Search
Search
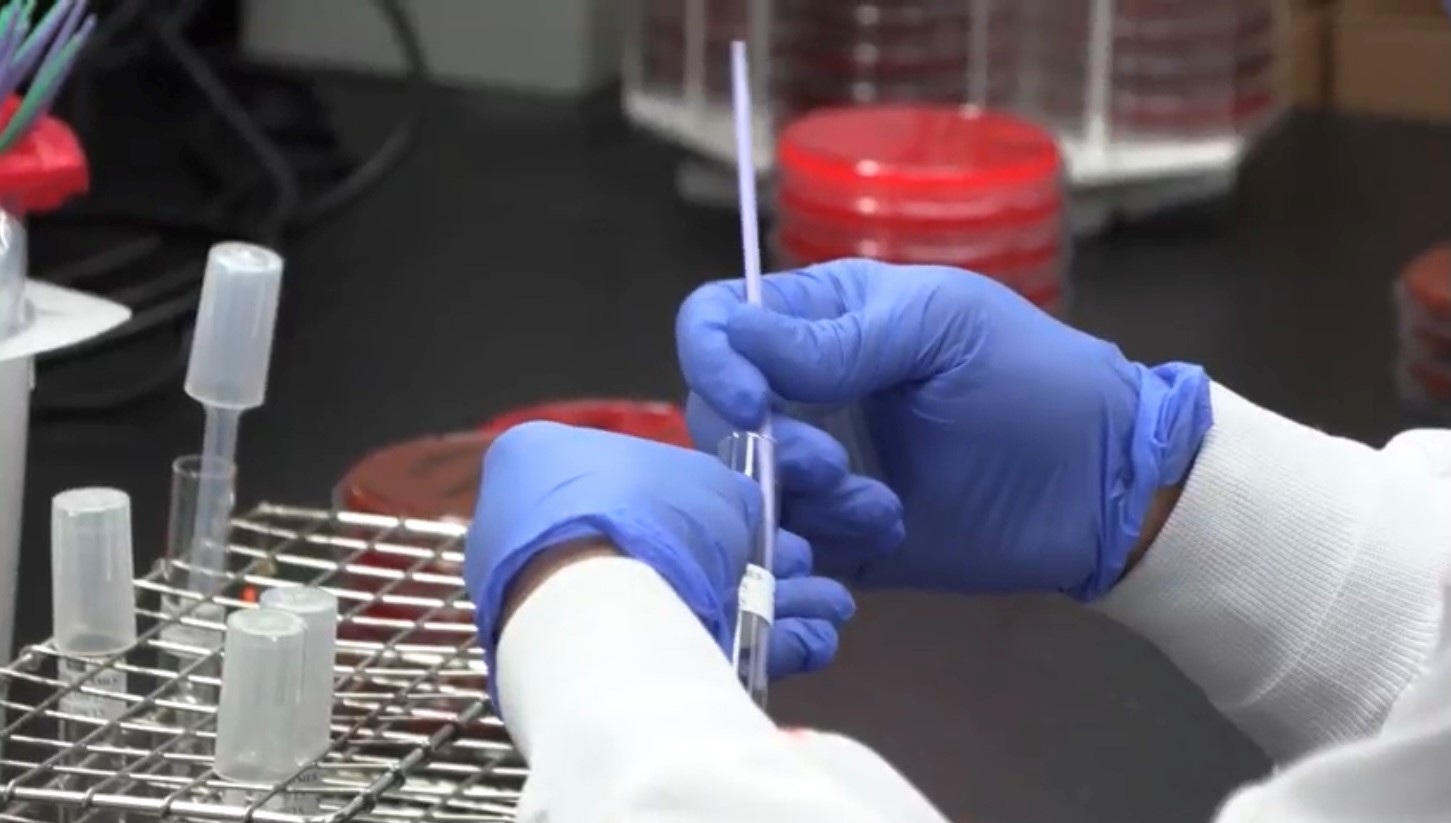
A new study is examining if probiotics can improve outcomes in knee replacement surgeries
LONDON, ON - Researchers at Lawson Health Research Institute are examining whether the use of a daily probiotic can improve outcomes in patients who undergo a total knee replacement surgery.
There are more than 70,000 knee replacement surgeries in Canada each year, and up to 10 per cent of patients experience complications following the procedure.
“One in five patients are dissatisfied after surgery due to pain and discomfort, and some patients need a repeat surgery because there is complication, infection or loosening of the joint,” says Dr. Matthew Teeter, Lawson Scientist at London Health Sciences Centre (LHSC).
Dr. Teeter and the research team are focused on improving patient outcomes. Recognizing that knee replacement patients who are considered healthy tend to have better outcomes, they are interested in how they can better support patients’ overall health as one way to optimize their outcomes.
“The knee replacement patients I see in clinic are very diverse - from young healthy active patients to medically complex to socioeconomically disadvantaged,” says Dr. Brent Lanting, Lawson Scientist and Orthopaedic Surgeon at LHSC. “We know those with poor health do not do as well as those with good health, good diet, and good supports. This study is profound in that it investigates a core aspect of our health – the gut microbiome.”
The research team will recruit 30 participants who are scheduled for a knee replacement surgery. Half of the participants will receive a daily probiotic for six-weeks ahead of the surgery, and the other half will act as a control group.
“Our microbiome is a large part of why we are healthy. A healthy person has a microbiome that produces vitamins and other things which cross over to our system and helps promote healing,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London. “We are hoping it will improve more deep healing and prevention of the rejection of the joint by improving the microbiota by giving probiotics.”
The team will assess outcomes using CT imaging, looking at the bone and implant and how it is fixing into place. They will also use PET/MRI to look at the cellular activity around the joint and inflammation.
“This should give us a sharp focus of what is going on with the joint and help us determine if there was a positive effect by using probiotics,” explains Dr. Teeter.
If the pilot study proves to be promising, the team will then work towards a larger clinical trial, combining probiotics into pre-surgical care.
“Ultimately, we want better patient outcomes with a simple treatment,” adds Dr. Burton. “If we can help improve outcomes with the use of a daily probiotic, that is a great win.”
The research team received a New Frontiers in Research Fund (NFRF) of $250,000 over three years to conduct this study.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
A vision for the future of ICES Western: Q&A with Dr. Kristin Clemens
Dr. Kristin Clemens has been selected as the new Site Director for ICES Western, the London, Ontario division of a province-wide non-profit focused on using health-related data to evaluate outcomes. ICES Western is a collaborative initiative between Lawson Health Research Institute, Western University, London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London.
Dr. Clemens is a Scientist at Lawson and an Endocrinologist at St. Joseph’s. She is also an Assistant Professor in epidemiology and biostatistics at Western’s Schulich School of Medicine & Dentistry. Dr. Clemens recently sat down to discuss the impact of the work being done through ICES Western and her hopes for the future.

1. What are you most excited for as ICES Western’s new site director?
I get to continue to work closely with an amazing group of ICES Western staff and scientists. ICES Western is already a well-oiled machine and home to scientific hubs of research in neurological health, homelessness and socioeconomic disparities, surgery, mental health, kidney disease and more. As a leader, I will not only be able to help harness some of our existing strengths, but have a chance to continue to move our institution forward. For example, Dr. Amit Garg (outgoing Site Director) will be advancing new and innovative randomized controlled trials in London, and ICES Western's going to continue to play a major role in that. There is so much more potential for innovation using our data sources; I think it's going to be a really exciting next few years for us.
2. Why did you choose to become involved with ICES Western?
I have been with ICES for about 14 years. I have lived it as an ICES trainee as a Medical Student and Resident/Fellow and became an ICES Adjunct Scientist after completing the inaugural ICES Faculty Scholars program hosted by ICES Western. I became more and more engaged with the community as a member of local ICES committees and then started to lead some of the larger research programs at ICES Western. It was the perfect time and really a natural fit for me to embark on a new leadership journey with the institution.
3. What do you hope to bring to your new position?
I'm an enabling and collaborative researcher and have been fortunate to work with multidisciplinary teams of scientists from across Western and Lawson. What I hope to do is not only support existing ICES staff, scientists, and initiatives, but also attract new researchers to the institution. I think London, Ontario, is such an incredible city for academia. I really want to use my collaborative skills and strong relationships to try to grow and expand our reach.
4. Has the work at ICES played a role in your research?
Yes, absolutely. My clinical and research focus has been on improving the care and outcomes of patients who live with complex comorbidities and disparities. ICES research allows us to focus on real-world gaps in care in Ontario and it gives us an opportunity to study people and patients who have not been able to participate in randomized trials or traditional research studies.
5. What impact does the work at ICES have on research being done in Ontario and across Canada?
ICES is home to one of the world's largest collections of administrative data sets that contain everything from hospital visits and physician encounters to use of medications and long-term care. We also have the unique ability to link data from national surveys or existing cohorts with administrative data. Because of this, ICES is very much at the forefront of improving care and quality for all Ontarians. Our research is shared internationally with both academics and non-academics, and it has changed practice and policy; it's an extremely impactful organization.
6. What do you see in the future for the organization?
I think in the future we will continue to do what we're already great at, like studying the use of health services and existing hubs of research, but also find ways to use our rich data sources, methods and talented staff to really innovate and advance research in London. With new collaborations in the city, we can also continue to grow and contribute.
7. What is the most important thing people should know about ICES?
ICES Western is here for London’s community of researchers, health care providers and decision makers. We have more than 20 scientists and dozens of highly qualified staff who are passionate about advancing high-quality, impactful work. ICES Western is a valuable resource for the community.
Addressing the impacts of the COVID-19 pandemic
As the COVID-19 pandemic has continued for a year and a half, many people from all walks of life are feeling the impacts especially when it comes to their mental health and wellbeing.
Hospital researchers through Lawson Health Research Institute, along with its hospital partners, have been studying the impacts for some key groups.
Health care workers have been at the forefront of the pandemic. These heroes have worked tirelessly through every wave and continue to provide excellent care to their patients and community. Dr. Kamia Honarmand, Critical Care Physician at London Health Sciences Centre (LHSC), remembers the stress that she and her colleagues were feeling, and know that something needed to be done.
“Our team wanted to better understand the impact of the pandemic on the lives of health care workers, both personally and professionally, and understand how they were coping when it came to their mental health,” says Dr. Honarmand who is also an Associate Scientist at Lawson. “There was a lot of reasons to be stressed even before the height of the first wave in our region. There was a lot of anxiety. The hospital wanted to find ways to support health care workers and identify resources that would assist them.”

Dr. Kamia Honarmand, Critical Care Physcian at LHSC and Lawson Associate Scientist
Frontline health care workers across the region were invited to take part in an online survey about their experiences during the pandemic. “We looked at both the impacts and the preferred coping strategies, and what supportive strategies they would like to have in the hospital in the future.”
The Veterans Care Program located at Parkwood Institute, a part of St. Joseph’s Health Care London, provides complex continuing and long-term care for Canadian war Veterans. Dr. Don Richardson, Director of the MacDonald Franklin OSI Research Centre at Parkwood Institute, has been treating and studying mental health among Veterans for many years. He believed this was a group was likely to be affected by the pandemic in unique ways.
“We know that Veterans in general are at a higher risk for depression, anxiety and PTSD,” explains Dr. Richardson, who is also a Scientist at Lawson. “We also knew the pandemic and forced restrictions would have significant impact on Veterans and their families who would be more isolated than they already are.”
More than 1,100 Veterans and around 250 spouses were recruited for the study, completing an online survey every three months for 18 months.
The study is still ongoing, but Dr. Richardson says the initial data has been telling. “We have been able to analyze some of the preliminary data and what we have found is that almost 50 per cent did not indicate their mental health had worsened during the pandemic but 40 to 50 per cent have had difficulty accessing care.”

Dr. Don Richardson, Director, Macdonald Franklin OSI Research Centre
The hope is that this study will lead to better preparedness in the future to safeguard the mental health of Veterans and ensure their access to care during a pandemic.
Many people have felt isolation during the pandemic, but that feeling may have even more of an impact for youth suffering from mood and anxiety disorders.
Dr. Elizabeth Osuch, Director of the First Episode Mood and Anxiety Program (FEMAP) at LHSC says the pandemic-led lockdown forced more than a hundred mental health clients out of in-person services.

Dr. Elizabeth Osuch, Director of FEMAP and Lawson Scientist
“They lost their resources for mental health services and support as soon as the quarantine was announced,” shares Dr. Osuch, who is also a Scientist at Lawson. “We were concerned that it would be devastating to people – and to some people it was. We wanted to make sure they had an avenue to connect with the program.”
Dr. Osuch and the FEMAP team created an online research platform to find out how patients were doing by having them fill out a symptoms and function questionnaire.
“We have analyzed the first wave so far and it shows that male patients were doing better and female patients were doing worse, which was a surprise. One of the risk factors for not doing well was the loss of their job.”
The pandemic added an extra layer of stress and worry for women who were having a baby.
“This has been an enormous and pivotal time for everyone in the world,” says Dr. Genevieve Eastabrook, Obstetrician-Gynecologist at LHSC. “The experiences during pregnancy and post-partum for both the birthing person and their baby can have effects later in life for children. For example, their overall cardiovascular and metabolic health, bonding experiences and the risk of mood disorders.”
Dr. Eastabrook, who is also an Associate Scientist at Lawson and Assistant Professor at Western University’s Schulich School of Medicine & Dentistry, is working with a team to examine the effects the pandemic may be having for mothers and their babies. As part of the study, the London research team is using an approach called ‘One Health’ which offers a holistic perspective to explore how various risk factors and social determinants of health interact.

Dr. Genevieve Eastabrook, OBGYN at LHSC and Lawson Associate Scientist
“The unique aspect is that we have a comparative group to see if there are differences in markers such as risk of depression, perceived stress and social supports,” adds Dr. Eastabrook.
Study participants are asked to complete a 30-minute questionnaire at around 6-12 weeks after their delivery. The research team is still recruiting patients for this study.
Advancing research during the COVID-19 pandemic
From the moment the COVID-19 pandemic was declared in March 2020, our teams at Lawson Health Research Institute have been at the forefront. Researchers at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London immediately began to work towards understanding the new virus in an effort to discover lifesaving health-care solutions.
To date, dozens of research projects have been advanced through Lawson with some receiving international attention as ‘world firsts’. As we mark the three-year anniversary of COVID-19 being declared a global pandemic by the World Health Organization (WHO), we share with you COVID-19 research highlighted over the past year.
Study finds acute kidney injury associated with severe COVID-19 leads to high mortality rates

Severe cases of a COVID-19 infection can cause a host of serious complications, including acute kidney injury. In a published study, scientists at Lawson found that acute kidney injury in patients with a severe COVID-19 infection leads to a high mortality rate.
By accessing data collected through the Ontario Renal Network (ORN), Dr. Peter Blake, Lawson Researcher and Provincial Medical Director at the Ontario Renal Network, and his colleagues examined 271 people at 27 renal programs across the province, including patients at LHSC, who received dialysis for acute kidney injury due to a COVID-19 infection. Read more.
Study shows a decline in Veterans’ mental health throughout the pandemic

In published findings from Lawson, more than half of Canadian Veterans reported a decline in their mental health over the course of the COVID-19 pandemic.
When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population.
To examine the potential impacts the research team launched a longitudinal study recruiting Canadian Veterans and spouses of Canadian Veterans. Participants complete online questionnaires every three months, with questions focused on mental health and virtual health care services. Read more.
Virtual care associated with significant environmental and patient cost savings

A study published in JAMA Network Open by researchers at ICES, Lawson and Western University found that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometers of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit. Read more.
London researchers discover novel method to diagnose long COVID

Published in Molecular Medicine, researchers at Lawson found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition.
The researchers studied 140 blood samples from participants at LHSC and St. Joseph’s Health Care London, including St. Joseph’s Post-Acute COVID-19 Program. Participants were those with presumed long COVID, hospital inpatients with acute COVID-19 infection and healthy control subjects. Read more.
Researchers are combining new technologies to examine blood proteins in COVID-19 patients
Published in the Journal of Cellular and Molecular Medicine, a team at Lawson discovered unique patterns of blood plasma proteins in critically ill patients that may help develop a more personalized approach to treating severe COVID-19.
Called the plasma proteome, the proteins studied are released by cells that often play an important role in the body’s immune response to viruses. The research team studied how they adapt and change to a COVID-19 infection. Read more.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Advocating for health research during “H on the Hill”
HealthCareCAN held its third annual Lobby Day “H on the Hill” event on Parliament Hill in Ottawa, on Tuesday, October 30, 2018.
Canada’s hospital CEOs and vice presidents of health research joined HealthCareCAN - the national voice of Canada’s healthcare organizations, community and research hospitals - to meet with MPs, Senators and senior government staff.
Collectively, they issued a call for federal action to unlock the tremendous economic potential of the health and life sciences sector to support better health for Canadians.
Dr. David Hill, Scientific Director for Lawson and Integrated Vice President of Research for London Health Sciences Centre and St. Joseph’s Health Care London, participated in the lobby day. Dr. Hill currently sits on the Board of Directors for HealthCareCAN.

Image

“Minister of Crown Indigenous Relations @Carolyn_Bennett, Parliamentary Secretary for Science, Sport, and Accessibility @KateYoungMP, and Dr. David Hill, catching up over lunch at #HontheHill #CDNpoli #CDNhealth”
Meeting participants stressed the need for action on HealthCareCAN’s recommendations for the 2019 federal budget, specifically:
- Setting a minimum 25% funding floor for the indirect costs of research under the Research Support Fund;
- Granting eligibility to federal infrastructure funding competitions to healthcare organizations, and;
- Investing in digital health platforms to support care, training, and research in healthcare organizations.
Diverse areas of the health and life sciences sector and key health issues were discussed, including:
- Health and science research, granting councils;
- Hospital infrastructure;
- Health innovation;
- Electronic health technology;
- Opioid crisis response;
- Mental health;
- Aboriginal health; and,
- Home care.
Read Dr. Hill’s recent column in Hospital News on bridging the gap from discovery to patient care.

HealthCareCAN provides high-quality policy research advocacy and leadership development services to our members while championing healthcare system transformation in Canada. Visit www.healthcarecan.ca to learn about our solutions to health and healthcare challenges. Follow us on Twitter: @HealthCareCAN