Search
Search
Pinpointing the role of language disruptions in psychosis
LONDON, ON - The ability of humans to use language may also be what puts us at the unique risk of developing psychosis, a subset of mental illness characterized by changes in emotions, impaired functioning, and a disconnection from reality.
Difficulties with communication – both the ability to use language and to comprehend what others are saying – are some of the earliest symptoms. New research from Western University and Lawson Health Research Institute has shown that this may be because in patients with psychosis parts of the brain not meant to process language are trying to perform this complex job. Like a small airport trying to handle all the air traffic from a big hub like Pearson International Airport, some brain regions may be overloaded in psychosis.
“The language system seems to be key to understanding this illness,” said Dr. Lena Palaniyappan, the Tanna Schulich Chair in Neuroscience and Mental Health at Western’s Schulich School of Medicine & Dentistry and Scientist at Lawson and Robarts Research Institute. “We don’t yet fully understand how the disorganization of language takes place in patients affected by psychosis.”
Embarking on a mission to find out, Dr. Palaniyappan worked with a team of imaging scientists at Robarts to perform MRI scans on the brains of patients with acute psychosis. Patients were recruited from the Prevention and Early Intervention Program for Psychoses (PEPP) at London Health Sciences Centre, a flagship clinic that supports young individuals from a very early stage of psychosis.
The team divided the patients into two groups – those with severe language disturbances, and those whose language symptoms were less pronounced. They found that both groups had weakening of connectivity, or ‘hubness,’ in the part of the brain generally associated with language -- the superior temporal area. The group with more severe language symptoms also showed an emergence of higher hubness in some unexpected regions of the brain that may be compensating for some of the lost connectivity elsewhere.
“This finding led us to believe that the language problems may occur because the main hubs that are supposed to conduct language are now retired, and so these peripheral hubs, which have no business of orchestrating language as their main function, are picking up the job and aren’t doing it very well,” said Dr. Palaniyappan.
The researchers hope that by understanding how language becomes disorganized in psychosis, the data can inform new interventions to focus on strengthening the language systems in the brain to reduce or delay psychotic symptoms.
Using ultra-high-field magnetic resonance imaging at Robarts Research Institute, they were able to look at the entire brain of patients with acute psychosis. Instead of homing in on one specific area, the team looked at 3-D pixels of the brain (voxels) to get a full picture of what was happening in the whole brain and how different areas were interacting.
Using the airport analogy, Palaniyappan said that if they had only looked at the language area it would have been like only walking into one airport, and not understanding how the reduced traffic in that airport was influencing the air traffic at other surrounding airports.
“We went in without any expectations, and searched the whole brain,” said Palaniyappan. “This unique approach allowed us to get a picture of the forest rather than a picture of the tree.”
The study was funded through an early-career foundation grant from the Canadian Institutes of Health Research and was supported by PEPP.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Poop in a pill helping advance cancer care
Lawson Research Institute scientists have perfected the delivery of fecal transplants via patient-friendly capsules now central in ground-breaking cancer treatment studies.
It’s one of the most exciting areas of research in cancer care.
Making waves in scientific and health care circles worldwide, it holds the potent potential to “jazz up” cells that attack cancer and boost the body’s response to treatment.
So what is this powerful ally? It’s poop in a pill – home-grown right here at St. Joseph’s Health Care London and Lawson Research Institute.
In fact, Lawson scientists Dr. Michael Silverman, Seema Nair Parvathy, PhD and their team are considered poop pill pioneers, having perfected the delivery of fecal transplantation by way of patient-friendly capsules that can be easily swallowed. These capsules contain healthy gut microbes that have become pivotal in many landmark cancer treatment studies.
Triggering an immune response
Understanding the role of poop in cancer treatment requires grasping the wonders of the human microbiome and its key role in influencing health and well-being.
The human microbiome consists of trillions of microorganisms that live inside and outside of the body, including bacteria, viruses and yeasts. While some bacteria are associated with disease, others are vital to the human immune system – the body’s main protective and disease-fighting tool – and many other aspects of health. Over the past decade, microbiome research has led to a revolution in medicine as scientists unravel just how an imbalance of these microorganisms interferes with many aspects of good health.
"(Fecal microbial transplants) allows us to harness the immune system to mount a stronger defence." Dr. Michael Silverman
The goal of fecal microbiota transplants (FMT) is to transfer healthy gut microbes from donors into patients with cancer and other diseases so that healthy bacteria will colonize in the patient’s gut and improve the microbiome, explains Silverman, Medical Director of St. Joseph’s Infectious Diseases Care Program and citywide Chief of Infectious Diseases for London’s hospitals.
To do so, stools are collected from carefully screened healthy donors, prepared in a lab into capsule format, and introduced into a patient’s gastrointestinal tract.
“What is so exciting when it comes to cancer treatment is the evidence we now have showing how a healthy microbiome activates the immune response to tumours to make the treatment more effective,” Silverman adds. “It allows us to harness the immune system to mount a stronger defense.”
St. Joseph’s capsules are central to several significant studies currently underway aimed at improving treatment for lung, kidney, breast, renal, pancreatic and other cancers.
Among the most notable is the London team’s lead role in a ground-breaking national study – one of the world’s largest randomized controlled clinical trials using FMT to improve the effectiveness of the standard of care for advanced melanoma, a type of skin cancer.
Improving melanoma survival rates
About 11,300 Canadians will be diagnosed with melanoma in 2024 and, even with standard treatment, about half that number will experience disease progression and die.
The 16-site Canadian trial builds off the work of Silverman, Parvathy and their team, in partnership with Saman Maleki, PhD, and Dr. John Lenehan at London Health Sciences Centre. Together, they were the first to demonstrate the safety and therapeutic potential of using the capsules produced at St Joseph’s to influence a patient’s gut microbiota to enhance immunotherapy and increase the odds of surviving advanced melanoma.
“London is seen as having the most expertise in use of FMT in cancer care in the world and is a driving force in moving this forward,” says Silverman. “Immunotherapy is rapidly expanding the number of treatable cancers and our FMT therapy is helping to accelerate this progress.”
Poor sleep linked to multiple chronic conditions
When clinicians are focusing on lifestyle changes for the management and prevention of multiple chronic conditions, they will often ask patients about their alcohol consumption, smoking habits, exercise regime and diet. But what about the quality and duration of their sleep?
Researchers at Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry have shown that how well you sleep and for how long is linked to increased odds of living with multiple chronic conditions, and argue that promotion of good sleep habits should be given greater focus in clinical practice and public health.
The study, “Sleep behaviours and multimorbidity occurrence in middle-aged and older adults,” was recently published in the journal Sleep Medicine. Funded through Lawson’s Internal Research Fund, it used data from more than 30,000 adults over the age of 45 who were part of the Canadian Longitudinal Study on Aging (CLSA).
“Sleep is still a neglected clinical and public health issue, and this study provides additional evidence of the potential role of sleep for the prevention and management of several chronic conditions,” said Dr. Saverio Stranges, principal investigator on the study, Professor and Chair of the Department of Epidemiology and Biostatistics at Schulich Medicine & Dentistry, and Lawson Associate Scientist.
The team looked specifically at the occurrence of multimorbidity, which is defined as having multiple chronic conditions (two or more) that have been diagnosed in a single individual. The conditions can include relatively common chronic disease such as diabetes and hypertension, to depression and cancer, among others.
The study found that there was a consistent relationship between the odds of multimorbidity and self-reported poor sleep quality and altered sleep duration, which includes both too much and too little sleep.
Specifically, male participants who were dissatisfied or very dissatisfied with their sleep had a 20 per cent increase in the odds of multimorbidity. And participants aged 65 to 74 years of age who self-reported dissatisfaction with their sleep quality had a 43 per cent increase in the odds of multimorbidity.
When looking at sleep duration, while the study found a link between multimorbidity and getting too little sleep, the researchers actually found that too much sleep had a much stronger link.
Female participants who self-reported short sleep duration (less than 6 hours a night) had a 16 per cent increase in the odds of multimorbidity and those who self-reported long sleep duration (more than 8 hours a night) had a 44 per cent increase in the odds of multimorbidity. Male participants who self-reported long sleep duration had a 45 per cent increase in the odds of multimorbidity.
Previous international research has shown an association between sleep and a range of chronic conditions, but this is the first Canadian study to look specifically at the relationship between sleep and multimorbidity among middle-aged and older adults.
“This study highlighted an important relationship between self-reported sleep patterns, both duration and satisfaction, and the odds of multimorbidity among older female and male adults in Canada,” said Dr. Kathryn Nicholson, Adjunct Assistant Professor at Schulich Medicine & Dentistry, who was the lead author on the study. “Although it is important to acknowledge that this relationship was cross-sectional and causation cannot be determined from this study, we were fortunate to utilize a comprehensive data source like the CLSA, which allowed us to examine both the self-reported patterns of sleep and the occurrence of multimorbidity.”
The authors point out in the paper that there is already established evidence showing that lack of sleep has negative effects on the cardio-metabolic, endocrine, immune and inflammatory systems, and that over the past several decades the population has been experiencing poorer quality of sleep.
“This is concerning because if poor quality of sleep can increase the risk of a range of chronic conditions, then we should be concerned about sleep hygiene and put that at the centre of our focus both as clinicians and as public health scientists,” said Dr. Stranges.
The researchers will be continuing their research by using the first set of follow-up data from the CLSA to begin to explore longitudinal patterns between multimorbidity and other health indicators.
“High-quality sleep can be very beneficial, but achieving this high-quality sleep can sometimes be a challenge. We hope that this study will continue to emphasize the importance of focusing on sleep as a key health indicator and ideally, this assessment of sleep will include a focus on sleep quality and sleep duration and be a point of conversation during a clinical encounter for all patients living with multimorbidity,” said Nicholson.
Additional study authors are Rebecca Rodrigues, Dr. Kelly K. Anderson, Dr. Piotr Wilk and Dr. Giuseppe Guaiana.
Precise, high-dose radiation safe and effective for inoperable kidney cancer, study suggests
LONDON, ON – A new study published in The Lancet Oncology suggests that a very precise, high-dose form of radiotherapy called stereotactic ablative radiotherapy (SABR) may be a new treatment option for patients with inoperable kidney cancer. Lawson Health Research Institute was one of 12 participating centres from around the world with patients recruited from London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP).
The analysis, among the first to look at the long-term impact across multiple centres, included 190 patients with primary renal cell carcinoma, the most common type of kidney cancer. It found SABR to be effective and safe with a low rate of cancer recurrence and acceptable impact on renal function. Five years after treatment, kidney function was largely maintained and only 5.5 per cent saw their cancer return in the treated kidney.
SABR directs highly accurate and intense radiation to eradicate tumours while limiting the impact on surrounding tissues. The treatment is offered to patients who are unable or unwilling for various reasons to have surgical treatment.
Previous studies on the use of SABR for primary renal cell carcinoma have been encouraging, but this publication represents the first report of long-term follow-up from a large, international group of patients.

“This study suggests that the positive outcomes seen in our prior studies are long-lasting,” says Dr. Rohann Correa. “It shows that this non-invasive treatment is worthy of further clinical study in patients with kidney cancer.”
Dr. Correa, a Lawson Scientist and Radiation Oncologist at LHSC, says this study was the result of many years of international collaboration.
“The International Radiosurgery Consortium of the Kidney (IROCK) brought together global experience with this completely non-invasive, pioneering way to treat localized kidney cancer,” Dr. Correa explains. “Our study has shown that at five years, this technique appears to be safe and effective, giving us confidence to launch clinical trials that provide patients access to this promising treatment.”
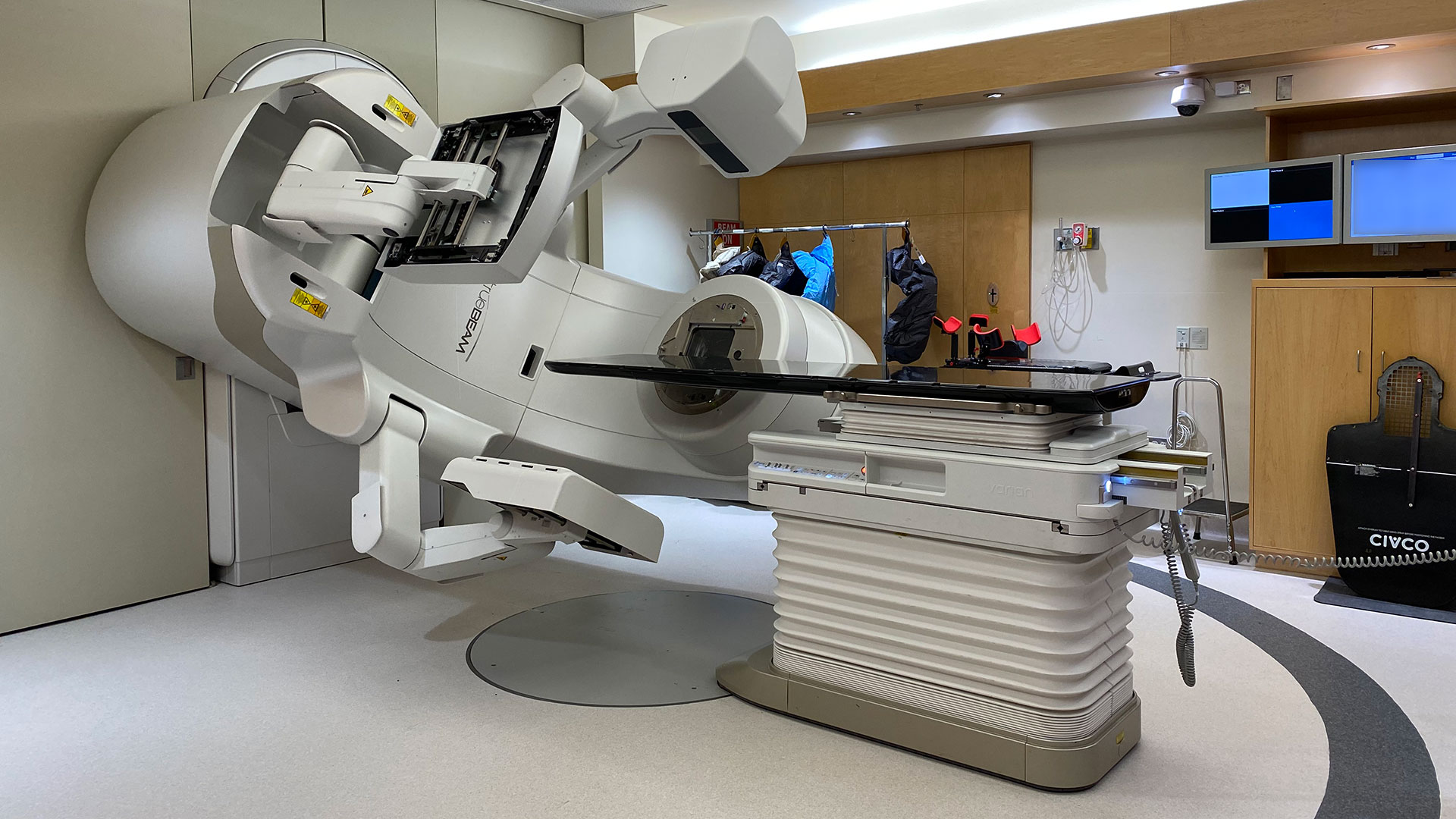
The study was led by Dr. Shankar Siva, a Radiation Oncologist at the Peter MacCallum Cancer Centre in Australia. Dr. Siva and Dr. Correa’s teams are part of the collaborative IROCK group whose members include Surgical Oncologists and Radiation Oncologists from around the world. The team at Lawson and LHSC was a key contributor to this high-profile study, with local patients participating in the study and all international data housed and analyzed through Lawson.

Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Pregnant women who use marijuana almost three times more likely to have low birth weight infant
In a new study, researchers in London, Ontario found that women who used marijuana while pregnant were almost three times more likely to have an infant with low birth weight than women who did not use marijuana.
The study analyzed data from perinatal and neonatal databases at London Health Sciences Centre (LHSC) and is the first large-scale study in Canada to show this association between marijuana use among pregnant women and low birth-weight infants.
It was conducted by researchers at Lawson Health Research Institute, Western University and Brescia University College.
Maternal amphetamine use, chronic hypertension and smoking were identified as other top risk factors for low birth weight. The study also examined predictors of preterm birth, which included previously diagnosed diabetes, maternal narcotic use and insulin-controlled gestational diabetes.
“Low birth weight and preterm birth are serious public health problems. Both are associated with a higher risk of infant mortality,” says principal investigator Dr. Jamie Seabrook, a Lawson associate scientist; and professor at Brescia University College, an affiliate of Western University, and Western University’s Schulich School of Medicine & Dentistry.
Low birth weight can lead to respiratory problems and asthma, and poor cognitive development during childhood. It also increases an infant’s risk of developing type 2 diabetes, hypertension and cardiovascular disease later in life. Preterm birth can cause childhood neurologic disability, as well as long-term medical consequences including respiratory, gastrointestinal and cardiovascular diseases and decreased immunity.
The research team investigated many potential factors that could be linked to birth outcomes, including demographics, prenatal factors and medical risks. The objective of the study was to determine the relationship between socioeconomic status and adverse birth outcomes, particularly low birth weight and preterm birth, in Southwestern Ontario.
However, they found that socioeconomic status had little influence on birth outcomes.
“There is a widely-held view that socioeconomic status is highly associated with low birth weight and preterm birth. However, there have been few population-based studies investigating this relationship in Canada. Most of this research has come from other developed countries, particularly the United States,” says Dr. Seabrook, who is also a Faculty Associate at Western’s Human Environments Analysis Laboratory. “It’s possible that Canada’s universal health care system provides a larger safety net for these mothers and their children.”
Live births between February 2009 and February 2014 at LHSC were included in the study. Infants with a birth weight of less than 2500 grams were classified as low birth weight. Preterm birth was defined as a live birth at a gestational age of less than 37 weeks.
The rates of low birth weight and preterm birth found in the study were 6.4 per cent and 9.7 per cent, respectively. The study notes that these rates are comparable to those reported by the Canadian Institute for Health Information in 2010-11, which found that 6.6 per cent of infants in Canada had low birth weight and 8.1 per cent were preterm births.
Median neighbourhood income was used as an indicator of socioeconomic status. Postal codes of the mothers were entered into a Geographic Information System and mapped to determine the location of home neighbourhoods, defined by boundaries of census dissemination areas. Dr. Seabrook adds that while the database used in the study included a large population-based sample, it is possible there may be incomplete or inaccurate data since it was obtained from chart records. For example, information on individual household income and length of time at an address was not available.
Along with Dr. Seabrook, the research team included Dr. Jason Gilliland, a scientist at Children’s Health Research Institute (a program of Lawson), Director of the Human Environments Analysis Laboratory at Western and professor at Schulich Medicine & Dentistry; Dr. Barbra de Vrijer, associate scientist at Children’s Health Research Institute, consultant in LHSC’s Obstetrics & Gynaecology department and associate professor at Schulich Medicine & Dentistry; Dr. Debbie Penava, Lawson scientist, LHSC physician and associate professor at Schulich Medicine & Dentistry; Dr. Paula Dworatzek, Chair and Associate Professor, School of Food and Nutritional Sciences at Brescia University College; and Emily Campbell, MScFN, RD, who was a graduate student at Brescia University College at the time of the study.
“Socioeconomic status and adverse birth outcomes: A population-based Canadian sample” was published in the Journal of Biosocial Science.

Above: Dr. Jamie Seabrook
Preventing infertility in men who undergo lymph node removal surgery for testicular cancer
When patients with testicular cancer undergo lymph node removal surgery there is a risk that their fertility will be affected if proper nerve sparing techniques are not used. Up to 75 per cent of men will not be able to father children if they receive the surgery without these techniques.
Lawson’s Internal Research Fund (IRF) has awarded a grant to Dr. Nicholas Power, a researcher at Lawson and urologic oncologist at London Health Sciences Centre (LHSC), who is leading a study to identify the nerves involved in fertility that are affected in lymph node removal surgery for testicular cancer.
“Sometimes patients go through a lot to be cured of testicular cancer only to be left dealing with long-term survivorship issues such as fertility. We hope to gain new insights into how fertility can be preserved after these men receive lymph node removal surgery,” says Dr. Power, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
In collaboration with Schulich assistant professors Dr. Marjorie Johnson and Dr. Brian Allman, and PhD candidate Tyler Beveridge, Dr. Power published initial results in The Journal of Urology announcing their discovery of a brand new anatomic structure, the pre-hypogastric ganglion, which needs to be spared in surgery to maintain fertility. They were also able to describe the first roadmap of retroperitoneal neuroanatomy – the anatomy of nerves in the space where surgeons locate lymph nodes most commonly affected by testicular cancer that has spread.
“There has never been a definitive anatomic study of the nerves of the retroperitoneum so it was our goal to provide the first comprehensive study of the nerves as they relate directly to patients who have testicular cancer,” explains Dr. Power. “After we published the initial results we were approached by textbook authors to use our data in upcoming editions of anatomy and surgical atlases. This will help to provide insight into nerve sparing techniques for surgeons who have not been trained at high-volume centers and ultimately improve the quality of care in testicular cancer patients overall.”
Already Dr. Power has found that using this knowledge when he performs lymph node removal surgery for testicular cancer has led to a 95 per cent success rate of preserving fertility.
The IRF will go towards their research to further investigate the actual function and physiology of the retroperitoneal neuroanatomy using a pig model.
“Lawson’s IRF provides incredible support for a field of study such as ours that is not yet at the stage of applying for a large grant. Receiving the funding gives us the independence to test out novel yet important hypotheses that will then lead us to further grants,” says Dr. Power.

Above: Dr. Nicholas Power
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
Prevention and Awareness: Delirium
You are invited to the first in a series of Research Bites,. These informative and interactive talks will focus on specific illnesses, their prevention and related research being conducted by researchers in London, Ontario.
Topic: Prevention and Awareness: Delirium

Dr. O'Regan will share about delirium and what it means, and provide highlights of her ongoing research happening locally. She will also be speaking about how to recognize delirium in a loved one and what to do in this scenario, as well as the steps you can take to help prevent it.
Date: Thursday, January 24, 2019
Time: 4 - 5 pm
Location: Parkwood Institute, Mental Health Building, Auditorium (F2-235)
550 Wellington Road South
London, Ontario N6C 0A7
Maps and Directions for Parkwood Institute.
Parking: The lot rate is $4.00 when you enter. $1 and $2 coins and credit card accepted (press the start button then insert payment)
Registration is required and spots will fill up quickly.
Click here to register.
These talks are hosted by Parkwood Institute Research, a program of Lawson Health Research Institute.
Prime Minister announces support for health research
Health researchers in London and across Canada welcomed news that the federal government will provide urgently-needed financial support for research teams whose work has been largely shut down by the COVID-19 pandemic.
Prime Minister Justin Trudeau has announced $450 million in new funding to help Canada’s academic research community during the COVID-19 pandemic.
“Research staff in Canada are the source of new innovations and ideas that help keep us healthy, protect our environment, and drive our economy. We are fortunate to have some of the world’s brightest minds. We are making sure Canadian universities and health research institutes have the support they need to sustain their research capacity through this difficult situation, and continue to attract and retain talent, for the benefit of all Canadians,” says The Rt. Hon. Justin Trudeau, Prime Minister of Canada.
The investment will:
- Provide wage supports to universities and health research institutes, so they can retain their research staff who are funded from industry or philanthropic sources and are unable to access some of the government’s existing COVID-19 support measures. This would apply even if their work has been temporarily suspended. The government will provide up to 75 per cent per individual, with a maximum of $847 per week.
- Support universities and health research institutes to maintain essential research-related activities during the crisis, and to ramp back up to full research operations once physical distancing measures are lifted. This will cover up to 75 per cent of total eligible costs, and will support activities such as the safe storage of dangerous substances and restarting data sets that were interrupted during the pandemic.
“Research personnel in our universities and health research institutes are significant drivers of science, discovery, and innovation in Canada. By providing these institutions with immediate support, we continue to nurture Canada’s talent pipeline and sustain our innovation capacity, while helping to mitigate the negative impacts of COVID-19 on the research community,” says The Hon. Navdeep Bains, Minister of Innovation, Science and Industry.
This announcement follows a tremendous effort by organizations and individuals across Canada over the course of this pandemic to secure support for hospital-based research. From outreach and meetings to letters and media interviews, many advocacy-based initiatives were undertaken to bring this important issue to the attention of key decision-makers. HealthCareCAN spearheaded these efforts, working tirelessly on behalf of the national health research community.
Lawson is extremely thankful to the federal government for recognizing the critical importance of protecting Canada’s research enterprise and providing urgently-needed financial support. “While we know financial pressure remains, this will help to keep research teams intact while research has been interrupted and provide assistance for when research activities gradually resume,” says Dr. David Hill, Lawson Scientific Director.
A special thank you to local MP Peter Fragiskatos for London North Centre who took up this issue in Ottawa. His strong leadership and representation made the key difference in successfully securing this new funding.
“Tackling the COVID-19 crisis in Canada has required an all-hands on deck approach and Canada’s health researchers have answered the call by suspending all other crucial hospital-based research to meet the challenge,” adds Dr. David Hill. “With this federal support we can now work to ensure that we can maintain other critically needed research on other diseases even as we pursue what promises to be a lengthy battle against COVID-19.”
Background:
- Canadian healthcare-based research is a $3 billion annual sector of the economy and employs 50,000 highly skilled researchers and other staff across the country.
- Health research is one of Canada’s great national achievements and biomedical research conducted in Canada is at the forefront of current essential research and clinical trials around COVID-19.
- This work is fundamental to life in a society and a key driver for progress, innovation and the economy. Canada’s health researchers are global leaders in driving improvements in disease prevention, diagnosis, treatment and care.
- Ontario’s research hospitals have long been the engines of health invention and discovery in provincial and national innovation. From Ottawa, London, Toronto, Kingston, Sudbury and Thunder bay, the more than 20,000 researchers and staff at these hospitals are driven by their passion to improve health.
See also:
- Prime Minister announces support for research staff in Canada – Government news release
- Canada’s health research enterprise welcomes federal support – HealthCareCAN media release
- OHA Media Statement re: Federal Government Supporting Ontario’s Hospital-Based Research Enterprise
Probiotics could improve survival rates in honey bees exposed to pesticide
In a new study from Lawson Health Research Institute (Lawson) and Western University, researchers have shown that probiotics can potentially protect honey bees from the toxic effects of pesticides.
Honey bees are critical to agriculture as they pollinate approximately 35 per cent of the global food crop, contributing an estimated $4.39 billion per year to the Canadian economy. Pesticides are currently used to maximize crop yields, but the most common pesticides, neonicotinoid insecticides, are a major factor in colony collapse disorder which is killing honey bee populations.
“The demise of honey bees would be disastrous for humankind. A current dilemma in agriculture is how to prevent bee decline while mitigating crop losses,” says Dr. Gregor Reid, Director for the Canadian Centre for Human Microbiome and Probiotic Research at Lawson, and Professor at Western’s Schulich School of Medicine & Dentistry. “We wanted to see whether probiotics could counter the toxic effects of pesticides and improve honey bee survival.”
The study was performed by trainees Brendan Daisley and Mark Trinder in Dr. Reid’s lab at St. Joseph’s Hospital in London, Ontario. The researchers utilized fruit flies as a well-known model for studying pesticide toxicity in honey bees. Both insects are affected similarly by neonicotinoids, have very similar immune systems, and share many common microbes present in their microbiota – the collection of microorganisms found in each insect.
The researchers found that fruit flies exposed to one of the world’s most commonly used pesticides, imidacloprid (IMI), experienced changes to their microbiota and were more susceptible to infections. The flies were exposed to a comparable amount of pesticide as honey bees in the field.
By administering a specific strain of probiotic lactobacilli, survival among fruit flies exposed to the pesticide improved significantly. The mechanism involved stimulating the immune system through a pathway that insects use to adapt to infection, heat and other stresses.
“Our study showed that probiotic lactobacilli can improve immunity and potentially help honey bees to live longer after exposure to pesticides,” says Daisley, an MSc candidate. He notes that probiotic lactobacilli could be easily administered through pollen patties, which are used by beekeepers to provide nutritional support and anti-pesticide effects to honey bees.

Above: Brendan Daisley, an MSc candidate at Western's Schulich School of Medicine & Dentistry, working in Dr. Gregor Reid's lab at St. Joseph's Hospital
Over the winter months, honey bee mortality has been steadily increasing with ranges of 38 to 58 per cent in recent years, two to three times higher than the sustainable level. In Ontario alone, 340 bee keepers reported an abnormally high number of bee deaths, with over 70 per cent of dead bees testing positive for neonicotinoid residues (Government of Ontario).
“While cessation of pesticide use would be ideal, farmers currently have little alternative to obtain the yields that keep their businesses viable,” says Dr. Reid. “Until we can cease using pesticides, we need to find ways to protect humans and wildlife against their side effects. Probiotics may prove as an effective protective intervention against colony collapse disorder.”
The researchers hope to further study the mechanisms involved in this process and perform field tests on honey bee populations in Ontario.
The study, “Neonicotinoid-induced pathogen susceptibility is mitigated by Lactobacillus plantarum immune stimulation in a Drosophila melanogaster model”, is published in Nature’s Scientific Reports. The research was funded by the Natural Sciences and Engineering Research Council of Canada (NSERC).

Above: Dr. Gregor Reid, Director for the Canadian Centre for Human Microbiome and Probiotic Research at Lawson, and Professor at Western’s Schulich School of Medicine & Dentistry
Probiotics for respiratory tract infections could save Canada nearly $100 million a year
A recent study suggests the use of probiotics to prevent respiratory tract infections in Canada could result in nearly $100 million per year in savings.
There is growing evidence that probiotics can reduce the risk of respiratory tract infections and lower their frequency, as well as reduce the duration of an infection, antibiotic use and absences from work. Replicating a research model used in France, researchers examined the potential clinical and economic impacts in Canada.
Sponsored by The Alliance for Education on Probiotics, the study included researchers from Lawson Health Research Institute (Lawson), Western University, Laval University and Utrecht University. It incorporated two separate scenarios from two meta-analyses. A meta-analysis combines data from multiple studies using a statistical approach.
Results from the study showed that regular probiotic use could eliminate between 573,000 to 2.3 million days per year of respiratory tract infections, resulting in 330,000 to 500,000 fewer sick days for Canadians and 52,000 to 84,000 fewer antibiotic prescriptions. This would translate to $1.3 to $8.9 million in health system savings. When accounting for productivity losses due to illness, it could save $61.2 to $99.7 million.
Respiratory tract infections are highly contagious infections of the sinus, throat or airways, including influenza or ‘the flu.’ Currently, 5 to 20 per cent of the Canadian population experience at least one respiratory tract infection per year. It’s estimated that respiratory tract infections represent 2.9 per cent of all health care costs in Canada.
“If we could reduce the burden of respiratory tract infections, it would benefit both patients and Canadian taxpayers,” says Dr. Gregor Reid, Director for the Canadian Centre for Human Microbiome and Probiotic Research at Lawson, and Professor at Western’s Schulich School of Medicine & Dentistry.
The research showed that children under the age of 10, individuals living in a community setting (including office work in open spaces) and those not vaccinated against influenza would benefit the most.
Respiratory tract infections are typically viral in nature. Existing treatments rely on symptom control while an estimated 26 per cent of patients are also prescribed antibiotics. These antibiotics are largely unnecessary since antibiotics are not effective against viruses. “Antibiotics are often prescribed even when an infection is likely to be viral. Antibiotics can have serious side effects like destroying many beneficial bacteria in the human body,” says Dr. Reid.
Probiotics are defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host.”
“People are increasingly making probiotics a part of their daily diet or dietary supplements for their proven health benefits,” explains Dr. Reid “The fact that probiotics can also be used to prevent respiratory tract infections makes them even more important.”
Dr. Reid notes that several probiotic products can be effective in preventing respiratory tract infections, as outlined in the Clinical Guide to Probiotic Supplements. These include probiotic yogurts and oral capsules.
The study, “The Clinical and Economic Impact of Probiotics Consumption on Respiratory Tract Infections: Projections for Canada,” is published on PLoS One.

Above: Dr. Gregor Reid (Photo credit: Schulich School of Medicine & Dentistry)
Probiotics to the rescue
As the world’s most important single species of pollinators, honey bees perform many ecosystem functions. They are critical to the global food supply.
Honey bee populations are declining at alarmingly high rates here in Ontario and around the world.
“If the bees disappear, humanity is in big trouble” states Dr. Gregor Reid, Lawson researcher and professor at Western. He is also the leading scientist for the study. “Imagine walking into the grocery store and a third of the food wasn’t there. That is what would happen.”
Pesticide exposure, infection and habitat loss are the main factors suspected to be causing the decline in honey bee populations. Pesticides in particular make infections more severe and exacerbate the consequences of nutritional deficiencies in habitat loss – making those problems even worse.

Since current industrialized agricultural practice rely on pesticides to maintain high crop volume, their complete removal from the equation is not currently feasible.
“We need an alternative solution that interferes with this process where high level of pesticides cause issues like infections and habitat loss to have more severe consequences for the honey bees,” says Dr. Reid. “Supplementing honey bees with probiotic bacteria is that solution, we believe.”
“It may sound overly dramatic to state the research will ‘save the world’s honey bees’, but that is the goal, and other groups around the world are trying to follow this lead.”
The group of researchers from Lawson Health Research Institute and Western University are supplementing honey bees with a nutritional food item containing three carefully chosen strains of beneficial or probiotic bacteria to improve the overall health of the hive and specifically address infection and nutritional needs.

From left: Graduate students Anna Chernyshova, John Antonio Chmiel and Brendan Daisley are working on the honey bee probiotics project with Drs. Gregor Reid and Graham Thompson.
“We are creating what we call a BioPatty. In addition to normal nutrient substances, we infuse it with a select recipe of probiotics,” explains Dr. Graham Thompson, the regional bee expert and professor at Western University who helped set up the field-testing site and manages of the honey bee hives. “Our goal is to make the bees healthier and their immune system more vigorous. This helps them stay efficient and do their important jobs, and not be so vulnerable to the stressors of living in an urban and industrial world.”
The team’s previous scientific findings in a fly model, showed that these bacterial strains could reduce the toxic effects of pesticides and increase resistance towards infection. In May 2018, they moved their research from the lab and into the field thanks to OMAFRA funding, and started to test their BioPatties in a local apiary.
American Foulbrood caused by the pathogen Paenibacillus larvae, attacked the hives. This is one of the most serious honey bee diseases. Infection outbreaks nearly always lead to complete colony collapse and loss of the hive. “But the hives that were given the probiotics were the only ones not to be destroyed, so that was an encouraging early result,” says Brendan Daisley, a PhD student with Dr. Reid who was involved with the development of the research and coordinates sample processing and data collection.
“These results have far-reaching implications as American Foulbrood, despite its geographically-suggestive name, infects honey bees worldwide. It causes a tremendous financial burden to apiary owners and famers alike, who rely on honey bees directly or indirectly as a means of livelihood,” explains Daisley.
The probiotic approach might reduce the need for antibiotics that are so commonly used in many apiaries.
This work is taking place in London, Ontario and the study will continue over the next three years. Going forward, the researchers are planning to work with collaborators in a number of other countries around the world to determine the feasibility of large-scale implementation of probiotics for honey bees.