
“We’ve opened the door to a new era and totally novel way of doing cardiac stress testing to identify patients with ischemic heart disease” says Dr. Dharmakumar. “This approach overcomes the limitations of all the current diagnostics – there would no longer be a need for injections or physical stress testing like running on treadmills.”
Through investigating this technique, they learned that the blurry images were showing normal physiological variability. People often think of heart rate as being stable, but in fact a heart that is unable to keep up with stressors indicates that disease is developing. In a healthy heart, the oxygen distribution to the tissue needs to vary.
“It’s a very exciting time. We had to bring all the technologies together to be able to image these kinds of changes in blood flow moment to moment,” says Dr. Prato.
He adds that “using MRI will not only be safer than present methods, but also provide more detailed information and much earlier on in the disease process.” Following initial testing through clinical trials, he sees this being used with patients clinically within a few years.
Moving forward
In addition to studying coronary artery disease, the method could be used in other cases where heart blood flow is affected such as the effects of a heart attack or damages to the heart during cancer treatment. Due to its minimal risk, this new tool could be safely used with the same patient multiple times to better select the right treatment and find out early on if it is working. Dr. Prato notes that “with this new window into how the heart works, we have a lot to explore when it comes to the role of oxygen in health and disease.”
The next steps of the research include a proof of principle study in London, Ontario with 20 patients. Following standard tests using the conventional technique at other sites, the participants will then come in for the experimental test to show that it produces the same result. The research would then move into a multi-centre clinical trial internationally.
The study “Accurate needle-free assessment of myocardial oxygenation for ischemic heart disease in canines using Magnetic Resonance Imaging” is published in Science Translational Medicine.
New national strategy to tackle dementia
Researchers in London, Ontario have been awarded $1.345 million over five years through the second phase of the Canadian Consortium on Neurodegeneration in Aging (CCNA), announced today as part of Canada’s first national dementia strategy. CCNA is a collaborative research program tackling the challenge of dementia and other neurodegenerative illnesses.
A Dementia Strategy for Canada: Together We Aspire focuses on preventing dementia, advancing therapies and finding a cure, as well as improving quality of life for people living with dementia and caregivers.
Clinician researchers from across the country working together
Dr. Manuel Montero-Odasso, Scientist at Lawson Health Research Institute, is world renowned for his findings on the relationship between cognition and mobility in the elderly, and gait as a predictor of frailty and dementia. He leads the Mobility, Exercise and Cognition (MEC) Team in London, comprised of top researchers in the areas of mobility, exercise and brain health.
“Evidence from other countries with dementia strategies shows that coordinated, targeted efforts at the national level improves results for all aspects of dementia care and also for research,” says Dr. Montero-Odasso, also a geriatrician and Director of the Gait and Brain Lab at Parkwood Institute, a part of St. Joseph’s Health Care London.
CCNA was purpose-built to synergize dementia research within the Canadian context. Phase I saw the creation of infrastructure fostering collaboration amongst Canadian researchers, and there are now 20 teams built around important research topics.
“This kind of effective national collaboration by scientists and clinicians from many disciplines gives the CCNA a cutting edge in research, prevention, treatment and management of all forms of dementia,” explains Dr. Montero-ODasso. “We created a national network of researchers form west to east coast with a high level of expertise to deliver lifestyle interventions to improve cognition and slow down progression to dementia. I feel privileged working with such excellent investigators and leading this important endeavour locally.”
Preventing dementia through lifestyle changes
The MEC team has several projects in the works, but the majority of the new funding is to complete the SYNERGIC Trial, SYNchronizing Exercises and Remedies on Gait and Cognition.
This first-in-the-world clinical study is testing a triple intervention aimed at treating Mild Cognitive Impairment (MCI) and delaying the onset of dementia. The SYNERGIC Trial incorporates physical exercises and cognitive training, along with vitamin D supplementation to determine the best treatment for improving mobility and cognition.
“We are looking at how interventions will work together and targeting cognitive decline at its earliest stage – individuals with MIC,” explains Dr. Montero-Odasso. “Both physical and cognitive exercises have shown promising effects for maintaining cognition, while vitamin D deficiency is associated with cognitive decline.”
A professor at Western University’s Schulich Medicine & Dentistry, Dr. Montero-Odasso partners with researchers from across the city including Dr. Rob Bartha, imaging scientist at Schulich Medicine & Dentistry and Robarts Research Institute at Western University, and Dr. Kevin Schoemaker who leads the Laboratory for Brain and Heart Health.
Study participants in the SYNERGIC Trial are asked to complete an individualized and progressive routine of exercises and cognitive training three times a week for six months, with one final assessment at 12 months. The main site for the study is Parkwood Institute with the physical exercises taking place at the Labatt Health Sciences Building on the Western campus.
To date, 138 research patients has been recruited across multiple sites in Canada.
One participant’s experience
One day, Peter Saracino saw an advertisement about a research study. They were looking for participants who were a minimum age of 60 and had minor cognitive impairment. He felt he fit the bill and he was interested in this kind of research.
“I have family members who suffered from forms of dementia and Parkinson’s Disease. I really understand how hard it hits and I liked that this study was about prevention,” explains Peter.
Going into it, Peter thought he was in pretty good shape. He has two dogs and walks them regularly. “But by going to the gym and doing the exercises and faster-paced walking, I realized that I wasn’t in as good shape as I thought. My diet was under control but I was still taking blood pressure medication. I didn’t have much energy.”
After 10 weeks in the study, he feels better than he has for over a decade. “I can garden for longer. I took two notches off my belt. I no longer take my blood pressure medication. I actually feel younger.”
He remembered that last year he slipped and fell four times, which was very unusual for him. Part of his cognitive impairment is that he had trouble with balance, and that has improved for him as well.
Peter feels that “this is exactly the kind of research that the government should be investing in – an ounce of prevention is worth a pound of cure. This kind of research leads to keeping people independent and healthier as they get older. People are happier. They feel like doing more. There is no downside to improving someone’s health through lifestyle changes, and in fact it is cost effective and helps ease the burden on the health care system.”
Looking forward
“Our preliminary analysis from SYNERGIC is giving us a strong indication that a multimodal approach, combining physical exercise, cognitive training and supplementation, has a synergistic effect. It seems the whole is greater than the sum of its parts,” says Dr. Montero-Odasso.
A major goal for the work of the MEC team in London is to translate their research findings into clinical guidelines that can be used at the front line of care. “Practitioners understand the overall importance of exercise and cognitive vitality, but we are missing more specific guidelines on what kind and how much will work for different patients. Basically, what is an effective lifestyle prescription.”

Dr. Montero-Odasso adds that “as our population ages, a comprehensive strategy is vital to ensure the growing number of those living with dementia receive the care and support they deserve. Over half a million Canadians are currently living with dementia. By 2031, this number is expected to nearly double.” More than one third of dementia cases might be preventable.
CCNA Phase II
In CCNA’s Phase II, researchers are working on analyzing the overall health of every patient in a large clinical cohort study, COMPASS-ND. This information will be used to enhance understanding of how changes in the brain affect dementia severity and ways to reduce and prevent this through lifestyle changes. Lawson is the leading recruitment site for COMPASS-ND and the London team will be instrumental in the larger lifestyle interventions moving forward.
CCNA is funded by the Government of Canada, Canadian Institutes of Health Research (CIHR) and other funding partners. CIHR is providing $31.6 million, and partners—including provincial agencies and non-profit organizations—are providing an additional $14.4 million for a total investment of $46 million over five years. The research on dementia prevention, diagnosis, treatment and care as part of Phase II of the CCNA will support the national strategy.
Related stories
New research on reducing harm for people who use methamphetamine
At a virtual event, a research team led by Lawson Health Research Institute announced details of the Methamphetamine Harm Reduction Project that will study the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose.
“Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk.
“We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
New research on reducing harm for people who use methamphetamine in hospital
LONDON, ON – At a virtual event today, a research team from Lawson Health Research Institute is announcing details of the Methamphetamine Harm Reduction Project that will test the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose. “Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk. “We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New research showcased at third annual Parkwood Institute Research Spring Update Half Day
More than 100 researchers, staff and trainees attended the third annual Parkwood Institute Research (PIR) Spring Update Half Day on April 27, 2018 to share their innovative research and learn about work from across PIR through interactive workshops and poster presentations.
A program of Lawson Health Research Institute and located at St. Joseph’s Health Care London’s Parkwood Institute, PIR represents three major research programs: cognitive vitality and brain health, mobility and activity, and mental health. The event allowed guests to hear about new studies and recent research developments from across these three themes.
“Parkwood Institute Research covers different research areas but what we want to emphasize with this event is the overlap and collaboration between our programs. Having an inter-disciplinary approach that encourages partnerships ultimately helps us to incorporate new knowledge into patient care at Parkwood Institute,” says Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery, and Assistant Director, Lawson.
Five interactive workshops were held on a variety of different topics, such as clinical trials, systematic reviews, innovation in health care, practice-based research methods and evaluating SMART technology. The workshops were led by some of Parkwood Institute’s research leaders, including Drs. Cheryl Forchuk, Robert Teasell, Michael Borrie, Dalton Wolfe, and Arlene MacDougall.
Attendees also had the opportunity to visit poster presentations on recent PIR projects.

Ashrafunissa Janmohammad (above), Lawson research coordinator at Parkwood Institute’s Chronic Wound Management Clinic, was one of the poster presenters at the event. She presented on a study led by Lawson associate scientist Dr. David Keast, which assessed whether chitosan gelling fibre dressing could be effective in controlling bleeding after minor wound surgery. Chitosan is derived from chitin, the structural component of the cell walls of fungi and the shells of arthropods such as crabs, lobsters, shrimps and insects.

Juweiriya Ahmed (above), a MSc candidate at Lawson and Western University’s Schulich School of Medicine & Dentistry, was another presenter. Her poster outlined a study investigating the interaction between neuroanatomical and genetic risk factors that may contribute to the development of psychotic symptoms (delusions and hallucinations) in patients with Alzheimer’s disease. Supervised by Lawson scientist Dr. Elizabeth Finger, the study could help inform the development of therapeutic targets and treatment plans.
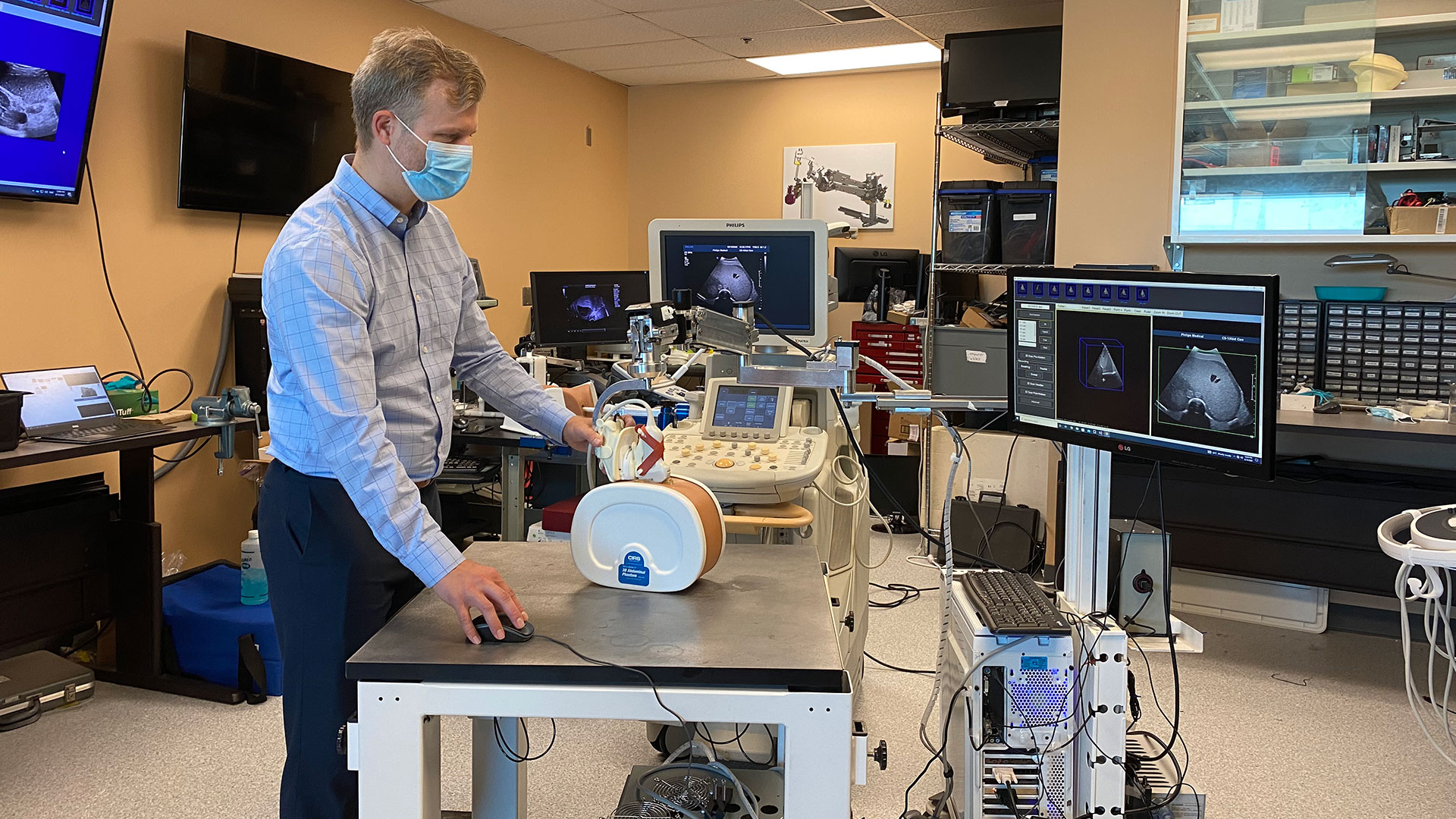
New robotic 3D ultrasound may improve accuracy of liver cancer ablation therapy
LONDON, ON – A new system that turns ultrasounds into a 3D image could make treatment of liver cancer using thermal ablation more accurate, a new simulated study from Lawson Health Research Institute and Western University has found.
Liver cancer is the fourth leading cause of cancer death globally. While surgery is one treatment option, thermal ablation, using heat to destroy the cancerous tumour, can have fewer complications and a shorter recovery time. It can also be used for patients who are not surgical candidates.
Thermal ablation requires precise needle placement to treat the cancer without damaging the vital organs and blood vessels around it.
“It's very important that we get the needle right in the centre of the tumour,” says Dr. Derek Cool, Associate Scientist at Lawson, Assistant Professor at Western University’s Schulich School of Medicine & Dentistry and Interventional Radiologist at London Health Sciences Centre (LHSC). “If the treatment area doesn't fully cover the tumour, patients are left with a small amount of residual cancer, risking recurrence and the need for additional treatment.”
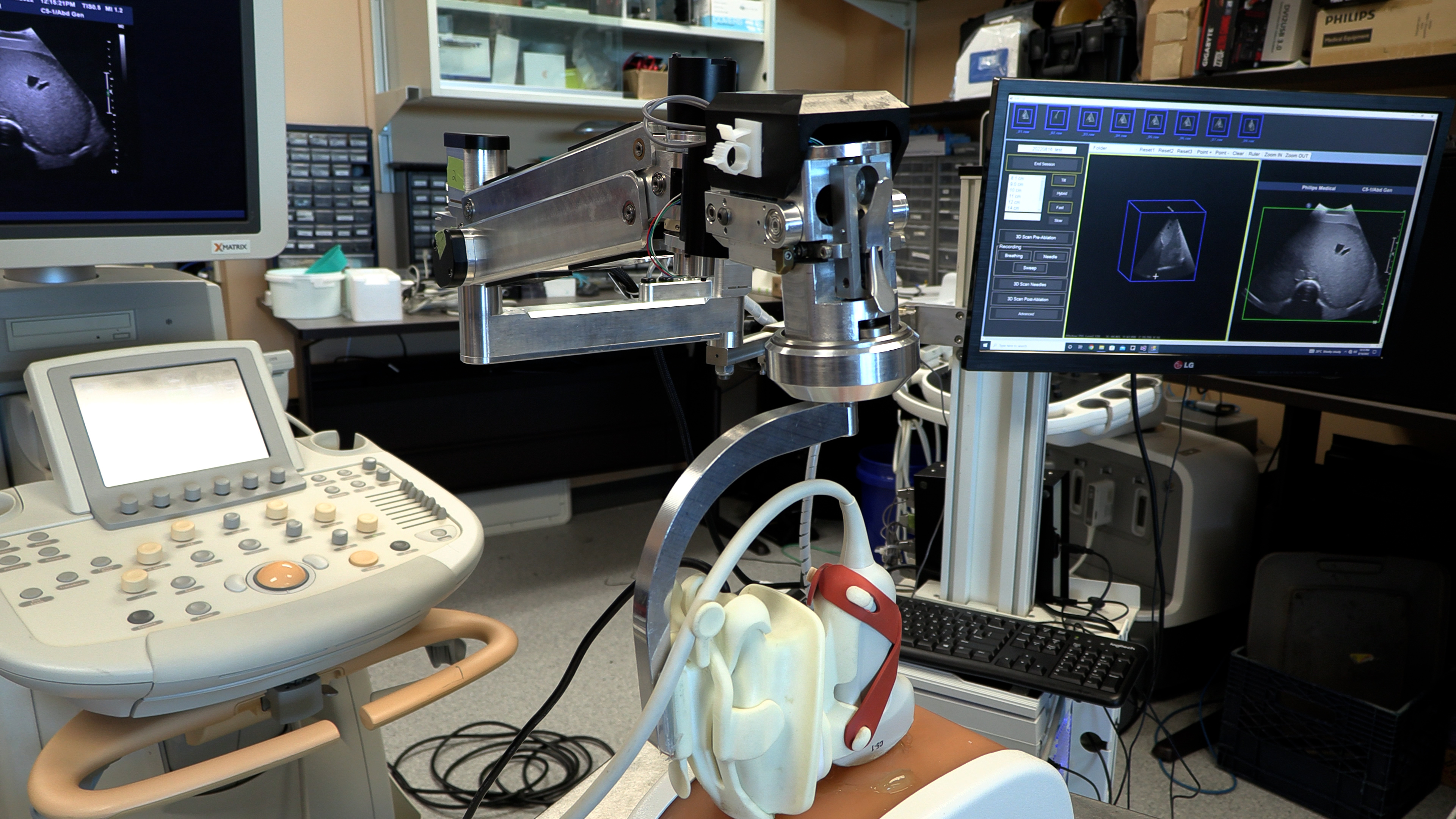
Ultrasound or CT (computerized tomography) imaging is normally used to guide needle placement, but both are limited. Ultrasound is widely available and can be done in real-time, but only delivers a 2D image. While a CT scan provides a 3D image, it isn’t in real-time and can be a lengthy process.
“We developed a new 3D ultrasound method that shows promise in analyzing whether the complete liver tumour will be ablated by the procedure,” explains Dr. Aaron Fenster, a Professor at Schulich and Scientist at Robarts Research Institute. “And we're now using the same system to guide the needle directly into the centre of the tumor.”
To create the 3D ultrasound images, a robotic cradle moves a standard ultrasound probe, collecting images and stacking them like puzzle pieces.
The simulated study, published in IEEE Transactions on Medical Imaging, used data from 14 patient cases at LHSC to analyze accuracy of the technology. It found that while 64.3 per cent of cases showed complete tumour coverage with standard imaging methods, the new system could result in complete coverage for 92.9 per cent of cases (13 of 14 cases). The researchers found that the remaining case could benefit from increasing the ablation time or intensity.
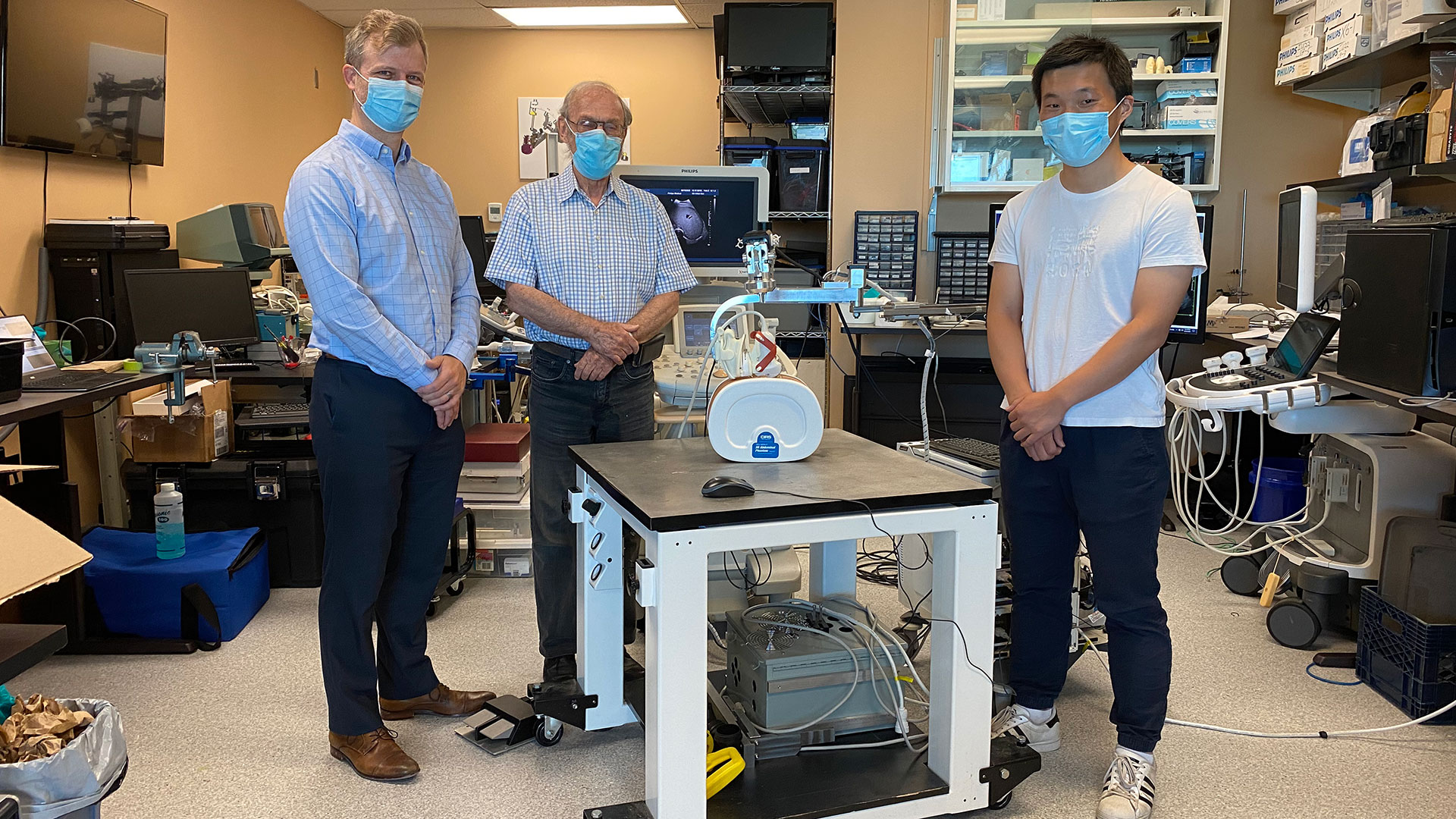
“Our next step is to move from simulation studies to a clinical trial,” says Dr. Cool.
If proven effective, the robotic ultrasound system’s portability could potentially allow for more widespread use of 3D ultrasound imaging, including in smaller health care centres. By eliminating the need for CT scans, it could also help to reduce imaging wait times.
“If a clinical trial shows the approach is more accurate and more precise than conventional techniques, there would be a direct impact on patient care,” says Dr. Fenster. “We hope to explore commercialization to license the technology and distribute it worldwide.”

Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study aims to improve mental health treatments for stroke patients
LONDON, ON- A team at Lawson Health Research Institute are looking to improve mental health treatments and resources for patients who have experienced a stroke. The team will recruit 100 stroke patients to assess whether the completion of a guided therapy program can improve mental health and quality of life.
Strokes affect approximately 400,000 Canadians each year and can be debilitating. They can negatively affect a person’s cognition and mobility, and severely impact mental health and wellbeing.
“More than sixty per cent of patients experience depression after stroke,” says Dr. Robert Teasell, Lawson Scientist and Physiatrist at St. Joseph’s Health Care London’s Parkwood Institute. “Having a stroke itself makes people more vulnerable and makes people feel their lives have changed negatively.”
During stroke rehabilitation, patients are typically offered mental health treatments, but the research team say it is post rehabilitation that stroke patients tend to experience worsening depression.
“Publicly funded allied health care services are available at inpatient and outpatient care; however, psychology is often limited across the rehabilitation continuum from acute to community care,” says Dr. Swati Mehta, Lawson Scientist. “We are looking at how we can provide a program that is cost effective to help those who have these barriers to access mental health services.”
The study will examine the use of cognitive behavioral therapy (CBT), which is an evidence based psychological intervention that aims to provide people with increased coping ability and self-efficacy. Participants will complete a 10-week guided program with specific targeted lessons, tailored to the needs of those post stroke, delivered virtually through a trained clinician. They will then complete a questionnaire to see if there have been any improvements to self-efficacy and emotional wellbeing.
“We have found this form of therapy (CBT) has been very effective and feasible for spinal cord injury patients with mild traumatic brain injury and we want to see how a modified version could potentially help those with stroke and depression,” says Randy Upper, Clinical Research Associate at Lawson.
If CBT is proven effective through this study, Dr. Mehta hopes it will encourage similar programming that would be available to stroke patients after rehab.
“We are hoping we can connect with community organizations and work with them to implement this program in a service delivery model that would be easily accessible for stroke patients living in the community.”
Recruitment for this study is currently underway, those interested in taking part can email Dr. Swati Mehta at: @email
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study aims to improve treatment for rheumatoid arthritis
A research team led by Lawson scientist Dr. Mamadou Diop has been awarded a Lawson Internal Research Fund to investigate whether a previously developed optical technique that can detect arthritis within one week of onset could also be used to provide early assessment of treatment response for rheumatoid arthritis (RA).
RA is a disease that causes chronic inflammation of the joints, which results in pain, reduced quality of life and loss of productivity. There is no cure for RA but a new category of drugs – biologic agents that can reduce pain and slow down or even halt disease progression – has revolutionized treatment.
However, these new drugs are expensive and only work in 30 per cent of patients, which means many RA sufferers are treated with no benefit for up to six months – the time it takes for current monitoring methods to reliably determine whether a treatment is working or not. “This is a direct consequence of the lack of sensitivity of current monitoring methods,” says Dr. Diop, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
Since their recently developed optical technique has a high sensitivity to arthritis, Dr. Diop and his team believes it could also be used as a safe and convenient method of assessing treatment efficacy in RA patients. Additionally, there are striking similarities between RA and cancer, and it has been shown that optical techniques can predict cancer in as early as one day after therapy starts.
At St. Joseph’s Health Care London, they will test this theory in a rat model of RA and compare the results of the optical technique to histology and CT imaging, other established methods of determining whether a treatment is effective.
“If successful, this project will generate a safe, low-cost technique that can detect treatment response in RA within days of starting treatment. This would reduce the risk of further joint damage experienced by many patients for whom the drugs are ineffective,” says Dr. Diop. “We hope this will enable early redirection of patients with non-responding RA to alternative treatments, such as a combination of multiple drugs and more frequent monitoring.”
Dr. Diop adds, “The Lawson IRF grant will enable us to test the validity of our hypothesis and subsequently generate valuable preliminary results to support grant proposals for larger external funding.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
New study aims to reduce recurrence of strokes by determining cause of Post-Stroke Atrial Fibrillation (PSAF)
The most frequent cause of stroke is Atrial fibrillation (AF), a cardiac arrhythmia consisting of irregular heartbeats. These strokes are the most devastating ones. Recent observations in stroke patients suggest that stroke can also cause AF. This Post-Stroke Atrial Fibrillation (PSAF), in turn, can produce more strokes.
Victoria Thorburn, a Master’s student at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry in the department of Anatomy and Cell Biology, has been awarded with a Lawson Internal Research Fund (IRF) Studentship to develop the first rodent model of PSAF. The goal of the study is to gain more understanding of the relationship between stroke and PSAF.
The cause of PSAF is currently unknown but it is believed that strokes occurring in the insular cortex, a brain region responsible for monitoring heart rhythm, may trigger PSAF. When this brain region is damaged by stroke, the heart is left without regulation, resulting in chaotic heart rhythms. Previous studies have not been able to confidently diagnose PSAF, since approximately one third of AF cases are silent or asymptomatic.
“Without continuous monitoring of heart rhythm prior to stroke, it is difficult to determine if PSAF is in fact a newly developed arrhythmia occurring after stroke or whether it was actually a silent form of AF that already existed before stroke,” Thorburn says.
Thorburn will experimentally induce stroke in the rat insular cortex to determine whether PSAF or other types of irregular heartbeats occur as a result. The project will be supervised by Dr. Luciano Sposato, Lawson scientist, physician at London Health Sciences Centre and associate professor in the Department of Clinical Neurological Sciences at Schulich, and Dr. Shawn Whitehead, assistant professor at Schulich. They will monitor heartbeat before and after insular stroke then assess potential biological factors or structural changes in the brain or heart that may be associated with PSAF. Animals that developed PSAF will be compared to those without the condition.
Since the proposed cause of PSAF, the involvement of insular cortex damage, differs greatly from the traditional cause of AF, which is often a structural abnormality in the heart, there could also be a difference in treatment. The hope is that the knowledge of PSAF formation gained from the first rodent model will lead to the development of prevention and therapeutic strategies, minimizing the number of stroke patients affected by PSAF and ultimately reducing the recurrence of stroke.
“I wanted to become involved with research that was currently relevant and had the translational potential to improve public health. With the current aging population, the number of individuals directly affected by stroke and AF will continue to rise,” says Thorburn. “Thanks to funding opportunities like Lawson’s IRF, students like myself are able to train alongside accomplished researchers and participate in research that uniquely integrates both basic science and clinical perspectives.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
New study aims to understand team-based care for chronic disease management
Chronic diseases, such as chronic obstructive pulmonary disease (COPD), are complex and require thorough care to help manage the condition. Patients often need support from an integrated team of health care professionals who work in different settings.
Dr. Shannon Sibbald, associate scientist at Lawson Health Research Institute, is leading a study to better understand integrated health care teams for chronic disease management and factors that help successful implementation.
Integrated team-based models of care include multiple health care providers working together to support patients with complex needs, such as those with chronic disease. There are many benefits to integrated team-based models of care. Patient outcomes are improved, health care providers feel more supported in their work and services are less likely to be duplicated.
Dr. Sibbald’s research focuses on chronic obstructive pulmonary disease (COPD), a devastating chronic disease affecting normal lung function in over 1.5 million Canadians. COPD is one example of a chronic disease where patients can benefit from team-based care. COPD is often underdiagnosed, and patients with COPD and other chronic diseases may not be receiving the ideal care for their condition.
While integrated team-based care is important, there are currently few studies to guide implementation. In this study, Dr. Sibbald’s research team will engage health care providers and patients to gain a rich understanding of successful integrated approaches to chronic disease management, including how team-based models of care are implemented. The team will also work to better understand how patients with chronic diseases view such models, and what their hopes and expectations are for their care.
“We want to explore innovative and successful approaches to implementing team-based models of care,” explains Dr. Sibbald. “We’re looking to learn how these methods can support practice, improve patient outcomes and spread innovation.”
The team will look at high performing integrated care teams that support current best practices at a family health team in London, Ontario.
When models are applied to practice, context is an important part to consider. For chronic diseases, context is often broad and elaborate. They hope to gain insight into what works well and what does not in dynamic contexts, and gain a better understanding of implementation facilitators and barriers.
The ultimate goal is to build knowledge that will support implementation and sustainability of high-performing integrated health teams across our health system.
“While motivation and momentum to use integrated teams is high, there is little guidance on how to do this well,” says Dr. Sibbald. “This research will provide insight into what works and what does not, reducing our gap in knowledge.”
Dr. Sibbald received a Lawson Internal Research Fund (IRF) grant to conduct this pilot study. Once complete, Dr. Sibbald’s team hopes to expand the study to look at integrated care models at other sites across the province.
"The IRF grant enables our team to validate our methods of evaluating the implementation of interprofessional team-based care in complex settings," adds Dr. Sibbald. "By examining the impact team-based care for patients with COPD, we hope to demonstrate the relevance of our findings, to support grant proposals."
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
