Search
Search
New clinical protocol after general surgery cuts opioid prescribing in half
In recent years deaths from opioid overdoses have become one of the most common injury-related deaths in North America. The continent also has the highest per capita rate of opioid prescription in the world.
Recognizing the role that opioid prescribing plays in the national opioid crisis, a team of researchers at Lawson Health Research Institute and Western University have developed a new clinical protocol called STOP Narcotics. A study demonstrating the efficacy of their protocol was presented at the American College of Surgeons Clinical Congress in Boston, Massachusetts on October 24.
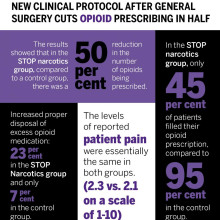
The protocol includes a combination of patient and health care provider education and an emphasis on non-opioid pain control. The study found that they were able to reduce the overall amount of opioids being prescribed after general surgery by 50 per cent while still adequately treating a patient’s post-operative pain.
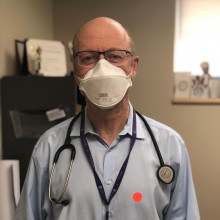
“By significantly reducing the amount of opioids prescribed, this decreases the exposure risk and potential for misuse of narcotic medication,” said Dr. Luke Hartford, a resident in general surgery at Western’s Schulich School of Medicine & Dentistry and first author on the study. “This also decreases excess medication available to be diverted to individuals for whom it was not intended.”
The study involved 416 patients at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London who underwent laparoscopic cholecystectomy or open hernia repair. They received medication for post-operative pain through the standardized protocol, specifically acetaminophen (Tylenol) and a non-steroidal anti-inflammatory drug (Naproxen) for the first 72 hours post-surgery.
The protocol instructs physicians to write a limited prescription of ten pills of opioids (Tramadol), with an expiry date of seven days after surgery, with instructions for the patient to fill this prescription only if adequate pain control was not otherwise achieved. There are also instructions on proper disposal of unused medication for the patient.
Dr. Ken Leslie, scientist at Lawson, associate professor in the Department of Surgery at Schulich Medicine & Dentistry, and Chair/Chief of the Division of General Surgery at London Health Sciences Centre led the implementation of the new protocol.
“We recognized that before STOP Narcotics, every surgeon had a different approach to pain control, and that most surgeons were prescribing more narcotics than are actually needed,” said Dr. Leslie. “When we looked at the data from this new protocol, we saw that the patient’s pain-control was just as good with this pathway, without a huge prescription for narcotics.”
The results showed that in the STOP narcotics group, compared to a control group, there was a 50 per cent reduction in the number of opioids being prescribed. They also demonstrated that only 45 per cent of patients actually filled their opioid prescription, compared to 95 per cent in the control group, and they were also able to increase appropriate disposal of excess opioid medication from 7 per cent in the control group to 23 per cent in the STOP Narcotics group. The levels of reported post-operative pain were the same in both groups.
The group now hopes to expand the protocol for applications beyond general surgery.
“If we can decrease the opioid exposure risk in our patients, and decrease the amount of excess medication available for diversion, and spread this to other institutions and surgical procedures and specialties, this has the potential to significantly impact the opioid crisis,” said Dr. Patrick Murphy, a resident in general surgery at Schulich Medicine & Dentistry and co-author on the study.
The study, “The Standardization of Outpatient Procedure (STOP) Narcotics: A Prospective Noninferiority Study to Reduce Opioid Use in Outpatient General Surgical Procedures,” is published in the Journal of the American College of Surgeons.
| Dr. Ken Leslie | Dr. Luke Hartford | Dr. Patrick Murphy |
Image

|
Image

|
Image
|
New imaging solution could help improve survival for patients with recurring prostate cancer
London, ON - A multicentre study led by London Health Sciences Centre Research Institute (LHSCRI), Lawson Research Institute of St. Joseph’s Health Care London (Lawson), and University Health Network (UHN) has found a novel imaging solution, called prostate-specific membrane antigen (PSMA) positron emission tomography (PET) scanning, can more effectively detect the recurrence of prostate cancer compared to standard imaging methods, and is associated with improved survival outcomes. The study, carried out over seven years, is published in The Journal of Nuclear Medicine.
During a PSMA PET scan, a radioactive molecule designed to target a protein in prostate cancer cells is injected into the bloodstream of a patient prior to the scan. The study uncovered that the molecule is effective in binding to prostate cancer cells, helping to detect recurring prostate cancer earlier and more effectively than standard imaging methods.
“This new technique gives physicians the information needed to determine the best treatment,” says Dr. Glenn Bauman, Scientist at LHSCRI and Radiation Oncologist at London Health Sciences Centre (LHSC). “When a blood test shows cancer has returned but standard imaging can’t find it, physicians may need to use less precise therapies like whole-body drug therapy. With this new imaging technique, we can locate the cancer and target it directly.”
The research team found that the overall detection rate was 70 per cent, much higher than the historical rates of detection of 10-20 per cent with conventional bone scan and CT scans. About half of all patients had their management of the disease changed based on the results of the scans. Almost 90 per cent of men with cancer detected by PSMA PET had a change in management of their recurring prostate cancer following the scan. They also found that patients who had their treatments modified based on results from the PET scan had a better overall survival rate than those who received standard imaging.
“We’re encouraged by how this imaging approach is already changing cancer care,” says Dr. Ur Metser, Division Head of Molecular Imaging at UHN and Clinician Scientist at UHN’s Princess Margaret Cancer Centre. “Our study showed that PET scans using this technique led to more personalized treatment decisions and those changes are linked to longer survival. That’s a meaningful step forward for patients and their care teams.”
Dr. Bauman and his colleagues from Lawson and LHSCRI were the first in Canada to image a patient using PSMA PET imaging in 2016. Since then, this study has enrolled thousands of men across six hospitals in Ontario through funding from Ontario Health - Cancer Care Ontario. Based on promising results from this and other research, PSMA PET scans are now funded as a standard of care test for men with advanced prostate cancer.
For more information, please contact: Deb Flaherty, Consultant, Communications & Public Affairs, St. Joseph's Health Care London.
519-646-6100 ext. 47560
ABOUT LAWSON RESEARCH INSTITUTE
Lawson Research Institute, the health innovation arm of St. Joseph's Health Care London, is committed to making and sharing discoveries that improve lives locally and internationally. Every day, Lawson researchers work to transform imagination to innovation to patient impact. Lawson leads health-care research. Find us at LawsonResearch.ca and @stjosephslondon on social media.
ABOUT LONDON HEALTH SCIENCES CENTRE RESEARCH INSTITUTE
At London Health Sciences Centre Research Institute (LHSCRI), our teams pioneer discoveries that transform the health of adult and paediatric patients around the world. As the research institute of London Health Sciences Centre (LHSC), we conduct research where patient care is delivered, working alongside patients, families, health-care providers and academic partners like Western University. We are leaders in advancing the understanding, diagnosis, treatment and management of diseases and health conditions through a diverse research program that ranges from laboratory-based science to clinical trials. Our research has a global impact as we build on LHSC’s 150-year legacy of health innovation and drive forward medical breakthroughs that
make a difference in the lives of patients and their families. Find us online at WWW.LHSCRI.CA and on social media @LHSCRI.
New national strategy to tackle dementia
Researchers in London, Ontario have been awarded $1.345 million over five years through the second phase of the Canadian Consortium on Neurodegeneration in Aging (CCNA), announced today as part of Canada’s first national dementia strategy. CCNA is a collaborative research program tackling the challenge of dementia and other neurodegenerative illnesses.
A Dementia Strategy for Canada: Together We Aspire focuses on preventing dementia, advancing therapies and finding a cure, as well as improving quality of life for people living with dementia and caregivers.
Clinician researchers from across the country working together
Dr. Manuel Montero-Odasso, Scientist at Lawson Health Research Institute, is world renowned for his findings on the relationship between cognition and mobility in the elderly, and gait as a predictor of frailty and dementia. He leads the Mobility, Exercise and Cognition (MEC) Team in London, comprised of top researchers in the areas of mobility, exercise and brain health.
“Evidence from other countries with dementia strategies shows that coordinated, targeted efforts at the national level improves results for all aspects of dementia care and also for research,” says Dr. Montero-Odasso, also a geriatrician and Director of the Gait and Brain Lab at Parkwood Institute, a part of St. Joseph’s Health Care London.
CCNA was purpose-built to synergize dementia research within the Canadian context. Phase I saw the creation of infrastructure fostering collaboration amongst Canadian researchers, and there are now 20 teams built around important research topics.
“This kind of effective national collaboration by scientists and clinicians from many disciplines gives the CCNA a cutting edge in research, prevention, treatment and management of all forms of dementia,” explains Dr. Montero-ODasso. “We created a national network of researchers form west to east coast with a high level of expertise to deliver lifestyle interventions to improve cognition and slow down progression to dementia. I feel privileged working with such excellent investigators and leading this important endeavour locally.”
Preventing dementia through lifestyle changes
The MEC team has several projects in the works, but the majority of the new funding is to complete the SYNERGIC Trial, SYNchronizing Exercises and Remedies on Gait and Cognition.
This first-in-the-world clinical study is testing a triple intervention aimed at treating Mild Cognitive Impairment (MCI) and delaying the onset of dementia. The SYNERGIC Trial incorporates physical exercises and cognitive training, along with vitamin D supplementation to determine the best treatment for improving mobility and cognition.
“We are looking at how interventions will work together and targeting cognitive decline at its earliest stage – individuals with MIC,” explains Dr. Montero-Odasso. “Both physical and cognitive exercises have shown promising effects for maintaining cognition, while vitamin D deficiency is associated with cognitive decline.”
A professor at Western University’s Schulich Medicine & Dentistry, Dr. Montero-Odasso partners with researchers from across the city including Dr. Rob Bartha, imaging scientist at Schulich Medicine & Dentistry and Robarts Research Institute at Western University, and Dr. Kevin Schoemaker who leads the Laboratory for Brain and Heart Health.
Study participants in the SYNERGIC Trial are asked to complete an individualized and progressive routine of exercises and cognitive training three times a week for six months, with one final assessment at 12 months. The main site for the study is Parkwood Institute with the physical exercises taking place at the Labatt Health Sciences Building on the Western campus.
To date, 138 research patients has been recruited across multiple sites in Canada.
One participant’s experience
One day, Peter Saracino saw an advertisement about a research study. They were looking for participants who were a minimum age of 60 and had minor cognitive impairment. He felt he fit the bill and he was interested in this kind of research.
“I have family members who suffered from forms of dementia and Parkinson’s Disease. I really understand how hard it hits and I liked that this study was about prevention,” explains Peter.
Going into it, Peter thought he was in pretty good shape. He has two dogs and walks them regularly. “But by going to the gym and doing the exercises and faster-paced walking, I realized that I wasn’t in as good shape as I thought. My diet was under control but I was still taking blood pressure medication. I didn’t have much energy.”
After 10 weeks in the study, he feels better than he has for over a decade. “I can garden for longer. I took two notches off my belt. I no longer take my blood pressure medication. I actually feel younger.”
He remembered that last year he slipped and fell four times, which was very unusual for him. Part of his cognitive impairment is that he had trouble with balance, and that has improved for him as well.
Peter feels that “this is exactly the kind of research that the government should be investing in – an ounce of prevention is worth a pound of cure. This kind of research leads to keeping people independent and healthier as they get older. People are happier. They feel like doing more. There is no downside to improving someone’s health through lifestyle changes, and in fact it is cost effective and helps ease the burden on the health care system.”
Looking forward
“Our preliminary analysis from SYNERGIC is giving us a strong indication that a multimodal approach, combining physical exercise, cognitive training and supplementation, has a synergistic effect. It seems the whole is greater than the sum of its parts,” says Dr. Montero-Odasso.
A major goal for the work of the MEC team in London is to translate their research findings into clinical guidelines that can be used at the front line of care. “Practitioners understand the overall importance of exercise and cognitive vitality, but we are missing more specific guidelines on what kind and how much will work for different patients. Basically, what is an effective lifestyle prescription.”

Dr. Montero-Odasso adds that “as our population ages, a comprehensive strategy is vital to ensure the growing number of those living with dementia receive the care and support they deserve. Over half a million Canadians are currently living with dementia. By 2031, this number is expected to nearly double.” More than one third of dementia cases might be preventable.
CCNA Phase II
In CCNA’s Phase II, researchers are working on analyzing the overall health of every patient in a large clinical cohort study, COMPASS-ND. This information will be used to enhance understanding of how changes in the brain affect dementia severity and ways to reduce and prevent this through lifestyle changes. Lawson is the leading recruitment site for COMPASS-ND and the London team will be instrumental in the larger lifestyle interventions moving forward.
CCNA is funded by the Government of Canada, Canadian Institutes of Health Research (CIHR) and other funding partners. CIHR is providing $31.6 million, and partners—including provincial agencies and non-profit organizations—are providing an additional $14.4 million for a total investment of $46 million over five years. The research on dementia prevention, diagnosis, treatment and care as part of Phase II of the CCNA will support the national strategy.
Related stories
New research on reducing harm for people who use methamphetamine
At a virtual event, a research team led by Lawson Health Research Institute announced details of the Methamphetamine Harm Reduction Project that will study the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose.
“Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk.
“We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
New research on reducing harm for people who use methamphetamine in hospital
LONDON, ON – At a virtual event today, a research team from Lawson Health Research Institute is announcing details of the Methamphetamine Harm Reduction Project that will test the integration of harm reduction strategies into hospital settings for people who use methamphetamine.
Evidence-based harm reduction strategies for methamphetamine use, for example needle/syringe services, supervised injection sites and safe supplies, have been used in the community to reduce health risks such as infection and overdose. “Harm reduction strategies are rarely used within hospitals in Canada. The current standard of care does not allow the use of illicit substances in hospitals as the safe consumption of substances requires an exemption under section 56.1 of the Controlled Drugs and Substances Act from Health Canada,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and study co-principal investigator.
Recent studies from London, Ontario found that substance use in hospital is happening and poses a greater risk of infection than in the community.
“There is an assumption that people in hospital aren’t using, but in fact we’ve found that almost 50 per cent of patients admitted to hospital with an infection related to substance use are continuing to inject during their stay. That is clearly an underestimate because many patients are worried about being stigmatized or other consequences of using in hospital and so may not be willing to report it to researchers or tell their health care providers,” explains Dr. Michael Silverman, Associate Scientist at Lawson, city-wide Chair/Chief of Infectious Diseases for London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, and study co-principal investigator.
Findings have shown that patients are more likely to get an infection related to substance use when being treated in the hospital as opposed to other settings and many people who are using leave hospital against medical advice, putting their health and safety at risk. “People aren’t able to access safe ways to use substances and they are doing it in secret, so it’s not the best way to do it to prevent infection. There are also gaps in support for withdrawal and other addiction services,” says Dr. Silverman.
The research team will lead a four-year project with recruitment of up to 360 adults aged 16-85 years with past experience or current use of methamphetamine, including inpatients, outpatients and those in community outreach programs. Up to 180 health care and service providers will be recruited to share their perspectives on harm reduction strategies. After the consultation phase in the first year, with approval from Health Canada, the identified set of strategies based on the perspectives of people with lived experience will be implemented within LHSC and St. Joseph’s hospital sites.
“To our knowledge, there are only five supervised consumption services based in acute care hospitals in the world. Three of these sites are in Europe and there are two locations in Canada that have implemented a similar approach. London will be the second place in North America to implement harm reduction strategies for substance users within hospital walls,” adds Dr. Forchuk. “We are leading the way towards a groundbreaking shift to greatly improve health care for Canadians who use substances.”
Potential harm reduction strategies are safe injection sites or safe places to use substances, new needles and syringes, available Sharp boxes, support for detox and withdrawal, medication, resources at discharge, and enhanced addiction services and counseling.
Sonja Burke, the Director of Harm Reduction Services at the Regional HIV/AIDS Connection, notes there has been a marked increase in more complex health care needs and a high rate of deaths in the community for people who are experiencing homelessness and addiction.
“Harm reduction is about meeting people where they are without stigma or assumptions, accepting that substance use is a part of their life,” says Burke. “Our experience in the supervised consumption services proves that once a person is able to use their pre-obtained substances, they will engage in further supports for their health care. We have to change how the supports are being provided within the system to ensure we are reducing health risks and death.”
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New research showcased at third annual Parkwood Institute Research Spring Update Half Day
More than 100 researchers, staff and trainees attended the third annual Parkwood Institute Research (PIR) Spring Update Half Day on April 27, 2018 to share their innovative research and learn about work from across PIR through interactive workshops and poster presentations.
A program of Lawson Health Research Institute and located at St. Joseph’s Health Care London’s Parkwood Institute, PIR represents three major research programs: cognitive vitality and brain health, mobility and activity, and mental health. The event allowed guests to hear about new studies and recent research developments from across these three themes.
“Parkwood Institute Research covers different research areas but what we want to emphasize with this event is the overlap and collaboration between our programs. Having an inter-disciplinary approach that encourages partnerships ultimately helps us to incorporate new knowledge into patient care at Parkwood Institute,” says Dr. Cheryl Forchuk, Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery, and Assistant Director, Lawson.
Five interactive workshops were held on a variety of different topics, such as clinical trials, systematic reviews, innovation in health care, practice-based research methods and evaluating SMART technology. The workshops were led by some of Parkwood Institute’s research leaders, including Drs. Cheryl Forchuk, Robert Teasell, Michael Borrie, Dalton Wolfe, and Arlene MacDougall.
Attendees also had the opportunity to visit poster presentations on recent PIR projects.

Ashrafunissa Janmohammad (above), Lawson research coordinator at Parkwood Institute’s Chronic Wound Management Clinic, was one of the poster presenters at the event. She presented on a study led by Lawson associate scientist Dr. David Keast, which assessed whether chitosan gelling fibre dressing could be effective in controlling bleeding after minor wound surgery. Chitosan is derived from chitin, the structural component of the cell walls of fungi and the shells of arthropods such as crabs, lobsters, shrimps and insects.

Juweiriya Ahmed (above), a MSc candidate at Lawson and Western University’s Schulich School of Medicine & Dentistry, was another presenter. Her poster outlined a study investigating the interaction between neuroanatomical and genetic risk factors that may contribute to the development of psychotic symptoms (delusions and hallucinations) in patients with Alzheimer’s disease. Supervised by Lawson scientist Dr. Elizabeth Finger, the study could help inform the development of therapeutic targets and treatment plans.
New study aims to improve treatment for rheumatoid arthritis
A research team led by Lawson scientist Dr. Mamadou Diop has been awarded a Lawson Internal Research Fund to investigate whether a previously developed optical technique that can detect arthritis within one week of onset could also be used to provide early assessment of treatment response for rheumatoid arthritis (RA).
RA is a disease that causes chronic inflammation of the joints, which results in pain, reduced quality of life and loss of productivity. There is no cure for RA but a new category of drugs – biologic agents that can reduce pain and slow down or even halt disease progression – has revolutionized treatment.
However, these new drugs are expensive and only work in 30 per cent of patients, which means many RA sufferers are treated with no benefit for up to six months – the time it takes for current monitoring methods to reliably determine whether a treatment is working or not. “This is a direct consequence of the lack of sensitivity of current monitoring methods,” says Dr. Diop, who is also an assistant professor at Western University’s Schulich School of Medicine & Dentistry.
Since their recently developed optical technique has a high sensitivity to arthritis, Dr. Diop and his team believes it could also be used as a safe and convenient method of assessing treatment efficacy in RA patients. Additionally, there are striking similarities between RA and cancer, and it has been shown that optical techniques can predict cancer in as early as one day after therapy starts.
At St. Joseph’s Health Care London, they will test this theory in a rat model of RA and compare the results of the optical technique to histology and CT imaging, other established methods of determining whether a treatment is effective.
“If successful, this project will generate a safe, low-cost technique that can detect treatment response in RA within days of starting treatment. This would reduce the risk of further joint damage experienced by many patients for whom the drugs are ineffective,” says Dr. Diop. “We hope this will enable early redirection of patients with non-responding RA to alternative treatments, such as a combination of multiple drugs and more frequent monitoring.”
Dr. Diop adds, “The Lawson IRF grant will enable us to test the validity of our hypothesis and subsequently generate valuable preliminary results to support grant proposals for larger external funding.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).
New study aims to understand team-based care for chronic disease management
Chronic diseases, such as chronic obstructive pulmonary disease (COPD), are complex and require thorough care to help manage the condition. Patients often need support from an integrated team of health care professionals who work in different settings.
Dr. Shannon Sibbald, associate scientist at Lawson Health Research Institute, is leading a study to better understand integrated health care teams for chronic disease management and factors that help successful implementation.
Integrated team-based models of care include multiple health care providers working together to support patients with complex needs, such as those with chronic disease. There are many benefits to integrated team-based models of care. Patient outcomes are improved, health care providers feel more supported in their work and services are less likely to be duplicated.
Dr. Sibbald’s research focuses on chronic obstructive pulmonary disease (COPD), a devastating chronic disease affecting normal lung function in over 1.5 million Canadians. COPD is one example of a chronic disease where patients can benefit from team-based care. COPD is often underdiagnosed, and patients with COPD and other chronic diseases may not be receiving the ideal care for their condition.
While integrated team-based care is important, there are currently few studies to guide implementation. In this study, Dr. Sibbald’s research team will engage health care providers and patients to gain a rich understanding of successful integrated approaches to chronic disease management, including how team-based models of care are implemented. The team will also work to better understand how patients with chronic diseases view such models, and what their hopes and expectations are for their care.
“We want to explore innovative and successful approaches to implementing team-based models of care,” explains Dr. Sibbald. “We’re looking to learn how these methods can support practice, improve patient outcomes and spread innovation.”
The team will look at high performing integrated care teams that support current best practices at a family health team in London, Ontario.
When models are applied to practice, context is an important part to consider. For chronic diseases, context is often broad and elaborate. They hope to gain insight into what works well and what does not in dynamic contexts, and gain a better understanding of implementation facilitators and barriers.
The ultimate goal is to build knowledge that will support implementation and sustainability of high-performing integrated health teams across our health system.
“While motivation and momentum to use integrated teams is high, there is little guidance on how to do this well,” says Dr. Sibbald. “This research will provide insight into what works and what does not, reducing our gap in knowledge.”
Dr. Sibbald received a Lawson Internal Research Fund (IRF) grant to conduct this pilot study. Once complete, Dr. Sibbald’s team hopes to expand the study to look at integrated care models at other sites across the province.
"The IRF grant enables our team to validate our methods of evaluating the implementation of interprofessional team-based care in complex settings," adds Dr. Sibbald. "By examining the impact team-based care for patients with COPD, we hope to demonstrate the relevance of our findings, to support grant proposals."
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
New study examining if probiotics can improve outcomes in knee replacement surgeries
Researchers at Lawson Health Research Institute are examining whether the use of a daily probiotic can improve outcomes in patients who undergo a total knee replacement surgery.
There are more than 70,000 knee replacement surgeries in Canada each year, and up to 10 per cent of patients experience complications following the procedure.
“One in five patients are dissatisfied after surgery due to pain and discomfort, and some patients need a repeat surgery because there is complication, infection or loosening of the joint,” says Dr. Matthew Teeter, Lawson Scientist at London Health Sciences Centre (LHSC).

Dr. Teeter and the research team are focused on improving patient outcomes. Recognizing that knee replacement patients who are considered healthy tend to have better outcomes, they are interested in how they can better support patients’ overall health as one way to optimize their outcomes.
“The knee replacement patients I see in clinic are very diverse - from young healthy active patients to medically complex to socioeconomically disadvantaged,” says Dr. Brent Lanting, Lawson Scientist and Orthopaedic Surgeon at LHSC. “We know those with poor health do not do as well as those with good health, good diet, and good supports. This study is profound in that it investigates a core aspect of our health – the gut microbiome.”

The research team will recruit 30 participants who are scheduled for a knee replacement surgery. Half of the participants will receive a daily probiotic for six-weeks ahead of the surgery, and the other half will act as a control group.
“Our microbiome is a large part of why we are healthy. A healthy person has a microbiome that produces vitamins and other things which cross over to our system and helps promote healing,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London. “We are hoping it will improve more deep healing and prevention of the rejection of the joint by improving the microbiota by giving probiotics.”
The team will assess outcomes using CT imaging, looking at the bone and implant and how it is fixing into place. They will also use PET/MRI to look at the cellular activity around the joint and inflammation.
“This should give us a sharp focus of what is going on with the joint and help us determine if there was a positive effect by using probiotics,” explains Dr. Teeter.
If the pilot study proves to be promising, the team will then work towards a larger clinical trial, combining probiotics into pre-surgical care.
“Ultimately, we want better patient outcomes with a simple treatment,” adds Dr. Burton. “If we can help improve outcomes with the use of a daily probiotic, that is a great win.”
The research team received a New Frontiers in Research Fund (NFRF) of $250,000 over three years to conduct this study.
New study looking at advanced imaging to optimize treatments for prostate cancer patients
Advanced imaging will help better guide radiation treatments
MEDIA RELEASE
For Immediate Release
January 12th, 2022
London, Ontario- Prostate cancer is the most common cancer among Canadian men, and it is estimated that one in eight men will be diagnosed with prostate cancer within their lifetime. Researchers at both Lawson Health Research Institute and Sunnybrook Research Institute, are teaming up on a study which is pairing advanced imaging technology with high precision short course radiotherapy, that could lead to better outcomes for patients.
“We have started to look at ways to integrate advanced imaging to help better understand the amount of cancer in the prostate and the location of cancer in the prostate to help guide radiation treatments,” says Lawson Scientist, and Radiation Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Dr. Glenn Bauman.
Currently when radiation is done, a computer tomography scan (CT) gives radiologists the location and boundary of the prostate, but it doesn’t give details about the location of the cancer within the prostate.
“What we are doing in the study is integrating two other forms of imaging; magnetic resonance imaging (MRI) and prostate specific membrane antigen (PSMA) PET scans, both of which can give information on the exact location of the cancer,” explains Dr. Bauman. “This will allow us to refine the radiation treatment and to target the cancer with more intensified radiation.”
Scientist at Sunnybrook Research Institute, Dr. Andrew Loblaw says using advanced imaging will also pinpoint if the cancer has moved into other areas of the pelvic region, which helps target all possibilities and lessens the chance of the cancer coming back. The type of radiation being used for this study is called stereotactic body radiotherapy (SBRT) which is more accurate, and reduces both radiation side effects to adjacent organs, while also reducing treatment visits.
“The combination of PSMA and SBRT gives us the ability to save some normal tissue and dramatically reduce treatment times,” explains Dr. Loblaw. “If we know the cancer is in one place and not another, we can spare radiation from areas not needing it which spares side effects.”
The team plans to recruit 50 men for the study that have advanced prostate cancer and need more intense treatments. Participants will undergo the advanced PSMA PET imaging at St. Joseph’s Health Care London. The same imaging techniques will be used to determine and track if the cancer is responding well to treatments.
“This is a smarter tool that will help us more accurately know what patients have,” says Dr. Loblaw. “We will know if they have more of a metastatic disease and who has localized disease. Cure rates are better when you know exactly what you are trying to cure.”
Study participants will be closely monitored for five years, to determine the success of the more targeted and intense radiation treatments. Dr. Bauman says this will also help quickly identify the potential need for more advanced therapies.
“Our treatments are good, but If there is a man we haven’t cured we want to know as soon as possible.”
The study has received funding by the Ontario Institute for Cancer Research (OICR) as part of the Institute’s new initiative that supports pre-clinical research and new clinical trials that focus on early stage, and recurrent cancers.
-30-
About Lawson Health Research Institute: Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
About Sunnybrook Research Institute: Sunnybrook Research Institute (SRI) is the research arm of Sunnybrook Health Sciences Centre, an internationally recognized academic health sciences centre fully affiliated with the University of Toronto. SRI is one of the fastest growing hospital-based research enterprises in Canada with well-established programs in basic and applied sciences which span across three scientific platforms and ten clinical programs, developing innovations in care for the more than 1.3 million patients the hospital cares for annually. Recognized as a Centre of Excellence in focused ultrasound, SRI has one of the most comprehensive and successful focused ultrasound research programs in the world, with technical, scientific and clinical experts accelerating progress in the field.
FOR MORE INFORMATION, PLEASE CONTACT:
Celine Zadorsky
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C. 519-619-3872
@email
www.lawsonresearch.ca/news-events
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study sheds light on the connection between the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
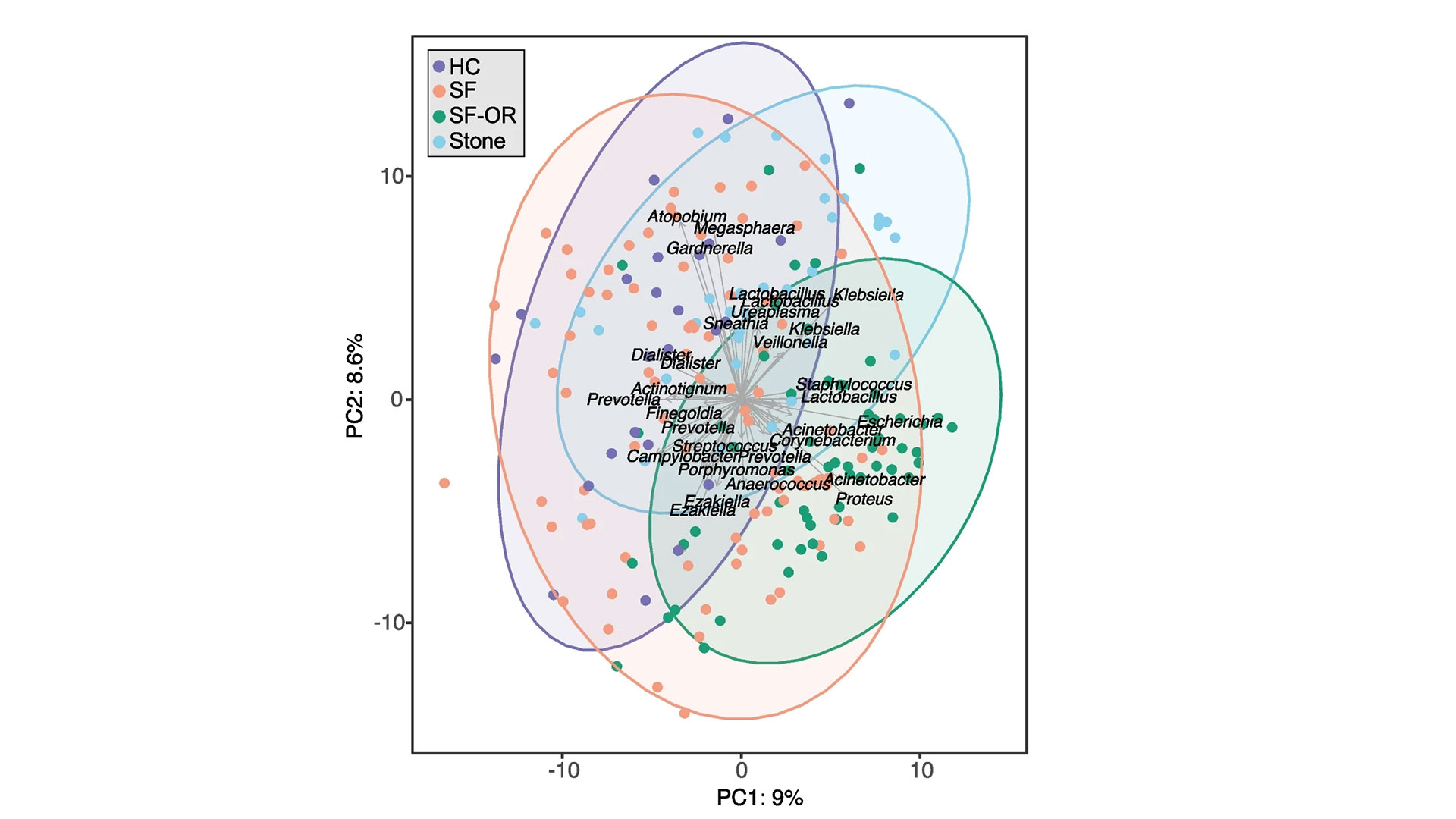
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study sheds light on the connection between the microbiome and kidney stones
A new study from Lawson Health Research Institute and Western University published in the journal Microbiome has found changes in the microbiome in multiple locations in the body are linked to the formation of kidney stones.
The human microbiome comprises trillions of microorganisms, including healthy bacteria. In recent years, research has begun to uncover its role in health and numerous diseases.
The research team examined the gut, urinary and salivary microbiomes in 83 patients who had kidney stones and compared them to 30 healthy controls. They found changes in all three microbiomes were linked to kidney stone formation.
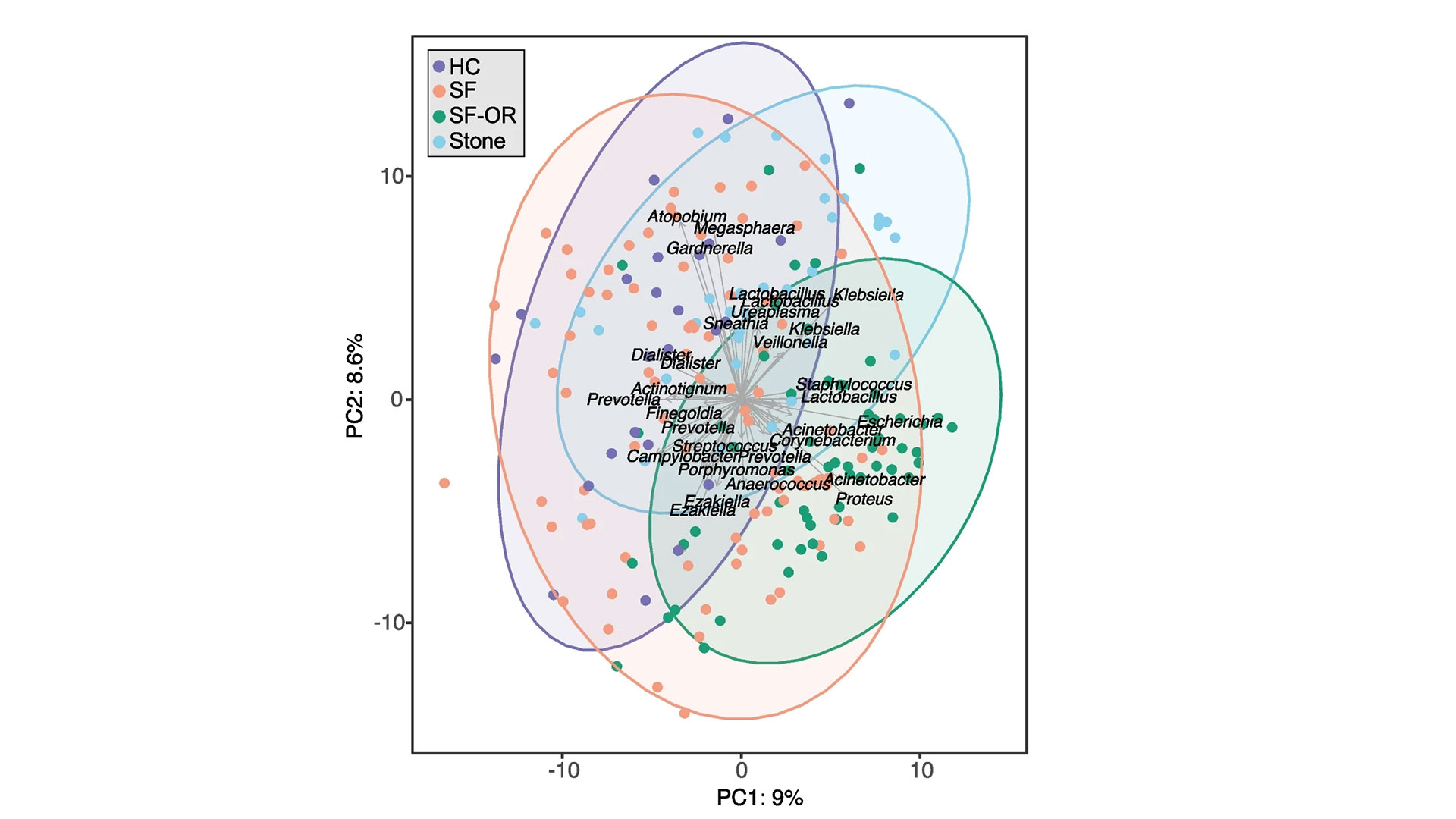
“Kidney stone disease has been rising in recent years, affecting roughly 10 per cent of people,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at St. Joseph’s Health Care London (St. Joseph’s). “While previous research has shown a connection between the gut microbiome and kidney stones in those who have taken antibiotics, we also wanted to explore the connection to other microbiomes in the hopes we can advance understanding and potential treatments.”
Study participants included people who had formed kidney stones, had not had antibiotic exposure in the last 90 days and were having the stones removed surgically at St. Joseph’s.
“Our testing – called shotgun metagenomic sequencing – allowed us to discover which bacteria were present in the gut and the genetic capabilities of those bacteria, or how it functions. We also did a simpler sequencing of the oral and urinary samples,” explains Dr. Kait Al, lead author on the study and Postdoctoral Research Fellow at Western’s Schulich School of Medicine & Dentistry.
Kidney stones are most commonly formed from calcium oxalate, which is a waste product produced by the body. Historically, it was thought people with specific gut microbes, like one bacterium called Oxalobacter formigenes that breaks down oxalate, were less likely to form kidney stones. This study suggests there are other factors.
“It’s a more complex story. The microbes form a kind of network that’s stable and beneficial in healthy people, but in those with kidney stones, that network is broken down. They’re not producing the same vitamins and useful metabolites, not just in the gut but also in the urinary tract and oral cavity,” Dr. Al explains.

There was also evidence that those with kidney stones had been exposed to more antimicrobials, as they had more antibiotic-resistant genes.
“We found not only that those who got kidney stones had an unhealthy microbiome, including a gut microbiome that was more likely to excrete toxins to the kidneys, but also that they were antibiotic resistant,” explains Dr. Burton, also an Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine & Dentistry.
The research team says that although more research is needed, these initial findings shed light on the overall importance of a person’s microbiome and keeping it as healthy as possible, with a microbiome-friendly diet and minimal antibiotic use potentially part of the solution.
The study was funded in part through the Weston Foundation and supported by the American Urological Association.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
New study shows technology could play an important role in mental health support
LONDON - In a study published in MDPI Journal, a team of researchers at Lawson Health Research Institute have shown that the use of technology may assist in better outcomes for those living with both mental health and physical disorders.
Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson, and her team embarked on a pilot study that used smart home monitoring solutions to assist those living with both a mental health disorder and other health challenges. The purpose of this pilot study was to see if technology could improve overall lifestyle and wellbeing.
“We began our research by using hospital prototype apartments – apartment style care spaces within hospital settings – that were equipped with smart home technology solutions such as a screen device, activity trackers, weigh scales and medication dispensers,” says Dr. Forchuk who is also the Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery at St. Joseph’s Health care London. “Once we tested it in a hospital setting, we wanted to find a way to take this idea out into the community in different kinds of housing and living situations to see if it would be beneficial.”
The research team partnered with the Canadian Mental Health Association (CMHA) and the London and Middlesex Community Housing (LMCH) to work together to retrofit the homes of the 13 study participants.
“We worked together with the participants and their care providers to choose what combination of technology they felt would be best for them,” says Dr. Forchuk. “No matter their health condition each participant wanted to be more active and independent, with the goal of staying out of hospital.”
All smart devices were connected to the Lawson Integrated Database, which is a database that can securely collect data from multiple sources such as health devices. This allowed care providers to send reminders to participants, while also tracking usage and results.
“The key benefits we noted was that study participants started to live healthier lives,” says Jonathan Serrato, Lawson Research Associate. “Participants logged going for walks and exercising more often, as well as making healthier food choices. Those who used the medication dispensers did not miss a single dose. The touch screen devices also allowed participants to easily communicate with care providers and support networks, and access more resources.”
Following the pilot study, the research team also published a subsequent paper, as a ‘how-to guide’ for utilizing smart home technology interventions as a health care tool.
“This paper is a helpful resource that outlines implications and considerations when it comes to smart home technologies,” adds Serrato. “There are many areas we touch upon such as security, privacy and feasibility as well as hardware and software information for those who would like to take on their own similar type of smart home technology project.”
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study will assess fecal transplants in treatment of pancreatic cancer
Scientists examining microbiome to improve cancer therapies
MEDIA RELEASE
For Immediate Release
LONDON, ON- Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes.
“Pancreatic cancer is very hard to treat, partially because when it’s detected, the cancer is usually in a later stage and spreads very quickly,” explains Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s London Regional Cancer Program (LRCP) and Associate Scientist at Lawson. “Our best chemotherapy treatments for the average patient, will give them a little less than a year to live.”
With the goal of improving treatments for these patients the research team led by Dr. Saman Maleki, Scientist at Lawson, is studying whether changing the gut microbiome can result in better response to cancer treatments.
“We know that the microbiome plays an important role in patients’ response to various forms of systemic treatments such as immunotherapy and chemotherapy for different cancers,” says Dr. Maleki.
This unique study will happen in three stages. The first stage is an observational study to examine fecal samples of 52 patients at LRCP with advanced pancreatic cancer. The second stage will focus on using the samples from these patients in preclinical models to test new combinations of treatments. The final stage of the study will focus on intervention through human clinical trials by modifying a patient’s microbiome with something called a fecal transplant prior to treatment.
“The microbiome is involved in many aspects of cancer development and these organisms aren’t just living in the gut but also within the tumor,” says Dr. Michael Silverman, Lawson Scientist and Chair/Chief of Infectious Diseases at LHSC and St. Joseph’s Health Care London. “We believe that by giving people a fecal transplant, we can change the bacteria that live within the tumor and gut and then optimize the immune response to both the tumour and to treatment, with the goal of improving patient outcomes.”
Fecal transplants involve collecting stool from a healthy donor, preparing it in a lab and safely transplanting it to the patient, in this case with a capsule. The goal is to transplant the donor’s microbiome so that healthy bacteria will colonize in the patient’s gut.
“If you think of microbiome, each bacterium is like a little factory and all together they are a giant factory within us producing things we need,” explains Dr. Jeremy Burton, Lawson Scientist who specializes in human microbiome research. “Over time, a person’s diet, medications, and lifestyle can change the microbiome and it can have a big impact to the rest of our body.”
The research team was recently awarded a $450,000 Catalyst 2021 grant from the Weston Family Foundation to conduct this study, which is the first in the world focusing on prospectively modifying the microbiome in pancreatic cancer patients for treatments and outcomes.
“We normally don’t see this in one study where we go through the full spectrum of learning from patients, to looking at treatments, and then moving to a final intervention stage,” explains Dr. Maleki. “This has not been tried in pancreatic cancer before, but we think leveraging the microbiome and improving the immune response can potentially move the needle in this patient population.”
The team is recruiting both pancreatic cancer patients, as well as healthy volunteers for fecal transplant samples. Those interested in helping with fecal transplant donations can contact Dr. Seema Parvathy at 519-646-6100 ext. 61726 or email seemanair@@email
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New study will assess fecal transplants in treatment of pancreatic cancer
Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes.
“Pancreatic cancer is very hard to treat, partially because when it’s detected, the cancer is usually in a later stage and spreads very quickly,” explains Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s London Regional Cancer Program (LRCP) and Associate Scientist at Lawson. “Our best chemotherapy treatments for the average patient, will give them a little less than a year to live.”
With the goal of improving treatments for these patients the research team led by Dr. Saman Maleki, Scientist at Lawson, is studying whether changing the gut microbiome can result in better response to cancer treatments. “We know that the microbiome plays an important role in patients’ response to various forms of systemic treatments such as immunotherapy and chemotherapy for different cancers,” says Dr. Maleki.

Dr. John Lenehan, Dr. Jeremy Burton and Dr. Saman Maleki
This unique study will happen in three stages. The first stage is an observational study to examine fecal samples of 52 patients at LRCP with advanced pancreatic cancer. The second stage will focus on using the samples from these patients in preclinical models to test new combinations of treatments. The final stage of the study will focus on intervention through human clinical trials by modifying a patient’s microbiome with something called a fecal transplant prior to treatment.
“The microbiome is involved in many aspects of cancer development and these organisms aren’t just living in the gut but also within the tumor,” says Dr. Michael Silverman, Lawson Scientist and Chair/Chief of Infectious Diseases at LHSC and St. Joseph’s Health Care London. “We believe that by giving people a fecal transplant, we can change the bacteria that live within the tumor and gut and then optimize the immune response to both the tumour and to treatment, with the goal of improving patient outcomes.”
Dr. Michal Silverman, Lawson Associate Scientist
Fecal transplants involve collecting stool from a healthy donor, preparing it in a lab and safely transplanting it to the patient, in this case with a capsule. The goal is to transplant the donor’s microbiome so that healthy bacteria will colonize in the patient’s gut. “If you think of microbiome, each bacterium is like a little factory and all together they are a giant factory within us producing things we need,” explains Dr. Jeremy Burton, Lawson Scientist who specializes in human microbiome research. “Over time, a person’s diet, medications, and lifestyle can change the microbiome and it can have a big impact to the rest of our body.”
The research team was recently awarded a $450,000 Catalyst 2021 grant from the Weston Family Foundation to conduct this study, which is the first in the world focusing on prospectively modifying the microbiome in pancreatic cancer patients for treatments and outcomes.
“We normally don’t see this in one study where we go through the full spectrum of learning from patients, to looking at treatments, and then moving to a final intervention stage,” explains Dr. Maleki. “This has not been tried in pancreatic cancer before, but we think leveraging the microbiome and improving the immune response can potentially move the needle in this patient population.”
The team is recruiting both pancreatic cancer patients, as well as healthy volunteers for fecal transplant samples. Those interested in helping with fecal transplant donations can contact Dr. Seema Parvathy at 519-646-6100 ext. 61726 or email seemanair@@email
New transportation resource for youth in crisis
LONDON, ON – Transitional aged youth in Middlesex County now have access to a free transportation resource to access mental health services. Called the County Transport initiative, it will help youth ages 16 to 25 in Lucan, Parkhill, Exeter and Strathroy-Caradoc get the mental health care they need, when they need it.
County Transport is being coordinated by MINDS of London-Middlesex, a program of Lawson Health Research Institute, in partnership with the Canadian Mental Health Association (CMHA) of Elgin-Middlesex, Star Taxi and Middlesex County through the Lucan and Parkhill Libraries.
“Through our collaborative work, we’ve heard from many youth that transportation is a barrier for them when trying to access mental health services when in crisis. Youth in rural areas find this very challenging since most services are not close to their location,” says Romaisa Pervez, Research Assistant at MINDS of London-Middlesex.
MINDS, a Mental Health INcubator for Disruptive Solution, is a social innovation lab with a mission to address the complexity of the mental health care system. Youth with lived experience, community members and researchers work together to understand and help those living with mental health challenges in London-Middlesex by designing, piloting and testing innovative solutions developed locally.
“We do not have the exact numbers of Transitional Aged Youth (TAY) living in rural Middlesex who would benefit from access to the County Transport Initiative, but we know that mental health services in rural communities are limited and that access to the services available in larger city centres is challenging due to transportation difficulties,” explains Cathy Burghardt-Jesson, Warden for Middlesex County. “Transportation from Middlesex to London, where the majority of mental health resources are located, is underdeveloped as there are limited bus routes and schedules. This leaves little in the way of affordable transit options for TAY in crisis.”
Youth in crisis who connect with CMHA’s Reach Out 24/7 line at www.reachout247.ca or by phone at 519-433-2023 will be supported and assessed by the Crisis Line staff. If it is determined that a visit to the London Crisis Centre is needed, the CMHA Crisis worker will ensure a smooth transition from the Crisis Line to the Star Taxi Service. The youth will be provided with free transportation to and from CMHA’s Mental Health and Addictions Crisis Centre located at 648 Huron Street.
To ensure the safety and wellbeing of the youth accessing this service, Star Taxi drivers have received training developed by CMHA regarding mental health and crisis de-escalation, as well as suicide prevention training by Living Works.
Funding for the initiative has been provided by St. Joseph’s Health Care Foundation and the generous support of individual donors in the community.
“With additional funding, the initiative could be scaled up to reach as many youth as possible in Middlesex County and beyond. We want to see all youth in rural areas who want to access mental health services able to do so, by removing the barriers of location and transportation,” adds Pervez. They will be collecting information regarding use of the transportation service and youth experience to refine and improve the initiative.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New transportation resource for youth in crisis
Transitional aged youth in Middlesex County now have access to a free transportation resource to access mental health services. Called the County Transport initiative, it will help youth ages 16 to 25 in Lucan, Parkhill, Exeter and Strathroy-Caradoc get the mental health care they need, when they need it.
County Transport is being coordinated by MINDS of London-Middlesex, a program of Lawson Health Research Institute, in partnership with the Canadian Mental Health Association (CMHA) of Elgin-Middlesex, Star Taxi and Middlesex County through the Lucan and Parkhill Libraries.
“Through our collaborative work, we’ve heard from many youth that transportation is a barrier for them when trying to access mental health services when in crisis. Youth in rural areas find this very challenging since most services are not close to their location,” says Romaisa Pervez, Research Assistant at MINDS of London-Middlesex.

Romaisa Pervez, Research Assistant at MINDS of London-Middlesex, is leading the County Transport initiative.
MINDS, a Mental Health INcubator for Disruptive Solution, is a social innovation lab with a mission to address the complexity of the mental health care system. Youth with lived experience, community members and researchers work together to understand and help those living with mental health challenges in London-Middlesex by designing, piloting and testing innovative solutions developed locally.
“We do not have the exact numbers of transitional aged youth living in rural Middlesex who would benefit from access to the County Transport Initiative, but we know that mental health services in rural communities are limited and that access to the services available in larger city centres is challenging due to transportation difficulties,” explains Cathy Burghardt-Jesson, Warden for Middlesex County.
“Transportation from Middlesex to London, where the majority of mental health resources are located, is underdeveloped as there are limited bus routes and schedules. This leaves little in the way of affordable transit options for youth in crisis.”
Youth in crisis who connect with CMHA’s Reach Out 24/7 line at www.reachout247.ca or by phone at 519-433-2023 will be supported and assessed by the Crisis Line staff. If it is determined that a visit to the London Crisis Centre is needed, the CMHA Crisis worker will ensure a smooth transition from the Crisis Line to the Star Taxi Service. The youth will be provided with free transportation to and from CMHA’s Mental Health and Addictions Crisis Centre located at 648 Huron Street.
To ensure the safety and wellbeing of the youth accessing this service, Star Taxi drivers have received training developed by CMHA regarding mental health and crisis de-escalation, as well as suicide prevention training by Living Works.
Funding for the initiative has been provided by St. Joseph’s Health Care Foundation and the generous support of individual donors in the community.
“With additional funding, the initiative could be scaled up to reach as many youth as possible in Middlesex County and beyond. We want to see all youth in rural areas who want to access mental health services able to do so, by removing the barriers of location and transportation,” adds Pervez.
They will be collecting information regarding use of the transportation service and youth experience to refine and improve the initiative.
New urinary microbiome study could be first step in providing personalized care to patients with ureteral stents
LONDON, ONTARIO - For patients with kidney stones, ureteral stents (hollow devices placed in the ureter – the tube between the kidney and bladder) can be used temporarily to relieve urinary obstruction. Despite the use of antibiotics, ureteral stents often become encrusted with minerals and coated with bacteria. This can lead to complications like infection and the need for replacement surgery.
Published today in Cell Reports Medicine, researchers at Lawson Health Research Institute and Western University conducted a novel microbiome study to examine bacteria associated with ureteral stents. They found that nearly all the stents, whether visibly coated or not, had unique bacterial profiles that were most associated with a patient’s medical condition rather than antibiotic use. For patients with ureteral stents, they may benefit from a personalized approach to care and antibiotic treatment.
The study included 241 patients from St. Joseph’s Health Care London. The research team collected and analyzed patient urine samples and ureteral stents following surgical removal, as well as relevant patient information such as antibiotic use and history of infections.
“We wanted to know which bacteria were present and whether the bacteria found in urine samples corresponded to the bacteria found on a patient’s stent,” explains Dr. Kait Al, Postdoctoral Fellow at Lawson and at Western’s Schulich School of Medicine & Dentistry. “We found that there was a bacterial community present on almost all stents, even if they were not visibly affected, and that it differed from the bacterial community found in a patient’s urine.”
These findings challenge long-held beliefs that the urinary tract is a sterile environment devoid of bacteria.
The study revealed that the bacteria present were determined by an individual patient’s medical condition. They differed significantly based on comorbidities like irritable bowel syndrome, obesity and hypertension. Antibiotic use within the past 30 days did not seem to have an effect on the types of bacteria detected on the stents.
“While more research is needed, our study suggests that antibiotic use during the placement of these stents could one day be more conservative or targeted based on each patient’s condition,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The team also discovered that in patients needing multiple stents, the bacterial community remained stable over time, suggesting that infections on a patient’s previous stent could direct the course of treatment for their future device placements.
“This is the largest study of its kind, investigating bacteria both in urine and adhered to ureteral stents,” states Dr. Hassan Razvi, Urologist at St. Joseph’s, Lawson Associate Scientist and Professor at Schulich Medicine & Dentistry. “We hope this will be the first step towards personalized care, ultimately leading to fewer stent-associated infections.”
The study was made possible through the generous support of The W. Garfield Weston Foundation and St. Joseph’s Health Care Foundation.
-30-
DOWNLOADABLE MEDIA

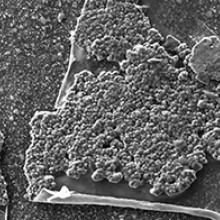
Scanning electron microscopy images showing organic material, crystals, and bacteria present on the surface of the ureteral stents.
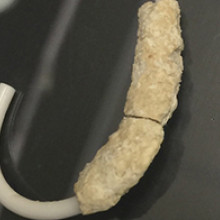
Recovered ureteral stent encrusted with minerals and bacteria.
See all Lawson Media Releases
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
New urinary microbiome study could be first step in providing personalized care to patients with ureteral stents
For patients with kidney stones, ureteral stents (hollow devices placed in the ureter – the tube between the kidney and bladder) can be used temporarily to relieve urinary obstruction. Despite the use of antibiotics, ureteral stents often become encrusted with minerals and coated with bacteria. This can lead to complications like infection and the need for replacement surgery.
Published today in Cell Reports Medicine, researchers at Lawson Health Research Institute and Western University conducted a novel microbiome study to examine bacteria associated with ureteral stents. They found that nearly all the stents, whether visibly coated or not, had unique bacterial profiles that were most associated with a patient’s medical condition rather than antibiotic use. For patients with ureteral stents, they may benefit from a personalized approach to care and antibiotic treatment.

The study included 241 patients from St. Joseph’s Health Care London. The research team collected and analyzed patient urine samples and ureteral stents following surgical removal, as well as relevant patient information such as antibiotic use and history of infections.
“We wanted to know which bacteria were present and whether the bacteria found in urine samples corresponded to the bacteria found on a patient’s stent,” explains Dr. Kait Al, Postdoctoral Fellow at Lawson and at Western’s Schulich School of Medicine & Dentistry. “We found that there was a bacterial community present on almost all stents, even if they were not visibly affected, and that it differed from the bacterial community found in a patient’s urine.”
These findings challenge long-held beliefs that the urinary tract is a sterile environment devoid of bacteria.
The study revealed that the bacteria present were determined by an individual patient’s medical condition. They differed significantly based on comorbidities like irritable bowel syndrome, obesity and hypertension. Antibiotic use within the past 30 days did not seem to have an effect on the types of bacteria detected on the stents.
“While more research is needed, our study suggests that antibiotic use during the placement of these stents could one day be more conservative or targeted based on each patient’s condition,” says Dr. Jeremy Burton, Lawson Scientist and Associate Professor at Schulich Medicine & Dentistry.
The team also discovered that in patients needing multiple stents, the bacterial community remained stable over time, suggesting that infections on a patient’s previous stent could direct the course of treatment for their future device placements.
“This is the largest study of its kind, investigating bacteria both in urine and adhered to ureteral stents,” states Dr. Hassan Razvi, Urologist at St. Joseph’s, Lawson Associate Scientist and Professor at Schulich Medicine & Dentistry. “We hope this will be the first step towards personalized care, ultimately leading to fewer stent-associated infections.”
The study was made possible through the generous support of The W. Garfield Weston Foundation and St. Joseph’s Health Care Foundation.
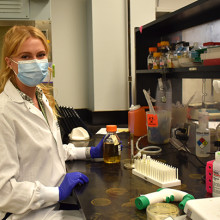
Dr. Kait Al, Postdoctoral Fellow at Lawson and Schulich Medicine & Dentistry
noteWORTHY – Teamwork and patients inspire clinical research assistant
St. Joseph’s celebrates people who provide exceptional care, grow stronger communities and contribute to a healthier world. Today, meet Heather LaPier, a clinical research assistant whose work helps keep clinical research running smoothly for four Lawson research scientists in diabetes and nephrology. She is a liaison among patients, researchers, clinicians, ethicists, regulatory bodies and pharmaceutical companies.
What values or people inspire your work:
I couldn’t ask for better than the physicians and researchers I work with. It’s a true team. We can bring our own ideas and expertise and know that we’re valued. We’re all good at showing appreciation for each other.
Best part of your workday:
Visiting with people receiving dialysis. They have treatment four hours a day, three times a week, so they’re used to talking with physicians and staff and we get to know them really well. They’re honest and funny – and, despite living with a chronic illness, they’re some of the most positive people I’ve ever met.
What one thing do you wish people knew about your work?
Our job is to advocate for patients and protect them, so every study is carefully designed, planned, regulated and monitored. We work to find solutions to patients’ health issues, and that means putting them first.
One big thing people should know is that participants in clinical trials and research studies get extra care and attention. Other patients have regular appointments, maybe every six months, but as a participant in research they’ll have even more frequent monitoring. So even though they’re helping advance medical knowledge generally and there’s no certainty of direct benefit to them from a specific clinical trial, they do have a whole team of people fully involved in their current care. Any time they have a question, they have direct access to an endocrinologist or nephrologist.
Why this work is meaningful to you:
It’s definitely exciting and always interesting. It can be easy to get caught up in the day-to-day tasks – but I never want to lose sight of the fact patients are living longer and better lives because of the work we’re doing. I have a front-row seat when patients come in for visits and tell us a diabetes treatment or a dialysis intervention is making them feel better.
Back-story:
My mom has been a nurse for over 30 years, so I grew up in a home where we talked about health and patient care a lot. We have a shared language. After my university degree, I applied to college for either forensic science or clinical research. I’m so glad clinical research is where I landed.
One other thing:
I love learning about the history of the Second World War, specifically naval ships and naval battles. It seems totally random, but I studied it as one of my non-science courses in university. I still find it fascinating.
Well said:
Heather is a true gem – highly skilled, creative, and an outstanding team player who expertly manages multiple research projects and investigators. She has been a game-changer for diabetes, metabolic, and chronic disease research at Lawson Research Institute, supporting everything from qualitative studies to large randomized-controlled trials with innovative designs. Our successes wouldn’t have been possible without her.
- Dr. Kristen Clemens, St. Joseph’s endocrinologist and Lawson Research Institute scientist

