Search
Search
Aging
At Lawson’s hub of research into aging and neurogenerative diseases, we weave together world-changing science with clinical practice.
Our determined team of experts seeks to help people live better and more independently throughout their lifespans, and to halt the rising toll that dementia is taking on Canadians.
It’s why we’re national and global leaders in:
- Seeking earlier, faster ways to diagnose and predict dementia and related neurodegenerative diseases through innovative biomarker tests and advanced brain imaging
- Leading rigorous trials of new medications that could delay or halt – or potentially even reverse – cognitive impairment
- Understanding the link between cognition and mobility, osteoporosis and bone health, falls and frailty,
- Helping translate our findings to patients, caregivers, clinicians and allied health professionals.
Our half-century legacy of groundbreaking research is bolstered by major, multi-year grants from national funding agencies and philanthropists, who recognize the depth of our expertise and the breadth of our partnerships.
We lead the world in researching diseases associated with aging. Read on to see where we can lead you.
Ali Bateman
Ali Bateman, MD
Assistant Professor, Schulich School of Medicine and Dentistry
Acquired and Traumatic Brain Injury; Spinal Cord Injury
Dr. Ali Bateman is a physiatrist at Parkwood Institute and an Assistant Professor in the Department of Physical Medicine and Rehabilitation Schulich School of Medicine & Dentistry at Western University. She is also an Associate Scientist at Lawson Health Research Institute, and the Quality Improvement Lead in the Department of Physical Medicine & Rehabilitation.
Dr. Bateman completed her medical degree and residency training at Western University, and is currently completing a master’s degree in Quality Improvement and Patient Safety through the Institute of Health Policy, Management, and Evaluation at the University of Toronto. She is also certified by the Canadian Society of Clinical Neurophysiologists and holds the designation of CSCN Diplomate (EMG). As a consultant physiatrist, Dr. Bateman provides care in acquired brain injury and spinal cord injury rehabilitation programs and the electrodiagnostic laboratory at Parkwood Institute.
Her research interests centre on quality improvement, patient safety, and knowledge translation with the aim of achieving best practices so that all persons with spinal cord and/or brain injury receive the best quality care.

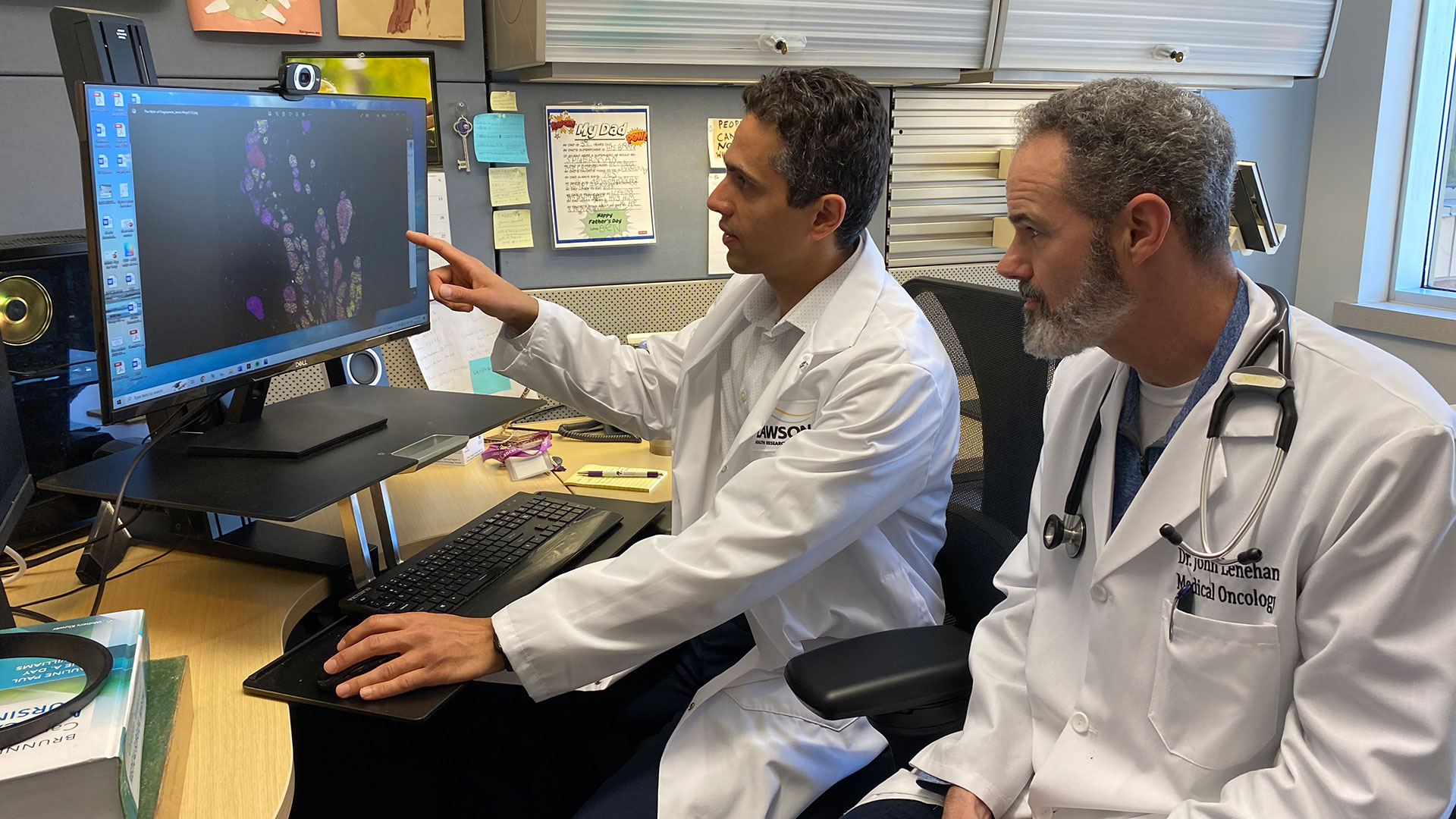
An image of the future: Innovations in imaging research
Lawson Health Research Institute (Lawson) has long been a leader in biomedical imaging. The first Canadian magnetic resonance imaging (MRI) of a human occurred at St. Joseph’s Health Care London (St. Joseph’s). The country’s first positron emission tomography/computed tomography (PET/CT) and positron emission tomography/magnetic resonance imaging (PET/MRI) scanners were also installed at St. Joseph’s. New developments in imaging research continue to enhance the diagnosis, prevention and treatment of a wide range of diseases, from cancer to post-traumatic stress disorder.
On May 23, Lawson hosted a Café Scientifique event where a panel of Lawson Imaging scientists discussed their cutting-edge work. Guests had the opportunity to ask questions as part of an open-forum discussion to gain insights from the speakers, and from one another.
In celebration of Canada’s 150th anniversary as a nation, this event is the first of a two-part series focusing on the future vision for health care in Canada and the legacy that research at Lawson will leave.
Imaging of the heart: Seeing the cause of chest pain more clearly
By Dr. Ting-Yim Lee, Lawson scientist, Medical Physicist at St. Joseph’s, professor at Western University’s Schulich School of Medicine & Dentistry, and scientist at Robarts Research Institute
When patients with chest pain arrive in the emergency department, they are given an electrocardiogram (ECG) and blood test. These diagnostic tests determine if the pain has a non-cardiac cause (such as heart burn), if it is caused by a heart attack, or if the patient has angina (plaque formation in the coronary arteries that either reduces or temporarily cuts off blood flow to the heart) but did not have a heart attack.
If a patient has angina, they are then given additional diagnostic testing to see whether a blood clot has formed and where it is located. This is determined by two different imaging techniques: x-ray imaging (angiogram) and nuclear imaging. This process is invasive and means that patients must be scheduled for two different exam days. Using two techniques also means that there can be image misalignment, and the images often provide poor detail.
Dr. Ting-Yim Lee’s lab has pioneered a Computed Tomography (CT) method for imaging blood flow to the heart muscle (CT Perfusion), which can help patients avoid unnecessary tests and treatment, as well as reduce health care costs.
“CT imaging is a non-invasive imaging technique that uses x-rays to create high-detail cross-sectional images of the body. Using this method, we can evaluate the degree of blockage in coronary arteries – with one diagnostic test instead of two,” says Dr. Lee.
Using light and sound to improve breast surgery
By Dr. Jeffrey Carson, Lawson scientist and associate professor at Western University’s Schulich School of Medicine & Dentistry
“Most women diagnosed with breast cancer undergo surgery, and months of chemotherapy and radiotherapy. They must deal with the discomfort, side-effects, emotional stress and financial burden of treatment. Almost one in four surgeries for breast cancer must be repeated, meaning many women have to go through this all over again,” says Dr. Jeffrey Carson.
In breast conserving surgery, there is a high chance of repeat surgery as the surgeon must see and remove 100 per cent of the tumour in order for it to be successful. They are not able to determine whether the entire tumour was removed until after the surgery has been completed.
Dr. Carson and his team at St. Joseph’s have developed a technology called Intraoperative Photoacoustic Tomography (iPAT), which has the potential to reduce the chance of repeat surgery for breast cancer. The technology is able to image surgery specimens in the operating room during surgery, allowing surgeons to determine whether the whole tumour has been removed before the surgery is complete.
How imaging can improve the management of epilepsy
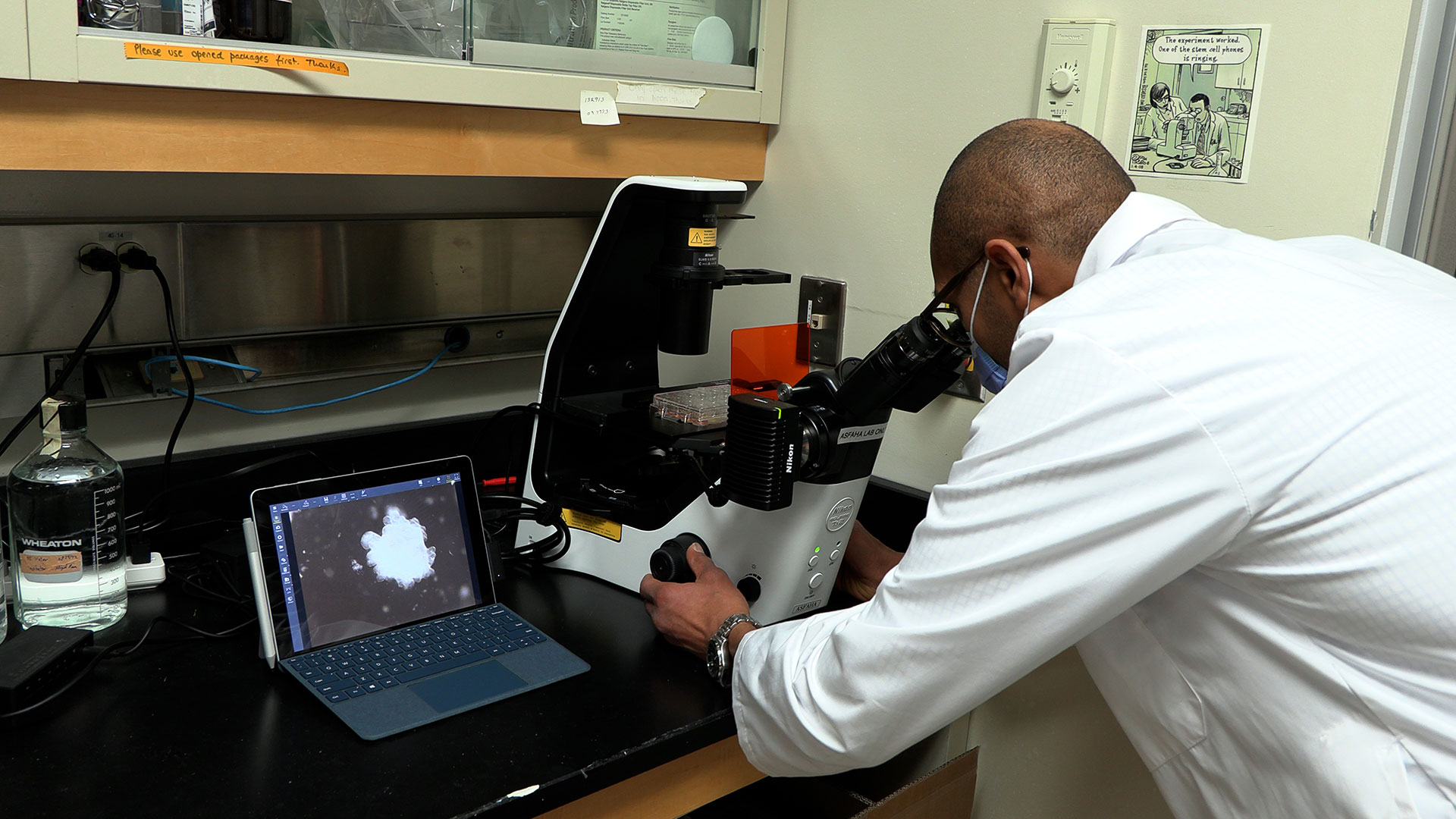
By Dr. Udunna Anazodo, postdoctoral fellow at Lawson
Most patients with epilepsy are effectively treated with antiepileptic drugs. However, 36 per cent will not respond to the drugs. For these patients, surgery on the area of the brain that is causing seizures is the standard of care – if patients are good surgical candidates.
“If patients with epilepsy are to undergo surgery there must be a good indication of where the seizure focus is and it must be possible to determine that removing this portion of the brain will not affect brain function,” says Dr. Udunna Anazodo.
To see whether they are good candidates for surgery, patients must undergo an invasive procedure called intracranial monitoring, where electrodes are placed on the brain.
Dr. Anazodo has been studying how PET/MRI can be used to map seizures with the goal of minimizing the need for invasive intracranial monitoring. This technique makes it possible to locate areas in the brain that cause seizures and to see if the seizures affect brain functions.
See photos from the event on Lawson’s Facebook page.

Above: Café Scientifique presenters (from left to right): Drs. Jeffrey Carson, Frank Prato (moderator), Ting-Yim Lee and Udunna Anazodo.
An innovative year: Top 12 research stories of 2023
It’s been another year of transformational research at Lawson Health Research Institute. Our teams have published groundbreaking findings and launched new studies that will have a profound impact on patient care.
The following are 12 highlights of research and innovation from across London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s). From trialing new cancer treatments to advancing understanding of mental health, our research teams have achieved a number of important milestones.

1. New study suggests blood plasma proteins hold answers to better understanding long COVID
Lawson researchers continued to advance understanding of COVID-19 this past year. In one study, researchers found that unique patterns in blood plasma proteins of patients with suspected long COVID could act as a drug target to improve patient outcomes. Read more.

2. New study finds exercise, cognitive training combo boosts mental sharpness in seniors
A study from Lawson and Western University found that a combination of computerized cognitive training and aerobic-resistance exercises can improve functions like memory, attention, recognition and orientation in older adults with mild cognitive impairment. The results suggest a new way to address declining mental sharpness in older adults. Read more.

3. $7.55 million in funding to take LHSC-developed technology global
Technology to diagnose rare genetic disorders developed by researchers at Lawson and LHSC will be going global thanks to $7.55 million in funding from Genome Canada grant and Illumina Inc. The new artificial intelligence-led technology could allow rare diseases to be diagnosed with a simple blood test. Read more.
4. Fecal transplants show promise in improving melanoma treatment
Fecal microbiota transplants (FMT) from healthy donors are safe and could improve response to immunotherapy in patients with advanced melanoma, according to results from a world-first multi-centre clinical trial led by Lawson researchers. Read more.

5. New study shows technology could play an important role in mental health support
A team of Lawson researchers found that the use of ‘smart home’ technology like touch screen devices, activity trackers, weigh scales and medication dispensers may lead to better outcomes for those living with both mental health and physical disorders. The study found that participants using the technology started logging more exercise, making healthier food choices and not missing medication doses. Read more.

6. Canadian children’s hospital visits for suicidal thoughts, self-poisoning and self-harm up during pandemic, study finds
A national study with Lawson researchers found that during the first two years of the COVID-19 pandemic, adolescent emergency department (ED) visits and hospitalizations for suicidal thoughts, self-harm and self-poisoning increased across Canada, with the greatest increase occurring among adolescent girls. Read more.

7. St. Joseph’s to become Canada’s first centre of excellence in molecular imaging and theranostics
A partnership between Lawson, St. Joseph’s Health Care London and GE HealthCare will create Canada’s first centre of excellence in molecular imaging and theranostics at St. Joseph’s. The centre will focus on using precision diagnostic imaging and targeted therapy to advance personalized treatment of cancer and other diseases. Read more.

8. Researchers investigate a new method of sedation for paediatric patients
Intravenous sedatives are normally used to sedate critically ill children. However, they can contribute to a complication called delirium, which includes symptoms of confusion, disorientation, agitation, excessive drowsiness and poor attention. To improve outcomes, scientists at Children’s Health Research Institute (a program of Lawson), Sunnybrook Research Institute and The Hospital for Sick Children (SickKids) are collaborating on a pilot study to understand whether inhaled sedation could be a better alternative to keep critically ill children sedated and comfortable. Read more.
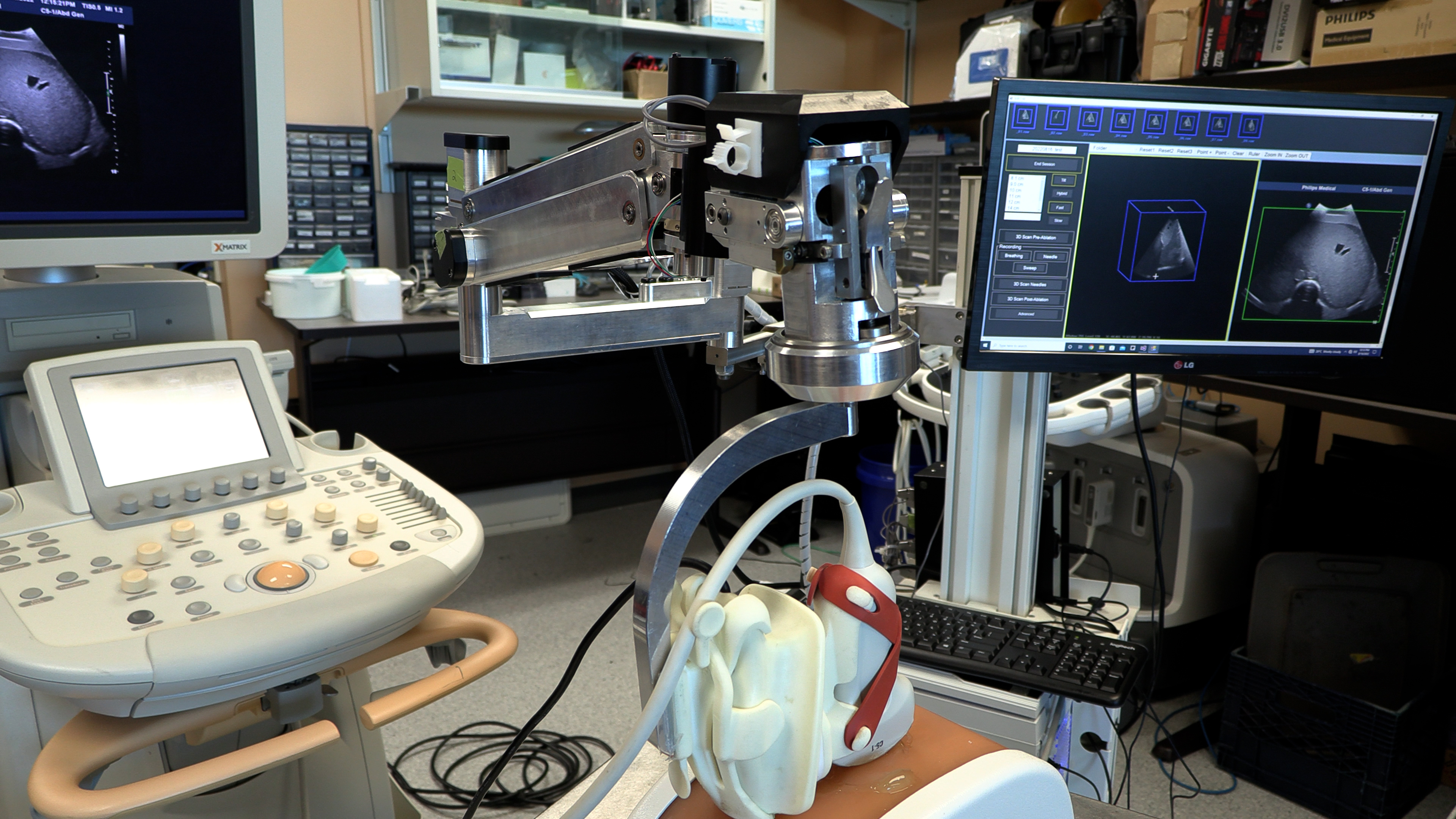
9. New robotic 3D ultrasound may improve accuracy of liver cancer ablation therapy
A technique that turns a normal ultrasound into a 3D image is showing promise in making thermal ablation for liver cancer treatment more accurate in a study from Lawson and Western University. Thermal ablation – using heat to destroy a cancerous tumour – can have fewer complications and a shorter recovery time than surgery. Read more.

10. Assessing neurofeedback in stroke survivors
Functional near-infrared spectroscopy (fNIRS) is used to detect changes in brain oxygen levels using light, but more recently it has also been used to develop brain-computer interfaces – allowing patients with brain injuries to control a device with their thoughts. Researchers at Lawson launched a new study to assess whether fNIRS can be used to improve patient outcomes during stroke rehabilitation. Read more.
11. Specific type of inflammation may be linked to risk of colorectal cancer
A preclinical study found that a specific type of inflammation may be linked to an increased risk of colorectal cancer. Previously, the degree of inflammation caused by illnesses like colitis, Crohn’s disease and other forms of inflammatory bowel disease were shown to be an important indicator of the development of colorectal cancer. However, this new study found the type of inflammation, rather than the severity and duration, may be more important in determining cancer risk. Read more.

12. New study examining if probiotics can improve outcomes in knee replacement surgeries
Lawson researchers launched a study to assess whether daily probiotics can improve outcomes in patients undergoing a total knee replacement surgery. Of the more than 70,000 knee replacement surgeries in Canada each year, nearly 10 per cent of patients experience complications. With patients who are considered healthy likely to have better outcomes, the research team is interested in improving the gut microbiome as a way to support patients’ overall health. Read more.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
An online approach to care
With an aging population, neurological conditions like stroke, brain injury and multiple sclerosis (MS) are on the rise in Canada. Those living with neurological conditions face many long-term challenges that can affect both their physical and cognitive functioning. They are also at an increased risk for mental health challenges such as depression and anxiety.
“While mental health challenges are common for those with neurological conditions, they often go untreated for a number of reasons,” says Dr. Swati Mehta, Scientist at Lawson Health Research Institute. “For example, those living in remote areas often do not have access to specialized services and many patients are concerned about stigma.”
Yet seeking mental health care is critically important for patients with neurological conditions. “Research suggests that depression among these patients can impair recovery, leading to decreased quality of life and increased health care costs.”
To improve patient outcomes, Dr. Mehta and a collaborative research team are developing an internet-delivered cognitive behavioural therapy (ICBT) program.

Cognitive behavioural therapy (CBT) is a specialized type of therapy that involves patients learning strategies and skills to self-manage mental health symptoms. It’s one of the most widely used therapies for the treatment of depression and anxiety.
A panel of researchers, persons with lived experience of neurological conditions and community organizations are working collaboratively to develop an accessible ICBT program that meets the needs of persons with neurological conditions and mild cognitive impairment who are also experiencing symptoms of depression or anxiety. The program, called The Neuro Course, will be a modified version of an existing course developed in Australia by the eCentreClinic.
“Through co-development with patients and experts in the field, the ICBT program will meet the specific needs of persons with neurological conditions who are also experiencing mental health challenges,” explains Dr. Mehta. “With online delivery, it can provide personalized treatment while being flexible and easily accessible.”
The Neuro Course will be piloted with a small group of research participants, including patients from Parkwood Institute, a part of St. Joseph’s Health Care London. Eligible participants can sign up to be notified of the course’s availability at https://www.onlinetherapyuser.ca/neuro.
The free online course consists of six easy-to-understand CBT lessons and will take approximately 10 weeks to complete. In addition to the six lessons, participants will be encouraged to work through various activities during the week.
Participants will also receive regular support from a designated online guide. Guides will be health educators who are certified providers or graduate students working under the supervision of certified providers. All guides will have training in psychology or social work. The participant’s guide will review the participant’s progress and answer any questions or comments through a secure messaging system.
Participants in the study will be asked to complete brief questionnaires before they begin the course, on a weekly basis throughout the course and then again three months after treatment ends. The research team will use the questionnaires to assess patient outcomes and improve future versions of the course.
The goal of the program is to overcome barriers to face-to-face therapy, such as limited access to specialized care and concerns about stigma related to seeking care, by providing an effective online alternative. By reaching those in need, the research team hopes to improve patient outcomes and overall wellbeing.
“The long term goal would be to implement the ICBT program into clinical practice to provide increased access to mental health services among this population,” says Dr. Mehta. “The program could be used to provide care to those with mild to moderate mental health concerns or those waiting to access face-to-face programs.”
The team is being funded for this project through Lawson’s Internal Research Fund (IRF) competition. “As an early career researcher, receiving funding from Lawson’s IRF is a great honour. It’s a great opportunity to help researchers obtain funding for small feasibility studies to develop evidence for larger grants that can be used to translate knowledge across the community,” states Dr. Mehta.
Antioxidants in the brain linked to improved treatment results in patients with psychosis
LONDON, ON – New research from Western University and Lawson Health Research Institute demonstrates that increased antioxidant levels in the brain may improve outcomes of early intervention in psychosis. In the paper published in Nature Molecular Psychiatry, the research team found that patients with higher levels of an antioxidant called glutathione responded more quickly to medication for psychosis and had improved outcomes.
“Once patients with psychosis start treatment, some get better in weeks while it can take months for others. We wanted to see if we could understand and influence this disparity,” said Dr. Lena Palaniyappan, Associate Professor at Western’s Schulich School of Medicine & Dentistry and Scientist at Lawson Health Research Institute. “We found that the amount of antioxidants that patients have in their brains predicts the time that it takes for them to respond to treatment.”
Previous research has shown that patients who respond early to antipsychotic medications have better overall outcomes in terms of symptoms and daily functioning. The research team has estimated that a 10 per cent increase in antioxidants could lead to a reduction in length of hospital stay by at least seven days.
“This study demonstrates that if we can find a way to boost the amount of antioxidants in the brain, we might be able to help patients transition out of hospital more quickly, reduce their suffering more quickly and help them return earlier to their work and studies,” said Dr. Palaniyappan who is also the Tanna Schulich Endowed Chair in Neuroscience and Mental Health at Western.
Antioxidant levels in the brain vary naturally from person to person and those variations can be attributed to lifestyle choices like exercise and diet. There are also ways to pharmaceutically boost these levels. A supplement called N-Acetyl Cysteine (NAC) as well as broccoli extracts can increase the brain’s antioxidants if given over a long period of time.
Dr. Palaniyappan and his team used high-field MRI imaging to examine antioxidant levels in the brains of 37 new patients to the Prevention and Early Intervention for Psychoses Program (PEPP) at London Health Sciences Centre. Antioxidant levels were studied prior to beginning treatment for psychosis and followed up for six months post-treatment.
The MRI scans were acquired at Western’s Centre for Functional and Metabolic Mapping at the Robarts Research Institute with the support of Western's BrainsCAN and the Canadian Institutes of Health Research.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Antioxidants in the brain linked to improved treatment results in patients with psychosis
Once patients with psychosis start treatment, some get better in weeks while it can take months for others.
“We wanted to see if we could understand and influence this disparity,” said Dr. Lena Palaniyappan, Associate Professor at Western’s Schulich School of Medicine & Dentistry and Scientist at Lawson Health Research Institute who is looking at chemicals in the brain with the aim of speeding up the time it takes a patient to respond to medication for psychosis.

The research team from Lawson and Schulich Medicine & Dentistry studied antioxidant levels in the brain, and found that these chemicals which rid the body of normal metabolic biproducts called free radicals, may improve outcomes of early intervention in psychosis. They looked specifically at an area of the brain called Cingulate Cortex which is well connected to a network of regions that play a major role in generating symptoms of psychosis.
The study, published in Nature Molecular Psychiatry, showed that patients with higher levels of an antioxidant called glutathione responded more quickly to medication for psychosis and had improved outcomes. They estimated that a 10 per cent increase in antioxidants could lead to a reduction in length of hospital stay by at least seven days.
“This study demonstrates that if we can find a way to boost the amount of antioxidants in the brain, we might be able to help patients transition out of hospital more quickly, reduce their suffering more quickly and help them return earlier to their work and studies,” said Dr. Palaniyappan who is also the Tanna Schulich Endowed Chair in Neuroscience and Mental Health at Western.
Antioxidant levels in the brain vary naturally from person to person and those variations can be attributed to lifestyle choices like exercise and diet. There are also ways to pharmaceutically boost these levels. A supplement called N-Acetyl Cysteine (NAC) as well as broccoli extracts can increase the brain’s antioxidants if given over a long period of time.
Dr. Palaniyappan and his team in collaboration with Dr. Jean Theberge at Lawson Imaging used high-field MRI imaging to examine antioxidant levels in the brains of 37 new patients to the Prevention and Early Intervention for Psychoses Program (PEPP) at London Health Sciences Centre. Antioxidant levels were studied prior to beginning treatment for psychosis and followed up for six months post-treatment.
The MRI scans were acquired at Western’s Centre for Functional and Metabolic Mapping at the Robarts Research Institute with the support of Western's BrainsCAN and the Canadian Institutes of Health Research.