Search
Search
Top 12 research stories of 2022
As the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, our teams impact the lives of people in Ontario, Canada and around the globe with groundbreaking studies, world firsts and translational research that enhances care, health and wellbeing. Here are some of Lawson Health Research Institute’s top research highlights of 2022.
Researchers looking to better personalize treatment for PTSD

In a new study through Lawson and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from post-traumatic stress disorder (PTSD). Read more.
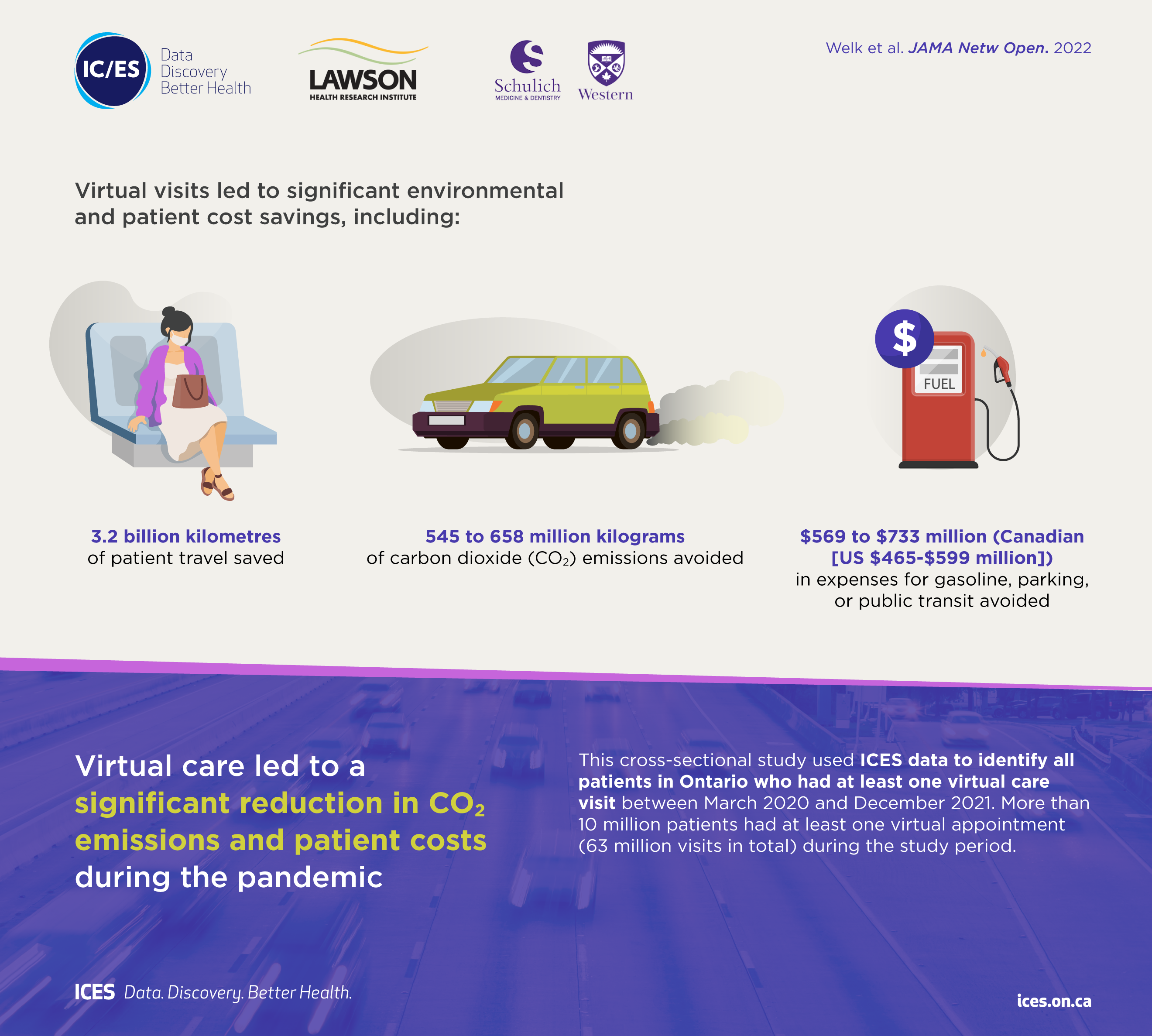
Virtual care associated with significant environmental and patient cost savings

A new study by researchers at ICES, Lawson and Western finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs. Read more.
Novel test that could easily diagnose blast injury created by local scientists

In a world first, researchers at Lawson and Defence Research and Development Canada have developed a breath test that could be used to diagnose repetitive blast injury – a mild traumatic brain injury resulting from pressure changes that occur during explosions. The device will soon go through clinical trials to validate its efficacy. Read more.
Local researchers using artificial intelligence to lead the way in bedside lung imaging
A team at Lawson is testing a new form of artificial intelligence (AI), paired with portable ultrasound machines, to image and identify lung concerns in real time, right at the beside of critically ill patients. Approximately 100 critical care patients at LHSC will be part of this study. Read more.
New tool shows promise in helping people manage traumatic brain injuries one pace at a time

A team at Lawson has developed a new app called MyBrainPacer™ which aims to better assist and treat those living with mild traumatic brain injuries (mTBI), including concussions. mTBI may come with lasting effects that can alter a person’s life. Although a person with a mTBI may appear fine on the outside, many have to pace their day-to-day activities in order to allow the time needed for the brain to properly heal. Much like point tracking used by dieters to monitor food choices, through MyBrainPacer™ App, users can assign values to tasks like driving, grocery shopping, screen use and exercise so they can plan and pace their daily activity. Read more.
Study shows a decline in Veterans' mental health throughout the pandemic

When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population. They found that more than half of Canadian Veterans reported a decline in their mental health. Read more.
Growing evidence that PSMA imaging improves prostate cancer detection
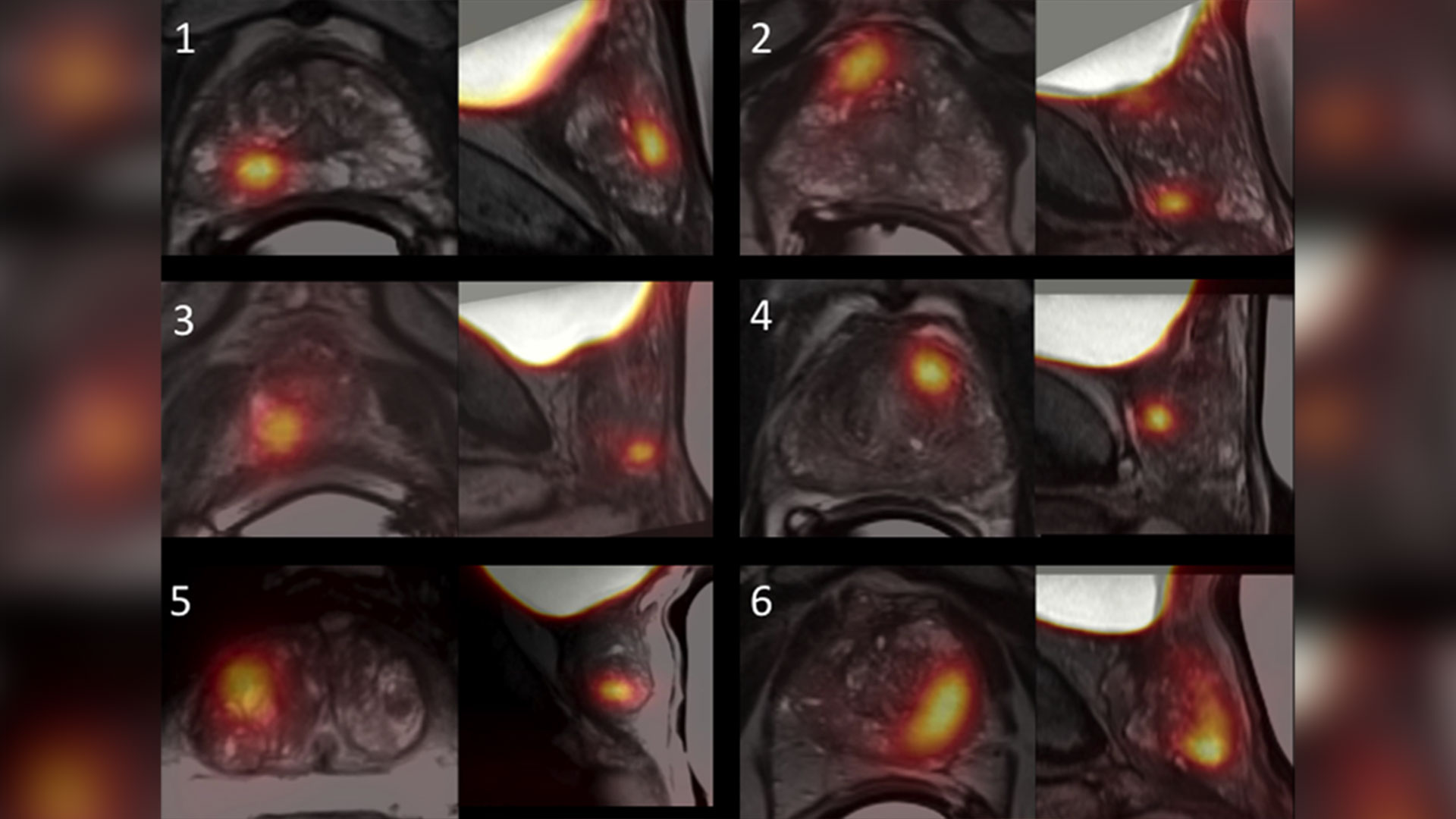
Scientists at Lawson are leading the way in using specialized imaging to detect prostate cancer – the fifth leading cause of cancer death in men around the world. Early evidence indicates that PSMA PET scans have changed how prostate cancer is being treated, but more work is underway to understand the impact of those treatment changes. Read more.
Leveraging virtual reality to manage pain in paediatric patients

A study underway through Lawson and Children’s Hospital at LHSC is using virtual reality (VR) to help paediatric patients during painful and distressing procedures. The study is focusing on paediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in paediatric cancer patients. Read more.
Team players: FMT and microbiome research could have widespread impact

There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system. FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis. Read more.
London researchers adapt MRI technology to image salt within the kidneys

Scientists at Lawson have adapted PET/MRI technology to accurately image salt within the kidneys of patients with kidney disease. Imaging salt within the kidneys has never been accurately accomplished in patients with kidney disease, but Dr. McIntyre and his team developed new technology and software that was adaptable to a PET/MRI machine at St. Joseph’s. Read more.
London researchers discover novel method to diagnose long COVID
Published in Molecular Medicine, researchers at Lawson have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition. Read more.
Largest trial ever done in hemodialysis care examines optimal dialysis temperature

Published in the Lancet findings from a large clinical trial through Lawson, ICES Western and Western University suggest that lowering dialysis temperatures does not lead to improved patient outcomes, despite previous studies suggesting otherwise. Read more.
To learn more about Lawson research studies, please visit our News and Media page
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Two new research chairs announced for imaging
In a historical-first, St. Joseph’s Health Care Foundation and Western University announced two research chairs that are a critical step toward new approaches in imaging research and patient care in London and around the world. The combined value of both innovative new research chairs is $6.5M, which will be endowed in perpetuity to advance imaging research at Western University and Lawson Health Research Institute.
The research chairs have been named after the two scientists who are revolutionizing health care through their groundbreaking imaging research – Drs. Ting-Yim Lee and Frank Prato.
“These Chairs build on the legacy of exceptional imaging leadership across our academic, research and healthcare organizations. They are a critical step towards new approaches in medical technology and hospital-based research that will revolutionize patient care,” says Dr. Gillian Kernaghan, President and CEO, St. Joseph’s Health Care London.
Research teams in the city are using state-of-the-art imaging technology to help clinicians better predict and diagnose illnesses before their unset. And uncover why, and how, illness forms to one day find a cure to some of the most devastating diseases in the world.
“We’ve come to know medical imaging as one of the cornerstones of innovation and discovery at Lawson, and the two new research chairs represent two monumental leaps forward in the field of imaging research,” adds Dr. David Hill, Lawson Scientific Director.
The Ting-Yim Lee Chair in Cardiac Computerized Tomography (CT) Imaging Research has been established through the generosity of Ting-Yim and Maggie Lee and a joint funding collaboration between St. Joseph’s Foundation and Western University.
Dr. Ting Yim Lee is a scientist and professor of the Schulich School of Medicine & Dentistry, medical physicist at St. Joseph’s Health Care London and a scientist with Lawson’s Imaging program. Through his leadership, The Ting-Yim Lee Chair in Cardiac Computerized Tomography (CT) Imaging Research will transform the way clinicians diagnose, and prevent, severe tissue damage in persons who have experienced a cardiac event.
“Over the past 28 years, St. Joseph’s and Western have created opportunities for me and supported my research endeavor in many ways. I feel this gift is the best way to repay the help that I have received. We are onto something that is worthwhile and successful. By setting up this Chair, there would be a significant person – a clinician-scientist – to lead the next phase of the cardiac CT program. I am really humbled that the institutions see the value in this research and have contributed to guarantee that we have the necessary leader to carry forth this development,” says Dr. Lee.
This Chair represents the next phase of CT imaging research, focused on developing software and new methods that will save people’s lives.
The Dr. Frank Prato Research Chair in Molecular Imaging has been established to further enhance scientific understanding in the specialty of molecular imaging – building upon St. Joseph’s internationally-recognized leadership in imaging excellence.
Dr. Frank Prato is a scientist and professor of the Schulich School of Medicine & Dentistry, Chief Medical Physicist at St. Joseph’s Health Care London and the Founder and Program Leader of Lawson’s Imaging Program. Through his visionary leadership, The Dr. Frank Prato Research Chair in Molecular Imaging will improve the way clinicians effectively diagnose disease and actively correct the course of treatments in real time for life-threatening illnesses.
“I am truly honoured to have this Research Chair in Molecular Imaging named after myself. Over the past 40 years I have been privileged to work with outstanding people and incredible resources. Today Medical Imaging has become a cornerstone of care at St Joseph's Hospital. Here at St Joseph's we realize patient stewardship includes research as an essential part of the patient care continuum and that discovery, through research, leads to improved patient care. The holder of this chair will help lead us into the next frontier of medical imaging directly benefiting our local, national and global communities,” says Dr. Prato.
This Chair represents the next phase of precision medicine using molecular imaging to distinguish between varying forms of dementias, cancers, and to detect the early onset of cardiac disease and diabetes before symptoms emerge.
“With this historic announcement, we are marking a new phase of partnership and collaboration between our institutions and celebrating the generosity of donors who have helped create two significant research chairs,” explains Dr. Amit Chakma, President and Vice-Chancellor, Western University. “Together we will ensure that London remains at the forefront of medical imaging research and teaching.”
These Chairs will also have a greater role to play in the local health care community by attracting, and retaining, the research talent needed to innovate the way London’s hospitals and Western tackle the most pressing health issues Canadians face today.
Understanding the COVID-19 virus through health research
In the early months of the COVID-19 pandemic, there was little known about the virus that was causing the COVID-19 illness. Hospital researchers in London, Ontario, through Lawson Health Research Institute, quickly got to work to study and better understand the SARS-CoV-2 virus. Lawson is the research arm of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London.
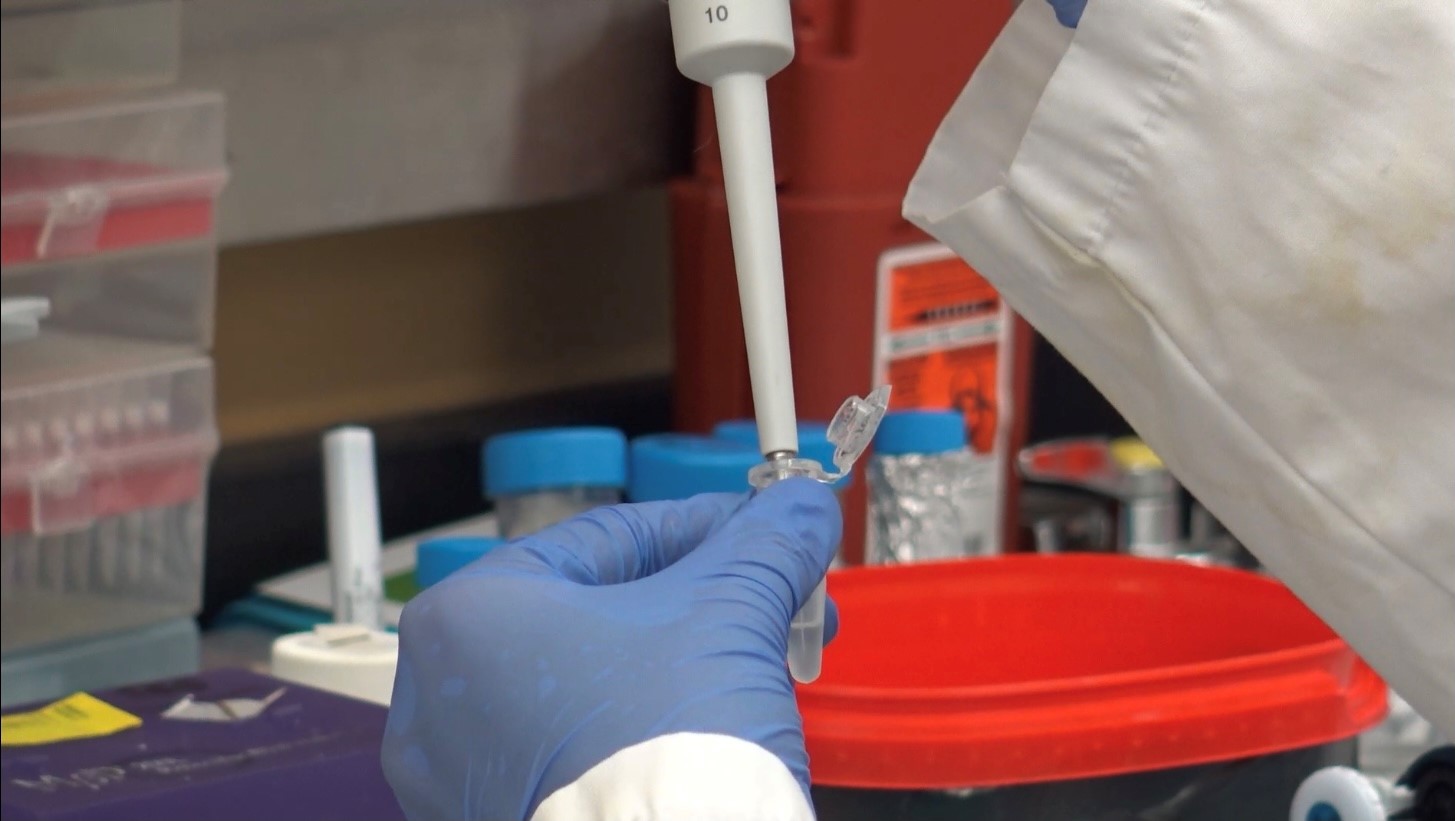
“When the pandemic hit, we were well prepared in London to start research studies. We had existing expertise, laboratories and teams through the hospitals, Lawson and Western University that could be mobilized quickly,” explains Dr. Douglas Fraser, Critical Care Physician at LHSC and Scientist at Lawson. “Patients started coming to hospital with COVID-19 and we began research that involved collecting human samples and bringing them to the lab for analysis.”
Dr. Fraser, who is also a Professor at Western’s Schulich School of Medicine & Dentistry, led the research team studying the samples from COVID-19 patients in hospital. “We learned very quickly that COVID-19 patients were experiencing a strong inflammatory response to the virus. We looked at the molecules involved because many of these are signaling molecules to the immune system.”

Dr. Douglas Fraser, Critical Care Physician (LHSC) and Lawson Scientist
“By studying the molecules, we were able to determine the pathways. This is important because it also points to how we should be targeting our diagnostics and therapeutics,” adds Dr Fraser.
As a hospital research institute, Lawson is uniquely positioned to address the medical questions posed by a new virus. Its Clinical Research Services (LCRS) and Center for Clinical Investigation and Therapeutics (CCIT) teams responded rapidly when researchers initiated COVID-19 studies, including Dr. Fraser’s study to examine the immune response in patients with COVID-19.
“Starting a clinical trial usually takes a certain amount of time to put together, but the pandemic created a perfect storm,” explains Sue Tereschyn, Manager of LCRS at Lawson. “Clinical researchers had to develop studies at a speed they have never seen, and they needed implementation support at the same speed. In Dr. Fraser’s case, we needed samples from the Intensive Care Unit (ICU) and we were processing samples from COVID-19 patients seven days a week. A high level of skill was needed.”
Dr. Fraser and his team soon became the first in the world to understand the immune response and several pathophysiological features of the virus. This work led to a critical understanding of how the virus was impacting patients and potential avenues for therapy.
“It’s important to understand what’s happening in the body when someone has COVID-19 because that gives us information as to why some patients don’t do well and why others recover,” shares Dr. Fraser. “This helps us know who is vulnerable to COVID-19 and how to best offer treatments in the future.”
Read about Dr. Fraser's COVID-19 research:
- Researchers team up with Diagnostics Biochem Canada to study COVID-19
- Study identifies biomarkers that could be used in a quick, inexpensive COVID-19 blood screening tool
- Researchers unravel two mysteries of COVID-19
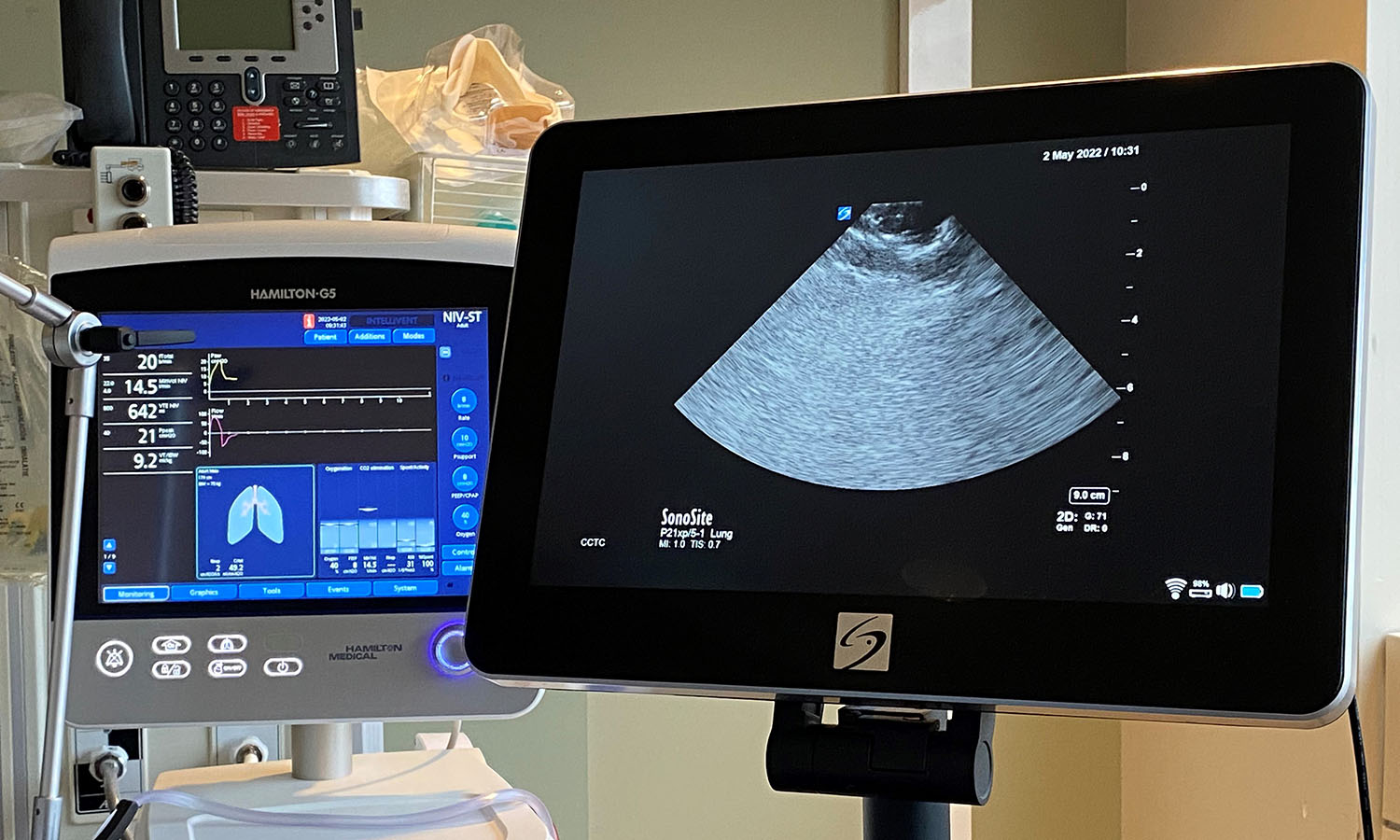
Work is also underway to find the unique fingerprint that the COVID-19 virus can leave on the lungs. Hospital researchers at Lawson have developed and tested an artificial neural network for diagnosing COVID-19.

Dr. Robert Arntfield, Medical Director, Critical Care Trauma Centre (LHSC) and Lawson Researcher
“The lung ultrasound techniques and the findings of COVID-19 by looking at the lungs didn’t initially look unique when compared to other conditions like pneumonia. Our group wanted to investigate whether or not there were differences that were possibly subvisible,” says Dr. Robert Arntfield, Medical Director of Critical Care Trauma Centre at LHSC and Lawson Researcher. “Through our work, we were able to show that in fact artificial intelligence could outperform a trained clinician in identifying a COVID-19 lung from a similar affected lung that was not due to COVID-19.”
This new technique just scratches the surface of the beneficial use of AI when it comes to medical imaging for patients. “It shone a light on the idea that there were hidden details within all the noise of the image,” adds. Dr. Arntfield. “When you can input that into a machine that is extremely portable the way ultrasounds are, you have a precise diagnostic machine that you can take anywhere a tablet can go.”
The team is now expanding on these findings with further research. Lawson has recently approved Dr. Arntfield’s “Project Deep Breath” which aims to go beyond COVID-19 and explore multiple conditions where lung ultrasounds and AI can be paired together.
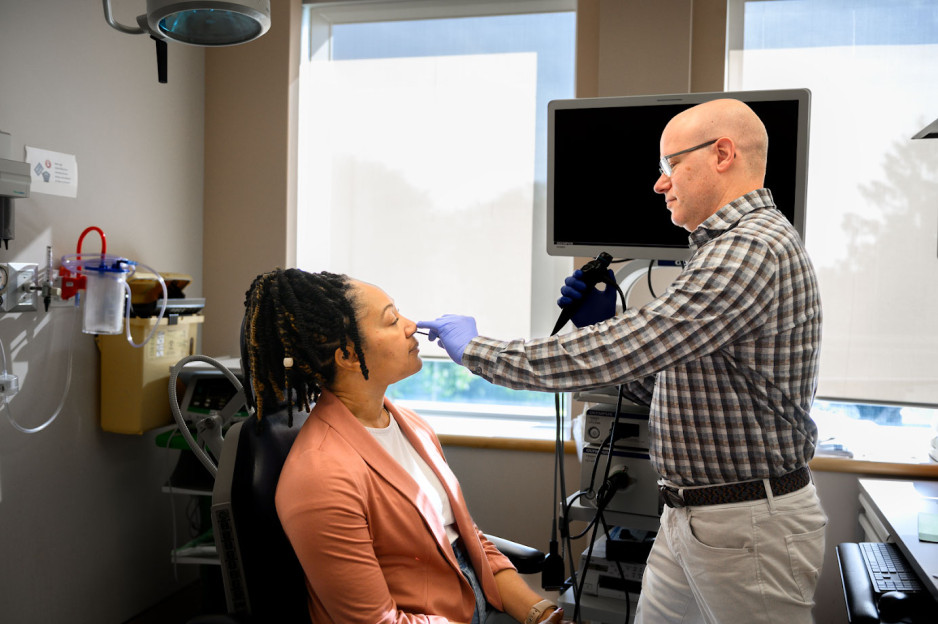
Viral mouth-taping trend ‘sus’ says Canadian sleep expert
Mouth taping, a growing trend on social media channels like TikTok, carries serious health risks, especially for those with sleep-disordered breathing and obstructive sleep apnea, according to a paper published in PLOS One.
The study from Lawson Research Institute (Lawson) of St. Joseph’s Health Care London, London Health Sciences Centre Research Institute (LHSCRI) and Western University’s Schulich School of Medicine & Dentistry also found no strong evidence of health benefits.
The trend involves placing tape over the mouth to stop ‘mouth breathing’ and promote breathing through the nose during sleep. It has been recommended by many social media influencers and celebrities who claim it can lead to better sleep, enhanced oral health and anti-aging results.
“It was concerning to us that celebrities and influencers are endorsing mouth taping without scientific evidence,” says Dr. Brian Rotenberg, researcher at Lawson, LHSCRI and Schulich Medicine & Dentistry. “In the language of social media influencers, it seemed a bit ‘sus,’ so we examined what science is telling us about this trend and whether or not it is safe.”
Rotenberg collaborated with Dr. Elise Graham, paediatric otolaryngologist head and neck surgeon at IWK Health and Jess Rhee a Schulich School of Medicine & Dentistry resident who is training at London Health Sciences Centre (LHSC) on the research. He and his team examined 86 existing scientific studies on the topic, including an in-depth review of 10 studies representing the experience of 213 patients. The team found mouth taping:
- Has no strong scientific evidence of health benefits, contradicting claims on social media.
- Can make existing sleep-disorder breathing worse by restricting airflow, putting additional stress on the respiratory system and increasing risk of suffocation when patients experience a nasal obstruction.
“Our research shows that taping the mouth shut during sleep is dangerous, especially among those who may not be aware they have sleep apnea,” adds Rotenberg, who is also an otolaryngologist and sleep surgeon at St. Joseph’s Health Care London and London Health Sciences Centre (LHSC). “These individuals are unknowingly making their symptoms worse and putting themselves at greater risk for serious health complications like heart disease.”
Rotenberg and his team point to the importance of health research in combatting misinformation and pseudoscience.
“It’s easy for misinformation to run rampant on social media; we’ve seen this countless times over the past few years,” says Rhee. “We need to make health decisions based on strong scientific evidence. Our hope is that people stop taping their mouths during sleep and recognize it is dangerous.”
Virtual care associated with significant environmental and patient cost savings
London, ON - A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can
be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Virtual care associated with significant environmental and patient cost savings
A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
What happens to our bodies when we feel social emotions?
Feeling emotions based on the interactions we have with other people is a common part of daily life, yet we know very little about how these emotions are experienced in the body.
Chloe Stewart, a PhD candidate at Lawson Health Research Institute (Lawson) and Western University’s Schulich School of Medicine & Dentistry, has been awarded a Lawson Internal Research Fund (IRF) Studentship to conduct the first study to comprehensively explore the physical experience of social emotions. The study will be supervised by Dr. Elizabeth Finger, a Lawson scientist, neurologist at St. Joseph’s Health Care London’s Parkwood Institute, and associate professor at Schulich Medicine & Dentistry.
“We feel social emotions based on our awareness, interpretation or anticipation of the thoughts and feelings of others. For example, we feel embarrassment not only because we have done something potentially embarrassing, but also because we know that another person is aware of it, or could become aware of it. Other social emotions include pride, empathy and guilt,” explains Stewart.
“These are distinct from basic emotions, such as anger and happiness, which only require us to be aware of how we ourselves are feeling and can occur completely independently of other people. Whether it’s your heart beating faster when you’re angry or the lump in your throat when you’re sad, the ways that our bodies experience basic emotions are very well understood. However, we do not have a good understanding of what happens to our bodies when we feel social emotions,” she adds.
Unhealthy levels of certain social emotions are associated with many conditions, including certain kinds of dementia, obsessive compulsive disorder and psychopathy. The results of the study, which will be conducted at Parkwood Institute, could help in developing potential interventions or treatment approaches to restore these emotions to healthy levels.
The first phase of the study will look at the physical experience of social emotion in healthy adults. Noninvasive electrodes will be attached to participants’ torso, hands and throat. The electrodes are connected by wires to receivers, which in turn send signals to a computer. The researchers can assess how the signals change based on the stimulus the participant is looking at. Stewart expects the emotions will influence several different physical responses, including heart rate, swallowing rate and movement of the stomach muscles.
The research team will then extend the study to patients with frontotemporal dementia, which can impair social functioning. They will compare the physical experience of social emotions in these participants to participants with Alzheimer’s disease and dementia with Lewy bodies. Patients with Alzheimer’s disease or dementia with Lewy bodies usually have healthy levels of social emotions, but those who have dementia with Lewy bodies often have impaired physiological functioning while those with Alzheimer’s do not.
Their goal is to compare how social emotions look in healthy adults to what happens in the body when social functioning is impaired.
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
What is ICES Western? Q&A with Dr. Amit Garg
As ICES Western recruits a new Site Director, Dr. Amit Garg, who currently holds the position, sat down to talk about the importance of the work being done. Dr. Garg is also a Scientist at Lawson Health Research Institute, Nephrologist at London Health Sciences Centre (LHSC) and Professor at Western University’s Schulich School of Medicine & Dentistry.
What is your role with ICES Western?
Starting in 2009, I supervised the team responsible for the ICES Western build over an approximately three-year period. Since then, I have spent the last decade serving as the inaugural Site Director for ICES Western.
Can you briefly describe the work that ICES Western does?
For those people who don't know, ICES is a province-wide non-profit research institute, founded in 1992, that is focused on translating data into trusted evidence. Our community is comprised of world-class research, data and clinical experts who evaluate health care delivery and population outcomes.
ICES scientists and staff (currently about 570 in Ontario) and trainees (currently about 700) access a vast and secure array of Ontario’s demographic and administrative health-related data. ICES currently has 108 linked data holdings (with over one trillion data points), and the amount of data that ICES has available for use in research grows each year. The linked data include vital statistics, hospital services, physician claims, drug benefits, laboratory results, biosamples and immigration records. Our research, including 1,200 active investigator-initiated projects, is focused on making health policy and health care better, and people healthier.
ICES Western is physically located at LHSC’s Victoria Hospital and is one of seven ICES satellite sites across Ontario. The site’s development is an ongoing partnership between LHSC, St. Joseph’s Health Care London, Lawson, the Academic Medical Organization of Southwestern Ontario (AMOSO) and Western.
How does ICES’ work impact research being done in Ontario and across Canada?
ICES Western is a core facility that researchers use for research, training and decision support. Organizations such as our local hospitals and public health agencies make requests for decision support through a procedural mechanism called Applied Health Research Questions.
Over the last two years, our researchers have conducted a great deal of COVID-19 research. Several projects at ICES Western have examined vaccine effectiveness and spread of the virus. Investigators have used a data-driven approach to help protect people experiencing homelessness in Ontario. Another study quantified the impact of COVID infections on physicians, including how many of them became ill, were hospitalized and received care in the intensive care unit.
Research done through ICES Western has led to important changes in health care. For example, Health Canada instituted labeling requirement changes based on drug safety studies done through ICES.
Why is this work so important?
We all want better health outcomes for citizens, both in Ontario and throughout the world. Ideally, we want people to live longer, healthier lives without needing many health care resources, and we want that to be done in an equitable fashion. There is a substantial amount of research needed in multiple areas to achieve this goal. ICES provides a cutting edge infrastructure to enable this work.
What kind of researchers are involved with ICES?
At ICES Western we support a whole host of individuals and entities as they conduct research. Health care delivery organizations and health agencies including LHSC, the Ontario Renal Network and Trillium Gift of Life Network use knowledge received through reports completed at ICES. Our typical individual investigators include both basic science and clinical investigators. We also support trainees in the areas of epidemiology and statistics, as well as many other fields of study, such as computer science and geography. These are all students who have an interest in working with ‘big’ data. Finally, we have personnel that work with privacy, data, analysis, epidemiology and more.
What do you see in the future for the organization?
We've made a lot of progress in the last 10 years and I can't wait to see what's going to happen in the future. We're still just scratching the surface in terms of what's possible. While what we have done in building this site and supporting important research is impressive, in terms of the possibilities – the sky's the limit. There is so much opportunity around new research and trial methodologies, new insights and new evaluation techniques. I expect ICES Western will continue to develop, enabling a growing number of people to make a large impact. I see ICES continuing to contribute to a world where people live longer, healthier lives.
What is the most important thing people should know about ICES?
How enabling it is. It's time well spent to really understand what is and is not possible with ICES data and research expertise. Once you invest in it – really spend your time and energy to understand the potential– you start realizing all of these opportunities that would not be possible otherwise. With more than a thousand research studies underway across all ICES sites, we have great discoveries ahead to shape the future of health care in Ontario.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
When connections break down
In Ontario alone, an estimated 285,000 individuals currently live with some form of neurodegenerative disorder. This includes Alzheimer’s Disease, Parkinson’s Disease, mild cognitive impairment, dementia and movement disorders.
The experiences and symptoms for each person vary, but they share a progressive decline in their cognitive and motor function. It can affect their ability to work, socialize and live independently.
As our population ages, there is an urgent need to understand markers that will predict decline and identify targets for therapy that might improve long-term function and outcomes.
This is where hospital-based research can make a real difference.
On June 21, 2018, Lawson Health Research Institute hosted Café Scientifique, a community event highlighting the groundbreaking and specialized research on neurodegenerative diseases happening right here in London.
Moderated by Lawson researcher Dr. Arlene MacDougall, a panel of three expert Lawson scientists shared their unique perspectives as both clinicians and researchers, and how the knowledge we are gaining is being applied to improve health and health care for people here and around the world.
Watch the video from the event featuring the three talks from our experts.
Café Talks
Back to the beginning: Targeting early markers for Alzheimer’s Disease
By Dr. Jennie Wells
Time stamp: 5 minutes
Dr. Wells is the Medical Care Coordinator for Geriatric Rehabilitation at St. Joseph's Health Care London's Parkwood Institute, and Chair of the Division of Geriatric Medicine and associate professor in the Department of Medicine at Western Univeristy’s Schulich School of Medicine. Her clinical and research interests are Alzheimer’s Disease and Geriatric Rehabilitation. She has particular interest in Mild Cognitive Impairment (MCI) and the potential for non-drug interventions, such as exercise and nutrition to slow progression of dementia. She is a principal site investigator in randomized controlled trials of new drugs to treat dementia, MCI, and Subjective Cognitive Impairment (SCI).
Highlights:
- What causes dementia?
- How early do changes happen in the brain before symptoms even appear?
- What is the single best diet approach for a healthy body and mind?
- How does exercise keep your brain healthy?

Neuroinflammation and dementia: The old and the new
By Dr. Elizabeth Finger
Time stamp: 24 minutes
Dr. Finger, a neurologist at St. Joseph's Parkwood Institute, received her MD from Cornell University. She completed an internship in Internal Medicine at Massachusetts General Hospital, followed by residency in Neurology at Massachusetts General Hospital and Brigham and Women's Hospital in Boston. Her research focuses on understanding the cognitive, neural, and genetic substrates of abnormal decision-making, emotion and social behavior. Using a variety of different diagnostic techniques and modalities, the research program investigates the cognitive and neural systems affected in patients with Frontotemporal Dementia, related disorders and their at-risk family members.
Highlights:
- Do anti-inflammatory medications reduce the risk of dementia or slow the rate of decline?
- How do genes related to the immune system increase the risk of developing dementia and Alzheimer’s Disease?
- What about the effects from dysfunction of the brain’s own immune system?
- Do conditions or events causing systematic inflammation (surgery, infection, auto-immune diseases) also increase neuroinflammation which can lead to dementia?

New Frontiers in the Treatment of Parkinson’s Disease: Addressing the unmet needs
By Dr. Mandar Jog
Time stamp: 45 minutes
Dr. Jog is a Lawson researcher, Director of the National Parkinson Foundation Centre of Excellence at LHSC, Director of the Movement Disorders Centre in London and Professor of Neurology at Western University. His research interests include topics such as motor control, neurophysiology and computational modeling, multichannel recording and web-based teaching of movement disorders. Dr. Jog has a passion for clinical and scientific innovation and holds numerous patents that are reaching commercialization with strong collaboration with university technology transfer and industry partners.
Highlights:
- How do clinician researchers take questions from the bedside and solve them at the bench using technology in order to treat movement disorders?
- How can wearable technology be used to detect movement disorders and monitor for optimized treatment – remotely from anywhere in the world?
- How can we use machine-guided sensors for personal diagnostics and therapy for essential tremors and Parkinson’s Disease?
- How can spinal cord stimulators improve movement and gait for patients, including those previously using wheelchairs and scooters?

Did you miss the event? Add your email address to our Café Scientifique invite list so that you’ll be the first to know when the next event takes place.
Sign up here.