Search
Search
Mobility and Activity
Researchers at Lawson are propelled by the people who will benefit from the best in complex rehabilitative science.
One in 10 Canadians has a mobility disability – and we’re laser-focused on discovering how to help people whose lives have been upended by spinal cord injuries, stroke, brain injuries, chronic pain, accidents, falls, trauma or degenerative disease.
Situated at the Gray Centre for Mobility and Activity within St. Joseph’s Health Care London’s Parkwood Institute, the region’s largest provider of rehabilitation and recovery health, we bring our research into practice using all the resources a health institute and teaching hospital can offer together.
We share our innovations with the world – and we share the world’s research too, as we’ve created and curated the biggest database of international research on stroke, traumatic brain injury and spinal cord injuries.
Lawson mobility researchers comprise one of the largest and most accomplished teams in the country: including a research chair, established world-class scientists, emerging researchers, dozens of trainees and more than 100 students.
Our work helps people around the world lead active and healthy lives. Read on to discover where it will lead you.
Lawson leads mobility and activity research:
Mobilizing hospital-based research in the battle against COVID-19
The COVID-19 pandemic is proving to be one of the most pressing health challenges of our time. With a rising number of cases and deaths worldwide, there’s a global urgency to finding a solution.
As the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, Lawson Health Research Institute excels in rapid response research and is uniquely positioned to tackle this problem from within hospital walls.
Our researchers belong to a health system at the forefront of the pandemic. With close proximity to patients and access to samples, they are mobilizing to address COVID-19.
“Lawson researchers include clinicians directly involved in the treatment of COVID-19 patients, as well as laboratory-based scientists and those with other expertise related to the pandemic response,” says Dr. David Hill, Scientific Director at Lawson and Integrated Vice President at LHSC and St. Joseph’s. “They are eager to contribute a solution and are combining their knowledge to address this issue from all angles.”
Already, Lawson research teams are initiating projects ranging from pre-clinical studies to clinical trials. They are planning to explore diagnosis, prevention and treatment of the disease, as well as long-term and mental health impacts. An immediate goal is to partner with other research hospitals to improve outcomes for COVID-19 patients around the world.
There are numerous COVID-19 studies underway at Lawson and many more going through the necessary approval processes. Recognizing the importance of a rapid response to this pandemic, Lawson’s Administration team is working to fast-track approval of the studies.
Lawson also offered a special internal COVID-19 funding competition to assist our researchers in their efforts. Lawson’s COVID-19 Pandemic Response Internal Research Fund supports projects that are identified as having the potential to impact the management of this pandemic and those that enhance our understanding of the pathophysiology of COVID-19. See the results of this competition and the 14 funded projects, for a total of more than $202,000 invested.
While there is much to learn about COVID-19 and its impact on human health and our health care system, Lawson researchers are tackling the disease head-on.
How can you support COVID-19 research and clinical care?
Research at Lawson can be supported through three hospital foundations. With an outpouring of support from our community, the foundations are collecting donations to support our hospitals through this challenging time. Learn more about donating:
- St. Joseph’s Health Care Foundation – St. Joseph’s Health Crisis Fund
- London Health Sciences Foundation - COVID-19 Response Fund
- Children’s Health Foundation - COVID-19 Response Fund
Learn more about COVID-19 research at Lawson:
National award honours innovator Frank Prato’s excellence in medical physics
Dr. Frank Prato is a man of many firsts:
First in Canada to conduct magnetic resonance brain imaging. A pioneer in magnetic resonance cardiac imaging. Driving force behind the installation of Canada’s first PET/MR scanner. Founder of the Canadian Organization of Medical Physicists (COMP) while president of the Canadian College of Medical Physicists.
And while Dr. Prato admits to a competitive streak that constantly propels him to break new ground in medical physics, the renowned, prolific researcher is keen to note these innovations have been part of a larger team effort.
“My career has been filled with opportunities to work with and train some spectacular scientists who have made major contributions across Canada and around the world,” he says. “I’m proud of the whole group that has developed over the years and the support St. Joseph’s has provided.”
Chief Medical Physicist at St. Joseph’s Health Care London (St. Joseph’s), Dr. Prato has been awarded the 2024 COMP Gold Medal, the organization’s highest award for outstanding career achievement.
“Dr. Prato’s ground-breaking work in the field of medical physics has not only advanced the scientific community but also significantly impacted patient care in Canada and beyond,” says COMP President Boyd McCurdy, “His pursuit of innovation and excellence exemplifies the highest standards of our profession, and we celebrate his outstanding contributions to medical physics with admiration and gratitude.”

Dr. Prato is also Assistant Scientific Director and Imaging Program Leader at Lawson Health Research Institute (Lawson) and professor of medical imaging and medical biophysics at Western University.
“I have worked with Frank for 36 years now and have come to recognize him as one of the finest people I know,” says Dr. Ting-Yim Lee, Director of PET/CT Research at Lawson, medical physicist at St. Joseph’s Hospital, and one of the nominators of Dr. Prato for the award.
“Frank is unfailingly helpful and authentic, a great listener and a tenacious problem-solver. He demonstrates excellence and professionalism in medical physics locally, nationally and internationally.”
Dr. Lee cites Dr. Prato’s leadership in being “at the forefront of numerous international innovations in nuclear medicine and diagnostic radiology.”
Throughout his 48 years as a medical physicist, Dr. Prato has been inspired by the potential of technology’s reach into human health.
“I’ve always wanted to work in an area where we can do research, with a vision of what’s going to be important in patient health. I get excited about being on the leading edge of discovery that’s embedded in patient care.”
Critical advancements in nuclear medicine and diagnostic radiology, thanks to the work of Dr. Prato and his St. Joseph’s/Lawson team, have included:
- Introducing the first bone mineral density imaging procedure on a patient in Canada, a tool now essential for managing osteoporosis.
- Performing the first magnetic resonance brain imaging in Canada, setting a national standard.
- Pioneering magnetic resonance cardiac imaging techniques, enhancing the understanding of myocardial scarring and blood flow assessment.
- Introducing the first PET/CT and PET/MR scanners in Canada, revolutionizing molecular imaging and proving the economic value of advanced imaging technologies.
- Imaging the brains of premature infants, a world first.
- Developing Canada’s first self-sustaining cyclotron infrastructure.
- Conducting the world’s first MRI-compatible, high-resolution brain PET scan.
- Early diagnosis and treatment of dementia, mental illness and prostate cancer.
Dr. Prato’s leadership extends beyond his technical achievements. As the founder of COMP, an organization that now includes more than 800 professionals, he played a crucial role in establishing the organization, advocating for medical physicists' independent voice and professional growth.
His tenure as President and board member of the Canadian College of Physicists in Medicine (CCPM) was marked by significant advancements, including enhancing certification processes and establishing reciprocity with the American Board of Medical Physics. Dr. Prato also received the Valuable Service Award from CCPM in 2002 and was named a Fellow of COMP in 2013.
Earlier this spring, Dr. Prato received a Dean’s Award of Excellence for Research Faculty from Western University’s Schulich School of Medicine & Dentistry. He is also the sole Canadian to have won the d'Arsonval Award, an international honour from the Bioelectromagnetics Society.
A dedicated mentor, Dr. Prato has guided more than 60 Masters of Science students, PhD students and Post-Doctoral Fellows, many of whom have won awards and secured prominent positions in the field. His mentorship has been instrumental in the success of numerous scientists within the Imaging Program at Lawson, contributing to a legacy of innovation for years to come.
“At 78 years old,” he says, “I am pleased to say I have achieved things at St. Joseph’s that will far outlast me.”
National research collaboration leads to Health Canada approval of life-saving radioisotope production
A Canadian consortium, which includes Lawson Health Research Institute (Lawson), TRIUMF, BC Cancer and Centre for Probe Development and Commercialization, is the first in the world to receive regulatory approval to produce the world’s most commonly used medical isotope, technetium-99m (Tc-99m), using small particle accelerators known as cyclotrons.
Tc-99m is used in tens of millions of nuclear medicine procedures globally each year. These include cancer scans, cardiac tests, as well as several other diagnostic procedures. As the world moves away from uranium-based nuclear reactors, there has been growing concern in the medical community of a global shortage of these life-saving compounds. This development helps secure a domestic supply of Tc-99m for Canadian patients.
For over a decade, Dr. Michael Kovacs, Director, Lawson Cyclotron & PET Radiochemistry Facility, and Steven Foster, Business Manager, Lawson Imaging, have been working on research that has contributed significantly to this major development. They have demonstrated the successful production of Tc-99m on a standard hospital-based cyclotron at Lawson, confirming that this technology can be used by almost half of the world’s already installed cyclotrons. Clinical trials were conducted across Canada and locally at St. Joseph’s Health Care London.
“In 2011, we received federal funding to see if we could develop a technology to produce Tc-99m in hospital cyclotrons,” explains Dr. Kovacs. “Canada’s Chalk River nuclear reactor was one of the world’s largest suppliers, and it was set to close in 2016. Cyclotron facilities offer a greener, safer, more sustainable approach for producing critical medical isotopes. Our goal was to find an alternative to the traditional means of producing this isotope, and we have been successful.”
Nuclear medicine is a functional imaging technique, meaning that it images biological function. Medical isotopes are converted to radiopharmaceuticals which get injected into the patient during a procedure. According to the specific biological properties of the isotope, they move throughout the body, rendering a 3D map of where the isotope has gone. This gives researchers and medical professionals valuable information of how various physiological processes are performing.
“Canada is a global leader in nuclear imaging technology. With the help of our collaborators across the country, we have home-grown technology to produce commercial quantities of Tc-99m on common cyclotrons,” adds Mr. Foster. “This technology has been patented and licensed to ARTMS Inc., a spin-off from the consortium, and is now being commercialized and sold throughout the world.”
The process was approved by Health Canada in November, 2020, and is expected to be deployed in British Columbia by 2022.
Nature's healing power
Using virtual technology, St. Joseph’s Health Care London is bringing the outdoors in for forensic mental health care patients.
Imagine sitting on a white sandy beach in a tropical location. The sun warms your face and a gentle breeze ripples across the water when, out of the corner of your eye, you spot a sea turtle slowly and curiously approaching.
You turn your gaze towards this beautiful creature and watch in wonder. You’ve never seen a sea turtle up close like this before.
For some, this type of experience is part of a dream vacation, attainable with enough money or imagination. But for many patients at St. Joseph’s Health Care London’s Southwest Centre for Forensic Mental Health Care (Southwest Centre) – including those not yet well enough to leave the facility – a new virtual-reality connection to nature offers a missing link in their journey towards recovery.
Immersive experiences in nature have been linked to positive mental health outcomes and a healthier sense of self – a benefit that staff researchers at Southwest Centre call eco-spirituality.
Occupational therapists Jared Scott, Clark Heard, and spiritual care practitioner Stephen Yeo, have explored just what this means for patients. Through a novel study published in 2022, Southwest Centre patients were provided with opportunities to become immersed in nature in the community, with tremendous therapeutic results.
The patients experienced a stronger connection with nature, a chance for open reflection and relaxation, and a restorative experience that provided a sense of peace and personal significance.
"There's something very human about connecting with, or in, nature ... It offers a sense of connectedness, whether to creativity, to beauty or the transcendent." spiritual care practitioner Stephen Yeo
The research team wondered if these experiences could be replicated in a virtual reality (VR) environment for patients who aren’t yet able to leave the facility.
“We realized we can translate these types of experiences through VR goggles where the patient has the ability to make their choices on how to engage,” says Heard. “This enables someone to experience something that's a little harder to touch in real life.”
For example, if the patient wishes to sit and reflect on a beach, they can. If they wish to be immersed in the jungle and experience giraffes and elephants walking among them, the choice is theirs.
“There’s something very human about connecting with, or in, nature,” adds Yeo. “True, virtual reality is not the same as the real thing, but we believe it offers a sense of connectedness, whether to creativity, to beauty or the transcendent. We see how it enlivens patients, even in sometimes very simple, subtle ways.”
Heard believes that this type of immersive experience nurtures the innate intellectual curiosity present in everyone.
“The first time people try it and look over their shoulder, they realize it's a full 360-degree experience. They look above and there are birds flying over them the same as anywhere else,” he explains.
Ultimately, Heard and Yeo believe the power and innovative experience of eco-VR is encouraging discovery in patients, energizing them at an intellectual and spiritual level.
With the purchase of VR equipment made possible through community support from donors to St. Joseph’s Health Care Foundation, the team has embarked on an eco-VR study, looking at what patients experience via VR and how that participation impacts their care journey. They are exploring with patients whether VR immersion in nature helps them cope with being in hospital at a difficult time in their lives.
Far beyond forensic mental health care, the answer just may open the door to a world out of reach for many others receiving care in various settings.
Psychiatry at Southwest Centre for Forensic Mental Health Care
St. Joseph’s Health Care London’s Southwest Centre for Forensic Mental Health Care (Southwest Centre), located in Elgin County, is devoted to caring for people with a mental illness who have also come into contact with the criminal justice system.
Encompassing a recovery philosophy of care, the state-of-the-art building provides a healing environment that promotes each individual’s journey of recovery.
The Forensic Psychiatry Program at Southwest Centre includes assessment, treatment and rehabilitation programs, and an outpatient Forensic Outreach Team that serves Southwestern Ontario. Through intensive work with their care teams, patients develop new skills needed to successfully reintegrate back into their communities.
New Alzheimer’s research aims to improve treatment and support for patients with agitation
Two new interventional studies have been brought to London, focused on improving quality of life for patients with Alzheimer’s disease and their caregivers. Both hope to improve upon standard approaches to treating agitation, a core symptom of Alzheimer’s.
Agitation is a significant source of stress for patients and caregivers. It is complex and difficult to treat. Often, families do not know about this particular symptom of Alzheimer’s and are not properly trained on how to manage care while dealing with agitation.
“These studies are designed to have a direct impact on patients, families and care providers, to improve quality of life and function in those suffering from agitation due to Alzheimer’s,” says Dr. Amer Burhan, Associate Scientist at Lawson Health Research Institute (Lawson) and Geriatric Neuropsychiatrist, St. Joseph’s Health Care London (St. Joseph’s).
Parkwood Institute, a part of St. Joseph’s, is one of multiple sites participating in these studies across Canada and the United States.
One study aims to identify patients early in their diagnosis, while they are living at home or in the community, and apply a comprehensive psychosocial approach, with or without medication, to help with the management of agitation. “We hope to identify participants and have them participating in our program before they experience a crisis due to agitation,” explains Dr. Burhan.
Psychosocial intervention is a way of helping patients and caregivers understand the reasons for agitation. Agitation can develop due to a wide range of causes. For example, patients may just be bored and need help to find something meaningful to occupy their time, they could be upset about something in their current environment, or may be suffering from physical discomfort or pain.
Interventions can include communicating with patients in a manner that creates calm, scheduling meaningful activities, and maintaining routine and rhythm in life. The research team will connect with families early after diagnosis to give them the tools and support they need.
Initially, participants will be treated using structured psychosocial intervention to help reduce and manage their agitation. After three weeks, they will be reassessed and if significant agitation continues to persist, the patient will be randomly selected to receive either a placebo, or medication known as S-Citalopram to treat agitation while they continue to receive psychosocial care.
Sylvia Wilson is the wife of one of the study participants. By enrolling in this trial, she feels she has gained a much better understanding of her husband’s disease, and is grateful for the support that study participants receive.
“My husband typically does not like going to visit doctors, but Dr. Burhan and his team are great,” says Wilson. “They understand agitation, and other symptoms of the disease very well, and I notice a difference in his mood with the treatment he receives through the study.”
Participants are still able to receive care from their primary physician and care teams, with the study providing an added layer of support.
Another study is focused on Alzheimer’s patients who are admitted to hospital or living in long-term care. The aim is to standardize the approach to care for agitation related to Alzheimer’s. After baseline assessment, participants will be randomized to receive the current treatment as per usual, or an integrated care pathway derived from evidence-informed treatment guidelines. These include washing out medications that have not helped, adding individualized behavioral and environmental support, and if medications are needed, use a specific set of medications and dosages based on best evidence.
“Better understanding agitation is a growing area of interest in geriatric research. The work being done locally is part of an international effort to create a paradigm shift in treating patients with Alzheimer’s disease and agitation,” explains Dr. Burhan.
Researchers are ready to offer these studies to patients and their families, hoping to make these treatment protocols an integral part of care for patients with agitation due to Alzheimer’s disease. Those interested in learning more about these studies can contact Dr. Burhan at @email or call 519-646-6100 x. 48170.
In the media: Study on 'agitation' in Alzheimer's patients seeks participants
New clinical protocol after general surgery cuts opioid prescribing in half
In recent years deaths from opioid overdoses have become one of the most common injury-related deaths in North America. The continent also has the highest per capita rate of opioid prescription in the world.
Recognizing the role that opioid prescribing plays in the national opioid crisis, a team of researchers at Lawson Health Research Institute and Western University have developed a new clinical protocol called STOP Narcotics. A study demonstrating the efficacy of their protocol was presented at the American College of Surgeons Clinical Congress in Boston, Massachusetts on October 24.
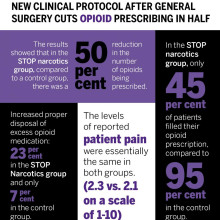
The protocol includes a combination of patient and health care provider education and an emphasis on non-opioid pain control. The study found that they were able to reduce the overall amount of opioids being prescribed after general surgery by 50 per cent while still adequately treating a patient’s post-operative pain.
“By significantly reducing the amount of opioids prescribed, this decreases the exposure risk and potential for misuse of narcotic medication,” said Dr. Luke Hartford, a resident in general surgery at Western’s Schulich School of Medicine & Dentistry and first author on the study. “This also decreases excess medication available to be diverted to individuals for whom it was not intended.”
The study involved 416 patients at London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London who underwent laparoscopic cholecystectomy or open hernia repair. They received medication for post-operative pain through the standardized protocol, specifically acetaminophen (Tylenol) and a non-steroidal anti-inflammatory drug (Naproxen) for the first 72 hours post-surgery.
The protocol instructs physicians to write a limited prescription of ten pills of opioids (Tramadol), with an expiry date of seven days after surgery, with instructions for the patient to fill this prescription only if adequate pain control was not otherwise achieved. There are also instructions on proper disposal of unused medication for the patient.
Dr. Ken Leslie, scientist at Lawson, associate professor in the Department of Surgery at Schulich Medicine & Dentistry, and Chair/Chief of the Division of General Surgery at London Health Sciences Centre led the implementation of the new protocol.
“We recognized that before STOP Narcotics, every surgeon had a different approach to pain control, and that most surgeons were prescribing more narcotics than are actually needed,” said Dr. Leslie. “When we looked at the data from this new protocol, we saw that the patient’s pain-control was just as good with this pathway, without a huge prescription for narcotics.”
The results showed that in the STOP narcotics group, compared to a control group, there was a 50 per cent reduction in the number of opioids being prescribed. They also demonstrated that only 45 per cent of patients actually filled their opioid prescription, compared to 95 per cent in the control group, and they were also able to increase appropriate disposal of excess opioid medication from 7 per cent in the control group to 23 per cent in the STOP Narcotics group. The levels of reported post-operative pain were the same in both groups.
The group now hopes to expand the protocol for applications beyond general surgery.
“If we can decrease the opioid exposure risk in our patients, and decrease the amount of excess medication available for diversion, and spread this to other institutions and surgical procedures and specialties, this has the potential to significantly impact the opioid crisis,” said Dr. Patrick Murphy, a resident in general surgery at Schulich Medicine & Dentistry and co-author on the study.
The study, “The Standardization of Outpatient Procedure (STOP) Narcotics: A Prospective Noninferiority Study to Reduce Opioid Use in Outpatient General Surgical Procedures,” is published in the Journal of the American College of Surgeons.
| Dr. Ken Leslie | Dr. Luke Hartford | Dr. Patrick Murphy |
Image

|
Image

|
Image
|

