Search
Search
Dr. Jean Théberge

Ph.D., FCCPM
The NeuroPsychiatry Imaging Lab (NeuroPIL), lead by Dr. Jean Théberge, is a research group dedicated to the development, implementation and application of brain imaging methodologies in psychiatry research.
Publications:
Dr. Théberge is a certified Medical Physicist specialized in magnetic resonance. His current work involves providing support to the clinical MRI programs of St. Joseph’s Health Care and LHSC, teaching MRI at the graduate level in the Medical Biophysics program of the University of Western Ontario and conducting MR imaging research within the Lawson Health Research Institute’s Imaging Division.
With a solid background in physics, significant computer programming skills and knowledge and experience of neuropsychiatry, Dr. Théberge has been able to forge several alliances with clinical collaborators that allow him to conduct a wide range of brain imaging research, methodological developments and applications centered around the theme of neuropsychiatric disorders.
His current research in this area includes investigations of progressive changes in brain chemistry in schizophrenia using magnetic resonance spectroscopy, investigations of brain functional connectivity in major depression in youth as well as in individuals with schizophrenia or post-traumatic stress disorder. Most recently, his group is applying functional MRS methods to the study of glutamate dynamics during the performance of a cognitive task in these disorders.
Dr. Lena Palaniyappan recognized for research using brain imaging to develop treatments for mental illness
Lawson associate scientist Dr. Lena Palaniyappan has won the Canadian College of Neuropsychopharmacology (CCNP)’s 2017 Young Investigator Award for outstanding contributions to the field of neuropsychopharmacology.
The Young Investigator Award is given for basic research or clinical research in alternating years. This year’s award was presented for clinical research. Scientists who have completed their post-doctoral or residency training 10 years ago or less are considered for the award.
Dr. Palaniyappan uses neuroimaging tools to study the processes that operate in the brain when patients experience symptoms of mental illness, including psychosis – repeated voices or visions (hallucinations) and disturbing thoughts (delusions). For many patients, it is not possible to prevent psychosis or reverse the condition fully. Through their research, Dr. Palaniyappan and his team are working to fully characterize the illness and create new treatments.
Recently he led a study that showed it is possible to use information from the brain’s connectivity maps to alter the chemistry of selected brain regions. The hope is that this approach can be used to target precise areas of dysfunction rather than altering the properties of the entire brain to treat psychiatric symptoms.
“Receiving this award highlights the importance of brain imaging in discovering new therapies for brain-based disorders,” says Dr. Palaniyappan. “I feel very inspired looking at the achievements of past recipients as many of them have gone on to change how we think about the brain and mind.”
Dr. Palaniyappan is the medical director of the Prevention and Early Intervention Program for Psychoses (PEPP), a community-focused mental health program located at London Health Sciences Centre (LHSC). He is also an associate professor at Western University’s Schulich School of Medicine & Dentistry.
“With the increasing sophistication of tools to understand the mysteries of the human brain and the world-renowned expertise available in London, there has never been a better time to study psychiatric disorders,” adds Dr. Palaniyappan. “I hope we will soon be able to use brain scans to provide patient-specific information on prognosis and monitor the effects of treatments.”
Dr. Mark Chandy
MD PhD FRCPC
Stem cell biology, induced pluripotent stem cells, cardiovascular disease.
My research employs molecular biology to understand the pathophysiology of cardiovascular disease. Early in my career, I studied the mechanisms of chromatin dynamics, which have broad implications in the influence of the environment in conditions such as diabetes and smoking. I later helped characterize how transcription factors and microRNA direct cardiovascular differentiation and how perturbations of these mechanisms are implicated in cardiovascular disease. My interest in stem cell biology attracted me to Joseph Wu, MD, Ph.D. at Stanford, to learn more about human induced pluripotent stem cell (iPSC) disease modeling endothelial dysfunction.
Advances in next-generation sequencing, bioinformatics, and gene editing make it possible to decipher SNPs contributing to cardiovascular disease and disease-specific transcriptome profiles. More precise diagnostic biomarker-based tests could be developed with a deeper appreciation of an individual’s molecular signature. Additionally, personalized medicine could emerge from iPSC disease and advance precision medicine.
As a recently appointed Assistant Professor at the University of Western Ontario, I am now an independent physician-scientist conducting research using iPSC disease modeling that I developed at Stanford University. My research focuses on cardiovascular disease modeling to 1) investigate the effects of the environment on the vasculature, 2) discover biomarkers to risk stratify cardiovascular disease, and 3) discover druggable target genes for cardiovascular disease. The overarching goal of my research is to use iPSCs to understand mechanisms underlying the relationship between inherited factors and how environmental stress, such as diabetes, e-cigarettes, and marijuana, sensitize an individual to exacerbated cardiovascular disease. The discovery of these gene and environment interactions will facilitate the identification of high-risk individuals who could benefit from therapy that alters disease trajectory. In the future, iPSC disease modeling could guide the discovery of sm! all molec ule agonists or inhibitors that could be used as personalized medical therapy for cardiovascular disease.
Aleksandra Leligdowicz
Dr. Neil Gelman
PhD
- Improving diagnosis and monitoring therapy for breast cancer
- Tracking cells labelled by reporter gene-based methods
| 2000 - present | Scientist, Imaging, Lawson Health Research Institute |
| 1997-2000 | Assistant Staff Investigator, Department of Neurology, Henry Ford Hospital, Detroit, MI, USA |
| 1996-1997 | Post-Doctoral Fellow, Medical Imaging, Henry Ford Hospital, Detroit, MI, USA |
| 1995 | Post-Doctoral Fellow, Medial Biophysics, University of Toronto |
| 1994 | Ph.D. Physics, University of Toronto |
Dr. Blayne Welk

MD, MSc
Dr. Welk obtained his Bachelors of Science degree and Medical Degree at the University of Western Ontario. He then went on to complete his urology residency at the University of British Columbia and obtained his Royal College certification in Urology. He completed additional clinical training at the University of Toronto, where he specialized in the evaluation and treatment of male and female incontinence, male urethral stricture disease, and neurogenic bladder dysfunction. During his 2-year fellowship he also completed a masters degree in Clinical Epidemiology at the University of Toronto.
In 2011 he was appointed as an Assistant Professor in the Department’s of Surgery (Urology) and Epidemiology and Biostatistics at Western University. He is an Adjunct Scientist at the Institute for Clinical Evaluative Sciences. He has received peer-reviewed grants from the Canadian Urologic Association, Academic Medical Organization of Southwestern Ontario, PSI Foundation, Rick Hansen Foundation and Ontario Neurotrauma Foundation.
Dr. Raymond Kao awarded John McCrae Memorial Medal by Canadian Medical Association
Captain (Navy) Dr. Raymond Kao, a Lawson associate scientist, has been awarded the 2017 John McCrae Memorial Medal by the Canadian Medical Association (CMA).
Dr. Kao has served in various military units as a Medical Officer since 1991 and has been a member of the Canadian Armed Forces since 1977. He has served in Africa and the Middle East. In 2013, Dr. Kao was named Canada’s first Chair in Military Critical Care Research. A major focus of his research has been on improving military trauma care and developing treatments that can be brought to the battle field.
The John McCrae Memorial Medal from the CMA recognizes clinical health services personnel of the Canadian Forces who perform exemplary service and demonstrate compassion, self-sacrifice or innovation beyond the call of duty to benefit the health or welfare of fellow military personnel or civilian populations.
“Receiving this honour is very humbling because one does not achieve anything without the help of others. My work would not be possible without the support of and collaboration with other researchers. This award represents the efforts of all the military physicians and surgeons, nurses, medical technicians, allied health care providers and physicians’ assistants on my deployments who have worked to provide excellent care,” says Dr. Kao, who is also the senior critical care advisor to the Surgeon General, a critical care physician at London Health Sciences Centre (LHSC), and an Associate Professor in the Department of Medicine at Western University’s Schulich School of Medicine & Dentistry.
In 2014, Dr. Kao was part of a military medical team sent to Sierra Leone to help combat the Ebola epidemic. He provided care to affected health care workers and studied prognostic factors to help improve care in future epidemics.
He is currently studying the use of C-Peptide to improve organ dysfunction after traumatic hemorrhagic shock caused by blunt or penetrating trauma. Hemorrhagic shock is treated with fluid resuscitation, or fluid replacement, which can also put stress on the organs. His recent studies have shown that C-Peptide, an insulin connecting protein, has the potential to reduce gut injury and lung inflammation from hemorrhagic shock and fluid resuscitation.
Dr. Kao is also widely recognized for his research on erythropoietin, a hormone produced by the kidneys that stimulates the production of red blood cells and, in turn, haemoglobin. He found that when combined with saline, erythropoietin can improve blood flow and tissue oxygen usage after an injury. Erythropoietin can easily be administered through a syringe and can be used to help stabilize wounded soldiers in the battlefield.
Dr. Ting-Yim Lee awarded the Meritorious Service Cross by the Governor General of Canada
Congratulations to Dr. Ting-Yim Lee who was awarded the Meritorious Service Cross from the Governor General of Canada. He was recognized for his development of CT Perfusion to measure blood flow in the body which has transformed the way stroke is assessed and treated around the globe.
The Civil Division Cross recognizes a deed or an activity that has been performed in an outstandingly professional manner, or with uncommonly high standards; the activity is often innovative, sets an example for others to follow, improves the quality of life of a community and brings considerable benefit or honour to Canada.
Dr. Lee, a scientist at Lawson Health Research Institute and Medical Physicist at St. Joseph’s Health Care London, as well as professor at Western University’s Schulich School of Medicine & Dentistry and scientist at Robarts Research Institute, fits the bill perfectly. Through his research program, Dr. Lee pioneered the development of CT Perfusion technology which is compatible with existing CT scanners and uses X-ray dye to assist doctors in assessing blood flow in the event of stroke.
The technology is now in use in more than 8,000 hospital imaging departments worldwide and has drastically improved patient care.
“I am humbled by this award. The work I’ve accomplished would not have been possible without the support of the institutions and collaboration of colleagues too many to name and the tireless effort of all members of my lab: graduate students, fellows, technicians and assistants,” said Dr. Lee. “I am really happy that this work has been found to help patient care. It gives me impetus to continue to search for new innovations that would benefit patients.”
The Meritorious Service Decorations recognize Canadians for exceptional deeds that bring honour to the country. The cross was originally created in 1984 by Her Majesty Queen Elizabeth II, for members of the military. In 1991, both the cross and medal were introduced for civilians to recognize remarkable contributions in many different fields including advocacy initiatives and health care services, to research and humanitarian efforts.
The recipients of the awards were announced by Governor General of Canada, David Johnston, and will be presented at an official ceremony later this year.
Dr. Ting-Yim Lee recognized by WORLDiscoveries for medical imaging innovation
An exceptional career of innovation prowess, influence and leadership has won Dr. Ting-Yim Lee the inaugural Career Achievement Award presented by WorldDiscoveries.
Dr. Lee, Director of PET/CT Research at Lawson Health Research Institute and Medical Physicist at St. Joseph’s Health Care London, is being recognized for the significance of his work in the field of medical imaging and outstanding success in turning innovative ideas into tangible products and services.
Each year, WORLDiscoveries, the technology transfer and business development office for Western University, Lawson, and Robarts Research Institute, hosts the Vanguard Awards. These prestigious awards honour the community’s brightest minds, visionary entrepreneurs, and the exceptional achievements they have made in technology and research. By partnering with WORLDiscoveries, recipients of the Vanguard Awards have reached significant market-readiness milestones, propelling their ideas toward real-world impact. All recipients have made remarkable strides in their respective fields, shaping the future of innovation.
Dr. Lee pioneered use of advanced methods to analyze medical images from machines like CT, MRI and PET to gather important information about diseases. Over the years, he has published 290 research papers, which have been cited nearly 19,000 times – an indication of their impact in the medical community.
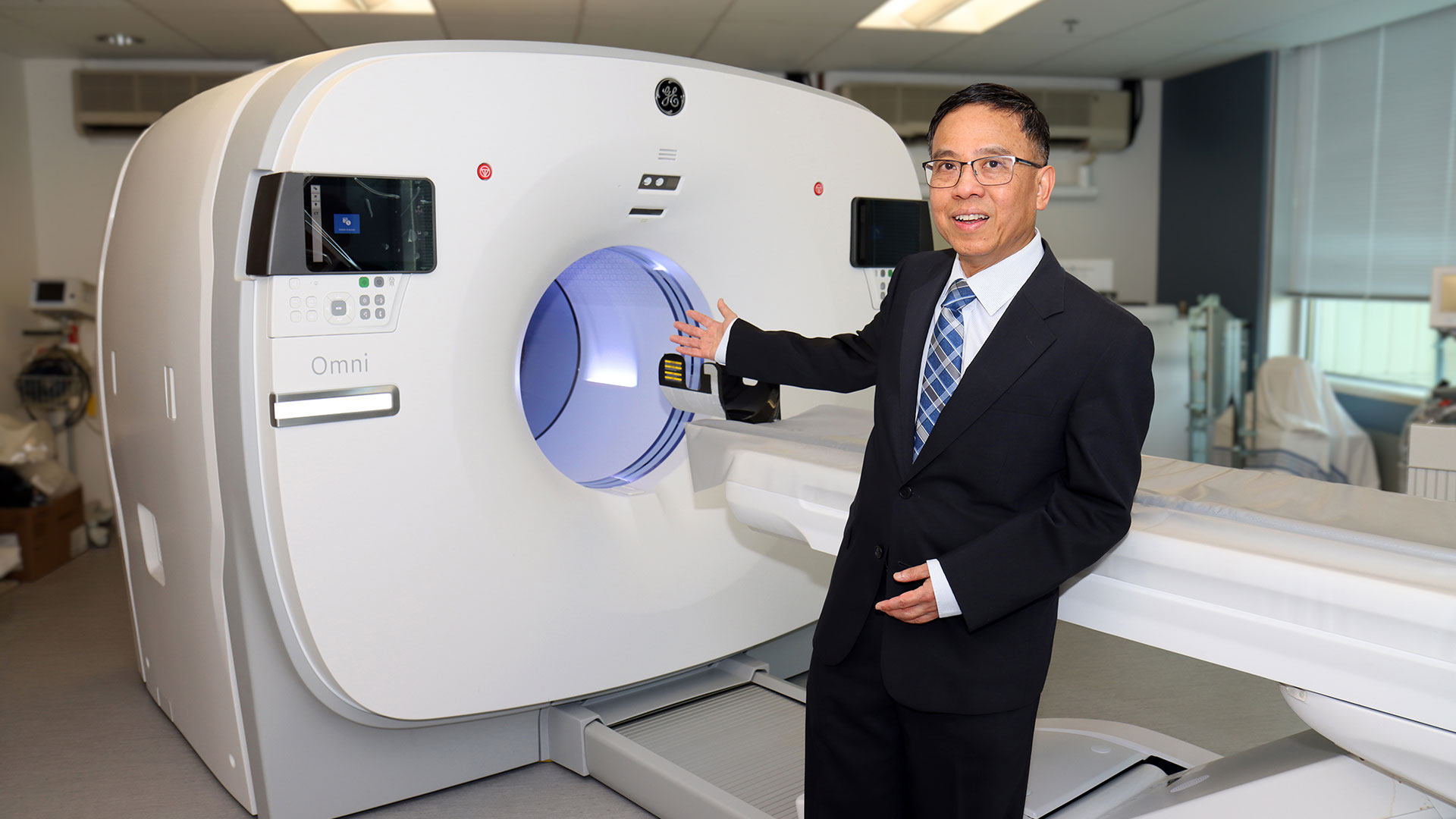
His work initially focused on using dynamic CT scans to study blood flow in stroke and cancer patients and to address challenges related to imaging the heart. With dynamic CT scans, images are taken continuously as change in vessels, organs and other structures is happening. The effect is similar to a real-time video. Dr. Lee also played a role in developing guidelines for using these scans to study the growth of new blood vessels that nourish the proliferation of cancer cells.
More recently, he shifted his focus to PET scans to examine biological processes in the body, demonstrating their effectiveness in detecting prostate cancer in a short, 22-minute scan. One of his notable contributions was the development of CT Perfusion software, which played a crucial role in a U.S. nation-wide ovarian cancer trial involving more than 20 medical centres. This software proved valuable as an early biomarker for assessing treatment response.
In addition to research, this world-renowned researcher has obtained eight patents and has licensed five enhanced versions of the CT Perfusion software to GE HealthCare, making it easier for clinicians to apply his techniques in real-world hospital settings.
Dedicated to creating the next generation of scientists, Dr. Lee has mentored and trained 70 graduate students, post-doctoral fellows, clinicians and research associates, many of them going on to earn prestigious research awards themselves.
“I am grateful for the support received over the decades from colleagues and trainees,” says Dr. Lee. “Without them, the work cannot be done. This award is not just for myself but for all collaborators and contributors on this journey.”
In presenting the award, WORLDiscoveries says Dr. Lee’s work has transformed industries, inspired countless individuals within the field to pursue innovation and entrepreneurship, and has left a lasting impact on society at large.
St. Joseph’s congratulates this remarkable and dedicated scientist on this prestigious and well-deserved award.
More on the Vanguard Awards and the 2023 recipients are available on the WORLDiscoveries website.
Dr. Vladimir Hachinski receives Canadian Medical Association’s highest honour
World-renowned brain researcher, Dr. Vladimir Hachinski, is named as this year’s recipient of the Canadian Medical Association’s (CMA) F.N.G. Starr Award for his contributions in stroke research and patient care. This prestigious award is the highest available to CMA members and is intended to recognize outstanding and inspiring lifetime achievement.
Dr. Hachinski, Lawson Scientist and Neurologist at London Health Sciences Centre is the co-founder of the world’s first successful stroke unit. Two earlier centres in the United States were deemed unsuccessful and eventually closed. Dr. Hachinski and his colleague, Dr. John W. Norris, applied their knowledge and fresh perspectives, and opened a stroke centre at Sunnybrook Hospital, Toronto, in 1975.
“We had a tremendous team of volunteer nurses, physiotherapists and other professionals who were very keen to have an impact,” explains Dr. Hachinski. “We implemented the A, B, C, protocol which focused on Accurate diagnosis, Balance and homeostasis in the patient’s physiology, and avoiding Complication. Dr. Josephine Somerville pioneered early rehabilitation in the stroke unit.”
At the time, stroke was still commonly misunderstood in medicine, until Dr. Hachinski coined the term “brain attack” in 1993, describing the similarities in urgency of strokes and heart attacks.
Realizing the success of their protocols on stroke patients, Dr. Hachinski and his colleagues also noticed improved outcomes for dementia rates in the stroke patients they saw. There is still no treatment for dementia, however they were confident they could delay onset through similar stroke prevention and treatment protocols.
After several studies on both animal models and humans, Dr. David Cechetto from Western University and Dr. Hachinski discovered that the region of the brain, known as the insula, is involved in regulating the parasympathetic and sympathetic nervous systems - evidence that there is an important connection in how the brain impacts the heart.
Today there are several stroke centres operating in Ontario. “We were able to prove that our model was successful at improving the lives of stroke patients, so the government facilitated the opening of these centres across the province. We can now say that we have improved outcomes not just for individuals, but at a population level, where public health policy has its true impact,” says Dr. Hachinski.
Currently Dr. Hachinski and his team are seeking funding for a nation-wide study to examine stroke and dementia outcomes across the country, including how several environmental factors play a role in the development of stroke and dementia with the aim of preventing both. “Since this research is multi-disciplinary, it is challenging to find a funding agency as most of them tend to invest in very specific fields of research,” he explains. “We are hopeful that someone will recognize the importance of this research, and we will be able to move forward with our study.”
“I am extremely appreciative and proud to be recognized with the F.N.G. Starr Award, however I am just the face of this honour. Behind me stands an amazing team. I feel that my greatest strength is to recognize and work with talent.”
Drug combats underlying causes of Alzheimer-related dementia
A “game-changing” new drug offers both hope and time to some people diagnosed with Alzheimer’s disease, says the head of a St. Joseph’s program that played a key role in the medication’s clinical trials. Health Canada has newly approved lecanemab (brand name Leqembi, developed by Eisai Co. and Biogen), which has been shown to slow progression of Alzheimer’s disease in people with mild symptoms.
St. Joseph’s Health Care London, and its innovation arm at Lawson Research Institute, has played a key role as one of multiple sites that have trialed the drug.
“This is game-changing,” says Dr. Michael Borrie, medical director of the Aging Brain and Memory Clinic at St. Joseph’s, whose work in dementia research and clinical practice spans more than three decades.
“We’ve been working for over 20 years to find a compound that is disease-modifying. This is the first approved drug in Canada that addresses the underlying pathology of Alzheimer’s, not just the symptoms.”
Lecanemab works by removing amyloid proteins that accumulate as sticky clumps in the brain and are associated with cognitive decline in people with Alzheimer’s. “It reverses one aspect of the disease by removing the plaque from the brain ,” Borrie explains.
“You can characterize its benefit in terms of time saved. If you were to have this medication for four years, you can ‘save’ one year of cognitive decline. It totally changes the course of their neurodegeneration in a way we haven’t seen before.”
Lecanemab was one of many clinical drug trials assigned to research coordinator Kayla Vander Ploeg when she arrived to work at St. Joseph’s more than a decade ago. “For so long, we had hope that one of these medications would benefit patients long-term. Now we have more than hope. We have results,” Vander Ploeg says.
“Today I’m seeing people who say, ‘my dad or my mom was in this study, and now there’s hope for me.’ ”
There are specific eligibility criteria, including confirmed diagnosis – through cognitive testing and through advanced brain imaging and biomarker tests – plus screening to rule out two gene variations that couldresult in more side effects.
Canada is now one of 51 countries to have approved lecanemab.
Borrie cautioned that Health Canada approval doesn’t necessarily translate to funding coverage. It’s not yet determined who will pay for the medication, or how: when lecanemab was approved in the United States in 2023, the annual cost per patient was more than $26,000.
The length of time from drug development to trials to approval illustrates how painstaking pharmaceutical research can be. But it also highlights how integrating health research into hospital settings can translate more quickly into improved patient care.


