Search
Search
Study examines new forms of treatment for those suffering from post-traumatic stress disorder
Researchers looking to better personalize treatment for PTSD
MEDIA RELEASE
For immediate release
January 25th, 2022
LONDON, ON – Post-traumatic stress disorder (PTSD) is a condition that often develops in those who have experienced a traumatic event. PTSD affects close to 10 per cent of Canadians, and in some cases, can be difficult to treat.
In a new study through Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from PTSD.
“In our study we are looking at ways of trauma processing at the foundation of the stress response,” explains Dr. Ruth Lanius, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry. “When you are faced with a stressor the first thing you do is turn your attention to it, and when you do that you engage your head and neck muscles.”
DBR was developed by Scottish psychiatrist Dr. Frank Corrigan and focuses on the muscles of the shoulders, neck, head and face of patients when recalling a traumatic event. This form of trauma processing starts right at the moment the stressor is noticed by the individual, which is often quickly followed by a moment of shock. By addressing the stressor at this level, doctors can target the foundation of where the stress response begins.
“When patients bring up a trigger in their mind, we look at what happens in terms of the tension in their head and neck. We process that gently by asking the patient to notice and stay with that tension without trying to release it, and over time the tension usually decreases,” explains Dr. Lanius, who is also a Psychiatrist at London Health Sciences Centre. “The second part involves addressing the shock response. You turn your attention to the stressor and then notice any moments of shock that follows, which is often associated with tension behind the eyes and in the shoulders. Finally, you address the visceral sensations associated with feelings and emotions associated with the stressor.”
Dr. Lanius believes that by using DBR and focusing on muscle and visceral responses, it will help patients suffering from PTSD to process the visceral feelings associated with the trauma and its triggers.
“After this form of treatment, patients often say they feel safer and don’t see themselves negatively, like they did in the past,” says Dr. Lanius. “This is because we change those intense visceral feelings and it allows the person to reevaluate who they are and how they interact with the world.”
The research team is hoping to recruit approximately 60 people to take part in the DBR study. Participants will undergo a psychological interview and an MRI, then eight sessions of treatments. Following those sessions, participants will have another interview and MRI to assess if any positive changes were made within the neurological networks and/or in psychological systems.
“Our hopes are to really personalize treatment for those living with PTSD,” says Dr. Lanius. “Some people have difficulty tolerating some forms of trauma processing and in my experience this treatment is a gentler approach for those individuals.”
Interested participants who have been diagnosed with PTSD can contact Suzy Southwell, Research Coordinator, at 519-685-8500 ext. 35186 or @email.
MEDIA CONTACT
Celine Zadorsky, Communications & External Relations, Lawson Health Research Institute, T: 519-685-8500 ext. 75664, C: 519-619-3872
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world.
ABOUT WESTERN
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
ABOUT THE SCHULICH SCHOOL OF MEDICINE & DENTISTRY
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study examining moral injury in health care workers is focusing on functional brain changes
LONDON, ON – For many health care workers, the past year and a half of the COVID-19 pandemic has taken a toll on their mental health. Recognizing this is a growing concern, a London research team from Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry is examining moral injury amongst health care workers by imaging the effects on the brain.
“We are trying to look closely at what happens in the brain when a person recalls a moral injury event,” says Dr. Ruth Lanius, Associate Scientist at Lawson and Professor at Western’s Schulich School of Medicine & Dentistry. “By understanding the changes happening in the brain, we may be better able to treat individuals suffering from moral injury.”
Moral injury refers to an injury to an individual’s moral conscious which can produce profound emotional guilt and shame. During this ongoing pandemic, some health care workers have experienced emotionally difficult situations that resulted in moral injury.
“Those suffering from moral injury have a cognitive or thinking component which may include repeated thoughts that they didn’t provide the best care for example, or that they let their family down do to their intense work schedule or need to self-isolated,” explains Dr. Lanius, who is also a psychiatrist at London Health Sciences Centre (LHSC). ‘These thoughts are coupled with intense visceral distress, a gnawing sensation in the stomach or the feeling like one is being eaten up inside. I think once we help resolve the visceral distress, we will also see the negative thinking patterns settle down.”
The new study will involve around 60 health care workers. These research participants will undergo a functional MRI scan at St. Joseph's Health Care London at the beginning of the study and have the option to receive eight weeks of treatment. Then, another MRI scan will be done to see if and how the moral injury changes and possibly resolves within the brain. “This can be very validating for the health care workers since brain scans can make the invisible wound of moral injury visible,” adds Dr. Lanius.
The research team’s goal is to better understand what networks of the brain are activated with moral injury. Dr. Lanius hopes this would help establish more neuroscientifically guided treatments. “We have to help our health care workers heal from the tremendous hardships they often endure.”
Health care workers are still being recruited for this study. Interested participants can contact Research Coordinator Suzy Southwell 519-685-8500 ext. 35186 or @email.
See all Lawson Media Releases
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study reveals clinical factors linked to reduced mortality in injection drug users with heart valve infection
Cases of endocarditis – infection of the heart valves – have risen dramatically in recent years as a result of the opioid crisis. In London, Ontario 55 per cent of people who experience heart valve infections are injection drug users. They are particularly vulnerable to the disease and a third die as a result.
In an effort to improve outcomes, researchers at Lawson Health Research Institute and Western University are studying which clinical factors are associated with improved survival in this patient population. In a new study, they showed that both surgery and in-hospital addictions counselling are linked to significantly reduced mortality in injection drug users with first-episode endocarditis. Surgery was associated with a 56 per cent reduction in mortality, while in-hospital addictions counselling was associated with a 72 per cent reduction.
The project was a retrospective cohort study that examined anonymous patient data from 2007 to 2016 at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. Of 370 patients with first-episode endocarditis, 202 were persons who inject drugs. Of those 202 patients, 39 had cardiac surgery at LHSC and 40 were referred for addictions counselling to start in while they were still in-hospital.
The study found that patients who received surgery experienced a 56 per cent reduction in mortality. Patients who received surgery were normally the most severely ill and most in need. While additional studies are necessary, the researchers point to these findings as a reason for cardiac surgery to be considered as a viable treatment option in carefully selected patients.
“In the past, many centres have not performed cardiac surgery in patients who inject drugs due to concerns about poor outcomes. Continued injection drug use was viewed as a risk for reinfection,” says Dr. Michael Silverman, author of the study, Lawson scientist and Chair/Chief of Infectious Diseases for Western’s Schulich School of Medicine & Dentistry, LHSC and St. Joseph’s. “Our study challenges those beliefs. It shows that when we account for the severity of a patient’s illness, they’re more likely to survive with surgery.”
Patients who were referred for addictions counselling while in-hospital experienced a 72 per cent reduction in mortality. Addictions counselling was provided by a consultant who would meet with patients to provide education on risks for infection, harm reduction strategies and support towards addictions recovery, including referral to community supports.
The study’s authors point out that, in other centres, patients are not commonly referred for addictions counselling while still being treated for an acute infection. It is commonly believed they are too ill to undergo this type of therapy. The more common approach is to treat the infection and refer patients for addictions counselling after discharge.
“Education and support for these patients is critical. The majority of the patients I see don’t understand what they’re doing to cause an infection and may be highly motivated to undertake a lifestyle change,” says Dr. Sharon Koivu, author of the study, Lawson scientist, associate professor at Schulich Medicine & Dentistry and palliative-care physician at LHSC. “This study shows the importance of working with patients towards harm reduction and addiction recovery while they’re still being treated in-hospital.”
London’s rates of endocarditis in persons who inject drugs are significantly higher than other regions. While injection drug users account for 55 per cent of all heart valve infections in London, they account for only 8 to 12 per cent in large studies in the United States. To address this issue, the research team is conducting a number of additional studies. Current projects are exploring the reasons behind such high local rates and the best strategies for treatment, including antibiotic and surgical interventions.
“We don’t often get a chance to look at large numbers of this particular patient population but there is a plethora of local data available,” says Dr. Laura Rodger, author of the study and a resident physician at Schulich Medicine & Dentistry and LHSC. “Our team wants to bring meaning to that data by asking the right questions to ultimately improve patient outcomes.”
The study, “Clinical Characteristics and Factors Associated with Mortality in First-Episode Infective Endocarditis Among Persons Who Inject Drugs,” is published in JAMA Network OPEN.
Study shows a decline in Veterans’ mental health throughout the pandemic
MEDIA RELEASE
For immediate release
February 16th, 2022
LONDON, ON – In newly-published findings from Lawson Health Research Institute, more than half of Canadian Veterans report a decline in their mental health over the course of the COVID-19 pandemic.
When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population.
“We anticipated the ongoing pandemic would have impacts to multiple domains of life such as loneliness, isolation, depression and PTSD,” says Associate Scientist at Lawson and the MacDonald Franklin Operational Stress Injury (OSI) Research Centre, Dr. Anthony Nazarov.
To examine the potential impacts the research team launched a longitudinal study in early 2021, recruiting Canadian Veterans and spouses of Canadian Veterans. A total of 1,136 Veterans have participated in the study which spans over 18 months. Participants complete online questionnaires every three months, with questions focused on mental health and virtual health care services.
“We looked at use of care services, including virtual care services, which we know have been on the rise during the pandemic,” says Lawson Associate Scientist and Scientific Director of the Macdonald Franklin OSI Research Centre, Dr. Don Richardson.
The team recently published preliminary findings based on the Veterans portion of the study, which confirm a decline in mental health amongst the Veterans that took part.
“One of the important preliminary findings demonstrated a little more than 55 per cent of Veterans (55.9 per cent) have indicated that their mental health has worsened over the pandemic.” explains Dr. Richardson.
The findings also revealed that nearly one in five Veterans used virtual health care and telepsychiatry services and found them to be helpful.
“Veterans have been having positive experiences with virtual care for mental health support,” adds Dr. Nazarov. “Most found it helpful, and more importantly, many would like to continue to use this form of health care services even post pandemic.”
The preliminary study findings have been published in the European Journal of Psychotraumatology. The longitudinal study will wrap up this summer, and then the team hopes to use the information to improve and innovate different forms of mental health supports for Veterans and their spouses in the future.
-30-
About Lawson Health Research Institute: Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
For more information, please contact:
Celine Zadorsky
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C. 519-619-3872
@email
www.lawsonresearch.ca/news-events
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study shows fewer higher-dose radiation treatments safe and well tolerated by women with uterine cancer
MEDIA RELEASE
FOR IMMEDIATE RELEASE
Sunnybrook Health Sciences Centre and Lawson Health Research Institute
April 14, 2022
LONDON,ON - Five high-dose radiation treatments targeting uterine cancer rather than the current standard 25 treatments are safe and well-tolerated by patients, a new study published in JAMA Oncology has found.
SPARTACUS (Stereotactic Pelvic Adjuvant Radiation Therapy in Cancers of the Uterus) — a multi-institutional non-randomized controlled trial — looked to assess the feasibility and safety of using a specialized technique called stereotactic body radiation therapy (SBRT) for women with uterine cancer where instead of 25 treatments over five weeks, five treatments can be delivered over 1.5 weeks.
SBRT uses many precise beams of radiation to target tumours or cancerous cells. It uses a higher dose of radiation in a smaller number of treatments. It can be done on a standard linear accelerator, the machine that delivers radiation treatments.
Sixty-one women were enrolled in SPARTACUS at two centres — Sunnybrook Health Sciences Centre and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC).
“Uterine cancer is a common cancer in women, usually treated with surgical removal followed by radiation and/or chemotherapy to reduce the risk of recurrence,” said Dr. Eric Leung, radiation oncologist at Sunnybrook’s Odette Cancer Centre. “External beam radiation is usually given over five weeks, and that can place a heavy burden on women who have to travel to a radiation centre every day, spend time away from home and work, and incur the financial burden of these factors as well.”
With a median follow-up of nine months, the patients enrolled in SPARTACUS reported an acceptable level of side effects from the radiation that resolved, and also reported a reasonable quality of life during treatment, Dr. Leung said.
“We were interested in examining the toxicity of the higher dose – would it affect the nearby bowels or bladder and place a heavy symptom burden on patients? We were pleased to find that patients reported their symptoms as manageable.”
“This study represents a novel way of treating uterine cancer in a shorter time. It was conducted mainly through the COVID pandemic and gave women a chance to receive treatment in less time with fewer visits to our centres,” said Dr. David D’Souza, radiation oncologist at LHSC and the study co-lead through Lawson Health Research Institute.
Patients will continue to be followed on the study for late side effects and further research is planned to further compare this more convenient schedule to the standard five-week course of radiation.
“This novel treatment could lead to a practice change that places less burden on patients and on the healthcare system,” Dr. Leung said. “Delivering radiation over the course of a week and half rather than over five weeks for patients facing uterine cancer would open up healthcare resources by reducing visits and usage of the linear accelerators.”
-30-
ADDIONAL QUOTES – Dr. David D’Souza:
“Giving radiation in a shorter time can have several advantages for both the patient and the health care system."
“Our study assessed the safety of delivering a higher dose of radiation in fewer treatments for patients with uterine cancer by adapting what has successfully been done for other types of cancer in the pelvis like prostate and rectal cancer.”
“This study was made possible with advances in treatment planning, radiation machine capabilities, and an outstanding radiation therapy program at LRCP.”
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
ABOUT SUNNYBROOK HEALTH SCIENCES CENTRE
Sunnybrook Health Sciences Centre is inventing the future of health care for the 1.2 million patients the hospital cares for each year through the dedication of its more than 10,000 staff and volunteers. An internationally recognized leader in research and education and a full affiliation with the University of Toronto distinguishes Sunnybrook as one of Canada’s premier academic health sciences centres. Sunnybrook specializes in caring for high-risk pregnancies, critically-ill newborns and adults, offering specialized rehabilitation and treating and preventing cancer, cardiovascular disease, neurological and psychiatric disorders, orthopaedic and arthritic conditions and traumatic injuries. The Hospital also has a unique and national leading program for the care of Canada’s war veterans.
Media Contacts:
Celine Zadorsky
Communications & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C: 519-619-3872
@email
Sunnybrook Health Sciences Centre
Communications & Stakeholder Relations
416-480-4040
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Supporting a rapid research response during the pandemic
LONDON, ON – Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Supporting a rapid research response during the pandemic
Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
Congratulations to all of the researchers and their teams who have been awarded funding:
- Dr. Ian Ball - Predictors of clinical deterioration in hospitalized patients with COVID-19: The CORAL study
- Dr. Doug Fraser - Translational Research Centre: Repository of biological specimens from patients
- Dr. Sean Gill - Rapid identification of therapeutic targets mediating pulmonary microvascular endothelial cell dysfunction in COVID-19 patients
- Dr. Marnin Heisel - Testing Online Meaning-Centered Men’s Groups to Promote Psychological Well-Being and Reduce Despair in the Face of the COVID-19 Pandemic
- Dr. Kimia Honarmand - The impact of the COVID-19 pandemic on frontline healthcare workers: A Southwest Ontario survey
- Dr. Michael Knauer - Improving diagnostic and epidemiologic detection of SARS-CoV-2
- Dr. Jim Koropatnick - Targeting the SARS-CoV-2 receptor with candidate antisense drugs to prevent infection and disease progression
- Dr. Eldon Loh - COVID-19 and Disability: The Impact of a Societal Lockdown on those with Spinal Cord and Brain Injuries
- Dr. Len Luyt - Stapled Peptides as SARS-CoV-2 Fusion Inhibitors
- Dr. Claudio Martin - COVIDOPATHY – An observational study of coagulation abnormalities in patients with COVID-19
- Dr. Tianqing Peng - Developing new ssDNA aptamers targeting S protein receptor binding domain of SARS-CoV-2 to disrupt virus infection cycle as a potential therapy
- Dr. Eva Turley - Hyaluronan signaling through the inflammasome is a target for blunting acute respiratory distress syndrome (ARDS) in COVID-19 patients
- Dr. Ruud Veldhuizen - Next generation exogenous surfactants for COVID-19 and future respiratory pandemics
- Dr. Blayne Welk - Characterizing the burden of surgical care in COVID-19 positive patients
Symposium features research on health through food and microbes
The past decade has featured rapid acceleration in the study of microbes and how they influence human and planetary health. This includes the study of probiotics and their diverse benefits.
On Friday, May 4, Lawson Health Research Institute (Lawson) and Western University hosted a free public symposium on health through food and microbes.
With more than 80 attendees, the symposium covered dynamic areas of research that are collectively impacting society and human wellbeing. These include the critical role of honey bees in pollination, bioremediation of toxic compounds, fermented food, maternal and infant nutrition and how microbes can confer a range of health benefits. The topics included a view of life in developing countries and efforts to help people overcome many challenges.
The event was opened by Dr. Bing Gan, Lawson scientist, plastic surgeon at St. Joseph's Health Care London and professor at Western’s Schulich School of Medicine & Dentistry, who described his harrowing experience working for Doctors Without Borders in the Congo.
“We live in a microbial world, and beneficial ones are essential to the future of our planet and for human wellness and longevity,” says Dr. Gregor Reid, a scientist at Lawson, professor at Western’s Schulich School of Medicine & Dentistry and lead organizer of this symposium. “The highly respected speakers at this event highlighted the potential for microbes to improve global health, and reminded us of the fragility of life on this planet.”
The event was made possible by a grant from the Gairdner Foundation for a lecture titled, “Food for 9.7 billion people,” by Dr. Rob Vos, Director Markets, Trade and Institutions, International Food Policy Research Institute, Washington, DC. The lecture was delivered by Dr. Reid as Dr. Vos unfortunately experienced travel delays.
The event also featured locally produced fermented foods provided by Booch and Nuts For Cheese.
Team players: FMT and microbiome research could have widespread impact
There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson Health Research Institute, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system.
FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis.
FMT is already in clinical use for the treatment of C. diff (Clostridium difficile), and in addition to showing promise in the treatment of other diseases, it is also being studied as a way to improve response to existing cancer treatments and ease treatment side effects.
Dr. Saman Maleki, a Scientist at Lawson Health Research Institute and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC), says they’ve just begun to explore the possibilities.
"We are just starting to study FMT as an intervention outside its traditional use in patients with C. difficile infection, and we will be expanding to other areas, particularly in cancer.”
FMT can overhaul a patient’s microbiome, Dr. Maleki explains, and a healthy microbiome is beneficial especially when a treatment is trying to activate the body’s immune system.
Dr. Michael Silverman, Lawson Associate Scientist and Medical Director of St. Joseph’s Health Care London’s Infectious Diseases Care Program, is a pioneer in the field of FMT. He has been performing the procedure since 2003 with C. difficile patients and was one of the first in North America to do so. He sees a wide range of possible applications.
“FMT has enormous potential in being an important adjunctive therapy in many cancers. It may, for example, help cancer patients respond to immunotherapy,” says Dr. Silverman, who is also Chair/Chief of Infectious Disease at St. Joseph’s Health Care London, LHSC and Western University. “The potential to impact autoimmune and metabolic diseases is also quite exciting, but still in early development.”
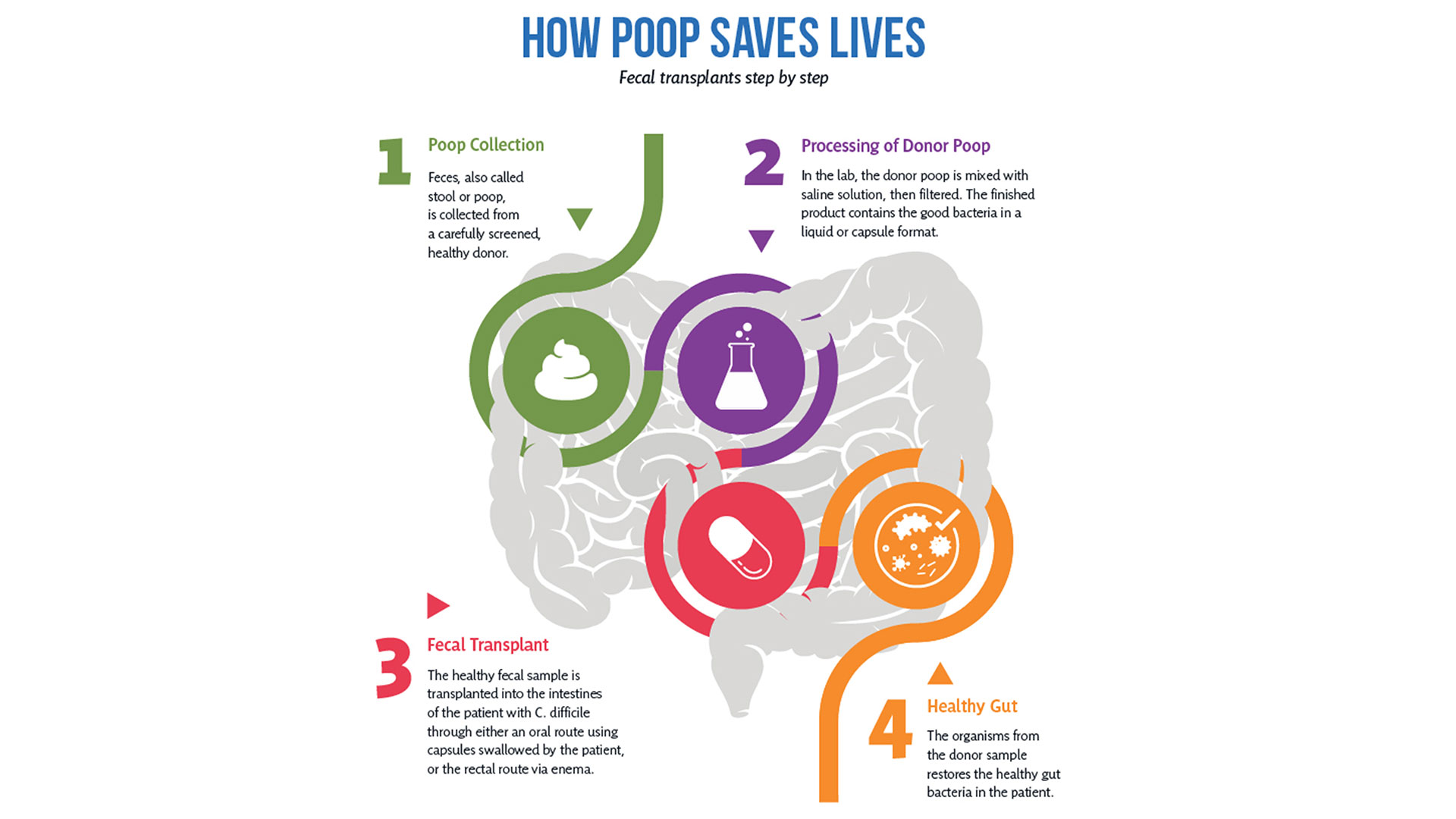
So how does it work?
After rigorous screening, stool from a healthy donor is collected and then processed in a lab into a liquid or capsule containing the good bacteria, which can then be administered to a patient’s gastrointestinal tract.
The Lawson team is also one of few delivering FMT using specially-prepared oral capsules. Introduced in 2018, they have been a game changer in patient acceptance and ease of administration, according to Research Coordinator Dr. SeemaNair Parvathy, who has been coordinating the program since 2015.
“There is a link between the fitness of the intestinal microbiome and the fitness of the immune system,” says Dr. John Lenehan, Associate Scientist at Lawson and Medical Oncologist at LHSC. “A ‘healthy’ microbiome leads to a more robust immune response when using immunotherapy. FMT from a healthy donor is expected to improve the fitness of the recipient’s intestinal microbiome and promote a better immune response.”
People with chronic disease can often experience what’s called a ‘leaky gut,’ allowing food, bacterial and microbial components to pass through the intestinal wall, negatively impacting the immune system.
“When people get FMTs their intestinal permeability improves – meaning it actually reduces,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at Lawson and St. Joseph’s. “What changes that intestinal permeability? The microbes at the site. They play a role in interacting with the host cells, providing nutrients and vitamins.”
With the immune system so closely tied to the health of the microbiome, it’s not surprising scientists are exploring how strengthening one can have a big impact on the other.
Boosting immunotherapy
Immunotherapy can be used to either stimulate or suppress the immune system to help the body fight disease, and FMT is showing promise in reducing resistance to the treatment.
While immunotherapy has been effective in treating a number of cancers – the number one cause of death in Canada – not all patients respond to the treatment.
But early work presented at a conference by the Lawson team for the Journal for ImmunoTherapy of Cancer has shown that using FMT to modify the microbiome could reduce resistance to immunotherapy. The study involved patients from LHSC with advanced melanoma, a type of skin cancer.
While in the very early stages, the combination of FMT and anti-PD1 immunotherapy has been found to be safe, and it appears that FMT could make tumours more responsive to the immunotherapy treatment.
“Microbiome-based treatment strategies, including FMT, have a high potential in oncology,” says Dr. Maleki. “Our team is also exploring its potential in treating pancreatic cancer.”
The research is so interesting that a recent Nature article listed the Phase I melanoma trial as “seminal” research. The study was also unique in that it used healthy donors, as opposed to donors who had previously responded to immunotherapy treatment.
A separate Lawson study with LHSC patients with metastatic renal cell carcinoma, a type of kidney cancer, published in the Journal of Clinical Oncology, also looked at combining immunotherapy and FMT to ease the adverse effects of the treatment.
The Phase I study, led by Dr. Maleki and Dr. Ricardo Fernandes, Medical Oncologist at LHSC, found adding FMT to doublet immunotherapy was safe, but further study is needed to determine whether it could bring about changes in the microbiome and immune system.
Dr. Lenehan says Lawson researchers are in a position to be leaders in this field in the near future for two reasons.
“One is that other academic researchers have not been able to assemble the expertise, and some who have, do not have the access to healthy donor stool. The second is that some biotechnology companies are interested in FMT, but almost exclusively for C. difficile infections.”
Autoimmune, metabolic and other illnesses
Two other areas that have seen recent advances include FMT for the treatment of non-alcoholic fatty liver disease (NAFLD) and multiple sclerosis.
“The gut microbiome is very important in the metabolism of foods and metabolic products. It can therefore have a major effect on obesity and atherosclerosis,” says Dr. Silverman. “It also is tightly involved in regulating the immune system and therefore moderating the microbiome may potentially impact autoimmune diseases.”
A study published in 2020 by the team in The American Journal of Gastroenterology showed that FMT appears to reduce intestinal permeability in patients with NAFLD.
The number of people with NAFLD is growing rapidly and studies show patients have different microbiota than healthy persons.
The trial included 21 NAFLD patients from LHSC and St. Joseph’s. While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Metabolic syndromes including obesity and its complications of NAFLD and atherosclerosis are massive public health problems. Any impact on these would be of huge importance,” Dr. Silverman adds. “Autoimmune diseases also cause major morbidity and mortality. We have a lot of work to do before we can consider FMT as a routine therapy for any of these conditions, but the long-term promise is great.”
Research into the use of FMT for treatment of patients with multiple sclerosis is in the very early stages. But patients with MS show a difference in gut microbiota and higher small intestine permeability, which could contribute to the development of the disease.
A Phase I trial by the Lawson team published in the Multiple Sclerosis Journal – Experimental, Translational and Clinical, found FMT to be safe and tolerable.
While the study was very small, MS patients treated with FMT were found to have beneficial changes to gut microbiota and intestinal permeability, but further study is needed to determine if FMT could be used as a treatment.
Lawson scientists are also currently studying the use of FMT for patients with atherosclerosis, along with ongoing studies on melanoma and lung cancer. Funding for a study on pancreatic cancer has been secured and researchers are in the process of planning trials for a number of other applications.
Dr. Lenehan says, “The microbiome is connected to several diseases and their treatments. Evidence is growing that an individual’s health is related to their microbiome.”

The donor challenge
The challenge of finding fecal donors for FMT and the cost of that process remain an issue for research into this promising treatment, even as more potential applications are discovered.
There is currently no process in place to match donors and recipients – as with organ donation – but there is an extensive screening process for both infectious and non-infectious conditions, one that needs to be repeated if a donor experiences any lifestyle changes.
Dr. Burton says, “We still don't understand the full role of the microbiota. We have to ensure that we're not giving patients a microbiota that might cause them some other issue in the future, so the donors are screened very thoroughly for that.”
Screening also excludes donors with an increased risk of developing the diseases scientists are hoping to treat, such as metabolic syndrome related conditions.
A 2017 article published in Open Forum Infectious Diseases by Drs. Silverman and Burton found the cost of screening high numbers of potential donors could make establishing local programs extremely difficult, so having a central program such as the one in London could help patients in many regions.
In the study, only five of 46 potential donors passed the history, examination, blood, stool and urine tests, and of the five, four later travelled or had illnesses that made donation inadvisable.
The search continues in London for potential donors to help drive this research forward. You can read one donor’s story and learn how you can get involved here.
More on FMT and the microbiome:
Drugs vs. bugs: Harnessing the microbiome to improve treatments
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
The invisible world inside us
The human microbiome is a wonder of nature.
Trillions of microbes call our body home. They live in our gut and many other places throughout our body. They are involved in virtually every aspect of how we function and we are learning that they are essential to staying healthy. An unhealthy microbiome has been linked to many diseases from allergies to cancer and even mental health.
Most people out there have heard about probiotics and fermented foods, and chances are you’re trying to get more of them in your diet.
Drinking kombucha or eating yogurt, anyone?
Join Lawson Health Research Institute for our next Café Scientifique event, "The invisible world inside us: Exploring the human microbiome."
Hear from a panel of researchers who are unraveling the mysteries about the microbiome and using that knowledge to improve health and health care. They will also bust some myths and share the important facts when it comes to probiotics, prebiotics and the microbiome.
Image

SPEAKERS
- Dr. Gregor Reid, Lawson Scientist and Professor of Microbiology & Immunology and Surgery at Western University.
Presenting: Probiotics and Prebiotics - Look beyond the fake news - Dr. Michael Silverman, Lawson Associate Scientist, Chair of Infectious Diseases, Schulich School of Medicine & Dentistry at Western University and Chief of Infectious Diseases for St. Joseph’s Health Care London and London Health Sciences Centre.
Presenting: Fecal Transplants: What does this crap have to do with me? - Dr. Jeremy Burton, Lawson Scientist and Assistant Professor of Surgery (Urology) and Microbiology & Immunology at Western University.
EVENT DETAILS
Date: Wednesday, November 27, 2019
Time: 7-9 pm (doors open at 6:30 pm)
Location: Best Western Plus Lamplighter Inn & Conference Centre (Regency Room), 591 Wellington Rd, London, ON N6C 4R3
Map and directions.
Parking: Free on-site parking
This is a free event and online registration is REQUIRED.
Registration for this evengt is now FULL.
Please fill out the form here to be added to the waitlist.
You will be notified should a spot open up.
Time for Canada to reclaim its place as a leader in scientific discovery
The following editorial was provided to Post Media by Dr. David Hill, scientific director, Lawson Health Research Institute.
Last week the Nobel Prizes for 2017 were announced, recognizing incredible advances in science that will impact all our lives for the better. If you were looking for Canadian scientists amongst the teams, you would be disappointed.
According to a federal government report commissioned by the minister of science titled Investing in Canada’s Future — Strengthening the Foundations of Canadian Research and released in April, Canada’s momentum in the sciences has never been worse.
Our country’s investment in key emerging areas such as artificial intelligence, clean technology, nanotechnology, immunotherapy, bioinformatics or bio-engineering is flat-lined or declining, and falling seriously behind competitor nations.
We are not talking about matching the United States or Germany. Canada invests less in science research and development relative to gross domestic product than does Taiwan or Singapore.
Why should we care?
Because smart science delivers technologies we take for granted every day, such as Siri on our iPhones, minimally invasive surgery and secure online banking.
Science also creates companies, delivers high-paying and rewarding jobs, and is the backbone of the economy.
In London, Ont., jobs that depend on advancing science include those at Lawson Health Research Institute, the research institute of London Health Sciences Centre and St. Joseph’s Health Care London and where I work; academic institutions such as Western University and Fanshawe College; and local businesses generating health devices, computer software and engineered products. A lack of investment in science could be devastating to our city.
This report places the failure to invest in science at the door of successive federal governments during the past decade.
Of course, it is not only government that should invest in science. It is industry that takes proven scientific findings and translates them into products we all consume.
But these innovative products need to start somewhere, most often in the laboratory. Fostering high risk, fundamental discovery science should be a core responsibility of government in a knowledge-driven economy.
In Canada, the contribution of federal funds to discovery science is now below 25 per cent of the total research investment, and lower than most of our competitor nations. Consequently, research funds are scarce, laboratories are closing, fewer students are receiving advanced training, and fewer new businesses are emerging.
It is not too late.
The report provides evidence to show that Canadian scientists are still respected leaders in their fields. The engine simply needs fuel.
To return Canada’s discovery science enterprise back to 2006 productivity levels, we require an additional investment of $1.3 billion during four years, representing 0.1 per cent of the entire federal budget for each of those years.
The investment quickly pays for itself. Every $1 invested in fundamental research has been calculated to return $2.20 to $2.50 in direct and indirect economic activity.
Next year’s federal budget is being put together right now in Ottawa, and we have an opportunity to reclaim our past reputation as a discovery nation; a nation that brought the world insulin, the Canadarm, Pablum, canola and the electron microscope.
The journey toward that next Canadian Nobel Prize needs to start now.
Dr. David Hill
Scientific Director
Lawson Health Research Institute
Tomorrow’s scientists tour Lawson research facilities
A group of senior chemistry students from H.B. Beal Secondary School visited Lawson Health Research Institute (Lawson) facilities at St. Joseph’s Hospital on Wednesday, November 8. In addition to learning about Lawson’s world-renowned imaging research, the group toured the Cyclotron and PET Radiochemistry Facility and Dr. Alexandre Legros’ brain stimulation lab.
The students first learned about Lawson’s simultaneous PET/MRI – the first in Canada – and its associated research. Led by Dr. Jonathan Thiessen, Lawson imaging scientist, the presentation focused on the benefits of combining Positron Emission Tomography (PET) with Magnetic Resonance Imaging (MRI) across multiple disciplines.

Above: Dr. Jonathan Thiessen discusses Lawson's simultaneous PET/MRI
Benjamin Wilk, a PhD candidate working under Dr. Thiessen’s supervision, presented on his research which is focused on developing methods to image the heart after myocardial infarction, or heart attack, using PET/MRI. Qi Qi, another of Dr. Thiessen’s PhD candidates, discussed his research that looks at multimodal imaging to evaluate tumour perfusion and glycolysis in brain tumours.
"It is an incredible opportunity to present our work to high school students,” said Dr. Thiessen. “By seeing examples of the research happening in their own community, my hope is that some of them will be inspired and work hard to become the scientists and healthcare professionals of tomorrow."
The students were then split into two tour groups. The first group toured Lawson’s Nordal Cyclotron and PET Radiochemistry Facility with the facility’s director, Dr. Michael Kovacs; Jeff Corsaut, engineer; and Dr. Justin Hicks, Lawson imaging scientist.

Above: Dr. Justin Hicks provides a tour of The Cyclotron and PET Radiochemistry Facility
The Cyclotron and PET Radiochemistry Facility is used to produce positron-emitting radiopharmaceuticals (PERs). PERs are injected into patients undergoing a positron emission tomography (PET) scan. The half-life of the radioactive isotopes in PERs is short, which necessitates generating them with a cyclotron that is in close proximity to the clinic where they are used.
The students learned how PERs are produced in the Cyclotron and research being conducted with PERs to advance imaging of complex diseases.
The second group toured Dr. Alexandre Legros’ brain stimulation lab which is part of the Bioelectromagnetics and Human Threshold Research Group at Lawson. Dr. Legros’ research focuses on the effects of specific electromagnetic stimuli - from deep brain stimulation to power-frequency magnetic fields - on human brain processing, motor control and cognitive functions. The students were guided by lab manager, Michael Corbacio, and postdoctoral scholar, Dr. Sebastien Villard.

Above: Dr. Sebastien Villard (second from right) and Michael Corbacio (far right) provide a demonstration of research being conducted in Dr. Alexandre Legros' Bioelectromagnetics and Human Threshold Research Group
The two groups of students then traded places, touring the facility they had not yet visited.
“The H.B Beal senior chemistry class was impressed and grateful with the opportunity to visit the facilities at Lawson Health Research Institute,” said Andrew Holmes, the class’ teacher and head of science at H.B. Beal. “The presentations, cyclotron tour and research lab gave students some valuable insight into some of the roads available to them with a scientific path in education. Students were particularly impressed with how enthusiastic and excited the researchers were in talking about their work at Lawson, and came away with a very positive view of scientific career paths.”