Search
Search
Researchers looking to better personalize treatment for PTSD
Post-traumatic stress disorder (PTSD) is a condition that often develops in those who have experienced a traumatic event. PTSD affects close to 10 per cent of Canadians, and in some cases, can be difficult to treat.
In a new study through Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from PTSD.
“In our study we are looking at ways of trauma processing at the foundation of the stress response,” explains Dr. Ruth Lanius, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry. “When you are faced with a stressor the first thing you do is turn your attention to it, and when you do that you engage your head and neck muscles.”

DBR was developed by Scottish psychiatrist Dr. Frank Corrigan and focuses on the muscles of the shoulders, neck, head and face of patients when recalling a traumatic event. This form of trauma processing starts right at the moment the stressor is noticed by the individual, which is often quickly followed by a moment of shock. By addressing the stressor at this level, doctors can target the foundation of where the stress response begins.
“When patients bring up a trigger in their mind, we look at what happens in terms of the tension in their head and neck. We process that gently by asking the patient to notice and stay with that tension without trying to release it, and over time the tension usually decreases,” explains Dr. Lanius, who is also a Psychiatrist at London Health Sciences Centre. “The second part involves addressing the shock response. You turn your attention to the stressor and then notice any moments of shock that follows, which is often associated with tension behind the eyes and in the shoulders. Finally, you address the visceral sensations associated with feelings and emotions associated with the stressor.”
Dr. Lanius believes that by using DBR and focusing on muscle and visceral responses, it will help patients suffering from PTSD to process the visceral feelings associated with the trauma and its triggers.

“After this form of treatment, patients often say they feel safer and don’t see themselves negatively, like they did in the past,” says Dr. Lanius. “This is because we change those intense visceral feelings and it allows the person to reevaluate who they are and how they interact with the world.”
The research team is hoping to recruit approximately 60 people to take part in the DBR study. Participants will undergo a psychological interview and an MRI, then eight sessions of treatments. Following those sessions, participants will have another interview and MRI to assess if any positive changes were made within the neurological networks and/or in psychological systems.
“Our hopes are to really personalize treatment for those living with PTSD,” says Dr. Lanius. “Some people have difficulty tolerating some forms of trauma processing and in my experience this treatment is a gentler approach for those individuals.”
Interested participants who have been diagnosed with PTSD can contact Suzy Southwell, Research Coordinator, at 519-685-8500 ext. 35186 or @email.
Researchers receive over $40,000 to study role of personality and resiliency in Veteran mental health
LONDON, ON – The unique and challenging experiences faced by Canadian Armed Forces (CAF) Veterans puts this group at high risk for developing symptoms of mental health disorders, such as Post traumatic stress disorder (PTSD), depression, and anxiety. Researchers at Lawson Health Research Institute (Lawson) have been awarded over $40,000 from Veterans Affairs Canada to study various risk and protective factors associated with mental health disorders in CAF Veterans.
The study aims to learn whether an individual’s personality traits serve as risk or protective factors for Veterans developing mental health problems. The traits that will be examined include openness, agreeableness, emotionality, honesty-humility, conscientiousness, extraversion, and resiliency. For example, someone who is high in openness and resiliency may have a lower risk of developing mental health symptoms.
“Veterans and military members experience uniquely challenging events when compared to the general population,” explains Dr. Rachel Plouffe, study co-lead and Postdoctoral Associate at Lawson. “Past research has identified some risk factors, including history of childhood trauma, age, gender, and education. However, no one to date has investigated the role that personality traits might play in Veterans’ symptoms of mental health conditions.”
The research team will look at the relationship between these personality traits, exposure to stressful experiences during military operations, and mental health outcomes through survey data provided by 500 treatment-seeking and non-treatment seeking Veterans. This information will be used to assess whether the individual’s expression of these personality traits can predict levels of depression, anxiety and PTSD.
They also hope to determine whether the association between combat exposure and PTSD is stronger for those higher in traits such as emotionality, which reflects those who tend to be anxious and fearful. On the other hand, this association will likely be weaker for those higher in more “positive” traits, such as agreeableness, as these individuals tend to be cooperative and forgiving toward others.
Plouffe notes that personalities are not completely stagnant. Certain traits can often change over time, and individuals can work to increase their levels of resiliency.
“Ultimately, our hope is to help improve the ability of CAF members and Veterans to thrive even in the face of great adversity. With the findings from our research, military organizations and mental health treatment centres could use the information from this study to predict which patients may be at greater risk of developing mental health disorders, and provide tailored treatment for these individuals,” she explains.
“This research is needed for military organizations to improve and implement strategies that enhance the well-being of Veterans and active service members,” says Dr. Don Richardson, study co-lead and Director of the MacDonald Franklin OSI Research Centre at Lawson. “Our Veterans give a lot to serve and protect, so it is our duty as researchers and clinicians to find ways that we can better serve them.”
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Researchers receive over $40,000 to study role of personality and resiliency in Veteran mental health
The unique and challenging experiences faced by Canadian Armed Forces (CAF) Veterans puts this group at high risk for developing symptoms of mental health disorders, such as Post traumatic stress disorder (PTSD), depression, and anxiety. Researchers at Lawson Health Research Institute (Lawson) have been awarded over $40,000 from Veterans Affairs Canada to study various risk and protective factors associated with mental health disorders in CAF Veterans.
The study aims to learn whether an individual’s personality traits serve as risk or protective factors for Veterans developing mental health problems. The traits that will be examined include openness, agreeableness, emotionality, honesty-humility, conscientiousness, extraversion, and resiliency. For example, someone who is high in openness and resiliency may have a lower risk of developing mental health symptoms.
“Veterans and military members experience uniquely challenging events when compared to the general population,” explains Dr. Rachel Plouffe, study co-lead and Postdoctoral Associate at Lawson. “Past research has identified some risk factors, including history of childhood trauma, age, gender, and education. However, no one to date has investigated the role that personality traits might play in Veterans’ symptoms of mental health conditions.”
The research team will look at the relationship between these personality traits, exposure to stressful experiences during military operations, and mental health outcomes through survey data provided by 500 treatment-seeking and non-treatment seeking Veterans. This information will be used to assess whether the individual’s expression of these personality traits can predict levels of depression, anxiety and PTSD.
They also hope to determine whether the association between combat exposure and PTSD is stronger for those higher in traits such as emotionality, which reflects those who tend to be anxious and fearful. On the other hand, this association will likely be weaker for those higher in more “positive” traits, such as agreeableness, as these individuals tend to be cooperative and forgiving toward others.
Plouffe notes that personalities are not completely stagnant. Certain traits can often change over time, and individuals can work to increase their levels of resiliency.
“Ultimately, our hope is to help improve the ability of CAF members and Veterans to thrive even in the face of great adversity. With the findings from our research, military organizations and mental health treatment centres could use the information from this study to predict which patients may be at greater risk of developing mental health disorders, and provide tailored treatment for these individuals,” she explains.
“This research is needed for military organizations to improve and implement strategies that enhance the well-being of Veterans and active service members,” says Dr. Don Richardson, study co-lead and Director of the MacDonald Franklin OSI Research Centre at Lawson. “Our Veterans give a lot to serve and protect, so it is our duty as researchers and clinicians to find ways that we can better serve them.”
Researchers seek Canadian health care workers for study on moral distress during COVID-19 pandemic
LONDON, ON - A team from Lawson Health Research Institute is seeking 500 Canadian health care workers to participate in a study on moral distress and psychological wellbeing during the COVID-19 pandemic. Participants will complete online surveys once every three months for a total of 18 months. The goal is to better understand the pandemic’s impact on health care workers in order to minimize moral distress and support wellbeing during future pandemic events.
Moral distress is a form of psychological distress that occurs following an event that conflicts with a person’s moral values or standards. Through previous research with military populations, moral distress has been linked to an increased risk of post-traumatic stress disorder (PTSD) and depression.
“Health care workers are facing unprecedented demands as a result of the pandemic and many may be working under extreme physical and psychological stress,” says Dr. Don Richardson, Lawson Associate Scientist and Director of the MacDonald Franklin Operational Stress Injury (OSI) Research Centre. “Health care workers may face difficult moral-ethical decisions including those around patient care and shortages of personal protective equipment (PPE), which could lead to moral distress.”
The study will consist of a series of surveys to assess moral distress during the pandemic. Participating health care workers will answer questions about moral-ethical dilemmas and symptoms of depression, PTSD, general anxiety, and burnout.
“Moral-ethical dilemmas must be considered in the context of other difficulties faced by health care workers during the pandemic, such as increased workloads, reduced social activities, and evolving work environments and health care delivery models,” explains Dr. Anthony Nazarov, Associate Scientist at Lawson and the MacDonald Franklin OSI Research Centre.
The team hopes that results can be used to cultivate wellness at the outset of future pandemics. This might include guiding emergency preparedness policies and moral-ethical decision-making training modules. They hope that by tracking psychological outcomes over time, they can identify early warning signs of distress that can be targeted with early interventions.
The researchers will also ask questions that explore how the pandemic is impacting health care delivery, such as increased reliance on virtual care appointments, and whether health care workers are satisfied with these changes.
“It is necessary to provide a voice to health care workers during this pandemic,” adds Dr. Richardson. “This is the first study to measure the moral-ethical dilemmas faced in a pandemic and the impacts of such dilemmas on moral distress. It is also the first to measure health care worker perceptions on the virtual migration of patient care.”
This project is in partnership with the Centre of Excellence on PTSD and Related Mental Health Conditions. The focus of the Centre of Excellence is to create knowledge networks across Canada to increase expertise and create the best possible supports and services for Veterans, first responders and their families.
Interested Canadian health care workers can learn more about the study and access the survey at https://participaid.co/studies/bYE4Ob.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Researchers seek Canadian health care workers for study on moral distress during COVID-19 pandemic
Researchers from Lawson Health Research Institute and the Centre of Excellence on PTSD and Related Mental Health Conditions are seeking 500 Canadian health care workers to participate in a study on moral distress and psychological wellbeing during the COVID-19 pandemic. Participants will complete online surveys once every three months for a total of 18 months. The goal is to better understand the pandemic’s impact on health care workers in order to minimize moral distress and support wellbeing during future pandemic events.
Moral distress is a form of psychological distress that occurs following an event that conflicts with a person’s moral values or standards. Through previous research with military populations, moral distress has been linked to an increased risk of post-traumatic stress disorder (PTSD) and depression.
“Health care workers are facing unprecedented demands as a result of the pandemic and many may be working under extreme physical and psychological stress,” says Dr. Don Richardson, Lawson Associate Scientist and Director of the MacDonald Franklin Operational Stress Injury (OSI) Research Centre. “Health care workers may face difficult moral-ethical decisions including those around patient care and shortages of personal protective equipment (PPE), which could lead to moral distress.”
The study will consist of a series of surveys to assess moral distress during the pandemic. Participating health care workers will answer questions about moral-ethical dilemmas and symptoms of depression, PTSD, general anxiety, and burnout.
“Moral-ethical dilemmas must be considered in the context of other difficulties faced by health care workers during the pandemic, such as increased workloads, reduced social activities, and evolving work environments and health care delivery models,” explains Dr. Anthony Nazarov, Associate Scientist at Lawson and the MacDonald Franklin OSI Research Centre.
The team hopes that results can be used to cultivate wellness at the outset of future pandemics. This might include guiding emergency preparedness policies and moral-ethical decision-making training modules. They hope that by tracking psychological outcomes over time, they can identify early warning signs of distress that can be targeted with early interventions.
The researchers will also ask questions that explore how the pandemic is impacting health care delivery, such as increased reliance on virtual care appointments, and whether health care workers are satisfied with these changes.
“It is necessary to provide a voice to health care workers during this pandemic,” adds Dr. Richardson. “This is the first study to measure the moral-ethical dilemmas faced in a pandemic and the impacts of such dilemmas on moral distress. It is also the first to measure health care worker perceptions on the virtual migration of patient care.”
Researchers testing triple intervention to combat dementia
Researchers at Lawson Health Research Institute are the first in the world conducting a clinical trial to test a triple intervention aimed at treating Mild Cognitive Impairment (MCI) and delaying the onset of dementia. The Mobility, Exercise and Cognition (MEC) team will be incorporating physical exercises, cognitive training and vitamin D supplementation to determine the best treatment for improving mobility and cognition.
“We have learned the brain processes involved in motor-control - for example how a person walks - and cognition - for example how that person solves a problem - share similar locations and networks in the brain,” explains Dr. Manuel Montero Odasso, Lawson Scientist and Geriatrician at St. Joseph’s Health Care London. “Problems with mobility are connected to lowering function in the mind, and so can be a good indicator of future progression into dementia.”
Dr. Montero Odasso is also an Associate Professor in the departments of Medicine and Epidemiology and Biostatistics at the Schulich School of Medicine & Dentistry, Western University.

Gait assessment looks at the way in which we move our whole body from one point to another, helping to analyze mobility and the brain processes involved.
MCI is an intermediate stage between the expected cognitive decline of normal aging and the more serious decline of dementia. It can involve problems with memory, language, thinking and judgment. While many older individuals experience decline in both mobility and cognition, each are assessed and treated separately with no specific recommendations available for physicians.
The SYNERGIC Trial will combine physical exercises, cognitive training and vitamin D to test how these interventions work together to improve cognition in older adults at risk for dementia. The trial is targeting cognitive decline at the earliest stage, individuals with MCI, where interventions are more likely to have an effect and can be monitored.

Dr. Manuel Montero Odasso, Lawson Scientist and lead for the SYNERGIC Trial.
Dr. Montero Odasso explains that both physical and cognitive exercises have shown promising effects for maintaining cognition, while vitamin D deficiency is associated with cognitive decline. A key feature of this trial is that participants will receive individualized and progressive training.
“By delaying declines in cognition, we can improve a person’s quality of life. This research will help to support a more comprehensive preventative treatment with clinical guidelines for physicians whose patients are at risk of developing dementia,” states Dr. Montero Odasso. “Even more, each one year delay of progression to dementia in older individuals at risk has the opportunity to save billions of dollars for the Canadian health care system.”
Individuals over 60 years old with mild cognitive impairment without dementia are eligible for this clinical trial. Those interested in participating are encouraged to contact Research Coordinator Alanna Black at 519.685.4292 ext. 42179.
Participants will be asked to complete a routine of exercises and cognitive training three times a week for six months, with one final assessment at 12 months. The main site for the study is Parkwood Institute with physical exercises taking place at the Labatt Health Sciences Building at Western University, in Dr. Kevin Shoemaker’s Laboratory for Brain and Heart Health.
This study has been funded by the Canadian Consortium on Neurodegenerative in Aging (CCNA) which represents Canada-wide research aimed at enhancing the quality of life and services for individuals diagnosed with a neurodegenerative disease. The MEC team in London, led by Dr. Montero Odasso, includes expert researchers in the field of mobility who aim to develop common assessments for the interaction of cognition and mobility for older people to aid as a diagnostic tool for detecting dementia.

Members of the study’s research team, from left to right: Korbin Blue, Research Assistant (Co-op Student); Yanina Sarquis-Adamson, Lab Research Assistant; Frederico Faria, Post-Doctoral Fellow; Dr. Montero Odasso, Director, Gait and Brain Lab; research participant; Alanna Black, Lab Research Coordinator; Stephanie Cullen, Research Assistant (Undergraduate Student); and, Navena Lingum, Research Assistant (Master Student).
Researchers to study inhaled sedatives as solution to COVID-19 drug shortages
A team from Lawson Health Research Institute are being funded by the Government of Ontario’s COVID-19 Rapid Research Fund to study whether inhaled sedatives can replace those that are delivered intravenously in COVID-19 patients requiring ventilation. The multi-centre clinical trial aims to address a global shortage of intravenous (IV) sedatives while improving patient outcomes.
“When COVID-19 patients develop severe respiratory failure and need to be ventilated, they require sedation. While IV sedatives are currently used, there is concern about global drug shortages, particularly if there’s a second wave of COVID-19 in the fall,” explains Dr. Marat Slessarev, Scientist at Lawson and Critical Care Physician at London Health Sciences Centre (LHSC). “Even if we have enough ventilators, we won’t be able to ventilate patients without sedatives.”
The clinical trial, being co-led by Dr. Slessarev and Dr. Angela Jerath at Sunnybrook Health Sciences Centre, will study the replacement of IV sedatives with inhaled sedatives. Inhaled sedatives, also called volatiles, are widely available due to their use in operating rooms to sedate patients during surgery. While they have not been routinely used to sedate patients needing ventilation, early studies suggest they could be safe and even more effective than IV sedatives.
“Preliminary studies in non-COVID patients with severe respiratory failure suggest that inhaled sedatives can reduce lung inflammation, shorten the duration of ventilation and potentially improve survival. Inhaled sedatives could therefore reduce the pandemic’s strain on ventilator capacity while improving patient outcomes,” says Dr. Slessarev. “Since these drugs are safe, cheap and readily available, they can easily be used to address IV sedative shortages if found effective.”
The researchers will recruit approximately 800 patients from across Canada and the United States including patients from LHSC. Each patient will be randomized to receive either IV sedatives or inhaled sedatives. Patient outcomes such as survival and length of ventilation will be compared between the two groups to determine which method of sedation is most effective.
“This is the largest trial of its kind. If inhaled sedatives can shorten the length of ventilation or improve survival in patients with serve respiratory failure, this could cause a paradigm shift in the way we sedate patients in intensive care units (ICUs) around the world,” notes Dr. Slessarev.
Given many survivors of critical illness experience cognitive impairment for months or even years after an intensive care unit (ICU) stay, the team is also planning a sub-study to assess whether one method of sedation results in better cognitive outcomes after treatment.
In addition to funding from the Government of Ontario, the study is being supported with funding from the Canadian Institutes of Health Research (CIHR), London Health Sciences Foundation and Sunnybrook Health Sciences Centre.

Dr. Marat Slessarev, Scientist at Lawson and Critical Care Physician at LHSC
Researchers to study inhaled sedatives as solution to COVID-19 drug shortages
LONDON, ON - A team from Lawson Health Research Institute are being funded by the Government of Ontario’s COVID-19 Rapid Research Fund to study whether inhaled sedatives can replace those that are delivered intravenously in COVID-19 patients requiring ventilation. The multi-centre clinical trial aims to address a global shortage of intravenous (IV) sedatives while improving patient outcomes.
“When COVID-19 patients develop severe respiratory failure and need to be ventilated, they require sedation. While IV sedatives are currently used, there is concern about global drug shortages, particularly if there’s a second wave of COVID-19 in the fall,” explains Dr. Marat Slessarev, Scientist at Lawson and Critical Care Physician at London Health Sciences Centre (LHSC). “Even if we have enough ventilators, we won’t be able to ventilate patients without sedatives.”
The clinical trial, being co-led by Dr. Slessarev and Dr. Angela Jerath at Sunnybrook Health Sciences Centre, will study the replacement of IV sedatives with inhaled sedatives. Inhaled sedatives, also called volatiles, are widely available due to their use in operating rooms to sedate patients during surgery. While they have not been routinely used to sedate patients needing ventilation, early studies suggest they could be safe and even more effective than IV sedatives.
“Preliminary studies in non-COVID patients with severe respiratory failure suggest that inhaled sedatives can reduce lung inflammation, shorten the duration of ventilation and potentially improve survival. Inhaled sedatives could therefore reduce the pandemic’s strain on ventilator capacity while improving patient outcomes,” says Dr. Slessarev. “Since these drugs are safe, cheap and readily available, they can easily be used to address IV sedative shortages if found effective.”
The researchers will recruit approximately 800 patients from across Canada and the United States including patients from LHSC. Each patient will be randomized to receive either IV sedatives or inhaled sedatives. Patient outcomes such as survival and length of ventilation will be compared between the two groups to determine which method of sedation is most effective.
“This is the largest trial of its kind. If inhaled sedatives can shorten the length of ventilation or improve survival in patients with serve respiratory failure, this could cause a paradigm shift in the way we sedate patients in intensive care units (ICUs) around the world,” notes Dr. Slessarev.
Given many survivors of critical illness experience cognitive impairment for months or even years after an intensive care unit (ICU) stay, the team is also planning a sub-study to assess whether one method of sedation results in better cognitive outcomes after treatment.
In addition to funding from the Government of Ontario, the study is being supported with funding from the Canadian Institutes of Health Research (CIHR), London Health Sciences Foundation and Sunnybrook Health Sciences Centre.
-30-
DOWNLOADABLE MEDIA

Dr. Marat Slessarev, Scientist at Lawson Health Research Institute and Critical Care Physician at London Health Sciences Centre (LHSC)
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Researchers unravel two mysteries of COVID-19
LONDON, ONTARIO - A team from Lawson Health Research Institute and Western University has made significant steps forward in understanding COVID-19 through two back-to-back studies published this week in Critical Care Explorations. In one study, the team has identified six molecules that can be used as biomarkers to predict how severely ill a patient will become. In the other study, they are the first to reveal a new mechanism causing blood clots in COVID-19 patients and potential ways to treat them.
The studies were conducted by analyzing blood samples from critically ill patients at London Health Sciences Centre (LHSC). They build on a growing body of work from the team who were first in the world to profile the body’s immune response to the virus by revealing a separate six molecules that could act as potential targets to treat hyperinflammation in critically ill patients.
“We’ve begun answering some of the biggest COVID-19 questions asked by clinicians and health researchers,” says Dr. Douglas Fraser, lead researcher from Lawson and Western’s Schulich School of Medicine & Dentistry, and Critical Care Physician at LHSC. “While the findings need to be validated with larger groups of patients, they could have important implications for treating and studying this disease.”
Predicting which COVID-19 patients will get worse
With no proven therapies, many COVID-19 patients admitted to intensive care units (ICUs) do not survive.
“When a patient is admitted to ICU, we normally wait to see if they are going to get worse before we consider any risky interventions. To improve outcomes, we not only need new therapies but also a way to predict prognosis or which patients are going to get worse,” explains Dr. Fraser.
The researchers identified six molecules of importance (CLM-1, IL12RB1, CD83, FAM3B, IGFR1R and OPTC). They found that these molecules were elevated in COVID-19 patients who would become even more severely ill. They found that when measured on a COVID-19 patient’s first day of ICU admission, the molecules could be used to predict which patients will survive following standard ICU treatment.
“While further research is needed, we’re confident in these biomarkers and suspect these patterns may be present even before ICU admission, such as when a patient first presents to the emergency department,” notes Dr. Fraser. “These findings could be incredibly important in determining how severely ill a patient will become.”
The team measured 1,161 plasma proteins from the blood of 30 participants: 10 COVID-19 patients and 10 patients with other infections admitted to LHSC’s ICU, as well as 10 healthy control participants. Blood was drawn on set days of ICU admission, processed in a lab and then analyzed using statistical methods and artificial intelligence.
The team notes that predicting a patient’s disease severity can help in a number of ways. It could allow for medical teams to have important conversations with family members, setting goals of care based on the patient’s health and personal wishes. Medical teams could use the knowledge to mobilize resources more quickly. If they know a patient is at higher risk of death, they may consider intervening sooner despite associated risks. The team also hopes the findings can be used to better design COVID-19 clinical trials by grouping patients based on their risk. This could allow for stronger results when examining potential treatments for the disease.
Understanding why blood clots occur and how to treat them
A major complication occurring in most critically ill COVID-19 patients is clotting in the lung’s small blood vessels which leads to low oxygen levels in the body.
“The reason for this clotting has been unclear. Most suspect the clotting mechanisms in our blood are put into overdrive and so many clinicians have been treating with anticoagulant therapies like the drug heparin,” says Dr. Fraser. “But we’ve uncovered an entirely different mechanism.”
The team further analyzed the blood samples from their 30 participants, and found evidence to suggest that the inner linings of small blood vessels are becoming damaged and inflamed, making them a welcoming environment for platelets (small blood cells) to stick.
They discovered that COVID-19 patients had elevated levels of three molecules (hyaluronic acid, syndecan-1 and P-selectin.) The first two molecules are products broken down from small hair-like structures (the glycocalyx) which line the inside of the blood vessels. Their presence suggests the glycocalyx is being damaged with its breakdown products sent into the bloodstream. The presence of P-selectin is also significant as this molecule helps to make both platelets and the inner lining of blood vessels adhere to one another.
“The glycocalyx keeps platelets from touching the inside wall of the blood vessel and helps facilitate the production of nitric oxide, which has an important role in preventing platelets from sticking,” explains Dr. Fraser. “We suspect the body’s immune response is producing enzymes that shear off these little hair-like structures, inflaming blood vessels and making them a welcoming environment for platelets to form clots.”
The team suggests that two therapies may hold promise for treating blood clots in COVID-19 patients: platelet inhibitors to stop platelets from sticking and molecules to protect and restore the inner lining of blood vessels.
“By exploring these therapies as potential alternatives to anticoagulant therapies, we may be able to improve patient outcomes,” says Dr. Fraser. “Through our combined findings, we hope to provide tools to predict which patients will become the most severely ill and treatments for both hyperinflammation and blood clots.”
-30-
DOWNLOADABLE MEDIA


Dr. Douglas Fraser, Researcher from Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Researchers using MRI scans to pinpoint moral injury effects in health care workers
Mental health concerns have been on the rise amongst health care workers during this ongoing pandemic. With long hours, fears of the unknown, and the pressure of keeping themselves and their families safe, some health care workers have suffered a moral injury.
Moral injury refers to an injury to an individual’s moral conscious, which can produce profound emotional guilt and shame. Recognizing this is a growing concern, a London research team from Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry is examining moral injury amongst health care workers by imaging the effects on the brain.
“We are trying to look closely at what happens in the brain when a person recalls a moral injury event,” says Dr. Ruth Lanius, Associate Scientist at Lawson and Professor at Schulich Medicine & Dentistry. “By understanding the changes happening in the brain, we may be better able to treat individuals suffering from moral injury.”

Dr. Ruth Lanius, Lawson Associate Scientist/Professor Schulich School of Medicine & Dentistry
During this ongoing pandemic, some health care workers have experienced emotionally difficult situations that resulted in moral injury. “Those suffering from moral injury have a cognitive or thinking component which may include repeated thoughts that they didn’t provide the best care for example, or that they let their family down due to their intense work schedule or need to self-isolated,” explains Dr. Lanius, who is also a psychiatrist at London Health Sciences Centre (LHSC).
“These thoughts are coupled with intense visceral distress, a gnawing sensation in the stomach or the feeling like one is being eaten up inside. I think once we help resolve the visceral distress, we will also see the negative thinking patterns settle down.”
The new study will involve around 60 health care workers. These research participants will undergo a functional MRI scan at St. Joseph's Health Care London at the beginning of the study and have the option to receive eight weeks of treatment. Then, another MRI scan will be done to see if and how the moral injury changes and possibly resolves within the brain. “This can be very validating for the health care workers since brain scans can make the invisible wound of moral injury visible,” adds Dr. Lanius.
The research team’s goal is to better understand what networks of the brain are activated with moral injury. Dr. Lanius hopes this would help establish more neuroscientifically guided treatments. “We have to help our health care workers heal from the tremendous hardships they often endure.”
Health care workers are still being recruited for this study. Interested participants can contact Research Coordinator Suzy Southwell 519-685-8500 ext. 35186 or @email.
Researching treatments for COVID-19
As we continue to live with a COVID-19 pandemic, patients will need good treatment options.
Hospital researchers in London, Ontario, through Lawson Health Research Institute, are testing treatment options for patients who have been hospitalized from a COVID-19 infection, often for severe symptoms.
During the peaks of the COVID-19 pandemic, there were concerns of a global drug shortage when it came to IV sedatives for patients needing ventilation. Through funding from the Government of Ontario’s COVID-19 Rapid Research Fund, a team of Ontario researchers studied whether inhaled sedatives could replace those that are delivered through IV.
“In addition to easing the burden on IV stocks, the inhaled sedatives have additional benefits,” says Dr. Marat Slessarev, a Critical Care Physician at LHSC. “They may reduce inflammation in the lungs and shorten the duration of sedation because they are eliminated from the body faster than IV sedatives.”
Dr. Slessarev, also a Scientist at Lawson, adds that using inhaled sedatives could also be safer for severe COVID-19 patients, who in many cases are on a ventilator for a long time. “When using IV sedatives, they can accumulate and metabolize with accumulation. This can leave the patient with the potential of developing kidney issues because it is hard to dispel them quickly.”

Dr. Marat Slessarev, Critical Care Physican at LHSC and Lawson Scientist
To date, around 800 patients across ten hospital sites have been enrolled in this trial, with the hopes of getting more hospital sites on board as the clinical trials continue.
A majority of people with severe COVID-19 infections in critical care end up developing sepsis, which is a potentially life-threatening condition that occurs when the body's response to an infection damages its own tissues.
“An inflammatory response is what the body uses to fight an infection, but sometimes it is more than necessary and it causes damage to the organs and the body,” explains Dr. Claudio Martin, a Physician in the Intensive Care Unit (ICU) at London Health Sciences Centre (LHSC). “This is why a patient with a severe COVID-19 infection caused by a virus can get sepsis.”
Dr. Martin, who is also an Associate Scientist at Lawson, began studying the use of a human protein called Annexin A5 as a potential treatment for COVID-19 patients with sepsis. “It can work in two ways. The annexin may coat injured cells and reduce the inflammatory response. Or, the injured cells and exposed proteins trigger the clotting mechanism in the body. Those with COVID-19 could get blood clots in the brain and the lungs, and using annexin may improve their outcomes.”

Dr. Claudio Martin, Critical Care Physician at LHSC and Lawson Scientist
Currently, a clinical trial using Annexin A5 on severe COVID-19 patients is underway at LHSC to look at the efficacy of using this human protein.
The COVID-19 virus is also known to cause respiratory failure, prompting Dr. Jim Lewis, Respirologist at St. Joseph’s Health Care London and Scientist at Lawson, to investigate the use of pulmonary surfactant as a potential treatment for these patients.
Bovine Lipid Extract Surfactant Suspension (BLES) is a pulmonary surfactant manufactured in London, Ontario. It’s currently used worldwide to help improve lung function in premature babies. Now, it is being studied with COVID-19 patients experiencing respiratory failure.

Dr. Jim Lewis, Repirologist at St. Joseph's Health Care London and Lawson Scientist
“We know that patients who have injury to their lung and require ventilation have inflammation in the airways of their lungs. Surfactant is a homogeneous layer of lipids and proteins that line the lungs to allow us to breath with minimal effort,” explains Dr. Lewis. “If we gave these patients surfactant as soon as possible after they were put on a mechanical ventilator, it may have some benefit in improving their outcome and getting them off the ventilator sooner.”
Dr. Lewis and his team conducted a clinical trial using pulmonary surfactant with ten critically ill COVID-19 patients and initial results have shown patient safety and efficacy.
Another team of hospital researchers turned to using modified dialysis machines to offer treatment options to those with severe COVID-19 symptoms. Nephrologist at LHSC, Dr. Chris McIntyre, was the first in the world to modify a dialysis device to treat a patient with COVID-19. The device gently removes a patient’s blood, modifies white blood cells, and returns them to fight hyperinflammation.

Dr. Chris McIntyre, Nephrologist at LHSC and Lawson Scientist
“It was quick. We went from the initial idea to the approvals, creating the device and appointing the first patient within 40 days,” says Dr. McIntyre who is also a Scientist at Lawson. “After the first 12 patients, we found that those treated with the device needed significantly less drugs to maintain their blood pressure. We were able to deliver the treatment for all the patients – none of the treatments failed and we had no safety issues.”
Dr. McIntyre is now looking into using this form of therapy for chronic dialysis patients to help modify organ injury.
Responding to the call for action during the COVID-19 pandemic
Quickly after the COVID-19 pandemic began to grip the world, Lawson Health Research Institute responded with action. Lawson is the research arm of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. With hospitals focused on providing excellent patient care in the face of an unknown virus, hospital researchers in London, Ontario began critical COVID-19 studies.
“A lot was unknown during the first wave of the pandemic. Any research that wasn’t essential was put on hold. At the same time, we had people with different expertise coming together with different perspectives to see how we could better understand the SARS-CoV-2 virus and the COVID-19 infection,” explains Dr. David Hill, Lawson Scientific Director and VP, Research at LHSC and. St. Joseph's. “Our hospital researchers formulated ideas and very quickly came up with research proposals. These were fast tracked through our processes and within two months we approved over 50 new studies surrounding COVID-19.”

Dr. David Hill, Lawson Scientific Director and VP, Research at LHSC and. St. Joseph's
Some of these studies were clinical trials, which are research studies performed with people. Many patients from London hospitals get involved as patient participants and when COVID-19 hit, many agreed to be a part of this important research.
“We saw the pandemic happening across the world, and suddenly it was happening here in London. This has probably been the biggest challenge of my career,” says Carol Young-Ritchie, Executive Vice President at LHSC. “We had to look at many of our processes and how we were doing things, and adjust appropriately and nimbly.”
Young-Ritchie adds that as the hospital continued to admit a growing number of COVID-19 patients, a strong focus on research was needed. “It was absolutely critical and important for LHSC as a leader and academic centre to contribute to our collective knowledge. We needed to keep that research going and although it has been challenging, it has also taught us to be innovative.”

Carol Young-Ritchie, Executive Vice President at LHSC
The same focus was happening at St. Joseph’s Health Care London, with health care providers and researchers finding ways to improve care and outcomes for patients who had contracted the virus. “COVID-19 research through the hospital has been incredibly important,” says Karen Perkin, Vice President of Patient Care at St. Joseph’s. “We had researchers busy looking at the impacts of COVID-19. We had patients on ventilators and we were trying to understand that more. We also had research looking at the impacts for staff members looking after patients. All important, helpful knowledge as we move forward.”

Karen Perkin, Vice President of Patient Care at St. Joseph’s
Hospital research in London through Lawson is proudly affiliated with Western University. At Western’s Schulich School of Medicine & Dentistry, the new state-of-the-art Imaging Pathogens for Knowledge Translation (ImPaKT) Facility was the perfect environment to conduct COVID-19 research.
“ImPaKT is a special containment facility where research on viruses like SARS-CoV-2 can be done safely,” says Dr. David Litchfield, Vice Dean of Research and Innovation at Schulich Medicine & Dentistry. “It has become a focal point for dozens of studies involving research through Schulich Medicine & Dentistry, as well as partners from the hospitals and other academic institutions and industries.”

Dr. Litchfield adds that collaboration between hospital partners and scientists has been the key to successful COVID-19 research. “This collaboration has enabled advances leading to new diagnostic testing for COVID-19, as well as studies using MRI or related imaging tools to investigate long-term impacts of the infection on individuals.”
The rapid research response to COVID-19 couldn’t have happened without community and foundation financial support. “Funding support from our hospital Foundation is something we are so grateful for,” says Perkin, referring to St. Joseph’s Health Care Foundation. “They came right out at the beginning and asked how they could help, as did our donors.”
LHSC’s London Health Sciences Foundation and Children’s Health Foundation were also pivotal in research funding during the pandemic. “Funding is a crucial part to how we do hospital research and the Foundations have been important partners in making sure our research continued,” says Young-Ritchie.
As the pandemic continues, so does the research within our community. Hospital research has already improved diagnostics, treatments and patient outcomes related to COVID-19 and helped people all around the world.
“If you look at some of the achievements that have occurred in just a little more than a year, we have had a number of landmark publications on ways to diagnose COVID-19 compared to other respiratory disorders,” notes Dr. Hill. “We have had many rapid advances and it can take a crisis to bring out the best in people. Then things come together quickly, such as expertise, talent and money – and the job gets done.”
Revealing the culprit behind Parkinson’s disease
An estimated 55,000 Canadians are living with Parkinson’s disease. While researchers are advancing therapies to treat symptoms, such as tremors, there is currently no method to stop progression.
To begin addressing this problem, a team of scientists at Lawson Health Research Institute is developing an imaging tracer.
“There’s a protein in the brain called alpha-synuclein (α-syn) that scientists believe is a culprit in causing Parkinson’s disease. The protein forms in ‘clumps’ called Lewy bodies that kill brain cells and potentially lead to disease,” explains Dr. Justin Hicks, Lawson Imaging Scientist. “Unfortunately, we have no way to study it in human brains and this has limited our ability to test therapies against it.”
Efforts have been made to study the elusive protein through modern imaging techniques like positron-emitting tomography (PET). Scientists have attempted to develop a PET probe – a radioactive molecule that targets the specific protein in order to produce highly specific images or scans – but they have been unsuccessful.

Above: Dr. Justin Hicks working in the Nordal Cyclotron & PET Radiochemistry Facility
“Unfortunately, the Lewy bodies caused by α-syn are hard to distinguish from protein clumps found in Alzheimer’s disease and other dementias. This makes it very difficult to know whether a PET probe has found clumps associated with Parkinson’s disease.”
Through a new study, Dr. Hicks and his team are working to find a solution. To do so, they will examine a different but related protein.
“There’s another protein called fatty acid binding protein 3 (FABP3) and one of its roles is to ‘chaperone’ the α-syn protein in human cells. Past studies have shown that levels FABP3 are higher in patients with Parkinson’s disease when compared to healthy controls,” explains Dr. Hicks. “This suggests that high concentrations of FABP3 can be used as an alternate measure of α-syn.”
They hope to measure levels of the FABP3 protein in place of the α-syn protein, and gain a better understanding of the role that both proteins play in the development and progression of Parkinson’s disease. To image Lewy bodies associated with Parkinson’s disease, the researchers are working to produce a PET probe that targets FABP3.
To accomplish this, they will be working in their lab to find a chemical that targets FABP3. Once found, they will attach a radioactive isotope to the chemical and produce a finished tracer. The tracer will then be tested in preclinical models.
Once injected, the PET probe will find and stick to FABP3. The PET isotope will emit a small amount of radioactivity and these emissions will show up as PET images.
“The ultimate goal is to develop a PET probe that can be used to distinguish Parkinson’s disease from other neurodegenerative diseases. The probe could also be used to assess new therapies that reduce levels of the α-syn protein,” says Dr. Hicks. “If successful, we hope this research will lead to a better understanding of the progression of Parkinson’s disease and ways to prevent it.”
Dr. Hicks and his team are being funded for this project through Lawson’s Internal Research Fund (IRF) competition. “Lawson’s IRF is extremely important for early career researchers. It allows us to generate data and publications to then apply for larger external funding. It also permits an added level of risk to pursue projects that may not reach their end goal but often spur new lines of research.”
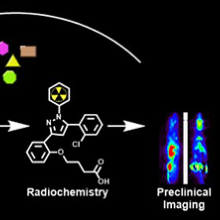
Above: A graphic depiction of this research project and its goals.
Revealing the secrets of dementia
The immune system is one of our greatest defenses against disease and injury. But what happens when it betrays us?
With conditions like rheumatoid arthritis the immune system is manipulated to attack the human body. Inflammation, normally a protective immune response, can be employed to cause symptoms like pain.
Surprisingly, research suggests our immune system may be similarly affected in patients with neurodegenerative dementias.
“We know there are increased numbers of inflammatory cells in the brains of patients with dementia but we don’t know what role they’re playing,” says Dr. Elizabeth Finger, a scientist at Lawson Health Research Institute and neurologist at St. Joseph’s Health Care London’s Parkwood Institute. “Are they doing their proper job of cleaning up damaged cells or is their presence more sinister?”
Dr. Finger’s research group aims to identify and understand changes in the brain that lead to symptoms of dementia, find novel treatments to improve patient quality of life and hopefully prevent the disease altogether. Critical to this work is Dr. Finger’s collaboration with Lawson Imaging scientists Drs. Keith St. Lawrence, Udunna Anazodo, and Justin Hicks.
The researchers utilize Canada’s first hybrid positron emission tomography and magnetic resonance imaging (PET/MRI) machine located at St. Joseph’s Hospital. This high-powered imaging allows them to assess changes to both structure and function in the brains of patients with neurodegenerative dementias like Alzheimer’s disease, frontotemporal dementia and Lewy body dementia.
In one of their many studies they are examining whether there is inflammation in the brains of patients with frontotemporal dementia and, if so, whether this inflammation is present in areas of the brain not yet damaged by the disease.
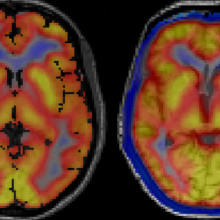
Images captured using a hybrid PET/MRI machine show activated immune cells in the frontal brain regions in a patient with frontotemporal dementia (right) compared to a healthy volunteer (left).
“A presence in those parts of the brain would suggest that inflammation is not playing its normal role of cleaning up damaged cells,” explains Dr. Finger. “It would suggest the brain’s immune response is overactive and that we should consider clinical trials for medications that modulate this response.”
Dr. Finger is an active investigator for novel therapies. In 2019, her group will participate in at least two clinical trials for medications that target genetic mutations that can cause frontotemporal dementia. The studies are phase I trials, which means they are the first time the medications are being tested in humans.
Dr. Finger is also leading a North American multi-centre trial called FOXY. The study will examine the therapeutic potential of a hormone called oxytocin to improve the loss of emotion and empathy that frequently occurs in patients with frontotemporal dementia.
“In the past there were very few treatments for frontotemporal dementia,” explains Dr. Finger. “We are glad to say that Lawson and St. Joseph’s will offer the opportunity to take part in these advances. Words cannot adequately express the appreciation we have for our patients, caregivers and healthy volunteers who participate in research. The time and effort they selflessly donate with the goal of helping future patients is truly inspiring and motivating.”
This story originally appeared in an annual publication from the Alzheimer Society London and Middlesex.
Ricardo Viana
Ricardo Viana, MD, OT
Associate Professor, Schulich School of Medicine and Dentistry
Amputation; Stroke
Dr. Ricardo Viana is a physiatrist at Parkwood Institute and an Associate Professor in the Schulich School of Medicine and Dentistry at Western University. Prior to studying medicine, Dr. Viana was an cccupational therapist. Dr. Viana completed his medical training in 2008 and his Physical Medicine and Rehabilitation residency training in 2013. Dr. Viana’s clinical focus is on Stroke and Amputee rehabilitation as well as neuromuscular and pain medicine.
Dr. Viana has two primary research interests. First, is understanding the impact of dual-task performance on mobility, balance and falls for those with amputation. And second, is systematic reviews in support of the Evidence Based Review Stroke Rehabilitation. Dr. Viana also has a growing interest in education, both medical education and knowledge translation in the clinical setting.