Search
Search
Cutting Edge: Surgical advancement through research
Before the bright lights of the operating room are turned on and the surgeons and operating room staff are gowned and ready, research conducted at Lawson Health Research Institute has backed many of the surgical innovations and firsts performed at London Health Sciences Centre and St. Joseph’s Health Care London.
On October 5, Lawson hosted a Café Scientifique event where a panel of surgeons who are also Lawson scientists discussed their cutting-edge work. Guests had the opportunity to ask questions as part of an open-forum discussion to gain insights from the speakers, and from one another.
In celebration of Canada’s 150th anniversary as a nation, this event was the second of a two-part series focusing on the future vision for health care in Canada and the legacy that research at Lawson will leave. Research and knowledge-creation have been a hallmark of the various surgical areas at LHSC and St. Joseph’s since their inception, and the relationship between innovation and improving patient care has been an enduring trademark. Surgeon scientists have conducted and published research that has changed clinical practice worldwide.
Hand surgery: How small advances turn into complex surgical achievements
Dr. Bing Siang Gan, Lawson scientist, plastic surgeon, Hand and Upper Limb Centre, St. Joseph's

Dr. Gan has a particular research interest in the biology and treatment of Dupuytren's contracture and he uses conventional as well as minimal invasive procedures such as needle aponeurotomy and new collagenase enzyme injections to treat patients.
Dr. Gan explained how a better surgical understanding of Dupuytren's contracture combined with an understanding of the underlying gene factors, DNA, RNA, proteins, receptors, and collagen formation of the condition has led to pharmacological treatment options. The next step will be developing treatment options at every stage of Dupuytren's contracture to keep patients away from the operating room.
Transplant organ preservation: The best option may be “Stinky”
Dr. Alp Sener, Lawson scientist, transplant surgeon, Multi-organ Transplant Program, LHSC

Dr. Sener maintains an active basic sciences and translational research laboratory focusing on gasotransmitter biology and therapeutics. Dr. Sener discussed the need to use “marginal” deceased donor kidneys - those from older donors, younger donors with existing medical issues, and donors post circulatory death – to treat end stage renal disease because due to a lack of donor supply.
Dr. Sener’s laboratory pioneered the use of hydrogen sulphide, a colourless gas with a strong “rotten egg” odor, to prolong organ storage, improve kidney re-perfusion, decrease dangerous inflammatory cells, promote quicker kidney function recovery, greater urine output and improve recipient survival.
Computer-assisted gastrointestinal surgery: Why can’t they see what I see?
Dr. Christopher Schlachta, Lawson scientist, medical director, Canadian Surgical Technologies and Advanced Robotics (CSTAR), LHSC

Dr. Schlachta’s current research interests are focused on development of computer-assisted surgical techniques and technologies to enhance care and training. Dr. Schlachta demonstrated how computer-assisted technologies in the operating room can enhance communication among surgeons and trainees to produce better outcomes for patients. He is currently partnering with industry to commercialize operating room technology he and a team of engineers at CSTAR have developed.
See more photos from this Café Scientifique on Lawson's Facebook page.
Cyclotron hits 10,000-bombardment milestone
Cyclotron staff at St. Joseph’s Health Care London have recorded a 10,000-mark milestone in the same understated way they work every day to improve patient care and cutting-edge research.
No balloons, no streamers, no fanfare: Just an efficient note atop a printout as the bombardment number spun past 9,999 in the early hours of Dec. 31.
“It’s taken us 15 years to get to this point and our work continues to grow,” says Michael Kovacs, PhD, Lead of Lawson’s Nordal Cyclotron & PET Radiochemistry Facility and Leader of the Imaging Research Program at Lawson Research Institute, the innovation arm of St. Joseph’s.
“The numbers are great but the real satisfaction is knowing every single bombardment means something important to a patient or a researcher working towards better patient health.”
St. Joseph’s GE PETtrace cyclotron is a particle accelerator that produces radioisotopes for use in positron emission tomography (PET) scans across Southwestern Ontario, from Windsor to Toronto. It is a vital tool for ultra-precise cancer diagnoses and for advanced research into scores of diseases.
In patient care, each “bombardment” – a grouping of radioisotopes that are then lab-processed, tested and made into smaller batches – can be used to aid cancer scans for as many as 25 people.
“A precise scan can make a dramatic difference, a life-changing difference, in how someone’s cancer is diagnosed and custom-managed,” Kovacs says. “If we think of the PET scanner as the engine of that transformative work, the cyclotron’s radioisotopes are its rocket fuel.”
Isotopes injected into patients are designed to have a short radioactive half-life – between two minutes and 110 minutes – which is another reason St. Joseph’s cyclotron is such an asset for timely care in the region.
“You can’t store or stockpile them. You have to use them almost immediately, so it’s essential to local and area hospital centres to have a ready, reliable source nearby,” Kovacs says.
About half the batched bombardments are used in patients to help with clinical diagnoses that will guide doctors’ treatment decisions.
The other half are used for research trials and pre-clinical research through Lawson, in fields as diverse as oncology, cardiology, neurology, psychiatry, metabolic disease and infectious diseases. In one promising study, for example, they’re being used to image specific brain proteins as researchers explore new disease-modifying treatment pathways for Alzheimer disease.
The next burgeoning field, Kovacs says, is theranostics: the science of diagnosing cancer and precision-attacking it at the same time. “That’s exciting for me, to be able simultaneously to see what we treat and treat what we see.”
About 15 highly specialized staff work at St. Joseph’s cyclotron facility, plus PhD-candidate researchers and other trainees.
Generous donors through St. Joseph’s Health Care Foundation have made much of this advanced research and next-level technology a reality. During the past few years, the Foundation granted nearly $800,000 in donor support to fund extensive renovations to the facility, making it possible to increase production of isotopes and expand life-saving care. Recently, $1 million in donations supported a new PET/CT scanner – the heart of Canada’s first national GE centre of excellence in molecular imaging and theranostics being developed at St. Joseph’s Hospital.
“We know the cyclotron is a critical tool in our imaging work and we are grateful to those donors who stepped up to help us with renovations that enabled the doubling of our facility’s production capability,” says Michelle Campbell, President and CEO of St. Joseph’s Health Care Foundation. “This renovation helps keep St. Joseph’s imaging program at the cutting edge of clinical care.”
The 40-tonne, room-sized cyclotron is more than a machine, and more than the experts who process, test, ship and use the radioisotopes, Kovacs notes.
It’s also testament to the vision of St. Joseph’s long-time chief medical physicist Frank Prato, PhD, and to the support of hospital administrators who saw its need and potential, he adds.
“We are innovators, and our vision is that we’re going to expand St. Joseph’s imaging expertise on an even larger world stage,” Kovacs says.
Dalton L. Wolfe
Dalton L. Wolfe, PhD
Lawson Scientist, Parkwood Institute Research
Implementation Science and Education; Spinal Cord Injury
Dalton Wolfe is a Scientist at Lawson Health Research Institute, an Assistant Professor in the Faculty of Health Science and leads the Research 2 Practice (R2P) team, which is a unique research program within Parkwood Institute that focuses on strategies for generating evidence and implementing best practice within rehabilitation. Professor Wolfe’s primary research interest is in the area of knowledge mobilization and best practice implementation with a focus on physical activity and activity-based therapies in spinal cord injury and brain injury rehabilitation.
Professor Wolf also co-leads the Ontario SCI Implementation, Evaluation and Quality Care Consortium, which focuses on implementation of quality indicators towards the enhancement of care across the 5 academic health centres involved in SCI rehabilitation in Ontario. As part of the Parkwood Rehabilitation Innovations in Mobility Enhancement initiative (PRIME), Professor Wolfe is focused on enhancing clinical decision-making to improve locomotor and other movement-related outcomes with activity-based therapies such as robotic, manual and FES-assisted therapies. As with many of the R2P initiatives this involves implementation science and participatory research methods to put in place practice-based research infrastructure that enables iterative knowledge generation as well as implementation. Trainees work alongside clinicians, administrators and persons with lived experience to tackle clinically relevant questions.

Detecting prostate cancer with a drop of blood and Gulf War technology
London, Ontario - Gulf War technology is making it possible for researchers to detect prostate cancer with a single drop of blood.
Hon Leong, PhD, assistant professor at Western University’s Schulich School of Medicine and Dentistry and scientist at Lawson Health Research Institute, and his team have repurposed a machine once used to detect airborne pathogens in the second Gulf War. The machine is now used for fluid biopsies – a non-invasive way to detect prostate microparticles in the blood in a matter of minutes. Microparticles are essentially garbage released by prostate cells that circulate throughout the bloodstream.
Most men who are more than 40 years old, regardless of their health, have detectable levels of prostate microparticles in their bloodstream. Leong’s research is the first clinical cancer research project to correlate the number of microparticles in the blood to the risk of having prostate cancer – the more microparticles, the higher the risk.
Used in the Gulf War, and more commonly to test water purity, the machine uses flow cytometry to detect microparticles. Flow cytometry measures the specific characteristics of a fluid, such as blood, as it passes through a laser.
Leong’s research provides a more accurate and less invasive testing method for patients suspected of having prostate cancer, and helps to identify patients who are at a higher risk of dying from prostate cancer.
Current methods of detecting prostate cancer, such as the prostate-specific antigen (PSA) test and biopsies, have limitations. PSA tests are based on measuring a specific protein released by the prostate gland, but do not provide a definitive diagnosis. A physical exam and biopsy are needed if PSA levels are elevated. However, even the painful biopsy procedure has a 15 per cent error rate. During biopsies, a painful and invasive procedure, 12 needles are inserted into the rectum, with the hope of extracting material from an area with a tumour.
“Our findings point to a new direction in how we can better identify patients who actually have prostate cancer,” said Leong. “With this test, we can improve the clinical outcomes for patients, reducing costs for unnecessary procedures and reducing errors in diagnosis.”
- 30 -
See all Lawson Media Releases
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Detecting the Undetectable
A simple fall can lead to long-term hand problems such as arthritis due to fracturing the scaphoid bone in the wrist. Scaphoid fractures are known to have the highest rate of healing failures. While this bone’s fragile blood supply is commonly thought to be the main reason for why it is difficult to heal, Dr. Ruby Grewal is looking into a different reason – infection.
Infections are known to cause difficulty in healing bones, but traditional tests for infections in the scaphoid have come up negative. With new advancements in detecting microbial DNA, scientists can now test for ‘clinically undetectable’ infections.

In a new study, Dr. Grewal will use microbial DNA test whether or not there are infections in the scaphoid fracture which causes improper healing of the bone.
“The goal of this study is to use advanced DNA sequencing technology to test whether or not we can detect evidence of microorganisms in non-healing scaphoids,” explains Dr. Grewal, Lawson Scientist and Orthopaedic Surgeon at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London.
Finding new causes of improper healing of the scaphoid bone could improve treatments for individuals with these injuries and prevent long-term problems with hand function. These insights into the causes of improper healing could also prevent young patients from developing wrist arthritis.
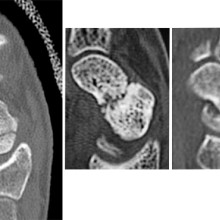
From left to right: Normal scaphoid fracture. Scaphoid fracture that is struggling to heal. Scaphoid non-union where the bone has failed to heal.
Dr. Grewal’s study is being funded through the Lawson Internal Research Fund (IRF).
“The financial support provided by Lawson’s IRF is of utmost importance to researchers. These funds will allow our team to embark on a new area of research and test a novel hypothesis,” says Dr. Grewal, “While traditional granting agencies are reluctant to fund completely novel areas of research without pilot data to prove feasibility, the Lawson IRF allows researchers to investigate new theories in a sound scientific manner. Without the ability to test new ideas we cannot innovate and make advancements in health care. Support for this project allows for that.”
Lawson’s IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
