Search
Search
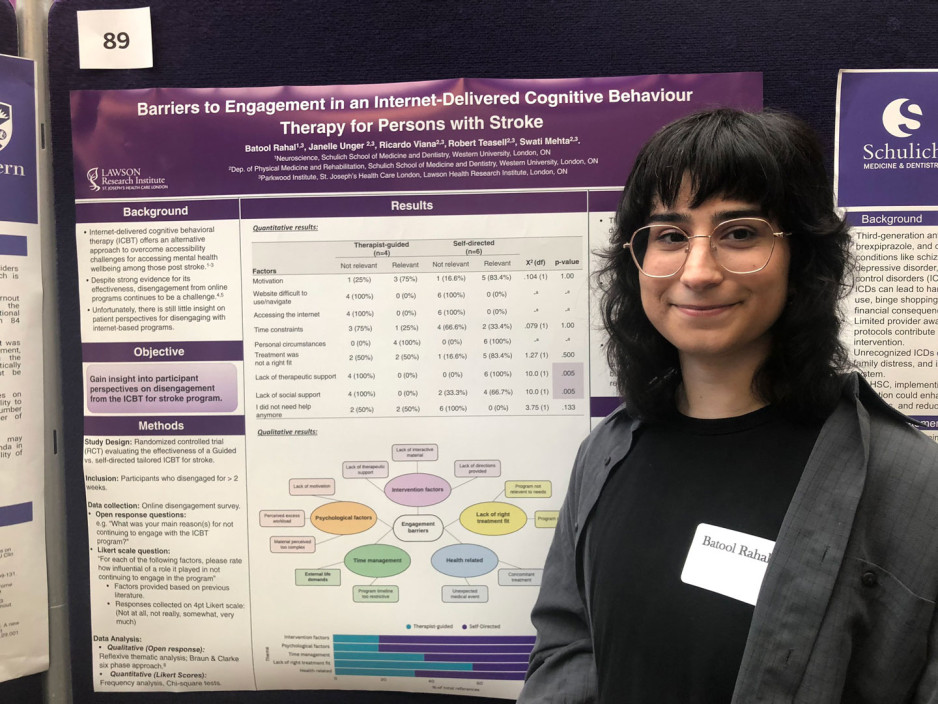
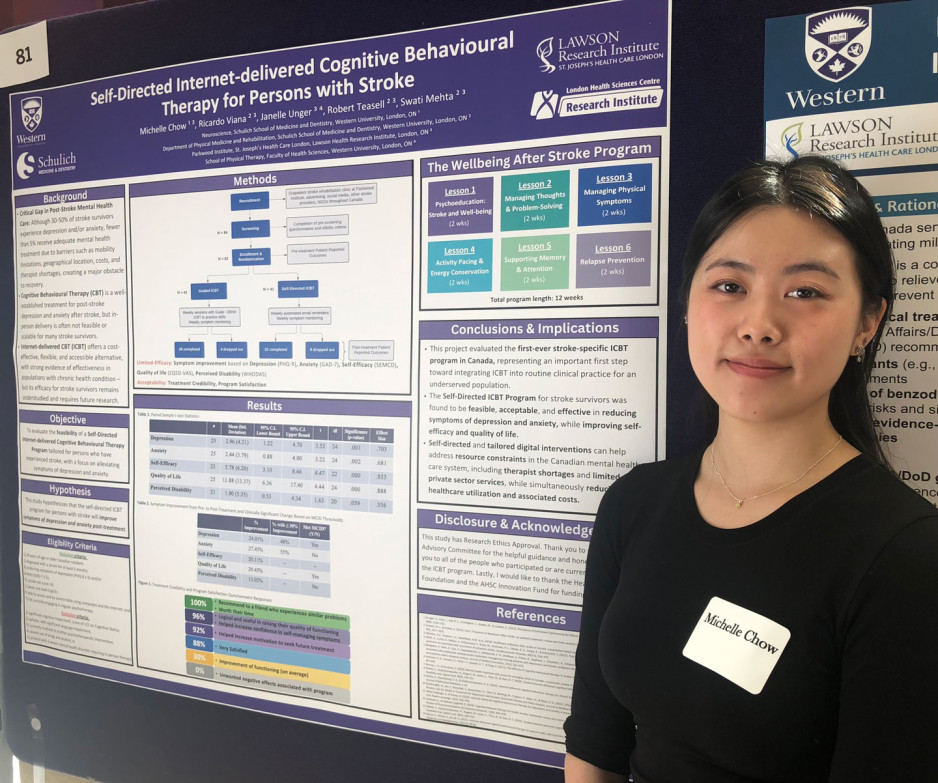
Student innovators showcase work at London Health Research Day 2025
The region’s largest celebration of emerging researchers’ work, London Health Research Day featured oral and poster presentations from undergraduates, grad students, postgraduates and trainees.
They shared their work with peers and globally renowned scientists in an array of specialized health and medical fields.
Their projects were as diverse as concussion treatment for children; large-language models to evaluate cancer diagnoses; brain imaging in people with dementia; and health system change to reduce surgical wait times.
Dozens of projects had Lawson Research Institute connections, included chronic pain’s impact on the brain; self-directed cognitive behavioural therapy for people recovering from stroke; and triaging care for people with shoulder injury.
Participants were also treated to a keynote address by Professor Francesca Ciccarelli, PhD, a global leader in cancer genomics who shared groundbreaking insights into the future of cancer research and precision medicine.
Her presentation was part of the Lucille and Norton Wolf Health Research Lecture Series through the generosity of the Bernard and Norton Wolf Family Foundation.
All told, about 500 people took in the day’s events, including several professional- and career-development workshops.
Student innovators showcase work at London Health Research Day 2025
The region’s largest celebration of emerging researchers’ work, London Health Research Day featured oral and poster presentations from undergraduates, grad students, postgraduates and trainees.
They shared their work with peers and globally renowned scientists in an array of specialized health and medical fields.
Their projects were as diverse as concussion treatment for children; large-language models to evaluate cancer diagnoses; brain imaging in people with dementia; and health system change to reduce surgical wait times.
Dozens of projects had Lawson Research Institute connections, included chronic pain’s impact on the brain; self-directed cognitive behavioural therapy for people recovering from stroke; and triaging care for people with shoulder injury.
Participants were also treated to a keynote address by Professor Francesca Ciccarelli, PhD, a global leader in cancer genomics who shared groundbreaking insights into the future of cancer research and precision medicine.
Her presentation was part of the Lucille and Norton Wolf Health Research Lecture Series through the generosity of the Bernard and Norton Wolf Family Foundation.
London Health Research Day is a shared project of Western’s Schulich School of Medicine & Dentistry, the Faculty of Health Sciences, Lawson Research Institute of St. Joseph's Health Care London and London Health Sciences Centre Research Institute.
All told, about 500 people took in the day’s events, including several professional- and career-development workshops.
Study casts doubt on clinical significance of gadolinium brain deposits
A new study from Lawson Health Research Institute and the Institute for Clinical Evaluative Sciences (ICES) has cast doubt on the clinical significance of brain deposits of gadolinium (a chemical contrast agent commonly used to enhance MRI imaging).
In 2015, the US Food and Drug Administration raised safety concerns over reports of retained gadolinium in the brain for patients undergoing four or more gadolinium-enhanced MRIs. The FDA launched an inquiry at the time, stating that “it is unknown whether these gadolinium deposits are harmful.” Pending further investigation, the FDA suggested limiting the use of gadolinium-based contrast agents (GBCAs) to circumstances where contrast information is clinically necessary, and to evaluate the need for repetitive GBCA MRIs based on treatment protocols.
Studies since that time have shown deposits of gadolinium may be found long after they are administered. They tend to concentrate in the globus pallidi, a region of the brain that can cause parkinsonian symptoms if it is damaged. Parkinson’s disease is an example of a specific brain disorder that is commonly associated with parkinsonian symptoms.
“Given the concern around possible neurotoxicity of gadolinium, and because these deposits were found in the globus pallidi region of the brain, we wanted to see if people exposed to gadolinium MRIs have higher rates of subsequent parkinsonism,” says Dr. Blayne Welk, the lead author of the study who is an adjunct scientist with ICES Western and Lawson.
To test a possible link between GBCAs and parkinsonism, Welk and his team examined anonymized health care records for 246,557 patients in Ontario over the age of 66 who underwent an initial MRI in a 10-year period between 2003 and 2013. They excluded patients whose initial MRI was of the brain or spinal cord and those with prior parkinsonism or neurosurgery. Comparing patients who were exposed to gadolinium-enhanced MRIs with patients whose MRIs did not include gadolinium enhancement, they looked for differences in rates of future parkinsonism symptoms or treatment.
They found that the rates of parkinsonism for exposed vs non-exposed patients were virtually identical, at 1.2 per cent. These findings indicate that there is no increased risk for parkinsonism associated with the use of gadolinium in MRIs.
However, the researchers caution that this study does not clear up all the worries about gadolinium, since they investigated only its connection to parkinsonism.
“While these findings should be reassuring for patients and their care providers that gadolinium exposure does not appear to be associated with higher risk of developing parkinsonism symptoms, there have been other reports of nonspecific neurologic symptoms including pain and cognitive changes associated with prior gadolinium exposure which do require further study,” comments Dr. Welk.
The researchers also note that gadolinium may have different effects in younger patients (who were not included in this study), or in those with neurologic diseases (who may have been excluded based on the types of MRIs included in this study).
“Association between Gadolinium contrast exposure and the risk of parkinsonism” was published on July 5, 2016 in the journal JAMA.
Author block: Blayne Welk, Eric McArthur, Sarah A. Morrow, Penny MacDonald, Jade Hayward, Andrew Leung, Andrea Lum.
Study gives Ontario men access to advanced prostate cancer imaging
Prostate cancer can be elusive.
Wayne Smith’s journey with prostate cancer began 16 years ago when his family physician noticed increasing levels of prostate specific antigen (PSA) in his blood. PSA is a protein expressed by the prostate. A blood test is used to monitor levels of the protein as a screening tool for prostate cancer.
“My doctor referred me to Dr. Stephen Pautler, Urologist at St. Joseph’s Health Care London. Although we did a number of tests, we weren’t able to locate any spots of cancer,” says Wayne, a 71-year-old man from Ingersoll, Ontario. “We were able to manage my PSA levels for a number of years until they jumped up too high.”

Above: Wayne Smith
In 2012, Wayne was sent for a CT scan. This test finally revealed spots of cancer at the back of the prostate. “Dr. Pautler discussed my treatment options with me and I chose to have surgery to remove my prostate,” explains Wayne. “The team did a great job but we eventually realized some cancer remained. I asked about a PET scan to locate it but the technology was not available at that time.”
After consulting with Dr. Pautler and Dr. Glenn Bauman, Radiation Oncologist at London Health Sciences Centre, Wayne chose to postpone further treatment and monitor the cancer over time. It was undetectable for five years before his PSA levels started rising again. Earlier this year, the levels doubled.
“I was told a PET scan was available through research and that it could help locate the disease,” says Wayne. He went for the scan earlier this year at St. Joseph’s Hospital, part of St. Joseph’s Health Care London. “Nothing showed up on the scan, but that was good news; it meant the cancer was microscopically small.”
The PET scan helped Wayne and his care team in making decisions about his treatment. They decided on hormone therapy and radiation therapy to hopefully eradicate any cancerous cells. He was treated at London Health Sciences Centre’s (LHSC) London Regional Cancer Program.
“Early evidence suggests that a clear PET scan despite rising PSA levels is likely associated with persistent cancer at the original site,” explains Dr. Glenn Bauman, Lawson Scientist and Radiation Oncologist at LHSC. “Based on the scan, Wayne was able to do a much shorter round of hormone therapy – six months rather than being on hormone therapy indefinitely.”
“After the first hormone treatment, my PSA levels dropped significantly. With the added radiation, we’re confident this will be the end of my battle with prostate cancer,” says Wayne, who is currently enjoying retired life by spending time with his wife, two children and five grandkids. “Despite my diagnosis and treatments, I carried on with my life. I did what I had to do but still went places on weekends, did chores around the house and went golfing.”

Above: Dr. Glenn Bauman (left) and Wayne Smith (right)
Wayne is one of 1,500 Ontario men who will participate in the PSMA-PET Registry Trial. Led by researchers at Lawson Health Research Institute, the multi-centre registry trial is testing the use of a new imaging tracer, called a PSMA tracer, for early detection of recurrent prostate cancer. The registry gives patients access to a new type of imaging and will assess the impact on patient care.
PSMA tracers are used in positron emission tomography (PET) scans to target a protein found in prostate cancer cells called prostate specific membrane antigen (PSMA). Supported by Cancer Care Ontario and McMaster University’s Centre for Probe Development and Commercialization (CPDC), the goal of the registry trial is to capture detailed PET images to guide treatment decisions made by patients and their care teams.
Eligible participants are those with suspected prostate cancer that cannot be detected in conventional bone and CT scans. Participants have a PET scan using a specific PSMA tracer called 18F-DCFPyL. The tracer is injected and spreads out in the body to find spots of cancer which are then visible on the scan.
“With this trial, men in Ontario can access a promising test that could impact their treatment outcomes,” says Dr. Bauman. “The PSMA tracer may be able to locate prostate cancer that was once undiscoverable.”
Led by Dr. Bauman along with Drs. Ur Metser and Tony Finelli at University Health Network (UHN), the trial is currently available across multiple sites in Ontario: London Health Sciences Centre; St. Joseph’s Health Care London; St. Joseph’s Health Care Hamilton; Sunnybrook Health Sciences Centre; Princess Margaret Cancer Centre (UHN); and Thunder Bay Regional Health Sciences Centre. The trial is also expected to open at The Ottawa Hospital this year.
The PSMA tracer is considered an investigational agent in Canada and is currently only available through clinical trials. After studying the accuracy of the tracer in detecting early cancer recurrence, the research team hopes to have enough data to recommend when it could be used in the clinic.
Patients from London, Ontario and region who are enrolled in the PSMA-PET Registry Trial have their scans performed at St. Joseph's Hospital. In 2016, Lawson researchers were the first in Canada to use the 18F-DCFPyL PSMA tracer to capture PET images with a patient at St. Joseph’s Hospital. The tracer is provided by CanProbe, a joint venture between CPDC and UHN located in Toronto, and was set up with funding from the Movember Foundation.
“We conducted an initial trial that included 20 men with prostate cancer who were having their prostate removed. The goal was to determine how effective the PSMA probe was in detecting disease at the time of initial treatment,” explains Dr. Bauman. “We found the PET scan was able to detect spots of cancer in almost all participants, which corresponded to spots of cancer identified in the prostate after it was removed and examined under the microscope.”
The initial trial was made possible with donor funding through London Health Sciences Foundation, which provided initial funding to hire Research Associate, Catherine Hildebrand, who set up citywide cancer imaging workshops and helped the team prepare successful grant applications to secure key funding from CIHR and OICR.
Dr. Bauman notes that conventional imaging tests like bone scans and computed tomography (CT) are not always effective for detecting prostate cancer. While other PET probes can be used to detect a number of different cancer types, they are unable to identify prostate cancer. The PSMA probe opens new avenues for prostate cancer diagnosis, prognosis and treatment guidance.
For patients like Wayne Smith, access to this advanced imaging is critically important.
“It’s fantastic we have access to this PET scan. It certainly gave me relief knowing nothing showed up on the scan and that, even if something did, it would light up to show us where to treat,” says Wayne. “I know PET scans are used for other cancers too and I think they’re imperative. They give you more of a chance through knowledge of where the disease is located.”

Study may help explain why breast cancer often spreads to the lungs
A team from Lawson Health Research Institute has shown that triple-negative breast cancer cells can facilitate changes to the lung that both attract cancerous cells and allow them to grow, leading to lung metastasis.
Metastasis is the spread of cancer cells from a primary tumour to different organs. Lung metastasis is responsible for approximately 60 to 70 per cent of deaths related to breast cancer.
“The best way to explain lung metastasis is the seed and soil analogy,” says Dr. Alison Allan, Lawson Scientist. “The seeds are the breast cancer cells from a primary tumour and the soil is the lung’s microenvironment. Seeds can break away, but they only grow if the soil is fertile.”
The majority of studies on metastatic cancer have focused on the characteristics of tumour cells and not on the organs to which they spread. Dr. Allan’s team is studying how the lung microenvironment itself is contributing to lung metastasis.
In the new study, the team examined the lung microenvironment in preclinical models. They compared models with two different subtypes of breast cancer. The luminal A subtype is the least aggressive form of breast cancer and does not often metastasize to the lung. Triple-negative breast cancer, meanwhile, is the most aggressive form with a higher likelihood of metastasis and no targeted therapies available.
The team found that models with triple-negative breast cancer had a drastically different lung microenvironment that was much more hospitable to the growth of cancer. They also found that triple-negative breast cancer cells might be sending ‘signals’ to the lung to help it attract cancerous cells that enter the bloodstream.
“We suspect that triple-negative breast cancer cells release tiny particles called exosomes which are delivered to the lung,” explains Dr. Allan, who is also Chair of the Department of Anatomy and Cell Biology at Western University’s Schulich School of Medicine & Dentistry. “Once delivered, the exosomes signal the lung to start changing into a hospitable environment for tumour cells.”
With support from Lawson’s Internal Research Fund, the team is continuing to research this process. They are also studying ways to make the lungs less receptive to cancerous cells.
Their findings could help in the development of targeted therapies to prevent breast cancer from metastasizing. For example, in collaboration with investigators at the University of Alberta, they are developing an inhalable spray that is aimed at preventing cancer from spreading to and growing in healthy lungs.
“The ultimate goal is to eliminate the metastasis-promoting exosomes as a therapeutic strategy to prevent triple-negative breast cancer from spreading to the lungs,” says Dr. Allan.
The study “Triple-Negative Primary Breast Tumours Induce Supportive Premetastatic Changes in the Extracellular Matrix and Soluble Components of the Lung Microenvironment,” is published in Cancers. It was funded by the Cancer Research Society, the Canadian Cancer Society Research Institute, a London Regional Cancer Program Catalyst Grant, London Health Sciences Foundation, the Breast Cancer Society of Canada and an Ontario Graduate Scholarship awarded to Braeden Medeiros – the paper’s first author.
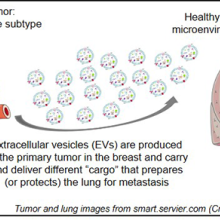
Above: Visual representation of the research findings
Study reveals clinical factors linked to reduced mortality in injection drug users with heart valve infection
Cases of endocarditis – infection of the heart valves – have risen dramatically in recent years as a result of the opioid crisis. In London, Ontario 55 per cent of people who experience heart valve infections are injection drug users. They are particularly vulnerable to the disease and a third die as a result.
In an effort to improve outcomes, researchers at Lawson Health Research Institute and Western University are studying which clinical factors are associated with improved survival in this patient population. In a new study, they showed that both surgery and in-hospital addictions counselling are linked to significantly reduced mortality in injection drug users with first-episode endocarditis. Surgery was associated with a 56 per cent reduction in mortality, while in-hospital addictions counselling was associated with a 72 per cent reduction.
The project was a retrospective cohort study that examined anonymous patient data from 2007 to 2016 at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. Of 370 patients with first-episode endocarditis, 202 were persons who inject drugs. Of those 202 patients, 39 had cardiac surgery at LHSC and 40 were referred for addictions counselling to start in while they were still in-hospital.
The study found that patients who received surgery experienced a 56 per cent reduction in mortality. Patients who received surgery were normally the most severely ill and most in need. While additional studies are necessary, the researchers point to these findings as a reason for cardiac surgery to be considered as a viable treatment option in carefully selected patients.
“In the past, many centres have not performed cardiac surgery in patients who inject drugs due to concerns about poor outcomes. Continued injection drug use was viewed as a risk for reinfection,” says Dr. Michael Silverman, author of the study, Lawson scientist and Chair/Chief of Infectious Diseases for Western’s Schulich School of Medicine & Dentistry, LHSC and St. Joseph’s. “Our study challenges those beliefs. It shows that when we account for the severity of a patient’s illness, they’re more likely to survive with surgery.”
Patients who were referred for addictions counselling while in-hospital experienced a 72 per cent reduction in mortality. Addictions counselling was provided by a consultant who would meet with patients to provide education on risks for infection, harm reduction strategies and support towards addictions recovery, including referral to community supports.
The study’s authors point out that, in other centres, patients are not commonly referred for addictions counselling while still being treated for an acute infection. It is commonly believed they are too ill to undergo this type of therapy. The more common approach is to treat the infection and refer patients for addictions counselling after discharge.
“Education and support for these patients is critical. The majority of the patients I see don’t understand what they’re doing to cause an infection and may be highly motivated to undertake a lifestyle change,” says Dr. Sharon Koivu, author of the study, Lawson scientist, associate professor at Schulich Medicine & Dentistry and palliative-care physician at LHSC. “This study shows the importance of working with patients towards harm reduction and addiction recovery while they’re still being treated in-hospital.”
London’s rates of endocarditis in persons who inject drugs are significantly higher than other regions. While injection drug users account for 55 per cent of all heart valve infections in London, they account for only 8 to 12 per cent in large studies in the United States. To address this issue, the research team is conducting a number of additional studies. Current projects are exploring the reasons behind such high local rates and the best strategies for treatment, including antibiotic and surgical interventions.
“We don’t often get a chance to look at large numbers of this particular patient population but there is a plethora of local data available,” says Dr. Laura Rodger, author of the study and a resident physician at Schulich Medicine & Dentistry and LHSC. “Our team wants to bring meaning to that data by asking the right questions to ultimately improve patient outcomes.”
The study, “Clinical Characteristics and Factors Associated with Mortality in First-Episode Infective Endocarditis Among Persons Who Inject Drugs,” is published in JAMA Network OPEN.
Study shows fewer higher-dose radiation treatments safe and well tolerated by women with uterine cancer
MEDIA RELEASE
FOR IMMEDIATE RELEASE
Sunnybrook Health Sciences Centre and Lawson Health Research Institute
April 14, 2022
LONDON,ON - Five high-dose radiation treatments targeting uterine cancer rather than the current standard 25 treatments are safe and well-tolerated by patients, a new study published in JAMA Oncology has found.
SPARTACUS (Stereotactic Pelvic Adjuvant Radiation Therapy in Cancers of the Uterus) — a multi-institutional non-randomized controlled trial — looked to assess the feasibility and safety of using a specialized technique called stereotactic body radiation therapy (SBRT) for women with uterine cancer where instead of 25 treatments over five weeks, five treatments can be delivered over 1.5 weeks.
SBRT uses many precise beams of radiation to target tumours or cancerous cells. It uses a higher dose of radiation in a smaller number of treatments. It can be done on a standard linear accelerator, the machine that delivers radiation treatments.
Sixty-one women were enrolled in SPARTACUS at two centres — Sunnybrook Health Sciences Centre and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC).
“Uterine cancer is a common cancer in women, usually treated with surgical removal followed by radiation and/or chemotherapy to reduce the risk of recurrence,” said Dr. Eric Leung, radiation oncologist at Sunnybrook’s Odette Cancer Centre. “External beam radiation is usually given over five weeks, and that can place a heavy burden on women who have to travel to a radiation centre every day, spend time away from home and work, and incur the financial burden of these factors as well.”
With a median follow-up of nine months, the patients enrolled in SPARTACUS reported an acceptable level of side effects from the radiation that resolved, and also reported a reasonable quality of life during treatment, Dr. Leung said.
“We were interested in examining the toxicity of the higher dose – would it affect the nearby bowels or bladder and place a heavy symptom burden on patients? We were pleased to find that patients reported their symptoms as manageable.”
“This study represents a novel way of treating uterine cancer in a shorter time. It was conducted mainly through the COVID pandemic and gave women a chance to receive treatment in less time with fewer visits to our centres,” said Dr. David D’Souza, radiation oncologist at LHSC and the study co-lead through Lawson Health Research Institute.
Patients will continue to be followed on the study for late side effects and further research is planned to further compare this more convenient schedule to the standard five-week course of radiation.
“This novel treatment could lead to a practice change that places less burden on patients and on the healthcare system,” Dr. Leung said. “Delivering radiation over the course of a week and half rather than over five weeks for patients facing uterine cancer would open up healthcare resources by reducing visits and usage of the linear accelerators.”
-30-
ADDIONAL QUOTES – Dr. David D’Souza:
“Giving radiation in a shorter time can have several advantages for both the patient and the health care system."
“Our study assessed the safety of delivering a higher dose of radiation in fewer treatments for patients with uterine cancer by adapting what has successfully been done for other types of cancer in the pelvis like prostate and rectal cancer.”
“This study was made possible with advances in treatment planning, radiation machine capabilities, and an outstanding radiation therapy program at LRCP.”
ABOUT LAWSON HEALTH RESEARCH INSTITUTE
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
ABOUT SUNNYBROOK HEALTH SCIENCES CENTRE
Sunnybrook Health Sciences Centre is inventing the future of health care for the 1.2 million patients the hospital cares for each year through the dedication of its more than 10,000 staff and volunteers. An internationally recognized leader in research and education and a full affiliation with the University of Toronto distinguishes Sunnybrook as one of Canada’s premier academic health sciences centres. Sunnybrook specializes in caring for high-risk pregnancies, critically-ill newborns and adults, offering specialized rehabilitation and treating and preventing cancer, cardiovascular disease, neurological and psychiatric disorders, orthopaedic and arthritic conditions and traumatic injuries. The Hospital also has a unique and national leading program for the care of Canada’s war veterans.
Media Contacts:
Celine Zadorsky
Communications & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. 75664
C: 519-619-3872
@email
Sunnybrook Health Sciences Centre
Communications & Stakeholder Relations
416-480-4040
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
SWAHN Presents: Choosing Wisely in Southwestern Ontario - A Knowledge Exchange Forum
Objectives of the day:
- To encourage knowledge exchange concerning the implementation of Choosing Wisely Canada projects – featuring special presentations by representatives from North York General Hospital and St. Michael’s Hospital in Toronto as well as local organizations in the SWAHN region;
- To foster networking and collaboration among participants to discuss how the information shared by forum presenters concerning best practices can be translated to organizations in the SWAHN region;
- To obtain recommendations for SWAHN’s next steps concerning its role in promoting and advancing Choosing Wisely initiatives in the region.
Registration Fee: $75.00 + HST = $84.75
(Students/Residents: $25 + HST = $28.25)
Deadline to Register: April 28, 2017.
Space is limited so register early!
To register please complete the information in the attached form and submit the information as indicated.
For more information contact Catherine Joyes, SWAHN Manager: @email.
The SouthWestern Academic Health Network (SWAHN) seeks to transform health in Southwestern Ontario through integrated excellence in research, education, and clinical practice. For more information please visit www.swahn.ca.
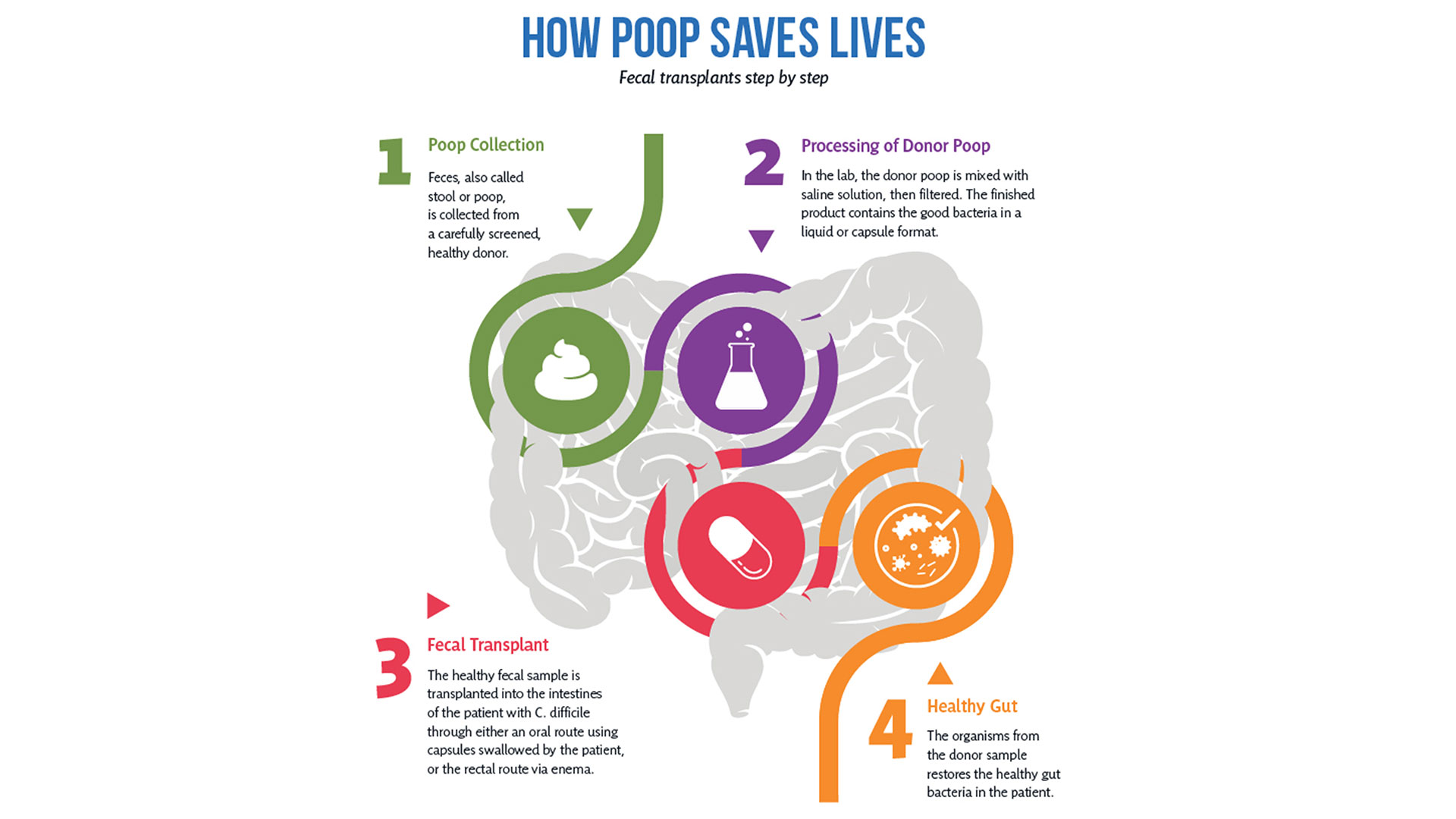
Team players: FMT and microbiome research could have widespread impact
There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson Health Research Institute, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system.
FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis.
FMT is already in clinical use for the treatment of C. diff (Clostridium difficile), and in addition to showing promise in the treatment of other diseases, it is also being studied as a way to improve response to existing cancer treatments and ease treatment side effects.
Dr. Saman Maleki, a Scientist at Lawson Health Research Institute and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC), says they’ve just begun to explore the possibilities.
"We are just starting to study FMT as an intervention outside its traditional use in patients with C. difficile infection, and we will be expanding to other areas, particularly in cancer.”
FMT can overhaul a patient’s microbiome, Dr. Maleki explains, and a healthy microbiome is beneficial especially when a treatment is trying to activate the body’s immune system.
Dr. Michael Silverman, Lawson Associate Scientist and Medical Director of St. Joseph’s Health Care London’s Infectious Diseases Care Program, is a pioneer in the field of FMT. He has been performing the procedure since 2003 with C. difficile patients and was one of the first in North America to do so. He sees a wide range of possible applications.
“FMT has enormous potential in being an important adjunctive therapy in many cancers. It may, for example, help cancer patients respond to immunotherapy,” says Dr. Silverman, who is also Chair/Chief of Infectious Disease at St. Joseph’s Health Care London, LHSC and Western University. “The potential to impact autoimmune and metabolic diseases is also quite exciting, but still in early development.”
So how does it work?
After rigorous screening, stool from a healthy donor is collected and then processed in a lab into a liquid or capsule containing the good bacteria, which can then be administered to a patient’s gastrointestinal tract.
The Lawson team is also one of few delivering FMT using specially-prepared oral capsules. Introduced in 2018, they have been a game changer in patient acceptance and ease of administration, according to Research Coordinator Dr. SeemaNair Parvathy, who has been coordinating the program since 2015.
“There is a link between the fitness of the intestinal microbiome and the fitness of the immune system,” says Dr. John Lenehan, Associate Scientist at Lawson and Medical Oncologist at LHSC. “A ‘healthy’ microbiome leads to a more robust immune response when using immunotherapy. FMT from a healthy donor is expected to improve the fitness of the recipient’s intestinal microbiome and promote a better immune response.”
People with chronic disease can often experience what’s called a ‘leaky gut,’ allowing food, bacterial and microbial components to pass through the intestinal wall, negatively impacting the immune system.
“When people get FMTs their intestinal permeability improves – meaning it actually reduces,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at Lawson and St. Joseph’s. “What changes that intestinal permeability? The microbes at the site. They play a role in interacting with the host cells, providing nutrients and vitamins.”
With the immune system so closely tied to the health of the microbiome, it’s not surprising scientists are exploring how strengthening one can have a big impact on the other.
Boosting immunotherapy
Immunotherapy can be used to either stimulate or suppress the immune system to help the body fight disease, and FMT is showing promise in reducing resistance to the treatment.
While immunotherapy has been effective in treating a number of cancers – the number one cause of death in Canada – not all patients respond to the treatment.
But early work presented at a conference by the Lawson team for the Journal for ImmunoTherapy of Cancer has shown that using FMT to modify the microbiome could reduce resistance to immunotherapy. The study involved patients from LHSC with advanced melanoma, a type of skin cancer.
While in the very early stages, the combination of FMT and anti-PD1 immunotherapy has been found to be safe, and it appears that FMT could make tumours more responsive to the immunotherapy treatment.
“Microbiome-based treatment strategies, including FMT, have a high potential in oncology,” says Dr. Maleki. “Our team is also exploring its potential in treating pancreatic cancer.”
The research is so interesting that a recent Nature article listed the Phase I melanoma trial as “seminal” research. The study was also unique in that it used healthy donors, as opposed to donors who had previously responded to immunotherapy treatment.
A separate Lawson study with LHSC patients with metastatic renal cell carcinoma, a type of kidney cancer, published in the Journal of Clinical Oncology, also looked at combining immunotherapy and FMT to ease the adverse effects of the treatment.
The Phase I study, led by Dr. Maleki and Dr. Ricardo Fernandes, Medical Oncologist at LHSC, found adding FMT to doublet immunotherapy was safe, but further study is needed to determine whether it could bring about changes in the microbiome and immune system.
Dr. Lenehan says Lawson researchers are in a position to be leaders in this field in the near future for two reasons.
“One is that other academic researchers have not been able to assemble the expertise, and some who have, do not have the access to healthy donor stool. The second is that some biotechnology companies are interested in FMT, but almost exclusively for C. difficile infections.”
Autoimmune, metabolic and other illnesses
Two other areas that have seen recent advances include FMT for the treatment of non-alcoholic fatty liver disease (NAFLD) and multiple sclerosis.
“The gut microbiome is very important in the metabolism of foods and metabolic products. It can therefore have a major effect on obesity and atherosclerosis,” says Dr. Silverman. “It also is tightly involved in regulating the immune system and therefore moderating the microbiome may potentially impact autoimmune diseases.”
A study published in 2020 by the team in The American Journal of Gastroenterology showed that FMT appears to reduce intestinal permeability in patients with NAFLD.
The number of people with NAFLD is growing rapidly and studies show patients have different microbiota than healthy persons.
The trial included 21 NAFLD patients from LHSC and St. Joseph’s. While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Metabolic syndromes including obesity and its complications of NAFLD and atherosclerosis are massive public health problems. Any impact on these would be of huge importance,” Dr. Silverman adds. “Autoimmune diseases also cause major morbidity and mortality. We have a lot of work to do before we can consider FMT as a routine therapy for any of these conditions, but the long-term promise is great.”
Research into the use of FMT for treatment of patients with multiple sclerosis is in the very early stages. But patients with MS show a difference in gut microbiota and higher small intestine permeability, which could contribute to the development of the disease.
A Phase I trial by the Lawson team published in the Multiple Sclerosis Journal – Experimental, Translational and Clinical, found FMT to be safe and tolerable.
While the study was very small, MS patients treated with FMT were found to have beneficial changes to gut microbiota and intestinal permeability, but further study is needed to determine if FMT could be used as a treatment.
Lawson scientists are also currently studying the use of FMT for patients with atherosclerosis, along with ongoing studies on melanoma and lung cancer. Funding for a study on pancreatic cancer has been secured and researchers are in the process of planning trials for a number of other applications.
Dr. Lenehan says, “The microbiome is connected to several diseases and their treatments. Evidence is growing that an individual’s health is related to their microbiome.”

The donor challenge
The challenge of finding fecal donors for FMT and the cost of that process remain an issue for research into this promising treatment, even as more potential applications are discovered.
There is currently no process in place to match donors and recipients – as with organ donation – but there is an extensive screening process for both infectious and non-infectious conditions, one that needs to be repeated if a donor experiences any lifestyle changes.
Dr. Burton says, “We still don't understand the full role of the microbiota. We have to ensure that we're not giving patients a microbiota that might cause them some other issue in the future, so the donors are screened very thoroughly for that.”
Screening also excludes donors with an increased risk of developing the diseases scientists are hoping to treat, such as metabolic syndrome related conditions.
A 2017 article published in Open Forum Infectious Diseases by Drs. Silverman and Burton found the cost of screening high numbers of potential donors could make establishing local programs extremely difficult, so having a central program such as the one in London could help patients in many regions.
In the study, only five of 46 potential donors passed the history, examination, blood, stool and urine tests, and of the five, four later travelled or had illnesses that made donation inadvisable.
The search continues in London for potential donors to help drive this research forward. You can read one donor’s story and learn how you can get involved here.
More on FMT and the microbiome:
Drugs vs. bugs: Harnessing the microbiome to improve treatments
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Two Lawson researchers each receive $400K CIHR grants to improve kidney care
Two researchers at Lawson Health Research Institute have each been awarded $400,000 as part of the Canadian Institute of Health Research’s (CIHR) new Health System Impact Embedded Early Career Researcher Awards.
The funding will see the researchers apply their skills to find and implement solutions to improve kidney care by focusing on challenges in the health-care system.
Dr. Kyla Naylor and Dr. Danielle Nash will each spend four years working with provincial organizations. Dr. Naylor will work with the Trillium Gift of Life Network -Ontario Health, which is the organization responsible for coordinating provincial organ and tissue donation and transplant services. Dr. Nash will work with the Ontario Renal Network - Ontario Health, which is the organization responsible for managing delivery of advanced kidney services in the province.

“The treatment options for kidney failure is either a kidney transplant or dialysis. The majority of Canadians who have kidney failure receive dialysis,” says Dr. Naylor, who is an Associate Scientist at Lawson and an Adjunct Scientist at ICES. “However, a kidney transplant compared to dialysis can improve a patients’ quality of life, can give on average 10 more years of survival, and when compared to dialysis, can save the health-care system millions of dollars.”
In her research program, Dr. Naylor will begin by developing a kidney transplant measurement framework that will enable continuous performance monitoring and increase equitable access to transplant.
“The first goal of this project will allow kidney transplant centres and regional renal programs to evaluate their performance and set goals towards improvement,” Dr. Naylor says. “The second is to improve kidney transplant education materials to provide patients with the information to make an informed decision about kidney transplant, and the third is to address geographical barriers to transplantation.”
Dr. Naylor will be using ICES data, which includes administrative health-care data for Ontario’s 14.5 million residents, with the goal of eventually making access to kidney transplantation more equitable for the thousands of Canadians living with kidney failure.
The goal of Dr. Nash’s research program is to use a learning health system model to better understand patient-identified gaps in kidney care across Ontario, and to develop solutions to fill these gaps in collaboration with the Ontario Renal Network and patient partners.
“Chronic kidney disease is a serious illness that can lead to kidney failure. The best way to prevent kidney failure is to detect chronic kidney disease early and provide optimal care during this time,” explains Dr. Nash, who is also an Epidemiologist and Scientist with London Health Science Centre’s (LHSC) Kidney Dialysis and Transplantation Program. “Since many patients do not have symptoms, it can go unnoticed for a long time. However, it can be detected using simple blood and urine tests.”
Province-wide data from ICES Ontario and the Ontario Renal Network will be used for the research data.
As part of both studies, the researchers will also be interviewing health-care providers and patients to assess additional barriers to treatment.
“One in four patients do not see a nephrologist in a timely manner and 60 per cent are not receiving adequate time in multidisciplinary kidney care clinics before initiating dialysis,” says Dr. Nash. “Education on treatment options (typically dialysis or a kidney transplant) needs to happen early for patients who are at high risk for kidney failure, so they can make an informed decision about treatment.”
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email