Search
Search
Exemplary leadership earns Ting-Yim Lee medical physics Gold Medal
Medical physicist Ting-Yim Lee still isn’t sure exactly what interviewers saw in him when they recruited him in 1988 to work in radiology research at St. Joseph’s Health Care London.
But he’s honoured they saw and cultivated that kernel of possibility.
Lee is now recognized as an innovative imaging scientist transforming research and patient care. In June, Lee will receive the Canadian Organization of Medical Physicists’ (COMP) Gold Medal Award for exemplary achievement. It is the organization’s most prestigious award.
“I was hired from Winnipeg to work here,” he says. “I had a thin CV, and very few publications. I was a nobody, I thought. But St. Joseph’s recognizes the potential in people and they saw potential in me. If not for St. Joseph’s nurturing environment, our imaging program would not be what it is today.”
Lee is director of PET/CT Research at Lawson Research Institute (Lawson) and medical physicist at St. Joseph’s Hospital. He is also a professor at Western University’s Schulich School of Medicine & Dentistry and a scientist at Robarts Research Institute.
At St. Joseph’s and Lawson, he has sparked the growth of the Molecular Imaging and Theranostics program. Recently it was chosen to be Canada’s first a GE Centre of Excellence in Molecular Imaging and Theranostics based on the past track record of the Lawson Imaging program of achieving a number of national and global firsts.
Mustard-seed growth
Lee says the Lawson Imaging Program’s development is symbolized by the mustard seed in the St. Joseph’s logo: “The mustard seed is the smallest of seeds and it grows into a strong and beautiful tree. When I started at St. Joseph’s, we’d installed a CT scanner one year earlier, and we were quite behind other hospitals. Then we started developing it bit by bit, piece by piece, leaf by leaf.”
Among his most celebrated achievements is developing CT Perfusion technology, a world-first in 2000 that has revolutionized stroke diagnosis and treatment by providing detailed images of blood flow in and to the brain.
The technology is used in more than 8,000 hospitals worldwide and more than 25,000 licences of the technology have been sold over the last 22 years– the royalties enabling the purchase of new, state-of-the-art CT and PET/CT equipment at St. Joseph’s to the benefit of researchers and patients alike.
Lee’s contribution helped secure a $30-million Canada Foundation for Innovation initiative in 2006, introducing hybrid imaging to Canada—including the nation’s first PET/MRI systems. His
expertise has turned contrast-enhanced CT into a powerful functional imaging tool with applications to oncology, cardiology, and neurology.
Excellence, multiplied
“It is no exaggeration to state that without Dr. Lee, the Lawson Imaging Research Program and the medical physics team would never have achieved the heights of success that it has,” says Frank Prato, PhD, founder of the program in 1982 and its leader until 2024.
Prato says Lee has had “a profound influence” on the careers of hundreds of medical physicists, including training and mentoring 60 graduate and postdoctoral students – many of whom are now training students of their own.
“These multipliers/amplifiers of Dr. Lee’s mentorship have had a profound effect on the excellence of the medical physicists we have in Canada and the excellence of the ones we train for the world,” Prato says.
Lee has published 290 research papers, which have been cited nearly 19,000 times – an indication of their impact in the medical community. He has been awarded the Meritorious Service Cross from the Governor General of Canada and received the Career Achievement Award as a WORLDiscoveries innovator.
The St. Joseph’s difference
More recently, Lee created, in partnership with St. Joseph’s Health Care Foundation and Western, two endowed chairs to research and translate liquid radiation therapy.
His considerable accomplishments are matched by his humility and his eagerness to deflect credit to his colleagues, St. Joseph’s, the St. Joseph’s Health Care Foundation and the broader imaging and research communities.
Excellent technology and research are an outgrowth of the people and culture of St. Joseph’s, Lee emphasizes. “I always feel that when I walk into St. Joseph’s, it immediately has that warm feeling that envelops you. It’s different. It’s a nurturing environment.”
The COMP Gold Medal is the highest award given by the Canadian Organization of Medical Physicists and is given to currently active or retired individuals to recognize medical physicists who have made outstanding contributions:
- A body of work fundamentally altering the knowledge base and practice of medical physics
- Leadership positions in medical physics organizations leading to improvements in the status and public image of medical physicists in Canada
- Significant influence on the professional development of the careers of medical physicists in Canada through educational activities or mentorship
Several London and Lawson-affiliated researchers have won the COMP Gold Medal, including Prato in 2024.
This year’s annual scientific meeting takes place in London on June 4 – 7.
Expanded No Fixed Address strategy houses half of those in danger of homelessness
At a community symposium on health care and homelessness attended by over 250 Londoners, a research team from Lawson Health Research Institute announced the results of a nine-month, federally funded project tackling the issue of homelessness from within hospital walls.
The No Fixed Address (NFA) strategy reaches and supports patients during the crucial transitional period when they are being discharged from the hospital and re-integrated into the community. The approach was initially tested with strong success for mental health patients across the city and the second ‘version’ of the project was extended to medical units at London Health Sciences Centre’s University Hospital and Victoria Hospital.

“Many of our patients with lived experience of homelessness were saying that their journey started with a hospital discharge,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and NFA project lead. “They were often experiencing major transitions in their lives and then experienced a hospital stay. Normally a relatively short visit, they aren’t able to gather the information and make a plan to be able to leave the hospital with somewhere to stay.”
Through partnerships between service providers and non-profit organizations, the NFA strategy helps prevent homelessness by providing timely and accessible supports to patients who would otherwise be discharged into homelessness. Staff from the Canadian Mental Health Association Middlesex, Salvation Army’s Housing Stability Bank, and Ontario Works in the City of London provided direct, on-site patient access to housing and income support databases
“Lawson’s No Fixed Address research project is the first evaluation anywhere of a strategy that aims to reduce the number of hospital patients being discharged into homelessness,” says Dr. Forchuk.
Over nine months, 74 people experiencing medical health issues accessed the NFA program. Of those, 54 per cent were also experiencing mental health challenges.
All of the study participants were in imminent danger of homelessness. Through the supports provided as part of this research study, half were able to arrange housing before being discharged.
“We were able to help a lot of people, with 50 per cent successfully securing housing,” shares Dr. Forchuk. “With the results and feedback we received, we learned a lot about how we can make the program even better.”
They found that there is a need for the supports to be extended as a transitional program in the community post-discharge, as the length of stay in the medical units tended to be short.
The project’s previous phase, involving acute and tertiary psychiatric care in the London region, prevented homelessness in 95 per cent of cases. “Going into the medical units, we found that people have highly complex needs that often involved mental health challenges.
By simply using the same approach that we did for those in psychiatric care, we helped half of the people find housing. To best serve the needs of everyone, we want to follow them after discharge.”
The team sees a solution in having a housing support worker provide transitional, wrap-around services that follow the person. They would continue to meet and work together after the hospital stay, helping to access community programs.
“This role would be embedded in both the health care system and the homeless serving system, supporting individuals who have complex physical and mental health issues as they are also navigating homeless resources.”
This project is funded by the Government of Canada's Homelessness Partnering Strategy’s (HPS) Innovative Solutions to Homelessness funding stream.
Overview and Numbers
Fast facts on homelessness and health care
- Stable housing after discharge is associated with higher quality of life, reduced substance abuse and fewer hospital admissions.
- Homeless clients are four times more likely to be readmitted to hospital within a month compared to low-income matched controls.
- Hospital care for homeless clients costs an average of $2,559 more per client.
- Finding appropriate housing or avoiding a potential eviction takes time – it is important to start as soon as possible during the discharge process.
Implementation of first phases of No Fixed Address
- Access on the unit to a housing advocate and income support staff.
- The initial intervention was accessed by 219 acute psychiatric clients, as well as 32 clients within a specialized tertiary care psychiatric hospital - only 3 became or remained homeless.
- Expanded to be an immediate wrap-around service with offices set up in the hospital mental health units.
- Staff from the Canadian Mental Health Association Middlesex (CMHA), Ontario Works (OW), and Salvation Army’s Housing Stability Bank (HSB) have on-site access to housing and income support databases.
- Clients can access service by drop-in or appointment.
- Services include assistance for finding housing, financial assistance, such as rent/utilities in arrears or first/last months’ rent for a new home, and access to high quality used furnishings, household supplies and a cleaning service.
Expanded second phase of No Fixed Address
- Program ran from July 2018 to March 2019 (9 months).
- 74 people accessed the program.
- Complex situations with both mental health and physical problems: 100% had medical issues and 54% had mental health issues.
- Lengths of stay were very short.
- People could not attend drop-in due to medical issues, so they relied on referral from staff.
- Although they were all in imminent danger of homelessness, 38 people (50%) were housed as a result of this program.
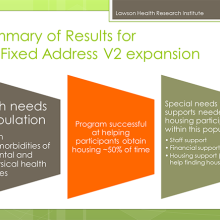
What were the main housing needs?
- Help finding a place to live
- Money for deposit
- Financial support
- Transportation support
- Help getting benefits
Recommendations and learnings for future models
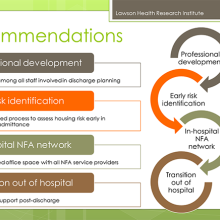
- Housing support worker needs to be a transitional support since work will be needed after discharge.
- Social work not the only key players (patient care facilitators, nursing staff, etc.).
- The transitional housing support role needs to be well embedded in the homeless serving system, as well as health care.
- People have physical and mental health issues and are also going to be navigating homeless resources.
- Despite the low success rate, many people were housed who would have otherwise been discharged to homelessness.
- We learned a lot about what was needed in an area where there was a knowledge vacuum.
- Future plans involve implementation with improvements to the model.
Exploring mobile software to better support youth mental health
Mental health services are rooted in relationships. When it comes to delivery, and specifically community-based and outpatient services, connection and communication between the individual and care provider need to be the focus.
When we think of youth in particular, technology is a regular form of communication for them.
“Our research team at Lawson is looking at how technology can assist in the delivery of mental health services for youth in a way that still supports the important components of treatment,” says Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson. “In our work with youth, they’ve talked about wanting the technology they are already using integrated into their care.”
In the health care sector, the use of technology needs to be carefully tested and implemented, to ensure it is not only meeting the needs of those using it but also that it complies with the standards for privacy and security.
On February 7, 2019, Lawson Health Research Institute and InputHealth welcomed community members and stakeholders for the announcement of a new health care technology solution that is being researched by Dr. Forchuk and her team, with generous contributions from the provincial government.
TELEPROM-Y is a mobile-based TELEMedicine and Patient-Reported Outcome Measurement Youth study aiming to improve access to specialized services and reduce inpatient mental health admissions for youth. The initiative is one of 11 that received funding from Ontario’s second round of the Health Technologies Fund (HTF), a program of the Ontario Ministry of Health and Long-Term Care administered by Ontario Centres of Excellence.
TELEPROM-Y received $395,109 in provincial funding with $494,630 in matching contributions for a total investment of $889,739.
InputHealth’s CEO Damon Ramsay and Chief Medical Officer Puneet Seth, along with Jennifer Moles from the Ontario Centres of Excellence were on hand with Dr. Cheryl Forchuk to hear more about how the technology and funding will help support youth. Project contributors Woodstock General Hospital and Youth Opportunities Unlimited (Y.O.U.) also attended the announcement.
This project is taking a unique approach to creating connections with youth. Researchers will use an electronic Collaborative Health Record (CHR) developed by InputHealth, an innovative Canadian digital health software company, which allows for secure communication. Patients will have access to virtual visits, prompts and reminders, text or email messages, and educational materials delivered by phone.

InputHealth's Puneet Seth and Damon Ramsay provided a demonstration of the software being used in the study.
Dr. Forchuk explains that “the study is focusing on an important transitional period. The majority of mental illnesses occur between the ages of 16 to 25 years old.” The research team is recruiting participants between these ages who have symptoms of anxiety and/or depression, and are receiving outpatient services from a hospital-based mental health care program at London Health Sciences Centre, St. Joseph’s Health Care London and Woodstock General Hospital, or community-based services from partner organizations.
A key aspect is to assess whether the technology is effective and efficient, while acceptable to both the staff and youth using the app.
“Careful evaluation is essential to make sure we are doing the right things for the people we serve,” adds Dr. Forchuk, who is also the Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery.
The mobile software will also be evaluated on its ability to improve the ease of access to care; monitor mood and behaviour changes for earlier intervention; enhance information exchange between patient and health care provider; and, support the overall experience for the youth.
Other project contributors include St. Michael’s Hospital Centre for Excellence in Economic Analysis Research, The Forge (McMaster University), Thunder Bay Regional Health Sciences Centre and Western University.
The study extends previous findings from the Youth Mental Health Engagement Network study (Y-MHEN), which developed, delivered and evaluated an interactive web-based personal health record, the Lawson SMART Record (LSR), to assist mental health patients in managing their care and connecting with care providers.
The Health Technologies Fund is a program of the Ontario Ministry of Health and Long-term Care and is administered by the Ontario Centres of Excellence. Program supports the development of made in Ontario health technologies by accelerating evaluating, procurement, adoption and diffusion within the Ontario health system.
