Search
Search
Study may help explain why breast cancer often spreads to the lungs
A team from Lawson Health Research Institute has shown that triple-negative breast cancer cells can facilitate changes to the lung that both attract cancerous cells and allow them to grow, leading to lung metastasis.
Metastasis is the spread of cancer cells from a primary tumour to different organs. Lung metastasis is responsible for approximately 60 to 70 per cent of deaths related to breast cancer.
“The best way to explain lung metastasis is the seed and soil analogy,” says Dr. Alison Allan, Lawson Scientist. “The seeds are the breast cancer cells from a primary tumour and the soil is the lung’s microenvironment. Seeds can break away, but they only grow if the soil is fertile.”
The majority of studies on metastatic cancer have focused on the characteristics of tumour cells and not on the organs to which they spread. Dr. Allan’s team is studying how the lung microenvironment itself is contributing to lung metastasis.
In the new study, the team examined the lung microenvironment in preclinical models. They compared models with two different subtypes of breast cancer. The luminal A subtype is the least aggressive form of breast cancer and does not often metastasize to the lung. Triple-negative breast cancer, meanwhile, is the most aggressive form with a higher likelihood of metastasis and no targeted therapies available.
The team found that models with triple-negative breast cancer had a drastically different lung microenvironment that was much more hospitable to the growth of cancer. They also found that triple-negative breast cancer cells might be sending ‘signals’ to the lung to help it attract cancerous cells that enter the bloodstream.
“We suspect that triple-negative breast cancer cells release tiny particles called exosomes which are delivered to the lung,” explains Dr. Allan, who is also Chair of the Department of Anatomy and Cell Biology at Western University’s Schulich School of Medicine & Dentistry. “Once delivered, the exosomes signal the lung to start changing into a hospitable environment for tumour cells.”
With support from Lawson’s Internal Research Fund, the team is continuing to research this process. They are also studying ways to make the lungs less receptive to cancerous cells.
Their findings could help in the development of targeted therapies to prevent breast cancer from metastasizing. For example, in collaboration with investigators at the University of Alberta, they are developing an inhalable spray that is aimed at preventing cancer from spreading to and growing in healthy lungs.
“The ultimate goal is to eliminate the metastasis-promoting exosomes as a therapeutic strategy to prevent triple-negative breast cancer from spreading to the lungs,” says Dr. Allan.
The study “Triple-Negative Primary Breast Tumours Induce Supportive Premetastatic Changes in the Extracellular Matrix and Soluble Components of the Lung Microenvironment,” is published in Cancers. It was funded by the Cancer Research Society, the Canadian Cancer Society Research Institute, a London Regional Cancer Program Catalyst Grant, London Health Sciences Foundation, the Breast Cancer Society of Canada and an Ontario Graduate Scholarship awarded to Braeden Medeiros – the paper’s first author.
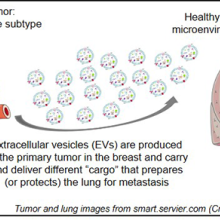
Above: Visual representation of the research findings
The Best in Breast Care Conference
On Oct. 15, 2016, the Breast Care Program of St. Joseph’s Health Care London will be hosting the first annual Best in Breast Care Conference, which will feature leading experts in breast screening, diagnosis, treatment, reconstructive surgery, research, support, and survivorship.
Open to health professionals, students/trainees and the general public, this group learning program meets the certification criteria of the College of Family Physicians of Canada and has been certified by Continuing Professional Development, Schulich School of Medicine & Dentistry for up to 6.25 Mainpro+ credits.
When: Oct. 15, 2016, 8:00 am to 4:00 pm
Where: Best Western Lamplighter Inn, London, ON
Host: Presented by St. Joseph’s Health Care London, Supported by ONERUN
Keynote address: Surgical oncologist Dr. May Lynn Quan, University of Calgary, will present on improving outcomes for young women with breast cancer.
For the full agenda and to register, visit www.sjhc.london.on.ca/breast-care-conference.
Unlocking boundless potential
Ashmeet Gill had her first PET/CT scan shortly after being diagnosed with Hodgkin’s lymphoma, a cancer of the body’s germ-fighting immune system. She was nervous. Claustrophobia is an issue for the young Stratford resident and the scan, necessary to determine if the cancer had spread beyond the lymph nodes in her neck, would take 34 to 45 minutes, she was told.
Wrapped in a sheet and tucked inside the tube of the PET/CT at St. Joseph’s Health Care London (St. Joseph’s), Ashmeet, then 24, steeled herself to remain calm. But near the end of the scan, a sense of panic set in.
“It was not pleasant but I endured it. I made it through.”
Ashmeet’s next PET/CT scan would be six months later, after six cycles of chemotherapy, to determine if the treatment had worked. She was terrified of another panic episode. By then, however, St. Joseph’s had a brand-new PET/CT – Canada’s first, next generation, state-of-the-art Omni Legend PET/CT from GE HealthCare.
This time, Ashmeet’s scan took “barely 15 minutes or so,” she recalled.
“I thought, seriously? I couldn’t believe I was done. I was so happy.”
With the very first patients scanned with St. Joseph’s new PET/CT machine, it was obvious the breakthrough technology was living up to high expectations.
The machine is fast – decreasing the time it took for a scan from about 45 minutes on the older system to less than 14 – head to toe. Patients are exposed to less radiation, and the ability to precisely detect disease and tiny abnormalities is outstanding.
“This is what we have been waiting for,” says Ting-Yim Lee, a pioneer in the use of machines like PET/CT to gather new, vital information about diseases. “St. Joseph’s new Omni Legend by GE HealthCare is answering the call for patients, clinicians and researchers alike.”
PET/CT is the medical ace in imaging for the assessment and treatment monitoring of cancer, neurodegenerative disorders, and metabolic and cardiovascular diseases. At St. Joseph’s, the possibilities of this technology took a giant leap forward in August 2023, thanks in part to the generosity of donors and a $1 million contribution from St. Joseph’s Health Care Foundation. With the arrival of the new system, St. Joseph’s is set to become Canada’s first national GE HealthCare centre of excellence in molecular imaging and theranostics. This two-pronged approach to diagnosing and treating cancers and other diseases merges molecular imaging with the use of radiopharmaceuticals to identify the location and extent of diseased tissues and selectively destroy the abnormal cells.
“The speed at which we can now do exams means significantly improved comfort for patients while the exceptional image quality changes the game in the hunt for cancerous lesions,” explains Ting, Director of PET/CT Research at Lawson Health Research Institute (Lawson) and medical physicist at St. Joseph’s Hospital.
“For young adults undergoing repeat PET/CT exams due to their medical conditions, managing the radiation dose is critical,” explains Dr. Narinder Paul, Lawson scientist and Chief, Medical Imaging, at St. Joseph’s. “These individuals already face an elevated life-time risk of developing cancer from radiation, and this risk further increases with additional exposures.”
For older adults, the time it takes for the examination is also of great concern. Lying still for long periods can be a hardship due to pain from bone metastases or other conditions, and is a challenge for those who have dementia, are claustrophobic or experiencing other issues, adds Dr. Paul.
“Reducing the exam time is a huge improvement in the patient experience for these individuals.”
While patients hail the new PET/CT experience, clinicians and scientists are raving about the machine’s imaging prowess. The advanced AI-driven image formation technology now empowers the precise detection of cancer within lymph nodes and other anatomical structures, “achieving remarkable accuracy even for very small lesions,” says Dr. Paul.
“The advantages we have seen so far are already impressive but what’s on the horizon in research and care – what we will be able to study and do – is even more exciting,” says Ting.
In particular, the new PET/CT is expected to be the catalyst for ground-breaking clinical research for patients facing breast cancer, Alzheimer’s disease, prostate cancer, epilepsy and obesity. Scientific exploration in these areas is currently being planned at St. Joseph’s that will pave the way for novel treatments, new, non-invasive ways to identify a patient’s risk of disease, the potential to clearly and painlessly view how treatment is working, and the ability to uncover the tiniest abnormalities at play when it comes to diseases and conditions.
The deets on PET-CT
Positron emission tomography (PET) is a medical imaging method that uses a small amount of radioactive material, called a radiotracer or radiopharmaceutical, along with a special camera and computer. This helps doctors see how organs and tissues in the body are working. The radiotracer moves through the body and collects in specific areas, showing where there might be a problem or disease. PET can also be used to check how well a patient is responding to treatment.
A computed tomography (CT) scan takes x-ray images of the body from different angles and uses computer processing to create highly detailed, cross-sectional images (slices) of the body’s structures. It is used to see things that regular X-rays can’t show.
A PET-CT machine allows both types of scans to be performed at the same time and information from these two different types of scans to be viewed on a single set of images. Together, PET-CT provides intricate views with fine details about both the body’s various structures and their functions.
Peering into the future
The following are landmark research projects nearing the starting gate at Lawson Health Research Institute made possible by St. Joseph’s Health Care London’s revolutionary new PET-CT machine.
Breast Cancer
Within the Breast Care Program at St. Joseph’s, research with the new PET-CT scanner will make breast cancer theranostics a clinical reality for the first time worldwide. In other words, it will be possible to treat breast cancer using the powerful, one-two punch of molecular imaging and radiopharmaceuticals to identify the location and extent of diseased tissues and selectively destroy the abnormal cells. Two exciting projects are on the horizon:
The one-two punch: Herceptin is a cancer medicine that interferes with the growth and spread of cancer cells in the body. HER2-positive breast cancer is a type of breast cancer that is more aggressive than other types. By using PET-CT imaging with a specialized form of Herceptin that has been chemically tagged, or "labeled," with a radioactive substance, researchers believe it’s possible for a woman to avoid undergoing a breast biopsy. They will be able to see – literally – if the radiolabeled Herceptin binds to the HER2 proteins and the extent of the HER2-positive cancer. Then, by tagging Herceptin with a therapeutic radioisotope – a special type of atom that emits radiation – the hope is to destroy the breast cancer. St. Joseph’s is investigating this approach first in animal studies before progressing into human trials.
Reducing the risk: Not all breast cancers can be effectively treated with Herceptin. For this group of patients, researchers plan to evaluate newer drugs to reduce the risk of both disease progression and death. The new PET-CT scanner will be able to monitor response from these new treatments.
Alzheimer's disease
The super sensitivity of St. Joseph’s new PET-CT will empower innovative methods to identify individuals at risk of Alzheimer’s disease, those who might benefit from treatment, and early response to treatment. The high-powered machine will allow researchers to simultaneously study both blood flow and glucose metabolism in the brain – something that has not been possible before. Both these mechanisms are believed to be contributing factors in the onset of Alzheimer’s. By measuring both at the same time, researchers hope to uncover early signs that the brain is in trouble and at risk of plaque deposits and toxic proteins that have been linked to the development of Alzheimer’s. Patients will be recruited from St. Joseph’s Aging Brain and Memory Clinic at Parkwood Institute for this ground-breaking study.
Epilepsy
Patients with uncontrolled seizures currently require a hospital stay and the implanting of electrodes deep into the brain to record brain signals that pinpoint where the epileptic seizures are originating. The hospital stay is often long as this method relies on the patient having seizures to properly record and identify the location in the brain responsible. Once the problem area is determined, surgeons intricately remove this part of the brain. Research with the new PET-CT will explore a more efficient approach – the ability to precisely reveal the brain’s seizure epicentre using non-invasive imaging looking at characteristics in the epileptic brain that is present between seizures.
Obesity
In Canada, one in four adults are currently living with obesity, a problem that is causing a surge of obesity-related health challenges. Ozempic is a ground-breaking drug that not only helps people shed weight but also slashes the risk of heart disease by an impressive 20 per cent. However, weight loss attributed to this drug is linked to a reduction in lean muscle mass and the long term effects of that muscle loss remain uncertain. Using PET-CT, researchers will explore potential alterations in muscle energy metabolism resulting from obesity treatment with Ozempic and similar drugs.