Search
Search
Revealing the secrets of dementia
The immune system is one of our greatest defenses against disease and injury. But what happens when it betrays us?
With conditions like rheumatoid arthritis the immune system is manipulated to attack the human body. Inflammation, normally a protective immune response, can be employed to cause symptoms like pain.
Surprisingly, research suggests our immune system may be similarly affected in patients with neurodegenerative dementias.
“We know there are increased numbers of inflammatory cells in the brains of patients with dementia but we don’t know what role they’re playing,” says Dr. Elizabeth Finger, a scientist at Lawson Health Research Institute and neurologist at St. Joseph’s Health Care London’s Parkwood Institute. “Are they doing their proper job of cleaning up damaged cells or is their presence more sinister?”
Dr. Finger’s research group aims to identify and understand changes in the brain that lead to symptoms of dementia, find novel treatments to improve patient quality of life and hopefully prevent the disease altogether. Critical to this work is Dr. Finger’s collaboration with Lawson Imaging scientists Drs. Keith St. Lawrence, Udunna Anazodo, and Justin Hicks.
The researchers utilize Canada’s first hybrid positron emission tomography and magnetic resonance imaging (PET/MRI) machine located at St. Joseph’s Hospital. This high-powered imaging allows them to assess changes to both structure and function in the brains of patients with neurodegenerative dementias like Alzheimer’s disease, frontotemporal dementia and Lewy body dementia.
In one of their many studies they are examining whether there is inflammation in the brains of patients with frontotemporal dementia and, if so, whether this inflammation is present in areas of the brain not yet damaged by the disease.
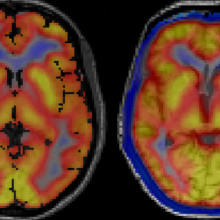
Images captured using a hybrid PET/MRI machine show activated immune cells in the frontal brain regions in a patient with frontotemporal dementia (right) compared to a healthy volunteer (left).
“A presence in those parts of the brain would suggest that inflammation is not playing its normal role of cleaning up damaged cells,” explains Dr. Finger. “It would suggest the brain’s immune response is overactive and that we should consider clinical trials for medications that modulate this response.”
Dr. Finger is an active investigator for novel therapies. In 2019, her group will participate in at least two clinical trials for medications that target genetic mutations that can cause frontotemporal dementia. The studies are phase I trials, which means they are the first time the medications are being tested in humans.
Dr. Finger is also leading a North American multi-centre trial called FOXY. The study will examine the therapeutic potential of a hormone called oxytocin to improve the loss of emotion and empathy that frequently occurs in patients with frontotemporal dementia.
“In the past there were very few treatments for frontotemporal dementia,” explains Dr. Finger. “We are glad to say that Lawson and St. Joseph’s will offer the opportunity to take part in these advances. Words cannot adequately express the appreciation we have for our patients, caregivers and healthy volunteers who participate in research. The time and effort they selflessly donate with the goal of helping future patients is truly inspiring and motivating.”
This story originally appeared in an annual publication from the Alzheimer Society London and Middlesex.
Revolutionizing rehab
St. Joseph’s Health Care London is taking giant strides in the science of rehabilitation and movement, with direct benefit to patients.
St. Joseph’s is setting a long-time vision into motion.
“Five years ago, we had a vision of leveraging our long history and expertise in providing innovative rehabilitation treatments to improve the lives of people with mobility needs on a larger scale,” says Roy Butler, President and CEO of St. Joseph’s Health Care London (St. Joseph’s). “That dream has come to life.”
While experts at St. Joseph’s had the knowledge, innovative spirit and passion to achieve the vision, they needed a partner who shared the same enthusiasm.
William and Lynn Gray answered that call. With their generosity and ground-breaking investment, The Gray Centre for Mobility and Activity was created.
“Lynne and I are very pleased with the steady forward advancement of the centre’s mission since its establishment just a few short years ago,” says Bill Gray. “The innovative thinking and idea generation that seeks new solutions to the issue of mobility have really taken root. We hoped that The Gray Centre would have an impact on care ... and it has.”
“We’ve watched the development of The Gray Centre with enormous pride and are pleased to have our name associated with it, and the excellence it stands for,” adds Lynne Gray.
A unique concept
Established in 2020, The Gray Centre at St. Joseph’s Parkwood Institute is a regional hub focused on researching leading-edge treatments and interventions in mobility and activity. The centre’s unique model of linking research and care allows researchers to work side-by-side with clinicians, patients, and caregivers to uncover optimal methods for maintaining mobility throughout a person’s life.
“Scientists at The Gray Centre are leading the way in integrating technology and solutions in care to better understand how we can enhance each patient’s treatment plan to improve their functionality and ability to move,” says Butler.
Pioneering Research
More than 50 ongoing rehabilitation research projects at Parkwood Institute are exploring areas such as spinal cord and traumatic brain injury rehabilitation, pain, outcomes for amputees, virtual exercise and cognitive behavioral therapy, gait analysis as a measure of dementia progression, and stroke rehabilitation and recovery.
The Gray Centre is a catalyst and connector for these projects by investing in cutting-edge technology, providing seed grants, embedding researchers from Western University, leveraging clinical expertise, attracting world-class researchers and translating new knowledge into clinical practice by training students and clinicians, and fostering sustainable practice change.
More than $1.3 million granted through St. Joseph’s Health Care Foundation has advanced work at The Gray Centre over the past year. From researcher support to new equipment such as two transcranial magnetic stimulators, a portable handheld ultrasound and several sensored mats for gait assessment donors have stepped up to advance this work.
Leadership with Purpose
At the helm of The Gray Centre is Siobhan Schabrun, PhD, a world-renowned neuroscientist and the inaugural William and Lynne Gray Research Chair in Mobility and Activity. Thanks to a partnership with Western University’s Faculty of Health Sciences and Schulich School of Medicine & Dentistry, donor funding for the chair made through St. Joseph’s Health Care Foundation was matched, creating a $5-million endowed position.
Schabrun’s innovative research benefits people suffering from chronic pain. With a focus on non-invasive brain stimulation techniques to enhance neuroplasticity and improve mobility and activity outcomes, she and her team are, in essence, retraining the brain’s pain response. This innovative work bridges the gap between neuroscience and rehabilitation, offering new hope for individuals with musculoskeletal and neurological conditions.
Originally trained as a physiotherapist with a PhD in neuroscience from the University of Adelaide in Australia, Schabrun has attracted more than $15 million in competitive research funding and written or contributed to more than 140 scholarly publications.
FLOATing Forwards
The newest advancement is a first-in-Canada and a marvel of medical engineering that is transforming options in rehabilitation research and practice.
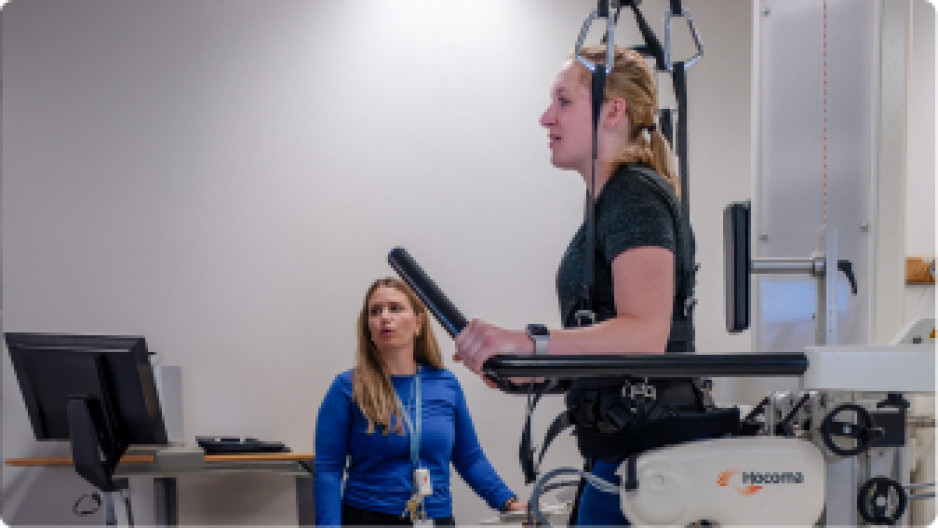
The Reha-Stim Medtec FLOAT system at St. Joseph’s Parkwood Institute enables patients with mobility limitations to walk, supported, without fear of falling. They "float" in a controlled environment using a combination of robotics, body-weight support and real-time feedback. The device has a harness attached to a robotic arm, which adjusts the level of support based on the patient's movements. Sensors provide continuous feedback for maximum learning and greatest benefit to physical therapists and patients alike. The FLOAT system has shown significant improvements in patients' mobility, balance and overall functional independence.
“Innovative equipment like the new FLOAT System is an example of the type of innovation that does not exist anywhere else in Canada,” says Bill Gray. “The real-life application of technologies like this are what The Gray Centre is intended to be about.”
Through the combined efforts of dedicated professionals, cutting-edge technology and philanthropist partners, St. Joseph’s Gray Centre has combined vision with passion and is transforming lives, one step at a time.
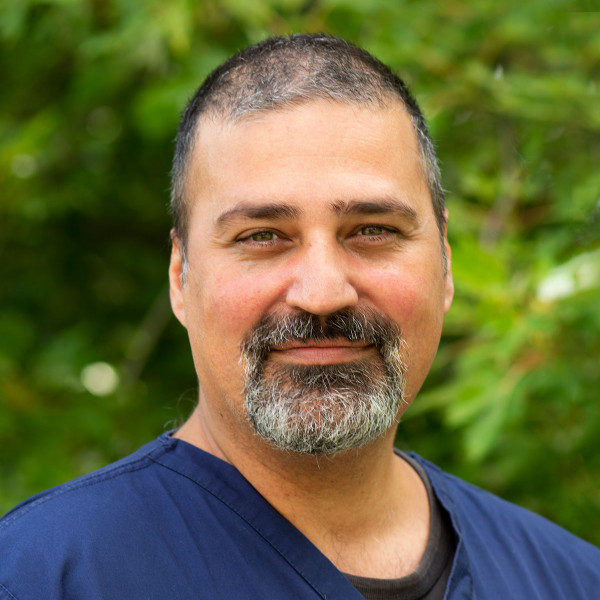
Ricardo Viana
Ricardo Viana, MD, OT
Associate Professor, Schulich School of Medicine and Dentistry
Amputation; Stroke
Dr. Ricardo Viana is a physiatrist at Parkwood Institute and an Associate Professor in the Schulich School of Medicine and Dentistry at Western University. Prior to studying medicine, Dr. Viana was an cccupational therapist. Dr. Viana completed his medical training in 2008 and his Physical Medicine and Rehabilitation residency training in 2013. Dr. Viana’s clinical focus is on Stroke and Amputee rehabilitation as well as neuromuscular and pain medicine.
Dr. Viana has two primary research interests. First, is understanding the impact of dual-task performance on mobility, balance and falls for those with amputation. And second, is systematic reviews in support of the Evidence Based Review Stroke Rehabilitation. Dr. Viana also has a growing interest in education, both medical education and knowledge translation in the clinical setting.
Running Against Ruptures
This event is raising funds for brain aneurysms research.
Did you know, ruptured brain aneurysms account for 3–5% of all new strokes?
How about that women, more than men, suffer from brain aneurysms at a ratio of 3:2?
It is a devastating medical issue many Canadians face.
You are invited to Running Against Ruptures on June 23, 2019 at Greenway Park in London, ON
Running Against Ruptures is committed to raising funds for patients and families affected by brain aneurysms so people can get the help they need earlier and with better results. By conducting research, we can help alleviate the pain many families encounter due to brain aneurysms.
However, each of these projects requires funding. That’s why Running Against Ruptures looks to raise money to support these life-saving research projects.
For more information, please visit the London Health Sciences Foundation.