Search
Search
New urinary microbiome study could be first step in providing personalized care to patients with ureteral stents
For patients with kidney stones, ureteral stents (hollow devices placed in the ureter – the tube between the kidney and bladder) can be used temporarily to relieve urinary obstruction. Despite the use of antibiotics, ureteral stents often become encrusted with minerals and coated with bacteria. This can lead to complications like infection and the need for replacement surgery.
Published today in Cell Reports Medicine, researchers at Lawson Health Research Institute and Western University conducted a novel microbiome study to examine bacteria associated with ureteral stents. They found that nearly all the stents, whether visibly coated or not, had unique bacterial profiles that were most associated with a patient’s medical condition rather than antibiotic use. For patients with ureteral stents, they may benefit from a personalized approach to care and antibiotic treatment.

The study included 241 patients from St. Joseph’s Health Care London. The research team collected and analyzed patient urine samples and ureteral stents following surgical removal, as well as relevant patient information such as antibiotic use and history of infections.
“We wanted to know which bacteria were present and whether the bacteria found in urine samples corresponded to the bacteria found on a patient’s stent,” explains Dr. Kait Al, Postdoctoral Fellow at Lawson and at Western’s Schulich School of Medicine & Dentistry. “We found that there was a bacterial community present on almost all stents, even if they were not visibly affected, and that it differed from the bacterial community found in a patient’s urine.”
These findings challenge long-held beliefs that the urinary tract is a sterile environment devoid of bacteria.
The study revealed that the bacteria present were determined by an individual patient’s medical condition. They differed significantly based on comorbidities like irritable bowel syndrome, obesity and hypertension. Antibiotic use within the past 30 days did not seem to have an effect on the types of bacteria detected on the stents.
“While more research is needed, our study suggests that antibiotic use during the placement of these stents could one day be more conservative or targeted based on each patient’s condition,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The team also discovered that in patients needing multiple stents, the bacterial community remained stable over time, suggesting that infections on a patient’s previous stent could direct the course of treatment for their future device placements.
“This is the largest study of its kind, investigating bacteria both in urine and adhered to ureteral stents,” states Dr. Hassan Razvi, Urologist at St. Joseph’s, Lawson Associate Scientist and Professor at Schulich Medicine & Dentistry. “We hope this will be the first step towards personalized care, ultimately leading to fewer stent-associated infections.”
The study was made possible through the generous support of The W. Garfield Weston Foundation and St. Joseph’s Health Care Foundation.
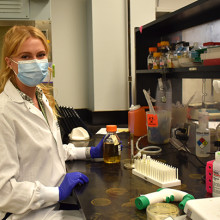
Dr. Kait Al, Postdoctoral Fellow at Lawson and Schulich Medicine & Dentistry
noteWORTHY – Teamwork and patients inspire clinical research assistant
St. Joseph’s celebrates people who provide exceptional care, grow stronger communities and contribute to a healthier world. Today, meet Heather LaPier, a clinical research assistant whose work helps keep clinical research running smoothly for four Lawson research scientists in diabetes and nephrology. She is a liaison among patients, researchers, clinicians, ethicists, regulatory bodies and pharmaceutical companies.
What values or people inspire your work:
I couldn’t ask for better than the physicians and researchers I work with. It’s a true team. We can bring our own ideas and expertise and know that we’re valued. We’re all good at showing appreciation for each other.
Best part of your workday:
Visiting with people receiving dialysis. They have treatment four hours a day, three times a week, so they’re used to talking with physicians and staff and we get to know them really well. They’re honest and funny – and, despite living with a chronic illness, they’re some of the most positive people I’ve ever met.
What one thing do you wish people knew about your work?
Our job is to advocate for patients and protect them, so every study is carefully designed, planned, regulated and monitored. We work to find solutions to patients’ health issues, and that means putting them first.
One big thing people should know is that participants in clinical trials and research studies get extra care and attention. Other patients have regular appointments, maybe every six months, but as a participant in research they’ll have even more frequent monitoring. So even though they’re helping advance medical knowledge generally and there’s no certainty of direct benefit to them from a specific clinical trial, they do have a whole team of people fully involved in their current care. Any time they have a question, they have direct access to an endocrinologist or nephrologist.
Why this work is meaningful to you:
It’s definitely exciting and always interesting. It can be easy to get caught up in the day-to-day tasks – but I never want to lose sight of the fact patients are living longer and better lives because of the work we’re doing. I have a front-row seat when patients come in for visits and tell us a diabetes treatment or a dialysis intervention is making them feel better.
Back-story:
My mom has been a nurse for over 30 years, so I grew up in a home where we talked about health and patient care a lot. We have a shared language. After my university degree, I applied to college for either forensic science or clinical research. I’m so glad clinical research is where I landed.
One other thing:
I love learning about the history of the Second World War, specifically naval ships and naval battles. It seems totally random, but I studied it as one of my non-science courses in university. I still find it fascinating.
Well said:
Heather is a true gem – highly skilled, creative, and an outstanding team player who expertly manages multiple research projects and investigators. She has been a game-changer for diabetes, metabolic, and chronic disease research at Lawson Research Institute, supporting everything from qualitative studies to large randomized-controlled trials with innovative designs. Our successes wouldn’t have been possible without her.
- Dr. Kristen Clemens, St. Joseph’s endocrinologist and Lawson Research Institute scientist
Ontario Brain Institute Public Talk: Dementia Beyond Alzheimer's
DEMENTIA BEYOND ALZHEIMER'S
Other neurodegenerative disorders like Parkinson's disease and ALS can also lead to dementia and other cognitive impairments. Hear from three London researchers who are re-examining how we speak, think, and move so we can understand, and eventually treat, dementia better.
Learn more at this free public talk by the Ontario Brain Institute featuring:
- Dr. Elizabeth Finger: Scientist and Neurologist, Lawson Health Research Institute
- Dr. Mandar Jog: Director of the National Parkinson Foundation Centre of Excellence, London Health Sciences Centre
- Dr. J.B. Orange: Professor, School of Communication Sciences and Disorders, Western University
Moderated by: Meredith Levine: Western Journalism Professor and Multimedia Journalist
Aeolian Hall, 795 Dundas Street East, London, ON N5W 2Z6
Registration: To register for the event, please visit the Ontario Brain Institute website.
The speakers are part of the Ontario Neurodegenerative Disease Research Initiative (ONDRI) - a provincial collaboration studying dementia and how to improve the diagnosis and treatment of neurodegenerative diseases. For more information, please visit: ondri.ca
Order of Canada honour for mental health researcher Cheryl Forchuk
Lawson Research Institute scientist Cheryl Forchuk focuses on ‘giving value and voice’
Renowned mental health and homelessness researcher Cheryl Forchuk, a Lawson Research Institute scientist and Distinguished University Professor, has been appointed an officer of the Order of Canada.
The award, one of Canada’s highest honours, was announced June 30 by Governor-General Mary Simon.
Forchuk has dedicated her career to driving change on complex issues, including addiction, homelessness and mental health challenges, emphasizing relationships and participation from the populations she studies.
“We’re talking about people that generally experience a lot of discrimination in society. When I started working in this field, it was really hard to get things funded because the groups themselves were not valued. Their opinion was not valued. A lot of my work is trying to give value and voice to these populations,” Forchuk said.
She said she was surprised and humbled by the appointment to the Order of Canada.
“I feel humbled, because all the research I do is part of a team effort. I have always had great support from community partners, people with lived experience, other researchers and my staff at the office.”
In addition to her role as Lawson scientist, Forchuk is a Distinguished University Professor in the Arthur Labatt Family School of Nursing in Western's Faculty of Health Sciences, with a cross-appointment in the department of psychiatry at Schulich School of Medicine & Dentistry.
Forchuk has published 200 articles and 12 books, delivered more than 600 conference presentations or workshops and supervised more than 60 graduate students.
Forchuk is known nationally and internationally for her work improving systems of recovery and community integration. Her team created the “transitional discharge model” to ensure people released from hospital maintain connections with service providers in hospital or in the community while receiving peer support from someone with lived experience. It was repeatedly shown to reduce the length of hospital stays while improving outcomes for patients.
The model has since been adopted in parts of Canada, the U.S. and Europe and was included as an example of mental health practice by the World Health Organization in its guidance on mental health services that respect human rights. Forchuk is currently conducting research on women veterans experiencing homelessness.
“A trailblazer in mental health and homelessness research, Dr. Forchuk has spent more than four decades advancing our understanding of these complex issues and shaping policies that have improved the lives of the unhoused,” said Jayne Garland, former dean of the Faculty of Health Sciences, and Forchuk’s nominator for the Order of Canada.
“She is a respected researcher, an influential leader and a passionate advocate for some of the most vulnerable members of our society. This recognition reflects the profound and lasting impact of her work.”
Forchuk’s studies have reduced crises and improved quality of life for hundreds of people, saving millions of dollars in health care and social service spending as a result.
“Dr. Forchuk is an innovative, forward-thinking leader in mental health, housing and homelessness,” said Victoria Smye, director of the Arthur Labatt Family School of Nursing.
“Her contributions in Canada and beyond to the mental well-being of some of the most vulnerable people in our society – people who have been highly marginalized by inequity – have made a real impact. She has truly changed lives.”
Forchuk said her appointment to the Order of Canada is meaningful, but not because of the personal or reputational benefits.
“Receiving this honour shows me there’s a recognition that these are important issues and these approaches to finding solutions – including people who are the experts, people with lived experience and those working on the frontlines – are valued,” Forchuk said.
“It tells me to keep going, and that it’s working, which we know. It solidifies that this is the right approach to address very complex societal issues, and to make sure we include the right voices.”
Those invested into the Order of Canada fall into three levels. Members of the Order of Canada are recognized for their service to a particular community or field, officers are appointed for their high degree of achievement or merit, especially for service to the entire country or humanity at large, and companions of the Order of Canada – the highest recognition – are those deemed to have made contributions of the highest degree to Canada or the world.
Over $10 million in funding announced from CIHR
Health researchers from across London were awarded more than $10 million from Canadian Institutes of Health Research (CIHR), with $2.8 million through Lawson Health Research Institute and $7.3 million through Schulich Medicine & Dentistry. A total of 15 projects were funded.
CIHR’s Project Grant program is designed to capture ideas with the greatest potential for important advances resulting in the creation of new knowledge and its translation into improved health and health care for Canadians.
Congratulations to all of the successful applicants!
Projects through Lawson Health Research Institute:
Karen Bosma, and Laurent Brochard: “Proportional Assist Ventilation for Minimizing the Duration of Mechanical Ventilation: The PROMIZING Study.”
Critically ill patients frequently require the life-sustaining technology of mechanical ventilation, but prolonged use can place patients at risk for long-term functional impairment and increased mortality, and is also costly to the health care system.
The PROMIZING Study is an international, multi-centre randomized clinical trial that will identify ways to reduce the duration of mechanical ventilation for patients at greatest risk and to determine whether a novel mode of ventilation developed in Canada could replace the standard of care.
“It is vital that Canada continue to invest in high impact, hospital-based research such as the PROMIZING study which enable researchers to develop and test treatments, technologies, and procedures that will improve clinically relevant, patient-important outcomes while also improving the efficiency of our healthcare system.” – Dr. Karen Bosma
Diane Bryant, and Alan Getgood: “Anterior Cruciate Ligament Reconstruction using Bone Patellar Bone or Quad Tendon Autograft with or without Lateral Extra Articular Tenodesis in Individuals who are at High Risk of Graft Failure (STABILITY II)”
Anterior cruciate ligament reconstruction (ACLR) is complicated by high failure rates in young active individuals, which is associated with worse outcomes and higher rates of osteoarthritis.
Currently, there are different types of grafts being used to rebuild a torn ACL. There is a need to evaluate whether one method is better at reducing failure, minimizing complications and creating better outcomes in terms of functional performance. This study will determine the best graft choice for young patients at risk of ACLR failure which will ultimately lead to positive effects on activity and quality of life.
Patrick Luke and Rabindra Bhattacharjee: “Therapeutic potential of bloodless oxygenated perfusion of donor kidneys for prolonged storage and protection for transplantation.”
Kidney failure among Canadians has tripled over the last 20 years. Transplantation improves the quality of life and survival of patients at a much lower cost than dialysis. However, only 40 per cent of patients receive functional kidneys due to lack of living organ donors.
To increase the number of kidneys available for transplantation, surgeons are accepting orgrans from deceased donors. Currently, during storage, the organs can suffer injuries from a lack of oxygen as well as cold temperatures and the conditions are not conducive to use drugs that can prevent damage.
The study is looking at the effects of a bloodless oxygen carrying perfusion liquid that will allow the storage of human donor kidneys for long periods of time at room temperature, and will also evaluate if certain drugs can maximize the preservation of these organs.
“Hospital-based research institutes are uniquely positioned to conduct patient-centred research. Investment through CIHR supports the physicians and researchers who are committed to improving treatments for patients at the front line of care.” – Dr. Patrick Luke
Emil Schemitsch: “The DECIPHER Study: DEterminants of Function and Clinically Important outcomes in Proximal Humerus Fractures in the Elder Population: A National CohoRt.”
Shoulder fractures are becoming increasingly common for older adults and cause considerable limitations and impacts for their daily life. While different approaches are taken to treat shoulder fractures, there is a lack of knowledge and evidence to show which of those methods are the most effective and for which patients.
The DECIPHER study will seek to answer important questions about which treatment and rehabilitation strategies are best for different patients, strengthening the clinical strategy for managing these difficult and prevalent injuries. It will also provide an economic analysis to understand the impact for healthcare system costs.
“Such an analysis has the potential to significantly affect patient care and Canadian practice patterns, as well as inform the development of future pivotal clinical trials. DECIPHER will have an important impact on patient care, health system costs and future research directions locally, nationally and internationally.” - Dr. Emil Schemitsch.
Projects through Schulich Medicine & Dentistry:
Subrata Chakrabarti, with collaborators Bekim Sadikovic, Krishna Singh, and Stephanie Frisbee: “Novel mechanisms in diabetic cardiomyopathy.”
Peter Chidiac and Jeffrey Dixon: “Allosteric regulation of GPCR signaling by extracellular nucleotides.”
Bryan Heit: “Role of ELKS1 and Rab17 in Differential Antigen Sorting and MHC II Trafficking Following Efferocytosis and Phagocytosis.”
Marlys Koschinsky and Michael Boffa: “B Apo(a):apoB100 interactions as key determinants of Lp(a) biosynthesis.”
Shawn Li: “Novel anticancer immunotherapy targeting the molecular mechanisms of T cell suppression by immune checkpoints.”
Julio Martinez‐Trujillo and Michael Poulter: “Reverse engineering working memory circuits in the primate brain: Implications for the study of memory deficits.”
Maria Mathews and Jennifer Shea with collaborators, Ivy Bourgeault, Emily Marshall, Amy Bombay, Nicole Doria, Julia Lukewich, and Amanda Myers: “Increasing Indigenous Participation in the Physician Workforce.”
Charles McKenzie, and Timothy Regnault: “Hyperpolarised 13C MRI of Placental Metabolism in Intrauterine Growth Restriction.”
Marco Prado: “A Regulation of chaperone‐mediated proteostasis by STI1.”
Lloy Wylie and Lana Ray with collaborators Christopher Mushquash, Victoria Smye, Nadine Wathen, Cheryl Forchuk, and Brock Pitawanakwat: “Educating for Equity: Building Culturally Safe Care through Indigenous Narratives.”
Xiufen Zheng: “The role of circular RNA in heart transplantation”
Over $2 million in federal funding to advance discoveries in health research
Last week, the Honourable Kirsty Duncan, Minister of Science and Sport, announced an unprecedented investment of more than $588 million through the Natural Sciences and Engineering Research Council of Canada’s (NSERC) Discovery Grants program.
The successful applications in London include 12 projects funded for Lawson Health Research Institute scientists, through Western University. In total, they will receive $2.3 million in funding over five years.
“The funding demonstrates our strong and enduring commitment to science and researchers. Since taking office, our government has worked hard to bring science and research back to their rightful place and this historic investment in the discoveries of tomorrow is just one example of how we are achieving this goal,” says The Honourable Kirsty Duncan, Minister of Science and Sport.
Across Canada, this funding will go to more than 4,850 researchers and students as they pursue their world-leading discovery work. It also includes support for nearly 500 early-career researchers who will bring a diversity of new voices and new insights to their fields.
Local research highlights
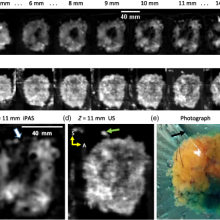
Dr. Jeffrey Carson is exploring the role of photoacoustic imaging as a method for detecting breast cancer. Currently, during the procedure the breast must be submerged in a tank of water to enhance the transmission of photoacoustic waves from the breast to the sensors.
“The water tank is cumbersome and impractical,” notes Dr. Carson. “Our goal is to eliminate the need for the water tank by detecting the photoacoustic waves through the air without making contact with the breast.” Their hope is that the project leads to the development of a non-contact photoacoustic scanner offering women the opportunity to sit or stand comfortably during breast imaging. “This simple improvement could greatly accelerate the adoption of photoacoustic imaging for breast cancer screening.”
Dr. Carson adds that funding like this provides graduate student trainees opportunities to develop knowledge and skills in engineering, mathematics, and biophysics. “They bring innovative new ideas to the Canadian medical device industry through employment and entrepreneurship.”
Dr. Rajnikant Patel is developing advanced robotic and intelligent systems for the next generation of systems and devices for minimally invasive surgery and therapy. These reduce trauma and costs while enhancing efficiency and reliability.
“For us, this funding opportunity is unique because it supports a program of research rather than a project,” says Dr. Patel. “We can explore new areas and directions that will lead to research projects and medical applications. A program that investigates novel robotic and AI technologies fits well with NSERC’s mandate.”

Dr. Gregor Reid is leading a revolutionary project that could save the world’s honeys bees, insects that are vital to human survival.
The intent is to develop an understanding of how lactobacilli strains can counter the most widely used pesticides that are wiping out nature's critically important pollinators. The lactobacilli appear to potentially degrade some of these toxic chemicals and improve the ability of honey bees to fight off early death.
“NSERC funding gives ideas like this a chance and even though the funding amount is relatively small, it allows graduate students to apply for their own awards and work on the project,” explains Dr. Reid. Students Brendan Daisley and Johnny Chmiel have been awarded NSERC scholarships to work on this important research.

Dr. Xiugen Zheng’s project is investigating the role of circular RNA AEBP in the development and function of dendritic cells which are very important immune cells in the immune system. This will provide insights into new molecular and gene regulators, and their impact on the immune system and overall health.
“NSERC research funding greatly supports us to study the basic scientific questions that are critical for better understanding health problems and developing treatment for diseases,” says Dr. Zheng.
Dr. Rudolf Veldhuizen’s laboratory aims to understand how surfactant performs its function at a molecular and biophysical level. Pulmonary surfactant is a material in the lung that allows people and other mammals to breath with minimal effort. You can see this in babies who are born prematurely and have trouble breathing due to the lack of surfactant.
“Previous work has established a generalized model of how surfactant improves lung function under standardized conditions. This, however, does not explain how surfactant functions in extreme conditions,” says Dr. Veldhuizen. “By exploring conditions in comparative, mechanistic studies we will be able to establish a more universal understanding of surfactant function.”
This funded work provides a foundation for clinically relevant studies to further explore the role of alterations to surfactant in lung injuries and the opportunities for therapeutic interventions.

Dr. Shou Li is developing state-of-the-art machine learning system able to analyze huge amounts of clinical data and provide human level intelligent analysis. This work will enable the prediction of disease onset, progression and prognosis. “It is added value that will lead to more effective and efficient health care,” explains Dr. Li.
He adds that this funding is supporting a multi-disciplinary research program that combines the strength of multiple teams. “We will look at both the fundamental side of machine learning systems and clinical applications. In this way, we connect basic science with clinical science.”

Congratulations to all the Lawson scientists who received funding:
- Dr. Dean Betts for Metabolic reprogramming to enhance the generation of canine induced pluripotent stem cells (Physiology and Pharmacology)
- Dr. Jeffrey Carson for Development of non-contact photoacoustic tomography (Medical Biophysics)
- Dr. Louis Ferreira for Multi-Directional Mechanical Testing of Bone using CTCompatible Loading Mechanisms (Mechanical and Materials Engineering)
- Dr. Shuo Li for Innovative Machine Learning for Medical Data Analytics (Medical Imaging)
- Dr. Penny MacDonald for Investigating cognitive functions mediated by ventral and dorsal striatum (Clinical Neurological Sciences)
- Dr. Charles McKenzie for Fetoplacental Molecular and Metabolic Magnetic Resonance Imaging; instalment (Medical Biophysics)
- Dr. Rajnikant Patel for Design and Control of Robotic Systems and Devices for Medical Applications (Electrical and Computer Engineering)
- Dr. Gregor Reid for Detoxification functionality of lactic acid bacteria (Microbiology and Immunology)
- Dr. Rudolf Veldhuizen for Mechanisms of surface tension reduction by pulmonary surfactant (Physiology and Pharmacology)
- Dr. Aaron Ward for Machine learning-based quantitative image, tissue, and clinical data analysis for lesion detection and characterization on prostate cancer imaging (Medical Biophysics)
- Dr. Eugene Wong for Optimization of spatiotemporal-modulated electric fields and fabrication of organs-on-chips for applications in Medical Physics (Physics and Astronomy)
- Dr. Xiufen Zheng for The role of circular RNA AEBP2 in dendritic cells (Pathology)
Parkwood Institute Research Open House
Join us for the Parkwood Institute Research Open House on Thursday, December 1st, 2022 from 11:00am-2:00pm.
The Parkwood Institute Research (PIR) Open House is your opportunity to virtually meet research teams working in the areas of cognitive vitality and brain health, mobility and activity, and mental health. This is an exciting opportunity to learn about the exciting research that is being done in London, ON Canada.
Your free registration gives you exclusive access to video presentations from our labs. Potential research participant opportunities include live polls, games, Q&A session, surveys, and discussion boards. You’ll also be able to provide feedback on the event. Whova is accessible on phones, tablets or laptops. You do not need a camera or microphone to participate.
Register now: Parkwood Institute Research Open House Registration (whova.com)
Quick link: https://whova.com/portal/registration/piroh1_202212/
Please feel free to share with your circles, everyone is invited to attend.
We hope to see you there!
Dr. Cheryl Forchuk and the PIR Open House Committee

Partnership with Siemens Healthineers will create a centre of excellence in advanced diagnostic imaging and therapeutics
Continuing to build on the established excellence in medical imaging, London’s academic teaching hospitals, London Health Sciences Centre (LHSC), and St. Joseph’s Health Care London, and Western University’s Schulich School of Medicine & Dentistry announced a partnership with Siemens Healthineers in magnetic resonance imaging (MRI), interventional angiography, cardiology and cardiac surgery that will create a centre of excellence in advanced diagnostic imaging and therapeutics in southwestern Ontario.
This new partnership includes the creation of an education, training and scientific research support fund in the area of advanced diagnostic imaging and therapeutics. Siemens will provide in excess of $1 million in support funding for research, advanced clinical applications, teaching and outcomes analysis.
“This partnership represents another important building block in the incredible foundation of imaging excellence that we have in London,” says Dr. Narinder Paul, Chair/Chief of the Department of Medical Imaging at LHSC, St. Joseph’s, and Schulich Medicine & Dentistry.
“Not only will we become leaders in state-of-the-art imaging and intervention through the centre of excellence, but thanks to the research contribution from Siemens Healthineers, we will also have dedicated funds for critical research in cardiovascular and neurological diseases that will translate to improved services and outcomes for patients in London and the region.”
The research fund will support collaborations between research teams in diagnostic and interventional radiology, cardiology, and cardiac surgery, with imaging scientists at Lawson Health Research Institute, the research institute of LHSC and St. Joseph’s, and Schulich Medicine & Dentistry’s Robarts Research Institute, as well as research teams from across Western. These teams will partner with scientists from Siemens Healthineers to focus on improving both the patient experience and the outcomes in important cardiovascular and neurological diseases. The research funds will be leveraged against provincial and federal research grants to increase the funds available to the research teams.
“Collectively, Western and our partner institutions in London are becoming a global powerhouse, recognized for our expertise and facilities in imaging that drives discovery and innovation across a broad range of disciplines,” says Alan Shepard, President & Vice-Chancellor of Western University. “This partnership with Siemens Healthineers builds on our strengths, increases capacity to enhance patient care, and expands opportunities to integrate education, training and research for the benefit of learners and faculty. It’s a huge win for London and southwestern Ontario.”
“Imaging scientists and clinicians, working on campus and within hospital walls, have positioned London as a leader in non-invasive biomedical imaging, conducting groundbreaking research that impacts health care here and around the world,” adds Dr. David Hill, Lawson Scientific Director and Integrated Vice President, Research for London’s hospitals.
“With strong industry partnerships and working seamlessly with our hospitals and academic partners, we can build on this success. The advancements made here can be quickly translated into care within the very units where the testing is being done, which ultimately improves care for the patients and families that we serve.”
The centre of excellence will provide hands-on training in MRI, diagnostic, and interventional catheter procedures through development of advanced simulation and phantom models. Medical learners and radiologists, cardiologists, cardiac surgeons, neurologists, neurosurgeons, and technologists in London and from across Canada will be able to access this centre to improve their diagnostic and therapeutic skills, which will in-turn improve patient access to skilled clinicians.
As well, LHSC and St. Joseph’s are acquiring six clinical MRIs and six angiogram suites to be used for patient care, which will include the introduction of the first 3T MRI in the region. University Hospital will acquire a 3T/1.5T pair of MRIs, and two biplane angiogram suites. Victoria Hospital will acquire a 3T/1.5T pair of MRIs, a biplane and two single plane angiogram suites. St. Joseph’s will acquire a 3T/1.5T pair of MRIs, and a single plane angiogram suite.
“Investments in capital equipment, such as these new MRI machines and angiogram suites, are incredibly important as they will immediately translate into safer, higher quality care for the patients we serve – in this case it’s by offering the highest resolution images available, in less time, and with improved comfort for patients,” says Dr. Paul Woods, President and CEO, London Health Sciences Centre.
“London has an illustrious history of innovation that has been groundbreaking in shaping the scope and possibilities of medical imaging within the health-care system,” says Dr. Gillian Kernaghan, President and CEO, St. Joseph’s Health Care London. “This exciting partnership ensures our ongoing leadership and expertise in the introduction of leading-edge medical imaging technologies and is a critical step toward new approaches in imaging research and patient care.”
MRI is used to provide critical diagnostic information about the physical structure and the biological processes of the body. MRI scanners differ from other imaging technologies as they use strong magnetic fields, magnetic field gradients, and radio waves, instead of X-rays, to generate images of the organs in the body. MRI is widely used in hospitals to facilitate medical diagnosis and/or the staging of disease without exposing patients to radiation.
