Search
Search
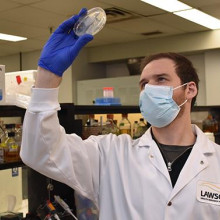
Lawson Impact Awards Staff Award of Excellence: Dr. Jeff Weiler
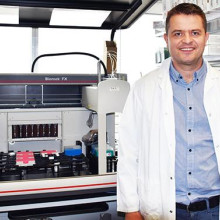
Dr. Jeff Weiler is being recognized for his role in helping launch the Gray Centre for Mobility and Activity.
Dedicated to helping enhance research to improve patient care, Dr. Jeff Weiler has won the 2022 Lawson Staff Award of Excellence.
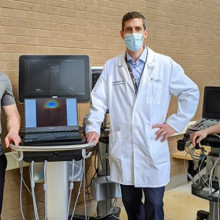
Dr. Weiler began his career with Lawson in 2020 and has been instrumental in helping launch the Gray Centre for Mobility and Activity as the coordinator of the program.
Established in 2020, The Gray Centre at St. Joseph’s Health Care London is expanding and advancing mobility and rehabilitation treatment and prevention solutions through research and collaborations. The Centre uses the latest technology to improve the lives of those living with disease, disability or injury.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Lawson Impact Awards: Strategic Research Fund Award 2022
Lawson Strategic Research Fund winners are using imaging to improve patient care and outcomes
Scientists at Lawson Health Research Institute are being recognized for their advanced imaging work by winning two Strategic Research Funds which will supports projects that advance science and generate high impact health solutions for patients.
Using advanced imaging to improve hip replacement outcomes
Dr. Matthew Teeter, Lawson Scientist, and Dr. Jonathan Thiessen, Lawson Imaging Scientist at St. Joseph’s Health Care London are using PET/MRI to better understand negative reactions in patients who have had total hip replacement surgery.
Improving outcomes for stroke patients
PET/MRI technology is also being used by another group of Lawson researchers to study inflammation that sometimes occurs in the heart following a stroke, headed by Dr. Luciano Sposato, Lawson Scientist and Neurologist at London Health Sciences Centre (LHSC) and Dr. Frank Prato, Scientist at Lawson and Lead for the Lawson Imaging research program.
Lawson ranks in top ten among Canada's research hospitals
Lawson Health Research Institute – the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London – is ranked seventh in the country in Re$earch Infosource’s 2023 list of Canada’s Top 40 Research Hospitals.
This is the 13th year in a row that Lawson has ranked top ten in the country, and the seventh-place ranking is up two spots from 2022 – highlighting continued dedication to hospital-based research at LHSC and St. Joseph’s.
Lawson also ranked second for research intensity among the large tier institutions with more than $776,000 of research spending per researcher.
“These rankings help LHSC and St. Joseph’s assess how we compare to similar hospitals across the country,” says Dr. David Hill, Scientific Director at Lawson and Integrated Vice President, Research at LHSC and St. Joseph’s. “Our continuous placement in the top 10 of all research hospitals shows we are doing important and relevant medical research that is making a difference to patient care.”
Lawson has been at the forefront of research in a wide range of specializations, making advances in areas from cancer care and mental health supports to molecular imaging and theranostics in recent years.
“Conducting research in hospitals means it can go from bench to bedside much more quickly,” says Dr. Hill. “Things move much faster now than they ever did. Our top 10 ranking shows we are leading the way, and that funders are confident in London’s hospital-based researchers.”
The top 40 list analyzes hospital-based research institutes from across the country on several metrics, including total research expenditure from the previous fiscal year. The ranking looks at funds from all sources, including both internal and external, to support research in hospitals.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Lawson ranks in top ten of Canada’s research hospitals
See all Lawson Media Releases
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Lawson ranks in top ten of Canada’s research institutes
For the 12th year in a row, Lawson Health Research Institute has ranked top ten in the country for the 2022 edition of Canada’s Top 40 Research Hospitals List by Re$earch Infosource.
Lawson, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has ranked in ninth place, and has also maintained the top ranking for research intensity among the large tier institutions with more than $700,000 of research spending per researcher.
“The most important metric is how we are growing year by year as an effective hospital research community,” says Dr. David Hill, Scientific Director at Lawson and Integrated Vice President, Research at LHSC and St. Joseph’s. “The rankings give us a measure of how we are comparing to peer hospitals across the country.”
Hospital-based research has been at the forefront since the COVID-19 pandemic began. The hard work and innovation to take research from bench to bedside during such a critical time has made a difference in patient outcomes around the world.
“Today’s research innovation is tomorrow’s health care. We need to maximize the former while shortening the gap between the two as much as possible. Being recognized in the top 10 reflects confidence research funders have in London’s hospital-based scientists.” says Dr. Hill.
The top 40 list analyzes hospital-based research institutes from across the country on several metrics, including total research income from the previous fiscal year. Lawson received $129,832 million in research income in 2022. The ranking looks at funds received from all sources, including both internal and external, to support research at LHSC and St. Joseph’s.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Lawson researchers win American Shoulder and Elbow Surgeons’ Neer Award
The American Shoulder and Elbow Surgeons association has awarded a team of London researchers the 2017 Charles S. Neer Award for Clinical Science, one of the most prestigious awards in the areas of shoulder and elbow surgical research in North America.
The award recognizes the scientists’ development of the PCR-RFLP (polymerase chain reaction restriction fragment length polymorphism) assay, a test that can accurately identify Propionibacterium acnes (P acnes) infection of the shoulder within 24 hours. Current methods take an average of six or more days, and are prone to sample contamination and false-positive results.
“We are incredibly honoured to receive this award,” says Dr. David O’Gorman, Lawson scientist, Co-Director of Molecular and Cellular Research at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London, and senior author of the publication. “We believe it illustrates the high quality of research being done at Lawson and marks the beginning of another clinically relevant research program at HULC.”
P acnes is a type of bacteria typically found deep in the hair follicles and sebaceous pores of the skin. A P acnes infection of the shoulder is a common and serious complication that occurs after arthroplasty (surgery to replace a damaged joint, most commonly with artificial material). It can cause pain in the shoulder joint and often loosens the implant. In most cases, the patient requires additional surgery to remove the infection and replace the implant.
It can be difficult to diagnose a P acnes infection as it often presents without symptoms that would be characteristic of an infection, such as pain, skin reddening or wound drainage. The prevalence of P acnes in the deeper layers of the skin also increases the chance of sample contamination and false-positive results making it hard to isolate and identify in a pathology lab.
Currently P acnes infection is identified by administering a tissue swab for anaerobic culture, which takes an average of six or more days but could take up to three weeks. This technique also carries substantial risk of contamination from the adjacent skin and other sites where P acnes is present.
The PCR-RFLP assay can identify P acnes in tissue from a shoulder biopsy within a 24-hour period. The extremely sensitive technology also has the ability to detect fewer than ten P acnes cells in the sample, which may decrease the false-positive rate in cultures caused by swab contamination.
“The accuracy of this test and the shorter period of time needed for identification can help with treatment decision making, targeted antibiotic therapy, and monitoring to minimize implant failure and revision surgery,” explains Dr. O’Gorman, who is also an Assistant Professor in the Departments of Surgery and Biochemistry at Western University’s Schulich School of Medicine & Dentistry. “We hope that the test can be further developed into a ‘point of case’ assay that can detect P acnes in tissue samples in real time while the patient is undergoing shoulder surgery.”
Since the PCR and RFLP mapping used for the assay are techniques routinely performed in many clinical microbiology and pathology labs, the test would be a cost-efficient approach not restricted to highly specialized research labs.
Other scientists who were part of the study include Dr. George Athwal and Dr. Kenneth Faber, HULC orthopaedic surgeons, Lawson scientists and Schulich professors; Ana Pena Diaz, research technician for the HULC Molecular and Cellular Biology Research Lab; and Scott Holmes, a medical student and Schulich Research Opportunities Program participant who was primarily responsible for designing and optimizing the assay.
Both Dr. O’Gorman and Dr. Faber are also members of Western’s Bone and Joint Institute.
“A rapid method for detecting Propionibacterium acnes in surgical biopsy specimens from the shoulder” was published in the Journal of Shoulder and Elbow Surgery (JSES).
Lawson study validates new biopsy method for breast cancer patients
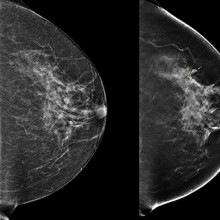
In a newly published study in the American Journal of Roentgenology, a team at Lawson Health Research Institute was the first in North America to find that a new breast cancer biopsy method may offer a more accurate and comfortable option for patients.
The method is a new form of mammography software that combines contrast enhanced mammography (CEM) with mammography guided biopsy technology at St. Joseph’s Health Care London’s Breast Care Program. These tools were combined in an effort to make the biopsy procedure more streamlined, accurate, and easier for patients and technicians.
CEM is a relatively new form of mammography that uses contrast iodine injected intravenously, which acts like a dye that allows radiologists to spot potential cancerous lesions more effectively. If potential lesions are found, a biopsy is often the next step.
Before this option was made available to patients through this research, suspicious lesion detection that was only seen on contrast enhanced mammography were biopsied under MRI. This meant longer procedures, and working with limited MRI availability.
“If a lesion is detected only by CEM we usually offer an MRI guided biopsy, but we first need to find the same lesion on an MRI,” says Dr. Anat Kornecki, Lawson Associate Scientist and Breast Radiologist Lead at St. Joseph’s Health Care London. “The problem is that it is sometimes hard to find the same lesion and the MRI itself can be uncomfortable for the patient. Also, some lesions that are close to implants or chest walls cannot be reached with MRI guided biopsy.”
Dr. Kornecki and her research team therefore decided to study this new method. They were the first in North America to trial CESM-guided biopsies by using new technology created by GE HeathCare. This software means that patients can have the biopsy done with the exact same modality, avoiding the need for an MRI.
The study included 50 patients through St. Joseph’s Breast Care Program. The research team found 51 potentially cancerous breast lesions. Biopsies were successfully performed for 46 of the lesions. The results showed that 11 were breast cancer, 10 were high-risk lesions, and the remaining were benign lesions.
“These are very similar results that were reported through MRI-guided biopsies, which means that this new method can replace the MRI,” explains Dr. Kornecki.
Patients also reported having a more comfortable experience with the CEM-guided biopsy method.
Researchers in London and at two other centres in Europe were the first to pilot this technique which has now been cleared by Health Canada and the FDA commercially. St. Joseph’s Breast Care Program was the first site in North America to offer this procedure as a clinical standard of care.
“It is a game changer with certainty,” adds Dr. Kornecki. “This is now a great added component for patients, which makes it a very good tool.”
Currently, CEM- guided biopsy can be offered to patients with lesions that were initially detected by MRI where a biopsy is not feasible due to the lesion location. While it is currently being used as a diagnostic tool only, Dr. Kornecki is hopeful that eventually CEM-guided biopsies will be approved as an initial breast cancer screening tool as well.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Lawson study validates new biopsy method for breast cancer patients
In a newly published study in the American Journal of Roentgenology, a team at Lawson Health Research Institute was the first in North America to find that a new breast cancer biopsy method may offer a more accurate and comfortable option for patients.
The method is a new form of mammography software that combines contrast enhanced mammography (CEM) with mammography guided biopsy technology at St. Joseph’s Health Care London’s Breast Care Program. These tools were combined in an effort to make the biopsy procedure more streamlined, accurate, and easier for patients and technicians.
CEM is a relatively new form of mammography that uses contrast iodine injected intravenously, which acts like a dye that allows radiologists to spot potential cancerous lesions more effectively. If potential lesions are found, a biopsy is often the next step.
Before this option was made available to patients through this research, suspicious lesion detection that was only seen on contrast enhanced mammography were biopsied under MRI. This meant longer procedures, and working with limited MRI availability.
“If a lesion is detected only by CEM we usually offer an MRI guided biopsy, but we first need to find the same lesion on an MRI,” says Dr. Anat Kornecki, Lawson Associate Scientist and Breast Radiologist Lead at St. Joseph’s Health Care London. “The problem is that it is sometimes hard to find the same lesion and the MRI itself can be uncomfortable for the patient. Also, some lesions that are close to implants or chest walls cannot be reached with MRI guided biopsy.”

Dr. Kornecki and her research team therefore decided to study this new method. They were the first in North America to trial CESM-guided biopsies by using new technology created by GE HeathCare.This software means that patients can have the biopsy done with the exact same modality, avoiding the need for an MRI.
The study included 50 patients through St. Joseph’s Breast Care Program. The research team found 51 potentially cancerous breast lesions. Biopsies were successfully performed for 46 of the lesions. The results showed that 11 were breast cancer, 10 were high-risk lesions, and the remaining were benign lesions.
“These are very similar results that were reported through MRI-guided biopsies, which means that this new method can replace the MRI,” explains Dr. Kornecki.
Patients also reported having a more comfortable experience with the CEM-guided biopsy method.
Researchers in London and at two other centres in Europe were the first to pilot this technique which has now been cleared by Health Canada and the FDA commercially. St. Joseph’s Breast Care Program was the first site in North America to offer this procedure as a clinical standard of care.
“It is a game changer with certainty,” adds Dr. Kornecki. “This is now a great added component for patients, which makes it a very good tool.”
Currently, CEM- guided biopsy can be offered to patients with lesions that were initially detected by MRI where a biopsy is not feasible due to the lesion location. While it is currently being used as a diagnostic tool only, Dr. Kornecki is hopeful that eventually CEM-guided biopsies will be approved as an initial breast cancer screening tool as well.
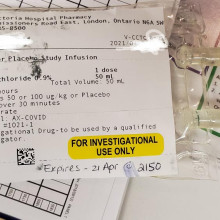
Lawson teams respond rapidly to call for research
When cases of COVID-19 began spreading in the London region, Lawson Health Research Institute (Lawson) had to rapidly adjust to a new environment.
As a hospital based research institute, Lawson is uniquely positioned to address the medical questions posed by a new virus. The expertise and infrastructure to begin these investigations was already in place. The global shortage of supplies, as well as physical distancing measures, forced many research projects to be put on hold. Other areas, however, were ramping up their work to support the scientists and physicians eager to figure out how we can better prevent, detect, and treat patients with COVID-19.
Lawson Clinical Research Services (LCRS) and the Center for Clinical Investigation and Therapeutics (CCIT) got to work immediately. The teams responded rapidly to research requests, getting new studies up and running within days.

Carolina Gillio Meina, Research Associate
Dr. Douglas Fraser, Lawson Scientist and Paediatric Critical Care Physician at London Health Sciences Centre (LHSC), initiated a study to examine the immune response in patients with COVID-19. Reports from other parts of the world identified a heightened immune response in more severe cases of the infection, also labeled the ‘cytokine storm’. Laboratories at Lawson were ready to handle this type of research, as close proximity to patients and sample collection is essential.

“Our world changed almost overnight,” adds Tereschyn. “We had to pivot on a dime and change the entire way we do business. Our staff have really risen to the challenge.”

Mala Ramu (left) and Sangeetha Balaji (right), Lawson Clinical Research Services
The LCRS and CCIT teams are supporting essential research in other ways as well, including logistics and administrative support, and supply sharing.
“We’ve developed many new partnerships throughout this pandemic, and figured out in very short order how to work efficiently together,” says Tereschyn. “While COVID-19 has presented us with many challenges, it has also been a great opportunity for us to support one another in ways that I don’t believe would have transpired otherwise.”
Lawson welcomes nursing students from South Korea
Dr. Dalton Wolfe, scientist, Lawson Health Research Institute, led a tour of the physiotherapy gym at St. Joseph Health Care London’s Parkwood Institute for 14 nursing students from Kyungil University in South Korea.
The nursing students have spent six weeks in Canada as part of the Health Care and English as a Second Language Program at King’s University College, during which they focused on English as a language instruction with a focus on medical terminology.
Dr. Wolfe showcased various physiotherapy tools, including a locomat and exoskeleton and explained how holistic and practice-based research can lead to better patient outcomes.

Lawson's Top 12 Research Stories from 2020
Image

3D imaging technology could improve outcomes for patients with breast cancer
During a conventional digital 2D mammogram, two x-ray images are taken of the breast, one from top-to-bottom and another from side-to-side at an angle. This technology is limited by the overlapping breast tissue that occurs from the required compression of the breast, and breast abnormalities may be hidden. A study at Lawson is looking to determine if digital breast tomosynthesis, a type of 3D imaging, is better at detecting breast tissue abnormalities than the 2D mammography regularly used today. Read more.
Image

Antioxidants in the brain linked to improved treatment results in patients with psychosis
Once patients with psychosis start treatment, some get better in weeks while it can take months for others. A research team from Lawson and Western University studied antioxidant levels in the brain, and found that these chemicals, which rid the body of normal metabolic biproducts called free radicals, may improve outcomes of early intervention in psychosis. Read more.
Image

Researchers awarded $4.8 million to validate locally developed test, EpiSign, for first-line diagnostic testing of rare hereditary disorders
A clinical trial named “EpiSign-CAN,” led by researchers at Lawson was awarded $4.8 million to measure the clinical impact of a new molecular genomics test for diagnosing genetic neurodevelopmental conditions. The diagnostic test, called EpiSign, uses machine learning to analyze the EpiSign Knowledge Database. This database compiles information on rare genetic diseases using laboratory analyses of the entire genome, referred to as the epigenome, from patients with suspected genetic abnormalities. Read more.
Image


Perceptions of confidentiality for Canadian Veterans discussing moral injuries
Lawson researchers are exploring Canadian Veterans’ beliefs about confidentiality in mental health care and whether those beliefs act as a barrier to seeking treatment for a type of trauma known as moral injury. Moral injury describes psychological distress following events where a person performs, witnesses or fails to prevent acts that conflict with deeply held moral standards. Evidence suggests that moral injuries are on the rise among deployed members of the Canadian Armed Forces, and that those exposed to such events are at a higher risk of developing post-traumatic stress disorder and depression. Read more.
Image


New device could reduce COVID-19 infection risk and demand for invasive ventilators
Researchers designed a non-invasive ventilation mask that could significantly reduce aerosolization – the production of airborne respiratory droplets that may contain viruses or bacteria – when treating patients with COVID-19. The new device aims to reduce infection risks associated with non-invasive ventilation and lessen the demand for invasive ventilators. It is currently being tested through a clinical trial with patients at London Health Sciences Centre (LHSC). Read more.
Image


Researchers first in world to profile the body’s immune response to COVID-19
By studying blood samples from critically ill patients at LHSC, researchers identified a unique pattern of six molecules that could be used as therapeutic targets to treat COVID-19. Studies show that part of what makes the virus so deadly is that the body mounts an overreactive immune response as the virus grows and replicates. This response releases inflammatory molecules in order to fight the virus, but also destroys healthy cells and organs in the process. Read more.
Image


Study suggests that surgery may be superior treatment for chronic sciatica
In a randomized controlled trial, surgery was found to be superior to non-operative therapy in the treatment of chronic sciatica. Chronic sciatica can be caused by a disc herniation which compresses a nerve in the lumbar spine causing pain from the lower back to the leg. The primary treatment options for sciatica are surgery or non-operative care. Researchers conducted this study to test if a surgical treatment called microdiscectomy results in better patient outcomes for those with chronic sciatica compared to non-operative care. Read more.
Image


Researchers unravel two mysteries of COVID-19
A team from Lawson and Western University made significant steps forward in understanding COVID-19 through two back-to-back studies. In one study, the team identified six molecules that can be used as biomarkers to predict how severely ill a patient will become. In the other study, they were the first to reveal a mechanism causing blood clots in COVID-19 patients and potential ways to treat them. The studies were conducted by analyzing blood samples from critically ill patients at LHSC. Read more.
Image

Gut microbiome may influence how cancer patients respond to oral therapies, study suggests
A study from Lawson and Western illustrated how the gut microbiome interacts with an oral medication in prostate cancer patients, suggesting bacteria in the gut play a role in treatment outcomes. The findings highlight how the drug abiraterone acetate is metabolized by bacteria in the gut to reduce harmful organisms while promoting those that fight cancer. The research team suspects this is one of many examples of how the microbiome influences our response to medications. Read more.
Image

First Contrast Enhanced Spectral Mammography guided biopsy in North America
Researchers at Lawson performed the first breast biopsy guided by Contrast Enhanced Spectral Mammography (CESM) in North America on June 12, 2020. CESM is a novel diagnostic imaging tool that is able to detect cancerous lesions at a greater rate than standard mammography, and at close rate to MRI. The procedure is faster and more accurate, comfortable and cost effective than an MRI biopsy. Read more.
Image


Assessing the pandemic's impact on Canadian Veterans and their spouses
A project from Lawson and the Centre of Excellence on Post-Traumatic Stress Disorder (PTSD) hopes to discover the impact the COVID-19 pandemic is having on the mental health of Canadian Veterans and their spouses. They are partnering with up to 1,000 Canadian Veterans and 250 spouses of Canadian Veterans. Through online surveys, the project will hear directly from Veterans and their spouses to assess the pandemic’s effects on their well-being over time. Read more.
Image


Fecal transplants show promise as treatment for non-alcoholic fatty liver disease
A randomized controlled trial found that fecal transplants in patients with non-alcoholic fatty liver disease (NAFLD) results in a reduction in how easily pathogens and other unwanted molecules pass through the human gut and into circulation, known as intestinal permeability. The results could have implications for the treatment of numerous conditions including metabolic syndrome and autoimmune diseases. Read more.
Lawson's top 12 research stories of 2021
Lawson researchers impact the lives of people not just locally, but around the world with groundbreaking studies and translational research that enhances care, health and wellbeing.
Here are some of the research highlights of 2021.
Differences in walking patterns could predict type of cognative decline in older adults

Canadian researchers are the first to study how patterns in the way older adults walk could more accurately diagnose different types of dementia and identify Alzheimer’s disease. A new study by a Canadian research team, led by London researchers from Lawson Health Research Institute and Western University, evaluated the walking patterns and brain function of 500 participants currently enrolled in clinical trials. Read more.
COVID-19 shown to leave a unique lung fingerprint
Researchers at Lawson Health Research Institute have developed and tested an artificial neural network for diagnosing COVID-19. The AI system was trained to learn and recognize patterns in ultrasound lung scans of patients with confirmed COVID-19 infection at London Health Sciences Centre (LHSC) and compared them to ultrasound scans of patients with other types of lung diseases and infections. Read more.
Kidney transplant patient experiences positive recovery with the help of a simple device

Getting the gift of life was an amazing moment for 68-year-old Ruben Garcia who was in late-stage kidney disease and starting dialysis when his daughter Ruby donated one of her kidneys to him. The father of four underwent transplant surgery this past March and remained in hospital for nine days recovering. Following his surgery, Garcia found it difficult to get out of bed due to pain and swelling, leaving the function of his new kidney at a very low level. Read more.
Air pollution exposures contributes to childhood asthma, population-based study shows

New findings from Ontario have shown that children born in Sarnia have a higher risk of developing asthma compared to neighboring cities. A research team from Lawson Health Research Institute and Western University, using provincial data from ICES, found that higher air pollution exposure in the first year of life very likely contributed to this higher risk. Read more.
Getting the data on homelessness

At a virtual event, a research team led by Lawson Health Research Institute announced details of a new project aimed at better understanding how many people in Canada are homeless and who they are. Developing more accurate sources of data related to homelessness helps ensure the proper supports and services are available. Read more.
Clinical trials begin to treat COVID-19 patients with sepsis
It’s a discovery that has been more than ten years in the making: the use of a human protein to potentially treat patients with sepsis. Lawson Scientist Dr. Qingping Feng noticed that a human protein called annexin A5 showed positive results with sepsis back in 2007. Fast forward 14 years later to now, and this discovery could very well be the first ever viable treatment for sepsis patients, including severe COVID-19 patients who develop sepsis. Read more.
Examining the health impact the COVID-19 pandemic is having on mothers and their new babies

It has been a challenging year for many with the ongoing COVID-19 pandemic creating changes to people’s lifestyles, education, employment and health care. The impacts of these changes may be posing a health risk to women who have given birth during this trying time, and for their babies. Read more.
New therapeutic tool proven effective for MS patients with mental health challenges

It was a diagnosis that came as a shock for 28-year-old Mitch Kuska who found out he had Multiple Sclerosis (MS) at the age of 26. “I went from being a young 26-year-old doing regular things, to having to learn about this disease and everything that goes along with it and how it will affect my life.” Kuska, an avid cyclist, says knowing that one day he may not be able to physically do the things he loves has been the hardest part of his MS journey so far. Read more.
Researchers using MRI scans to pinpoint moral injury effects in health care workers


Moral injury refers to an injury to an individual’s moral conscious, which can produce profound emotional guilt and shame. Recognizing this is a growing concern, a London research team from Lawson Health Research Institute and Western University’s Schulich School of Medicine & Dentistry is examining moral injury amongst health care workers by imaging the effects on the brain. Read More.
Scientists studying carbon monoxide as a possible treatment for sepsis

Sepsis is a life-threatening condition that occurs when the body’s response to an infection triggers excessive inflammation. The inflammatory response can cause damage to organs such as the heart, liver, lungs and brain. While there are currently limited treatments for sepsis, researchers at Lawson Health Research Institute are working to change that by examining the use of carbon monoxide-releasing molecules to treat patients. Read more.
Global study on heart valve repair surgery will improve patient outcomes around the world

Researchers at Lawson Health Research Institute and Western University had a leading role in a new global study that will change the way surgeons repair leaky valves in the heart. It’s one of the most common heart valve conditions, affecting around two per cent of the population, where many patients don’t even realize they have a leaky valve and are asymptomatic, often presenting to doctors once they are late stage into the disease. Read more.
New study will assess fecal transplants in treatment of pancreatic cancer

Pancreatic cancer is an aggressive disease that affects up to six-thousand Canadians a year and is the third leading cause of cancer deaths. In a new study a multidisciplinary team of scientists at Lawson Health Research Institute are examining the microbiome in the gut, as a possible gateway to improving treatment outcomes. Read more.
Leading the conversation on equity, diversity and inclusivity
The city of London, Ontario is home to a vibrant health research community. On Wednesday, May 9, researchers from across the city gathered to discuss the importance of equity, diversity and inclusivity (EDI) in the careers of health researchers. Through participation at Exchange: A London Health Research Day Forum on Diversity & Inclusivity, guests discussed the challenges associated with EDI and potential solutions for the future.
Exchange was held the evening before London Health Research Day, the region’s premier research showcase event which features nearly 400 trainee presentations. Trainees are the future of Canadian science and EDI is crucial to that future. This is a topic of national importance that has garnered attention and action from the federal government, funding agencies and scientists across the country.
Recognizing the importance of this topic, Canada’s Minister of Science, The Honorable Kirsty Duncan, and local Member of Parliament for London North Centre, MP Peter Fragiskatos, shared video greetings with Exchange guests.
“The Exchange event highlights a vital area of discussion. It is important to not only recognize but embrace the differences between scientists and the diverse perspectives they bring to research,” said Rebecca Sullivan, a third year PhD candidate at Western University’s Schulich School of Medicine & Dentistry, training in Savita Dhanvantari’s lab at Lawson Health Research Institute, and one of the organizers of the event. “Becoming aware of our own unconscious biases and trying to change these culturally ingrained implicit associations is the only way to make active change in science!”

Above: Rebecca Sullivan, a third year PhD candidate, leading a scenario-based group activity at Exchange
The evening’s first presenter was Dr. Janet Smylie, Director of the Well Living House Applied Research Centre for Indigenous Infant, Child and Family Health at St. Michael’s Hospital and CIHR Applied Public Health Research Chair in Indigenous Health Knowledge and Information. Dr. Smylie, who also delivered the keynote presentation at London Health Research Day, spoke about the role of anti-Indigenous racism and discrimination within health care professions, including its impact on research. This included a discussion of Dr. Smylie’s own research in the field of Indigenous health.

Above: Dr. Janet Smylie presenting on "Addressing anti-Indigenous racism and discrimination within health care professions"
Greta Bauer, PhD, a professor in the Department of Epidemiology and Biostatistics at Schulich Medicine & Dentistry, spoke about the role of epidemiology as a toolkit for building equity in health research. This included a discussion on incorporating intersectionality and multidimensionality into population health research methodology.
“The purpose of this work is to give researchers the measurement and statistical tools they need to shift the focus from studying broad population average effects to more heterogeneity within populations,” said Greta. “The whole point is to better study not only diversity in health outcomes, but in the processes that generate those outcomes.”

Above: Greta Bauer, PhD, presenting on "Epidemiology as a toolkit for building equity"
This talk was followed by a presentation on Gender-Based Analysis Plus (GBA+). GBA+ is an analytical tool used to assess how diverse groups of women, men and gender-diverse people may experience policies, programs and initiatives. The “plus” in GBA+ acknowledges that GBA goes beyond biological (sex) and socio-cultural (gender) differences. We all have multiple identity factors that intersect to make us who we are; GBA+ also considers many other identity factors, like race, ethnicity, religion, age, and mental or physical disability. GBA+ is a method for collecting and reviewing data in an unbiased manner, one that leaves aside many of the assumptions that can mask the GBA+ impacts of a given initiative. Alysha Croker, PhD, Manager, Tri-Agency Institutional Program Secretariat, discussed how GBA+ is being used in research and grant funding, including at the federal funding agencies.
“Diverse research teams can lead to more innovation, greater collective intelligence and an increased capacity to tackle complex issues,” said Alysha, when discussing the importance of EDI in the careers of health researchers.

Above: Alysha Croker, PhD, presenting on "Incorporating Gender-Based Analysis Plus (GBA+) in research and beyond"
The evening also included a presentation from Shantal Feltham, founder and CEO of Stiris Research, a North American clinical trials management company based in London. Shantal discussed the importance of ensuring that clinical trials are designed to recruit diverse research participants that represent real patient populations. She also discussed her own experiences and perspectives as a female entrepreneur.

Above: Shantal Feltham delivering a presentation titled "That’s a great idea – It’ll never work"
A group of health research trainees concluded the night with a scenario-based presentation and activity. Audience members were divided into small groups and given a diversity scenario to discuss. Topics ranged from the experiences of LGBTQ+ researchers, racial diversity, physical ability barriers in research labs and more. Notes and ideas from these conversations were recorded and displayed the next day at London Health Research Day.
“Exchange highlighted EDI in health research in action. It featured talks by leading female researchers on issues in Indigenous health and LGBTQ health, implementation of equity in the Canada Research Chairs program, and female entrepreneurship in the field of health research,” said Savita Dhavantari, PhD, assistant director and scientist at Lawson and assistant professor at Schulich Medicine & Dentistry. Savita was also one of the Exchange organizers and the facilitator for the event. “Above all, I hope attendees were encouraged to be fearless in advocating for equity, diversity and inclusivity in health research.”

Above: Guests at Exchange discussing a diversity scenario

Above: Savita Dhanvantari, PhD, facilitating the Exchange event
To see more photos from Exchange and London Health Research Day, visit the London Health Research Day website.
Exchange and London Health Research Day are presented in partnership by Lawson Health Research Institute and Western University’s Schulich School of Medicine and Dentistry.
Lens of compassion improves health care
Keynote speaker at joint mental health research day says compassion in action has proven benefit
Compassion in mental health care – and in all health care – is “what separates good from really great” patient outcomes, Calgary-based researcher Shane Sinclair, PhD, told mental health researchers during a conference Oct. 30, 2024, in London.
Sinclair, who heads the Compassion Research Lab at the University of Calgary, was the invited keynote speaker at the Joint Mental Health Research and Innovation Day, attended by about 130 people.
The event was hosted by Lawson Research Institute, London Health Sciences Centre Research Institute and Schulich School of Medicine & Dentistry.
The day also featured 17 poster presentations and 17 oral presentations on different aspects of mental health research. It’s one of the premier annual education-and-development events in mental health science regionally.
This year’s event showcased how compassion could transform health policy, partnerships, systems, care, research and service delivery.
Compassion, respect and excellence are core values of St. Joseph’s Health Care London.
Sinclair noted that the key role of compassion – responding to someone’s suffering with understanding and action – is evidence-based.
“We do patient-informed and patient-targeted research. And we’ve found compassion makes a difference in how people heal.”
-Shane Sinclair, PhD, compassion researcher
His lab examined the outcomes and satisfaction among patients at 14 emergency rooms across Alberta and found compassion to be the greatest predictor of quality care ratings.
“What separates good from really great comes down to compassion. These things matter,” Sinclair said.
“It improves their health and their quality of life. It reduces health-care costs, reduces adverse medical outcomes and helps build patients’ trust in the medical information and direction they receive,” he said.
Leveraging technology to diagnose psychiatric disorders
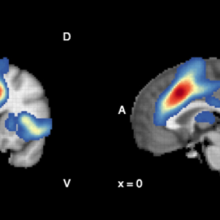
Psychiatric disorders are often difficult to diagnose. As research advances, we are learning there are multiple subtypes of illness that differ in symptoms and treatment needs, making classification even harder. Post-traumatic stress disorder (PTSD) is one example. Individuals with the more common type of PTSD experience active defensive responses like hyperarousal or outbursts of emotion while those with the dissociative subtype experience additional passive defensive responses like ‘shutting down’ or out-of-body experiences.
In a new study from Lawson Health Research Institute and Western University, researchers combined brain imaging and machine learning to classify with 92 per cent accuracy whether individuals had PTSD and whether or not it was the dissociative subtype. The results highlight the promise of brain imaging as a tool for early diagnosis of psychiatric illness, helping to predict symptom development and treatment needs.
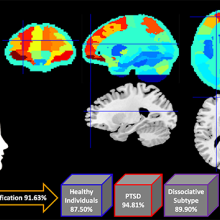
Brains scans and machine learning were combined to classify PTSD with 92 per cent accuracy.
The study involved 181 research participants, including those diagnosed with the more common form of PTSD, the dissociative subtype of PTSD, and healthy individuals with no history of PTSD. They participated in functional magnetic resonance imaging (fMRI) at St. Joseph’s Health Care London and Robarts Research Institute.
Researchers used the high-powered imaging to analyze patterns of resting-state brain activity where participants simply remained in a state of restful wakefulness in an fMRI scanner. The team found that unique patterns of brain activity differed significantly between the three groups.
“Our research group has been leading a number of studies that have shown differences in brain activity and neural connections between healthy individuals and those with different subtypes of PTSD,” says Dr. Ruth Lanius, a researcher at Lawson, professor at Schulich School of Medicine & Dentistry at Western University and psychiatrist at London Health Sciences Centre. “This study further validates that unique patterns of brain activity are associated with different forms of PTSD.”
In the second part of the study, the research team inputted the patterns of brain activity into a machine learning computer algorithm. They found the machine learning system could analyze brain scans to predict whether an individual had PTSD, the dissociative subtype of PTSD or no PTSD with 92 per cent accuracy.
“Our study suggests brain activity can be used to assist diagnosis of psychiatric disorders and help predict symptoms,” says Andrew Nicholson, PhD, lead author on the study and a post-doctoral fellow at Schulich Medicine & Dentistry who is conducting research at Lawson. “Patterns of brain activity are objective biomarkers that could be used to diagnose PTSD and, with more research, even predict response to treatment.”
Objective biomarkers hold promise for transforming psychiatric medicine.
“The field of psychiatry does not currently have objective biomarkers like those used to diagnose and understand other illnesses or diseases like cancer,” says Nicholson. “By discovering and validating patterns of brain activity as biomarkers, we can bring objective measures to psychiatry and transform patient care.”
The study, “Machine learning multivariate pattern analysis predicts classification of posttraumatic stress disorder and its dissociative subtype: A multimodal neuroimaging approach,” is published in Psychological Medicine.