Search
Search
Expert available to comment on COVID-19 in older adults
As the COVID-19 pandemic continues, data is showing that while illness and mortality occur across the lifespan, the death rate increases significantly for those over 65 years of age.
Dr. Manuel Montero-Odasso, Professor at Western University’s Schulich School of Medicine & Dentistry and Scientist at Lawson Health Research Institute is the co-chair of the Canadian Geriatrics Society COVID-19 Working Group. He is available to media for comment on the allocation of health care resources for older adults, and also on recommendations specific to this population to help prevent transmission.
“Particularly for older adults, they need to know that they are the most vulnerable but that there is no need to panic. They should follow evidence-based recommendations if they become sick. Importantly, we also stress the role of caregivers and family members, and we have specific recommendations for them on how to connect with their loved ones,” he said.
Dr. Montero-Odasso has also co-authored a position statement on behalf of the Canadian Geriatrics Society arguing that it is not acceptable to ration critical care admission or life-saving ventilation solely on the basis of age, as has been seen in other epicentres of COVID-19 when health care resource become scarce. They point out that while an established body of evidence supports that mechanical ventilation would likely be futile in some frail older adults with multiple comorbidities, there is a critical ethical difference between decisions made on the basis of futility versus those based on age alone.
“It is a concern not only because of ageism, but because it’s important to understand that age is not the only variable. It is also key to understand previous wishes of patients. You could have a 30-year-old with a chronic neurodegenerative condition who doesn’t want to be intubated and also an 80-year-old who has a high functionality and quality-of-life who does want to use all means possible to survive,” he said. “Age itself should not be the main driver of these decisions; important variables include previous functional capabilities, and levels of frailty. There needs to be a very thoughtful and thorough evaluation.”
Dr. Montero-Odasso says one example of how the COVID-19 Working Group has been involved in policy decisions is related to feedback on the Ontario Health Association Clinical Triage Protocol for Major Surge in COVID Pandemic.
“This important Ontario document does not use age alone in their recommendations and, moreover, it recommends to use proper geriatric tools, such as the Clinical Frailty Scale, in their triage algorithms to guide resources allocation,” he said.
Since COVID-19 was declared a pandemic, the first evidence that emerged was that the older adult population was being hit the hardest. As part of the Canadian Geriatrics Society COVID-19 Working Group, Dr. Montero-Odasso and colleagues have created resources and recommendations such as global recommendations for older adults, evidence-based position statements on ageism and healthcare resource utilization, and how to support health care workers on the front lines, such as the doctors and nurses in healthcare facilities.
Commentary reflects the perspective and scholarly interest of Western faculty members and is not an articulation of official university policy on issues being addressed.
-30-
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Fecal transplants show promise in improving melanoma treatment
LONDON, ON – In a world-first clinical trial published in the journal Nature Medicine, a multi-centre study from Lawson Health Research Institute, the Centre hospitalier de l’Université de Montréal (CHUM) and the Jewish General Hospital (JGH) has found fecal microbiota transplants (FMT) from healthy donors are safe and show promise in improving response to immunotherapy in patients with advanced melanoma.
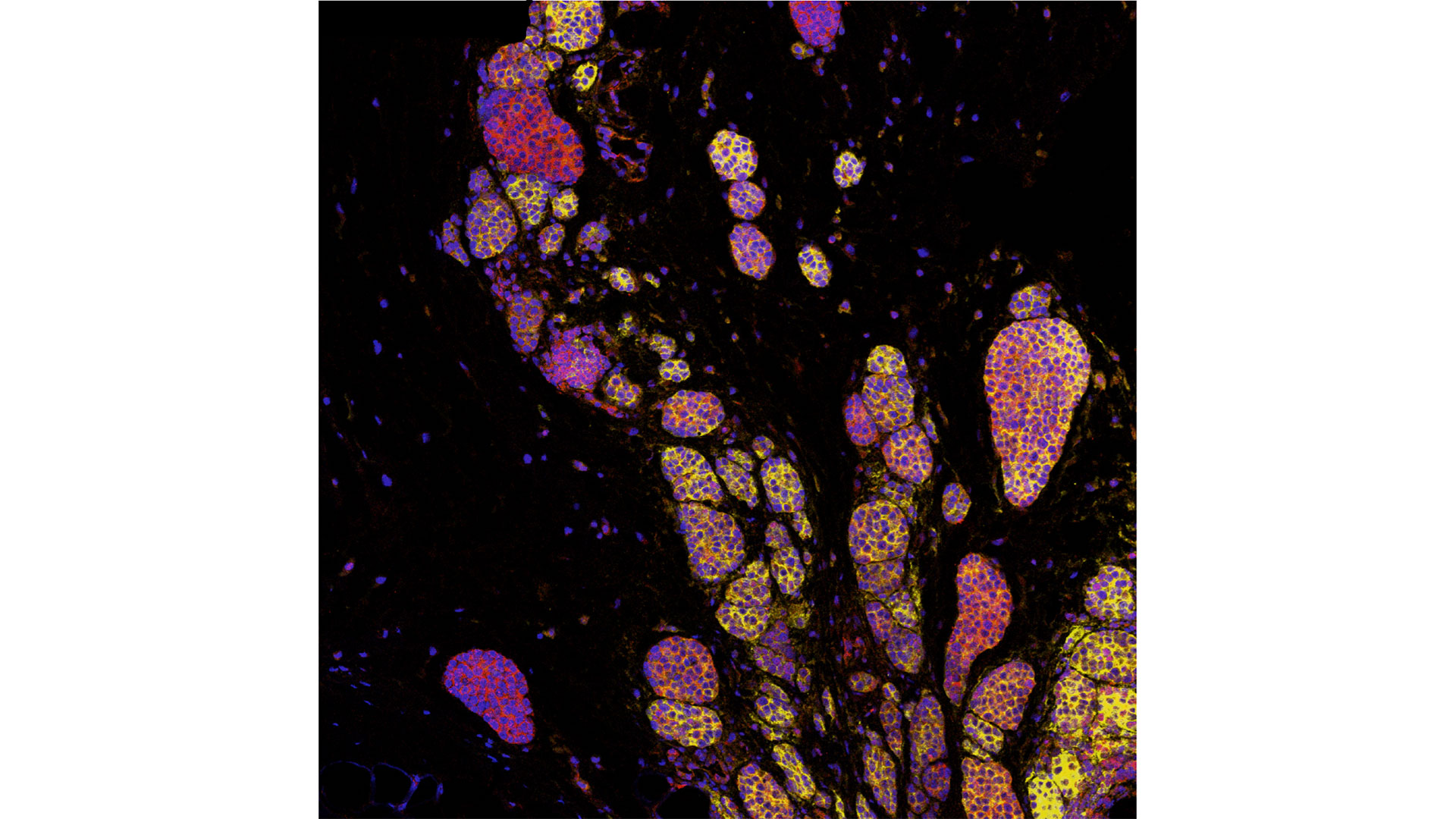
Immunotherapy drugs stimulate a person’s immune system to attack and destroy cancer. While they can significantly improve survival outcomes in those with melanoma, they are only effective in 40 to 50 per cent of patients. Preliminary research has suggested that the human microbiome – the diverse collection of microbes in our body – may play a role in whether or not a patient responds.
“In this study, we aimed to improve melanoma patients’ response to immunotherapy by improving the health of their microbiome through fecal transplants,” says Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Associate Scientist at Lawson and Associate Professor in the Department of Oncology at Western University’s Schulich School of Medicine & Dentistry.
A fecal transplant involves collecting stool from a healthy donor, screening and preparing it in a lab, and transplanting it to the patient. The goal is to transplant the donor’s microbiome so that healthy bacteria will prosper in the patient’s gut.
“The connection between the microbiome, the immune system and cancer treatment is a growing field in science,” explains Dr. Saman Maleki, Scientist at Lawson and LHSC’s LRCP, Assistant Professor in Schulich Medicine’s Departments of Oncology, Pathology and Laboratory Medicine, and Medical Biophysics, and senior investigator on the study. “This study aimed to harness microbes to improve outcomes for patients with melanoma.”
The phase I trial included 20 melanoma patients recruited from LHSC, CHUM and JGH. Patients were administered approximately 40 fecal transplant capsules orally during a single session, one week before they started immunotherapy treatment.
The study found that combining fecal transplants with immunotherapy is safe for patients – which is the primary objective of a phase I trial (also called ‘safety trials’). The study also found 65 per cent of patients who retained the donors’ microbiome had a clinical response to the combination treatment. Five patients experienced adverse events sometimes associated with immunotherapy and had their treatment discontinued.
“We have reached a plateau in treating melanoma with immunotherapy, but the microbiome has the potential to be a paradigm shift,” says Dr. Bertrand Routy, Oncologist and Director of CHUM’s Microbiome Center. “This study puts Canada at the forefront of microbiome research by showing we can safely improve patients’ response to immunotherapy through fecal transplants.”
“These exciting results add to a rapidly growing list of publications suggesting that targeting the microbiome may provide a major advance in the use of immunotherapy for our patients with cancer,” adds Dr. Wilson H. Miller Jr. of the JGH and Professor in the Departments of Medicine and Oncology at McGill University.
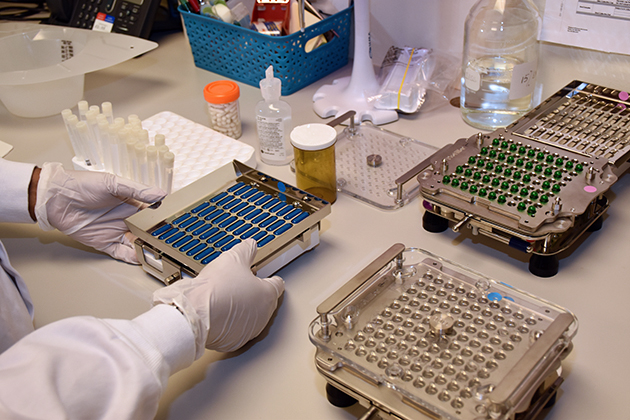
The study is unique due to its administration of fecal transplants (from healthy donors) in capsule form to cancer patients – a technique pioneered in London by Dr. Michael Silverman, Lawson Scientist, Chair of Infectious Diseases at Schulich Medicine and Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London.
“Our group has been doing fecal transplants for 20 years, initially finding success treating C. difficile infections. This has enabled us to refine our methods and provide an exceptionally high rate of the donor microbes surviving in the recipient’s gut with just a single dose,” says Dr. Silverman. “Our data suggests at least some of the success we are seeing in melanoma patients is related to the efficacy of the capsules."
The team has already started a larger phase II trial involving centres in Ontario and Quebec. Lawson researchers are also studying the potential of fecal transplants in the treatment of other cancers, including renal cell carcinoma, pancreatic cancer and lung cancer, as well as HIV and rheumatoid arthritis.
This research is supported in part through donor funding from London Health Sciences Foundation, Western University, the Lotte and John Hecht Memorial Foundation, the JGH Foundation, Canadian Cancer Society’s Impact Grant program and The Terry Fox Foundation.
-30-
ADDITIONAL DOWNLOADABLE MEDIA

About the CRCHUM
The CHUM Research Centre (CRCHUM) is one of North America’s leading hospital research centres. It strives to improve the health of adults through a continuum of research spanning disciplines such as basic science, clinical research and population health. More than 2,150 people work at the CRCHUM, including nearly 500 researchers and nearly 650 students and postdoctoral fellows. crchum.com
About the Jewish General Hospital
Part of the Integrated Health and Social Services University Network for West-Central Montreal (CIUSSS), the Jewish General Hospital has served patients from Montreal, elsewhere in Quebec, and beyond, since 1934. This McGill University teaching hospital, with approximately 600 beds, is one of the province's largest acute-care hospitals. It admits more than 22,000 patients per year, while handling approximately 578,000 outpatient visits, more than 84,000 emergency visits and more than 3,600 births. Treatment is provided by approximately 800 affiliated doctors, many of whom have teaching appointments at McGill University, as well as more than 300 medical residents per year, together with nursing and a wide range of allied health services.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email