Search
Search
Contact Lawson Research Institute
Contact us
For general information or Lawson-specific questions:
Phone: 519 646-6005
Email: @email
To reach a member of the Lawson/St. Joseph’s Communications team with a story idea or a media-related inquiry, contact:
Communication and Public Affairs
Phone: 519 646-6100 ext. 66034
Fax: 519 646-6215
Email: comdept@sjhc.london.on.ca
If you need to contact a communicator after office hours (Mon to Fri, 8:30 am to 4:30 pm), call Switchboard at 519 646-6100 and ask them to page the communicator on-call.
Directions and parking
The main office of Lawson Research Institute is located within St. Joseph's Hospital. You can find a map to St. Joseph's Hospital along with Parking information below.
Lawson Research Institute inside St. Joseph's Hospital
268 Grosvenor Street
London, Ontario, N6A 4V2
Parking options
For those planning to park at or near St. Joseph’s Hospital, please ensure you leave extra time to do so. Due to the high number of people coming for care at St. Joseph’s Hospital, our two parking garages located on Grosvenor Street and on Cheapside Street are often at capacity Monday to Thursday between 9:30 a.m. and 2 p.m. ‘Lot full’ signs are posted when the parking garage(s) are full. Metered parking is available on the streets around the hospital.
As parking availability isn’t guaranteed at or nearby the hospital, St. Joseph’s encourages patients and family caregivers to consider making alternate travel arrangements when coming to the hospital, such as using public transit, taxi or being dropped off and picked up. Drop off areas are available at Entrance 1 and 2 on Grosvenor Street and Entrance 4 on Cheapside Street.
St. Joseph’s recognizes the frustration the lack of parking availability may cause and apologizes for any inconvenience. Thank you for your patience and understanding while we seek solutions to this issue.
Grosvenor parking garage
Daily rate: Minimum rate of $4 for the first hour and then $2 increments every half hour to a maximum of $8.75 after 2 hours.
Monthly rate: $60.75
There are 989 parking spaces in the Grosvenor Street parking garage.
View a printable map of parking spaces at St. Joseph's Hospital, Grosvenor Street Parking Garage (including accessible spaces).
The parking garage entrance is located on Grosvenor Street, across the street from Grosvenor Entrance 1. The garage is connected to Mount Hope Centre for Long Term Care through the underground tunnel (take elevators at northwest corner of the garage, see below).
Tunnel access at St. Joseph's Hospital
When visiting St. Joseph's Hospital and parking in the parking garage on Grosvenor Street the safest and most accessible route is through the tunnel. You can access the tunnel from the west end of the parking garage (closest to Richmond Street) by taking the elevators or stairs to level "B". When returning to your vehicle from Zone A you will need to push "T" (for tunnel) in the elevator.
Parking pay stations
Parking pay stations are located on the ground floor of both elevator lobbies located at the north-west and north-centre area of garage.
Pay stations only accept coins and credit cards. To purchase a monthly pass visit the Parking Garage office on the Wellington Street side of the Grosvenor Street Parking Garage, ground floor.
For further information, please call the parking office at 519 646-6100 ext. 65113.
Parking office hours are 8 am to 4 pm, Monday to Friday. Outside those hours, calls are directed to Precise ParkLink Inc. at 1-888-783 PARK (7275). The call centre can also be reached by intercom available on the parking pay machines in the garage's elevator lobby.
Accessible parking spaces
Accessible parking is available on each floor of the Grosvenor Street parking garage at the west end of the garage (closest to the Richmond and Grosvenor Street corner.) These parking spots are located close to the elevator that will take you to the wheelchair-accessible ramp on street level (level 1) or the underground tunnel that connects to both Mount Hope Centre for Long Term Care and St. Joseph’s Hospital.
Limited spots for accessible parking is also available on Wellington Street and on Grosvenor Street across from the Urgent Care Centre entrance (Entrance 2).
Cheapside parking garage
There are 132 parking spaces in the Cheapside Street parking garage.
View a printable map to parking spaces at St. Joseph's Hospital, Cheapside Street Parking Garage (including accessible spaces).
This is the closest lot for outpatients with appointments in Zones C and D of the hospital (Medical Imaging, Roth McFarlane Hand and Upper Limb Centre, Hand Therapy, Breast Care Centre, Rheumatology Centre, Physiotherapy Therapy, Occupational Therapy, WSIB Specialty Clinic, Shuttleworth Auditorium).
The entrance to the lot is on Cheapside Street just east of Richmond. It is open from 5:30 am to 5:30 pm, Monday to Friday, and closed on weekends. The elevator in the garage connects directly with the Francis and Madeleine Saul Medical Imaging Centre (Level 0) and the G. A. Huot Surgical Centre (Level 1). For appointments in Zone D, exit the parking garage elevator on Level 0 and walk across the lobby to the west side.
The parking pay station is located by the main elevators next to the gift shop in the Zone C lobby.
Parking meters at St. Joseph's Hospital
There are many city parking meters located within walking distance to St. Joseph's Hospital.
Rates are posted on the meters.
Street parking at St. Joseph's Hospital
Some of the residential streets that are within walking distance to the health centre offer one or two hour parking. Overnight parking is not permitted.
Please be courteous and do not block driveways.
Courteous parking to ensure maximum lot capacity
Please be aware that the City of London enforces parking regulations across all of St. Joseph’s sites to ensure patients, visitors, staff and physicians have adequate parking. All users of our parking facilities are asked to pay attention to parking regulations and how you park your vehicle.
As well, those who park for more than 10 minutes in patient drop-off designated areas, in handicapped parking without a permit, at loading docks, and other restricted areas will also find their vehicles being ticketed.
Thank you for respecting our parking regulations. If you have any parking questions please contact Precise ParkLink Inc.
Email: @email
Phone: 1-888-783 PARK (7275)
Public transit to St. Joseph's Hospital
St. Joseph's Hospital is conveniently located in a central location, with easy access to public transportation. Bus stops are located along Richmond Street and close to the Cheapside Street entrances. Contact the London Transit Commission at 519 451-1347 for rates and times.
The following London Transit bus routes will drop you off near entrances to St. Joseph's, see the London Transit trip planner and route schedules and real time LTC bus route tracking for more information:
- 6 Richmond
- 13 Wellington
- 1 Kipps Lane
- 21 Huron Heights
St. Joseph's is also just a few blocks north of Oxford Street, providing easy access from the Oxford St. bus routes.
Current Participants
Thank you for volunteering as a clinical research participant at HULC. You are helping to contribute to our growing knowledge and the advancement of clinical care. Please use these resources to assist in your role as a research participant.
Getting Here
The Roth | McFarlane Hand & Upper Limb Centre (HULC) is located at St. Joseph’s Hospital.
St. Joseph’s Hospital
Room D0-101
268 Grosvenor Street
London, Ontario N6A 4V2 519 646-6100 ext. 64640
Find turn-by-turn directions to HULC.
Contact Us
If you have any questions related to the research study you’re participating in, please contact the HULC clinical research team at 519-646-6100 ext. 64640.
Detecting the Undetectable
A simple fall can lead to long-term hand problems such as arthritis due to fracturing the scaphoid bone in the wrist. Scaphoid fractures are known to have the highest rate of healing failures. While this bone’s fragile blood supply is commonly thought to be the main reason for why it is difficult to heal, Dr. Ruby Grewal is looking into a different reason – infection.
Infections are known to cause difficulty in healing bones, but traditional tests for infections in the scaphoid have come up negative. With new advancements in detecting microbial DNA, scientists can now test for ‘clinically undetectable’ infections.

In a new study, Dr. Grewal will use microbial DNA test whether or not there are infections in the scaphoid fracture which causes improper healing of the bone.
“The goal of this study is to use advanced DNA sequencing technology to test whether or not we can detect evidence of microorganisms in non-healing scaphoids,” explains Dr. Grewal, Lawson Scientist and Orthopaedic Surgeon at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London.
Finding new causes of improper healing of the scaphoid bone could improve treatments for individuals with these injuries and prevent long-term problems with hand function. These insights into the causes of improper healing could also prevent young patients from developing wrist arthritis.
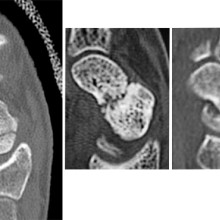
From left to right: Normal scaphoid fracture. Scaphoid fracture that is struggling to heal. Scaphoid non-union where the bone has failed to heal.
Dr. Grewal’s study is being funded through the Lawson Internal Research Fund (IRF).
“The financial support provided by Lawson’s IRF is of utmost importance to researchers. These funds will allow our team to embark on a new area of research and test a novel hypothesis,” says Dr. Grewal, “While traditional granting agencies are reluctant to fund completely novel areas of research without pilot data to prove feasibility, the Lawson IRF allows researchers to investigate new theories in a sound scientific manner. Without the ability to test new ideas we cannot innovate and make advancements in health care. Support for this project allows for that.”
Lawson’s IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Growing Tissues in the Lab
When challenged by surgeons to find better treatments for difficult-to-manage connective tissue diseases, Dr. David O’Gorman gladly accepted.
Dr. O’Gorman is a Molecular Biologist and Lawson Scientist based at St. Joseph’s Hospital, a part of St. Joseph’s Health Care London. His research focuses on understanding normal and abnormal connective tissue repair. He collaborates with researchers and clinicians working in many different disciplines, including those specializing in reconstructive surgery, orthopedics and urology.
Surgical reconstructions can be hampered by a lack of graft tissue, or graft tissue of insufficient quality, making it difficult to achieve optimal outcomes for the patients.
An example is a condition called urethral stricture disease (urethral scarring). This condition occurs in males and typically causes symptoms such as frequent and urgent urination, and slow urinary stream. In extreme cases, it can cause urinary tract infections, permanent bladder dysfunction and renal failure. Recurrence rates after minimally invasive treatments are high, and so many urologists recommend open surgical approaches.
Surgeons can use the patient’s own tissues to reconstruct the urethra after stricture removal. This tissue is normally sourced from the buccal cavity in the mouth but taking large tissue grafts can result in complications. In cases where buccal grafts have been used for previous reconstructions, there may not be enough intact tissue left.
Dr. O’Gorman sees a solution in growing sheets of human buccal tissues in the lab.
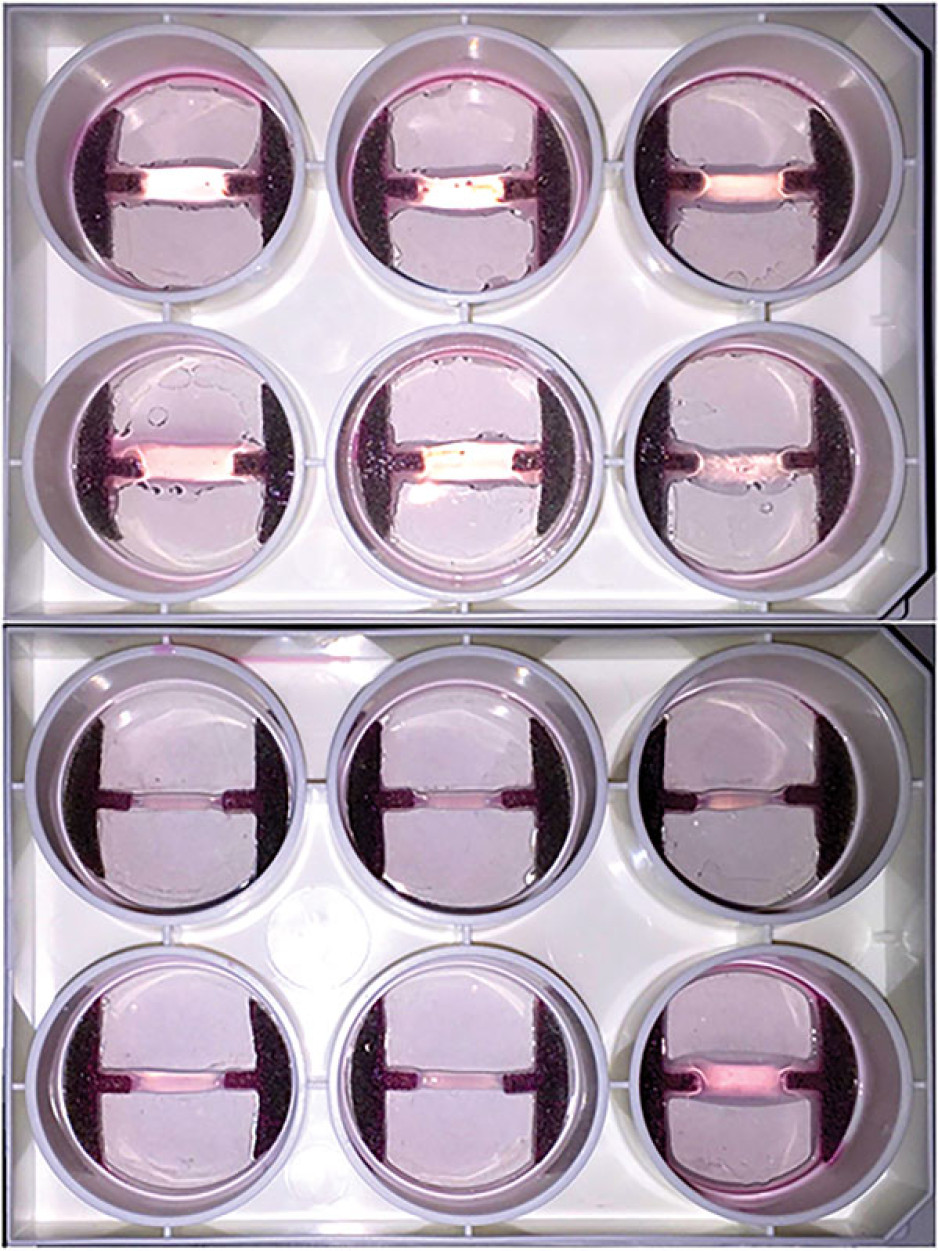
“We are currently using buccal graft trimmings as a source of cells, culturing them in a 3D environment and expanding them to create tissues of suitable size, density and elasticity.”
The patient’s own cells are used to generate a tissue graft for urethral reconstruction. While several research groups have developed this approach in the past, few have attempted to translate their models for clinical use.
“Our immediate goal is to provide proof of principle – that we can consistently generate grafts of suitable size and functional characteristics,” explains Dr. O’Gorman, “In the future, we could be providing bioengineered graft tissues for reconstructive surgeries here in London.”
Bioengineered human tissues can also be used as ‘mimetics’ – replications of human tissues – to study diseases, especially those difficult to model using routine laboratory methods.
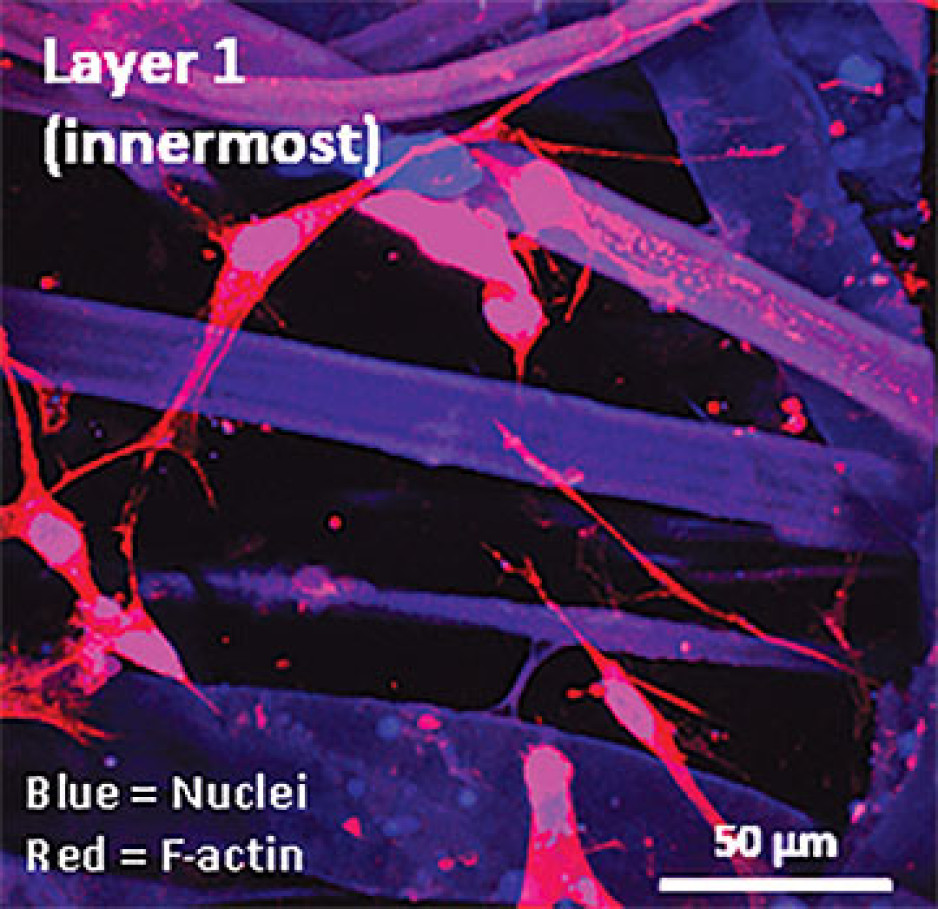
Instead of a using a growth media or sterile plastic dishes, 3D cell culture is achieved by embedding cells in a matrix of proteins and other molecules normally found in those tissues. In this environment, gene expression and growth is more similar to cells of connective tissues in the body being replicated.
Dupuytren’s disease (or Dupuytren’s Contracture) affects the palmar fascia in the hand, a connective tissue beneath the skin that extends from the base of the palm into the fingers. This disease can be understood as a type of excessive scarring, where normal tissue repair processes have gone awry and dense scar tissue forms, typically causing permanent palm or finger flexion that restricts hand function.
This condition is surprisingly common and may affect more than one million people in Canada. While there are surgical treatment options available, none consistently prevent this disease from recurring in at least a third of patients.
“Due to its high recurrence rate after treatment, Dupuytren’s disease is currently considered incurable. Our challenge is to understand it well enough to develop truly effective treatments,” says Dr. O’Gorman.
Human hands have unique characteristics not found in other species, making animal models impractical. Instead, Dr. O’Gorman’s team extracts cells from the diseased palmar fascia of patients undergoing hand surgeries and bioengineers them into palmar fascia ‘contractures’ in the lab.
“Since the cells from a single palmar fascia sample can be used to grow dozens of little contractures, we can test many different treatments simultaneously to see what works best for each patient.”
This approach may also allow them to determine if Dupuytren’s disease is truly one disease, or a group of similar diseases that cause palm and finger contractures.
“Often, Dupuytren’s disease is clearly heritable, but some individuals have no family history of it and develop apparently sporadic disease,” notes Dr. O’Gorman. “We want to determine if these are truly the same disease at the molecular level.”
Another major cause of abnormal connective tissue repair is infection, and tissue mimetics can play a role here, too. While rare, infections of artificial joint replacements are particularly devastating for patients, as they typically require readmission to hospital to remove the infected joint, weeks of antibiotic-based treatment, and an additional surgery to replace the artificial joint.
In addition to the associated pain and suffering, these procedures are technically challenging and costly to our health care system.
Artificial shoulder joint infections are most frequently caused by the microorganism Cutibacterium acnes (C. acnes). C. acnes infections disrupt normal tissue repair processes after surgery, cause shoulder tissues to die and promote loosening of the artificial joint. These infections are difficult to diagnose, and there is a lack of reproducible
models in which to study them. Dr O’Gorman’s team has set out to create the first human Shoulder-Joint Implant Mimetic (S-JIM) of C. acnes infection.
“While S-JIMs are more complex, they are 3D in vitro cell culture systems designed to mimic human tissues, like those that we use for studying Dupuytren’s disease.”
S-JIMs include layers of artificial human tissue, wrapped around cores of titanium alloy or cobalt chrome, the metals used to create artificial joints. They are co-cultured with C. acnes under low oxygen conditions similar to those that normally occur around artificial shoulder joints.
“We are bioengineering simple 3D cell cultures to more closely mimic the complexity of human tissues, with blood supply, nerves and interactions with other cells.” – Dr. David O’Gorman
Studying the connective tissue layers close to the infection allows researchers to investigate processes that promote infection, such as the formation of a biofilm that harbours and protects the bacteria from the body’s immune system. They are also able to test whether novel treatments can disrupt biofilm formation and increase the effectiveness of antibiotics.
Dr. O’Gorman predicts that in the future, medical researchers will routinely use bioengineered 3D human tissue and organ mimetics to accelerate our understanding of disease.
“The technology is in its infancy, but the potential for using bioengineered human tissues for surgical reconstructions or as disease models is huge. At Lawson, we’re ready to take on health care challenges and build on innovative approaches to improve the quality of life for patients.”
ONLINE EXCLUSIVE: What is 3D cell culture?
Medical researchers have grown human cells in culture media on or in sterile plastic dishes, such as Petri dishes, for more than 50 years.
Some cells, such as blood cells, can survive and grow in suspension, while others like smooth muscle cells need¬ to adhere to a surface to survive and grow. These are often called “2D cell cultures” because the cells grow horizontally across the bottom of the dish.
Some cells derived from connective tissues, such as fibroblasts, are not only adherent, but also very sensitive to the stiffness of their environment (“biomechanically sensitive” cells). Plastic dishes are at least 10,000 times stiffer than most connective tissues, and when biomechanically sensitive cells detect stiff surfaces, they can change the expression of their genes and behave abnormally.
The most common proteins in these tissues - and in the entire human body - are collagens, and one routine 3D cell culture approach is to embed fibroblasts in a collagen gel (gelatin). Fibroblasts in this environment can grow in any direction they choose, and their gene expression is more similar to cells in connective tissues.
These simple 3D cell cultures represent tissue engineering in its most basic form.
“Our challenge is to bioengineer simple 3D cell cultures in the lab to more closely mimic the complexity of human tissues, which have blood supply, nerves and interactions with other cells and tissues that modify their function and ability to heal after injury,” explains Dr. O’Gorman.
Dr. David O’Gorman is a Lawson Scientist and Co-director, Cell and Molecular Biology Laboratory at The Roth | McFarlane Hand and Upper Limb Centre in London, Ontario. He is also an Assistant Professor at Western University.
Improving surgery for wrist arthritis
Wrist arthritis can cause debilitating pain, weakness and decreased range of motion. When patients are first diagnosed, the condition can often be managed with activity modification and pain medication. However, as symptoms progress, patients eventually require surgery.
Surgeons typically perform a procedure called four-corner fusion to preserve wrist motion and provide pain relief. This surgery involves removing one of the carpal bones and fusing four of the remaining carpal bones. Although this procedure is one of the most common treatments for wrist arthritis, it is not known how the position of the fusion of the wrist bones affects range of motion and joint contact.
Lawson associate scientist Dr. Nina Suh is leading a study with the goal of improving the surgical technique for four-corner fusion to maximize wrist function and symptom relief, and delay wrist arthritis progression.
Dr. Suh and her team will use a customized active-motion wrist simulator to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
“We hope this research will lead to new surgical techniques that will help us to more effectively manage wrist arthritis with four-corner fusion,” says Dr. Suh, who is also an orthopaedic surgeon at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London and an assistant professor at Western University’s Schulich School of Medicine & Dentistry. “The project will also advance our understanding of wrist biomechanics, providing a foundation for the development of enhanced patient-specific surgical tools, such as custom wrist fusion devices and implants.”
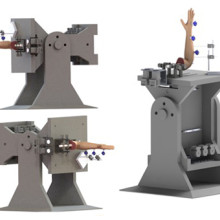
Image of the customized active-motion wrist simulator Dr. Nina Suh and her team are using to create different carpal bone fusion positions. They will then assess how these positions affect wrist motion and joint contact area.
The study is being funded through the Lawson Internal Research Fund (IRF), designed to allow scientists the opportunity to obtain start-up funds for new projects with exciting potential.
“The IRF program is valuable for scientists as external funding sources routinely require preliminary data to strengthen applications,” says Dr. Suh. “Particularly for new scientists such as myself, these grants provide seed funding that allows us to demonstrate the validity of our methodology and the clinical usefulness of our results.”
The IRF is designed to provide Lawson scientists the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph’s Health Care Foundation).
Lawson researchers win American Shoulder and Elbow Surgeons’ Neer Award
The American Shoulder and Elbow Surgeons association has awarded a team of London researchers the 2017 Charles S. Neer Award for Clinical Science, one of the most prestigious awards in the areas of shoulder and elbow surgical research in North America.
The award recognizes the scientists’ development of the PCR-RFLP (polymerase chain reaction restriction fragment length polymorphism) assay, a test that can accurately identify Propionibacterium acnes (P acnes) infection of the shoulder within 24 hours. Current methods take an average of six or more days, and are prone to sample contamination and false-positive results.
“We are incredibly honoured to receive this award,” says Dr. David O’Gorman, Lawson scientist, Co-Director of Molecular and Cellular Research at the Roth McFarlane Hand and Upper Limb Centre (HULC) at St. Joseph’s Health Care London, and senior author of the publication. “We believe it illustrates the high quality of research being done at Lawson and marks the beginning of another clinically relevant research program at HULC.”
P acnes is a type of bacteria typically found deep in the hair follicles and sebaceous pores of the skin. A P acnes infection of the shoulder is a common and serious complication that occurs after arthroplasty (surgery to replace a damaged joint, most commonly with artificial material). It can cause pain in the shoulder joint and often loosens the implant. In most cases, the patient requires additional surgery to remove the infection and replace the implant.
It can be difficult to diagnose a P acnes infection as it often presents without symptoms that would be characteristic of an infection, such as pain, skin reddening or wound drainage. The prevalence of P acnes in the deeper layers of the skin also increases the chance of sample contamination and false-positive results making it hard to isolate and identify in a pathology lab.
Currently P acnes infection is identified by administering a tissue swab for anaerobic culture, which takes an average of six or more days but could take up to three weeks. This technique also carries substantial risk of contamination from the adjacent skin and other sites where P acnes is present.
The PCR-RFLP assay can identify P acnes in tissue from a shoulder biopsy within a 24-hour period. The extremely sensitive technology also has the ability to detect fewer than ten P acnes cells in the sample, which may decrease the false-positive rate in cultures caused by swab contamination.
“The accuracy of this test and the shorter period of time needed for identification can help with treatment decision making, targeted antibiotic therapy, and monitoring to minimize implant failure and revision surgery,” explains Dr. O’Gorman, who is also an Assistant Professor in the Departments of Surgery and Biochemistry at Western University’s Schulich School of Medicine & Dentistry. “We hope that the test can be further developed into a ‘point of case’ assay that can detect P acnes in tissue samples in real time while the patient is undergoing shoulder surgery.”
Since the PCR and RFLP mapping used for the assay are techniques routinely performed in many clinical microbiology and pathology labs, the test would be a cost-efficient approach not restricted to highly specialized research labs.
Other scientists who were part of the study include Dr. George Athwal and Dr. Kenneth Faber, HULC orthopaedic surgeons, Lawson scientists and Schulich professors; Ana Pena Diaz, research technician for the HULC Molecular and Cellular Biology Research Lab; and Scott Holmes, a medical student and Schulich Research Opportunities Program participant who was primarily responsible for designing and optimizing the assay.
Both Dr. O’Gorman and Dr. Faber are also members of Western’s Bone and Joint Institute.
“A rapid method for detecting Propionibacterium acnes in surgical biopsy specimens from the shoulder” was published in the Journal of Shoulder and Elbow Surgery (JSES).