Search
Search
Revealing the culprit behind Parkinson’s disease
An estimated 55,000 Canadians are living with Parkinson’s disease. While researchers are advancing therapies to treat symptoms, such as tremors, there is currently no method to stop progression.
To begin addressing this problem, a team of scientists at Lawson Health Research Institute is developing an imaging tracer.
“There’s a protein in the brain called alpha-synuclein (α-syn) that scientists believe is a culprit in causing Parkinson’s disease. The protein forms in ‘clumps’ called Lewy bodies that kill brain cells and potentially lead to disease,” explains Dr. Justin Hicks, Lawson Imaging Scientist. “Unfortunately, we have no way to study it in human brains and this has limited our ability to test therapies against it.”
Efforts have been made to study the elusive protein through modern imaging techniques like positron-emitting tomography (PET). Scientists have attempted to develop a PET probe – a radioactive molecule that targets the specific protein in order to produce highly specific images or scans – but they have been unsuccessful.

Above: Dr. Justin Hicks working in the Nordal Cyclotron & PET Radiochemistry Facility
“Unfortunately, the Lewy bodies caused by α-syn are hard to distinguish from protein clumps found in Alzheimer’s disease and other dementias. This makes it very difficult to know whether a PET probe has found clumps associated with Parkinson’s disease.”
Through a new study, Dr. Hicks and his team are working to find a solution. To do so, they will examine a different but related protein.
“There’s another protein called fatty acid binding protein 3 (FABP3) and one of its roles is to ‘chaperone’ the α-syn protein in human cells. Past studies have shown that levels FABP3 are higher in patients with Parkinson’s disease when compared to healthy controls,” explains Dr. Hicks. “This suggests that high concentrations of FABP3 can be used as an alternate measure of α-syn.”
They hope to measure levels of the FABP3 protein in place of the α-syn protein, and gain a better understanding of the role that both proteins play in the development and progression of Parkinson’s disease. To image Lewy bodies associated with Parkinson’s disease, the researchers are working to produce a PET probe that targets FABP3.
To accomplish this, they will be working in their lab to find a chemical that targets FABP3. Once found, they will attach a radioactive isotope to the chemical and produce a finished tracer. The tracer will then be tested in preclinical models.
Once injected, the PET probe will find and stick to FABP3. The PET isotope will emit a small amount of radioactivity and these emissions will show up as PET images.
“The ultimate goal is to develop a PET probe that can be used to distinguish Parkinson’s disease from other neurodegenerative diseases. The probe could also be used to assess new therapies that reduce levels of the α-syn protein,” says Dr. Hicks. “If successful, we hope this research will lead to a better understanding of the progression of Parkinson’s disease and ways to prevent it.”
Dr. Hicks and his team are being funded for this project through Lawson’s Internal Research Fund (IRF) competition. “Lawson’s IRF is extremely important for early career researchers. It allows us to generate data and publications to then apply for larger external funding. It also permits an added level of risk to pursue projects that may not reach their end goal but often spur new lines of research.”
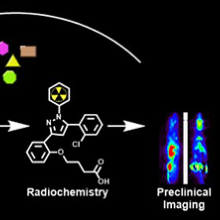
Above: A graphic depiction of this research project and its goals.
Revealing the secrets of dementia
The immune system is one of our greatest defenses against disease and injury. But what happens when it betrays us?
With conditions like rheumatoid arthritis the immune system is manipulated to attack the human body. Inflammation, normally a protective immune response, can be employed to cause symptoms like pain.
Surprisingly, research suggests our immune system may be similarly affected in patients with neurodegenerative dementias.
“We know there are increased numbers of inflammatory cells in the brains of patients with dementia but we don’t know what role they’re playing,” says Dr. Elizabeth Finger, a scientist at Lawson Health Research Institute and neurologist at St. Joseph’s Health Care London’s Parkwood Institute. “Are they doing their proper job of cleaning up damaged cells or is their presence more sinister?”
Dr. Finger’s research group aims to identify and understand changes in the brain that lead to symptoms of dementia, find novel treatments to improve patient quality of life and hopefully prevent the disease altogether. Critical to this work is Dr. Finger’s collaboration with Lawson Imaging scientists Drs. Keith St. Lawrence, Udunna Anazodo, and Justin Hicks.
The researchers utilize Canada’s first hybrid positron emission tomography and magnetic resonance imaging (PET/MRI) machine located at St. Joseph’s Hospital. This high-powered imaging allows them to assess changes to both structure and function in the brains of patients with neurodegenerative dementias like Alzheimer’s disease, frontotemporal dementia and Lewy body dementia.
In one of their many studies they are examining whether there is inflammation in the brains of patients with frontotemporal dementia and, if so, whether this inflammation is present in areas of the brain not yet damaged by the disease.
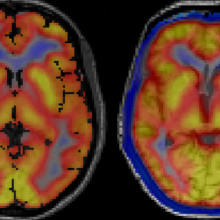
Images captured using a hybrid PET/MRI machine show activated immune cells in the frontal brain regions in a patient with frontotemporal dementia (right) compared to a healthy volunteer (left).
“A presence in those parts of the brain would suggest that inflammation is not playing its normal role of cleaning up damaged cells,” explains Dr. Finger. “It would suggest the brain’s immune response is overactive and that we should consider clinical trials for medications that modulate this response.”
Dr. Finger is an active investigator for novel therapies. In 2019, her group will participate in at least two clinical trials for medications that target genetic mutations that can cause frontotemporal dementia. The studies are phase I trials, which means they are the first time the medications are being tested in humans.
Dr. Finger is also leading a North American multi-centre trial called FOXY. The study will examine the therapeutic potential of a hormone called oxytocin to improve the loss of emotion and empathy that frequently occurs in patients with frontotemporal dementia.
“In the past there were very few treatments for frontotemporal dementia,” explains Dr. Finger. “We are glad to say that Lawson and St. Joseph’s will offer the opportunity to take part in these advances. Words cannot adequately express the appreciation we have for our patients, caregivers and healthy volunteers who participate in research. The time and effort they selflessly donate with the goal of helping future patients is truly inspiring and motivating.”
This story originally appeared in an annual publication from the Alzheimer Society London and Middlesex.
Revolutionizing rehab
St. Joseph’s Health Care London is taking giant strides in the science of rehabilitation and movement, with direct benefit to patients.
St. Joseph’s is setting a long-time vision into motion.
“Five years ago, we had a vision of leveraging our long history and expertise in providing innovative rehabilitation treatments to improve the lives of people with mobility needs on a larger scale,” says Roy Butler, President and CEO of St. Joseph’s Health Care London (St. Joseph’s). “That dream has come to life.”
While experts at St. Joseph’s had the knowledge, innovative spirit and passion to achieve the vision, they needed a partner who shared the same enthusiasm.
William and Lynn Gray answered that call. With their generosity and ground-breaking investment, The Gray Centre for Mobility and Activity was created.
“Lynne and I are very pleased with the steady forward advancement of the centre’s mission since its establishment just a few short years ago,” says Bill Gray. “The innovative thinking and idea generation that seeks new solutions to the issue of mobility have really taken root. We hoped that The Gray Centre would have an impact on care ... and it has.”
“We’ve watched the development of The Gray Centre with enormous pride and are pleased to have our name associated with it, and the excellence it stands for,” adds Lynne Gray.
A unique concept
Established in 2020, The Gray Centre at St. Joseph’s Parkwood Institute is a regional hub focused on researching leading-edge treatments and interventions in mobility and activity. The centre’s unique model of linking research and care allows researchers to work side-by-side with clinicians, patients, and caregivers to uncover optimal methods for maintaining mobility throughout a person’s life.
“Scientists at The Gray Centre are leading the way in integrating technology and solutions in care to better understand how we can enhance each patient’s treatment plan to improve their functionality and ability to move,” says Butler.
Pioneering Research
More than 50 ongoing rehabilitation research projects at Parkwood Institute are exploring areas such as spinal cord and traumatic brain injury rehabilitation, pain, outcomes for amputees, virtual exercise and cognitive behavioral therapy, gait analysis as a measure of dementia progression, and stroke rehabilitation and recovery.
The Gray Centre is a catalyst and connector for these projects by investing in cutting-edge technology, providing seed grants, embedding researchers from Western University, leveraging clinical expertise, attracting world-class researchers and translating new knowledge into clinical practice by training students and clinicians, and fostering sustainable practice change.
More than $1.3 million granted through St. Joseph’s Health Care Foundation has advanced work at The Gray Centre over the past year. From researcher support to new equipment such as two transcranial magnetic stimulators, a portable handheld ultrasound and several sensored mats for gait assessment donors have stepped up to advance this work.
Leadership with Purpose
At the helm of The Gray Centre is Siobhan Schabrun, PhD, a world-renowned neuroscientist and the inaugural William and Lynne Gray Research Chair in Mobility and Activity. Thanks to a partnership with Western University’s Faculty of Health Sciences and Schulich School of Medicine & Dentistry, donor funding for the chair made through St. Joseph’s Health Care Foundation was matched, creating a $5-million endowed position.
Schabrun’s innovative research benefits people suffering from chronic pain. With a focus on non-invasive brain stimulation techniques to enhance neuroplasticity and improve mobility and activity outcomes, she and her team are, in essence, retraining the brain’s pain response. This innovative work bridges the gap between neuroscience and rehabilitation, offering new hope for individuals with musculoskeletal and neurological conditions.
Originally trained as a physiotherapist with a PhD in neuroscience from the University of Adelaide in Australia, Schabrun has attracted more than $15 million in competitive research funding and written or contributed to more than 140 scholarly publications.
FLOATing Forwards
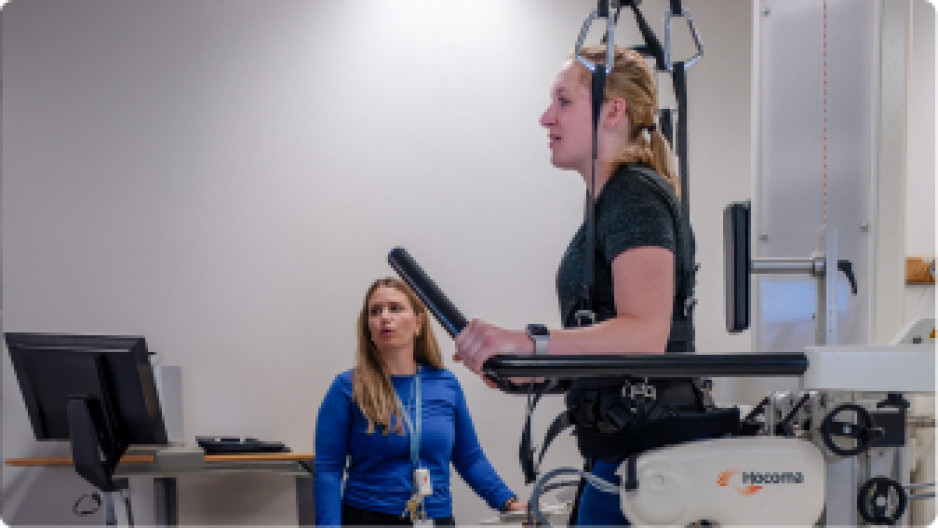
The newest advancement is a first-in-Canada and a marvel of medical engineering that is transforming options in rehabilitation research and practice.
The Reha-Stim Medtec FLOAT system at St. Joseph’s Parkwood Institute enables patients with mobility limitations to walk, supported, without fear of falling. They "float" in a controlled environment using a combination of robotics, body-weight support and real-time feedback. The device has a harness attached to a robotic arm, which adjusts the level of support based on the patient's movements. Sensors provide continuous feedback for maximum learning and greatest benefit to physical therapists and patients alike. The FLOAT system has shown significant improvements in patients' mobility, balance and overall functional independence.
“Innovative equipment like the new FLOAT System is an example of the type of innovation that does not exist anywhere else in Canada,” says Bill Gray. “The real-life application of technologies like this are what The Gray Centre is intended to be about.”
Through the combined efforts of dedicated professionals, cutting-edge technology and philanthropist partners, St. Joseph’s Gray Centre has combined vision with passion and is transforming lives, one step at a time.
Run for Retina Research
This event is supporting retina research.
Half marathon, 10K, 5K and 2.5K course routes that use London’s scenic park system and fitness trails in support of the Ivey Eye Institute.
When: Sunday, April 7, 2019
Where: Springbank Gardens
For more information, please visit St. Joseph's Health Care Foundation.