Search
Search
Top 12 research stories of 2022
As the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, our teams impact the lives of people in Ontario, Canada and around the globe with groundbreaking studies, world firsts and translational research that enhances care, health and wellbeing. Here are some of Lawson Health Research Institute’s top research highlights of 2022.
Researchers looking to better personalize treatment for PTSD

In a new study through Lawson and Western University’s Schulich School of Medicine & Dentistry, scientists are looking at a form of treatment called deep brain reorienting (DBR) for those suffering from post-traumatic stress disorder (PTSD). Read more.
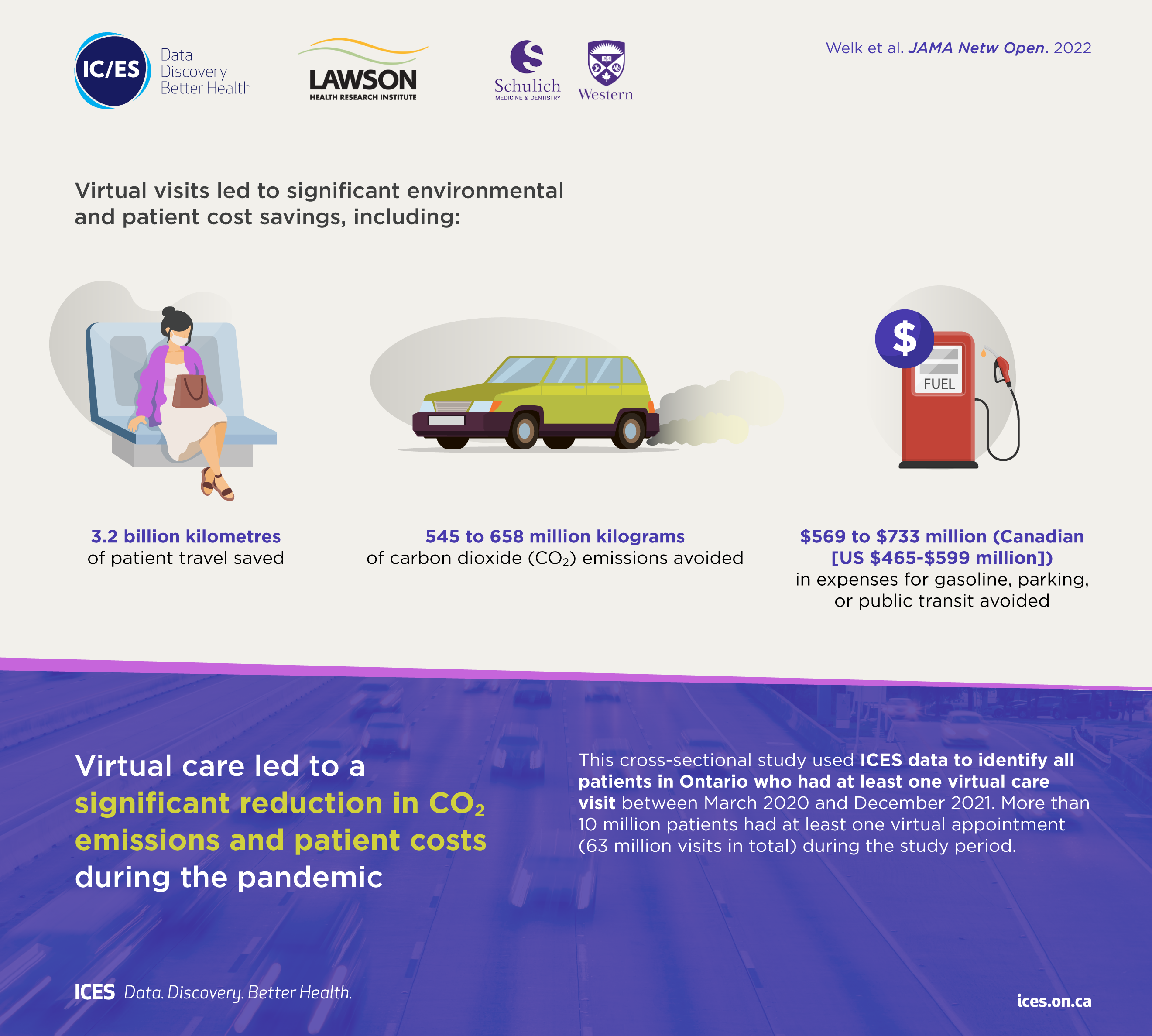
Virtual care associated with significant environmental and patient cost savings

A new study by researchers at ICES, Lawson and Western finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs. Read more.
Novel test that could easily diagnose blast injury created by local scientists

In a world first, researchers at Lawson and Defence Research and Development Canada have developed a breath test that could be used to diagnose repetitive blast injury – a mild traumatic brain injury resulting from pressure changes that occur during explosions. The device will soon go through clinical trials to validate its efficacy. Read more.
Local researchers using artificial intelligence to lead the way in bedside lung imaging
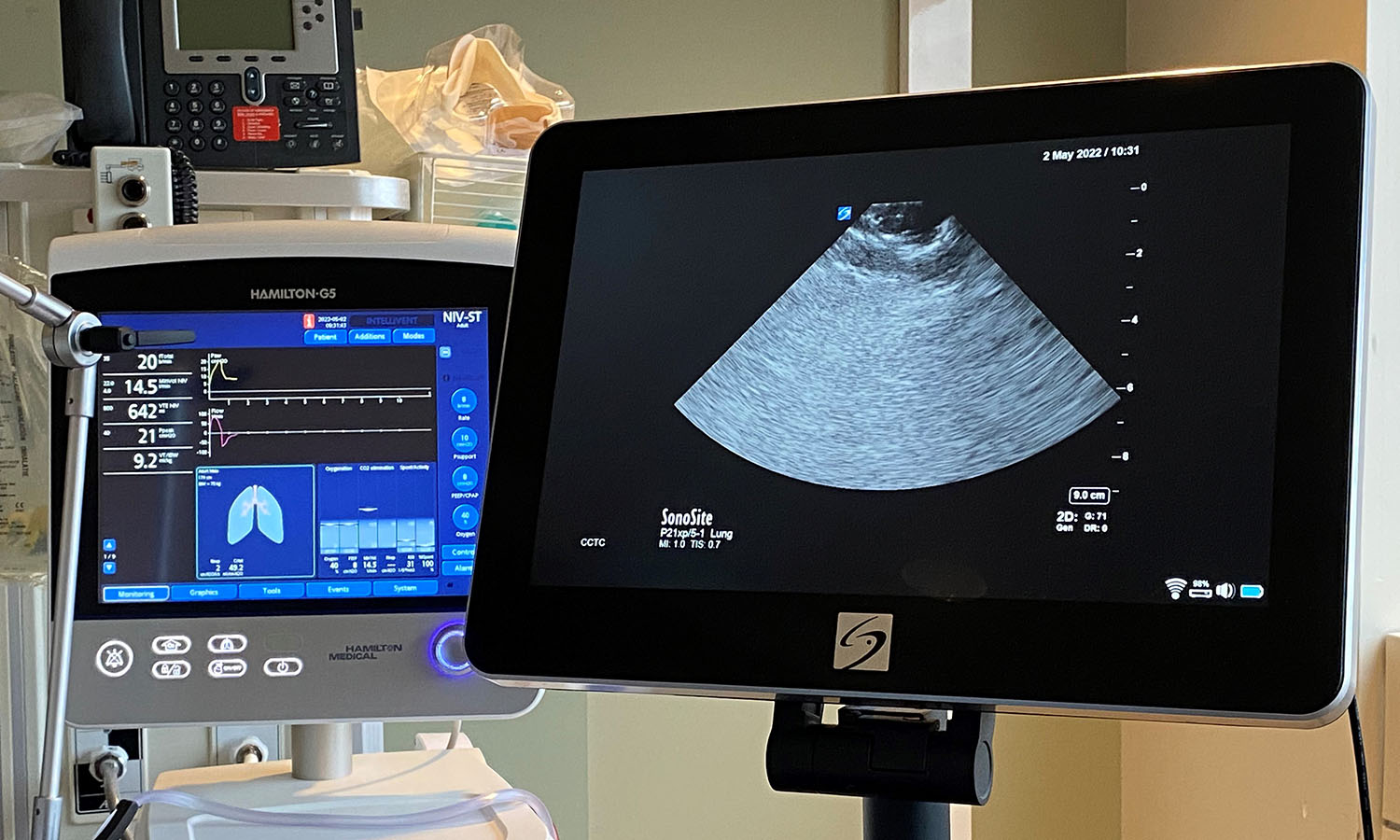
A team at Lawson is testing a new form of artificial intelligence (AI), paired with portable ultrasound machines, to image and identify lung concerns in real time, right at the beside of critically ill patients. Approximately 100 critical care patients at LHSC will be part of this study. Read more.
New tool shows promise in helping people manage traumatic brain injuries one pace at a time

A team at Lawson has developed a new app called MyBrainPacer™ which aims to better assist and treat those living with mild traumatic brain injuries (mTBI), including concussions. mTBI may come with lasting effects that can alter a person’s life. Although a person with a mTBI may appear fine on the outside, many have to pace their day-to-day activities in order to allow the time needed for the brain to properly heal. Much like point tracking used by dieters to monitor food choices, through MyBrainPacer™ App, users can assign values to tasks like driving, grocery shopping, screen use and exercise so they can plan and pace their daily activity. Read more.
Study shows a decline in Veterans' mental health throughout the pandemic

When it comes to mental health conditions, Veterans are an at-risk population, often having higher rates of depression and post-traumatic stress disorder (PTSD). When the COVID-19 pandemic hit, scientists at Lawson wanted to understand its effects on this already at-risk population. They found that more than half of Canadian Veterans reported a decline in their mental health. Read more.
Growing evidence that PSMA imaging improves prostate cancer detection
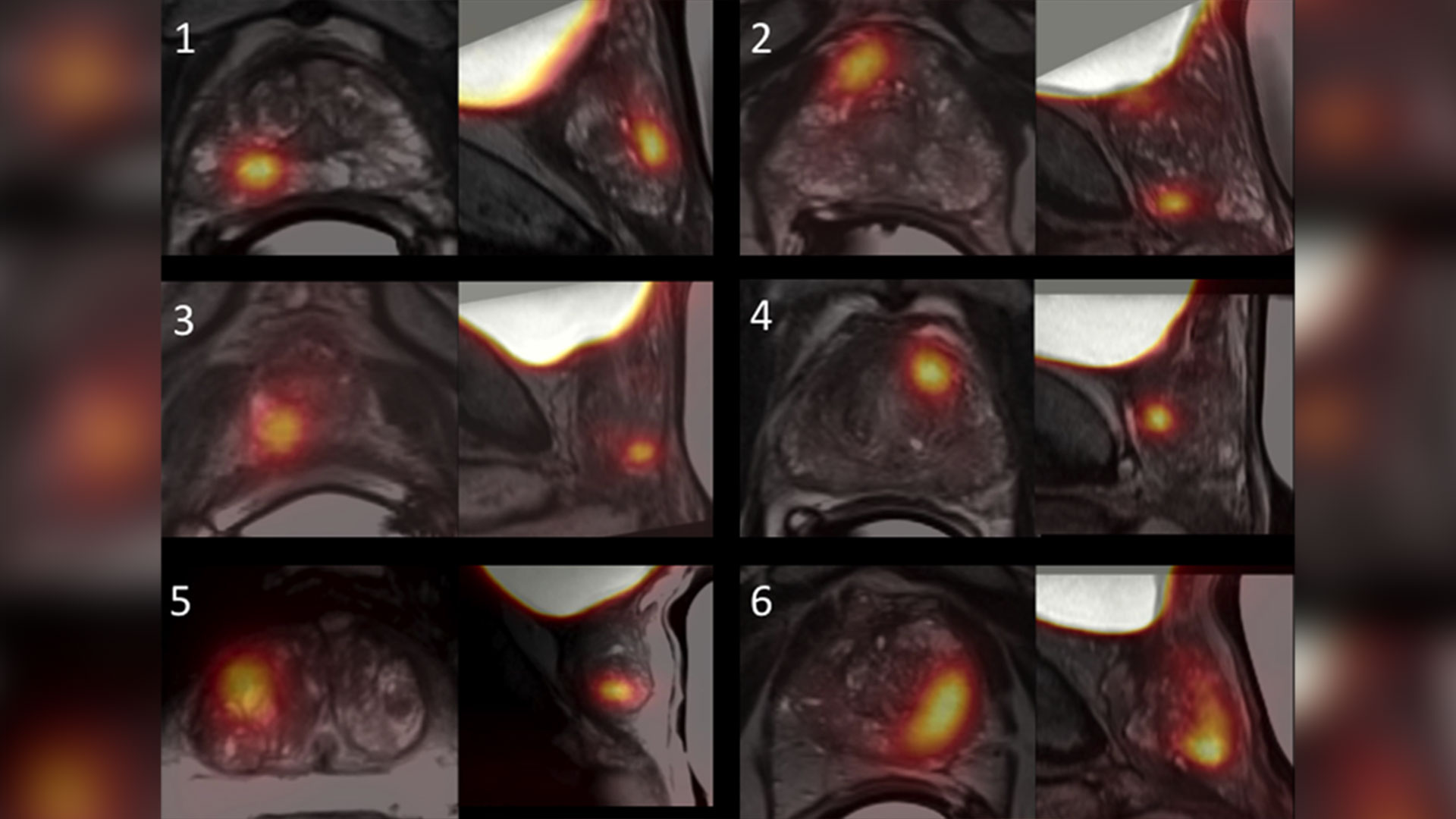
Scientists at Lawson are leading the way in using specialized imaging to detect prostate cancer – the fifth leading cause of cancer death in men around the world. Early evidence indicates that PSMA PET scans have changed how prostate cancer is being treated, but more work is underway to understand the impact of those treatment changes. Read more.
Leveraging virtual reality to manage pain in paediatric patients

A study underway through Lawson and Children’s Hospital at LHSC is using virtual reality (VR) to help paediatric patients during painful and distressing procedures. The study is focusing on paediatric patients who need port access. A port is a little reservoir that sits underneath the skin that allows access to blood or medication with the use of a needle. Ports are most commonly used in paediatric cancer patients. Read more.
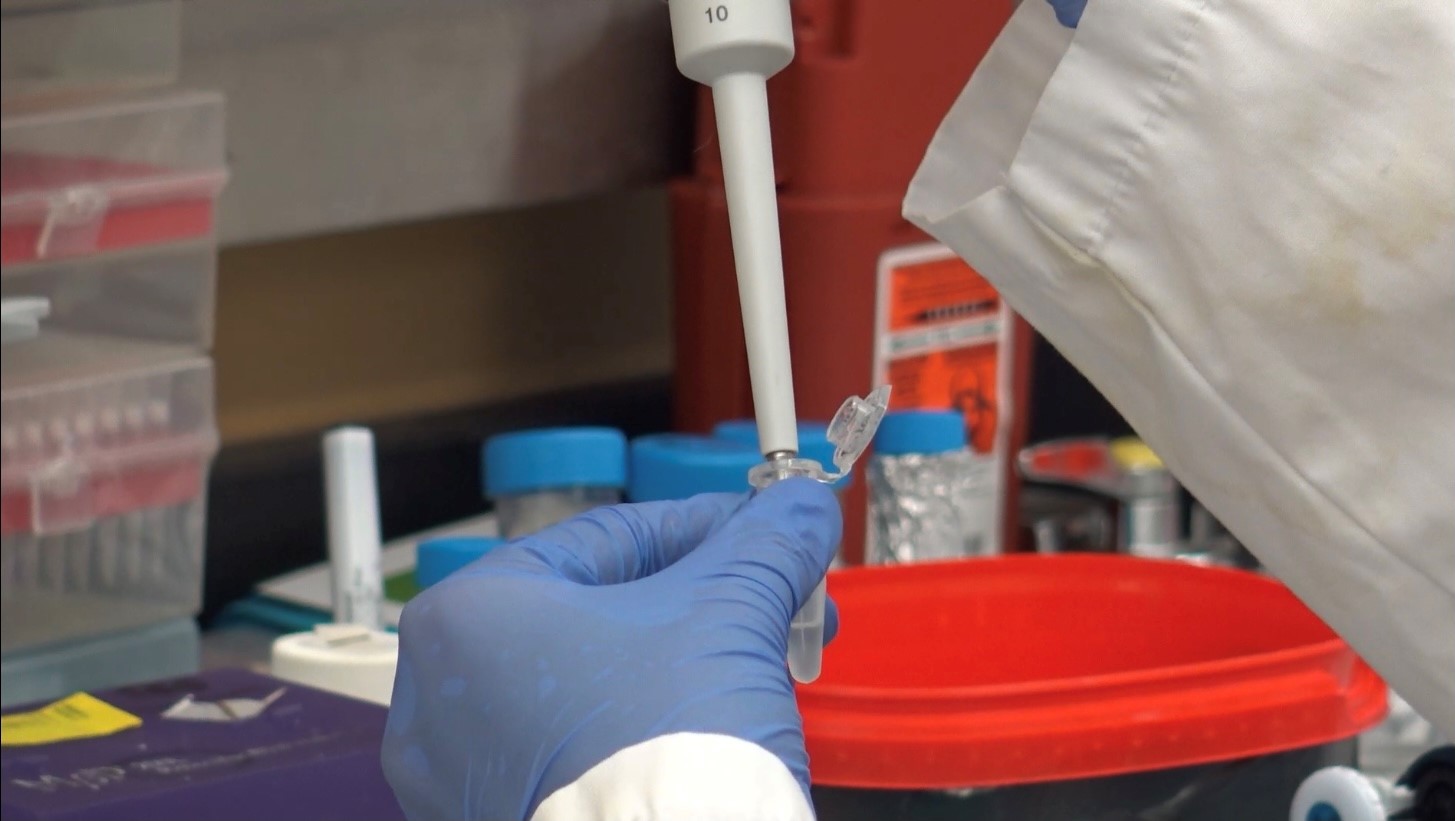
Team players: FMT and microbiome research could have widespread impact

There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system. FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis. Read more.
London researchers adapt MRI technology to image salt within the kidneys

Scientists at Lawson have adapted PET/MRI technology to accurately image salt within the kidneys of patients with kidney disease. Imaging salt within the kidneys has never been accurately accomplished in patients with kidney disease, but Dr. McIntyre and his team developed new technology and software that was adaptable to a PET/MRI machine at St. Joseph’s. Read more.
London researchers discover novel method to diagnose long COVID
Published in Molecular Medicine, researchers at Lawson have found that patients with post-COVID-19 condition (long COVID) have unique biomarkers in their blood. The team is now working on developing a first of its kind blood test that could be used to diagnose long COVID. The discovery could also lead to new therapeutics for this condition. Read more.
Largest trial ever done in hemodialysis care examines optimal dialysis temperature

Published in the Lancet findings from a large clinical trial through Lawson, ICES Western and Western University suggest that lowering dialysis temperatures does not lead to improved patient outcomes, despite previous studies suggesting otherwise. Read more.
To learn more about Lawson research studies, please visit our News and Media page
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Virtual care associated with significant environmental and patient cost savings
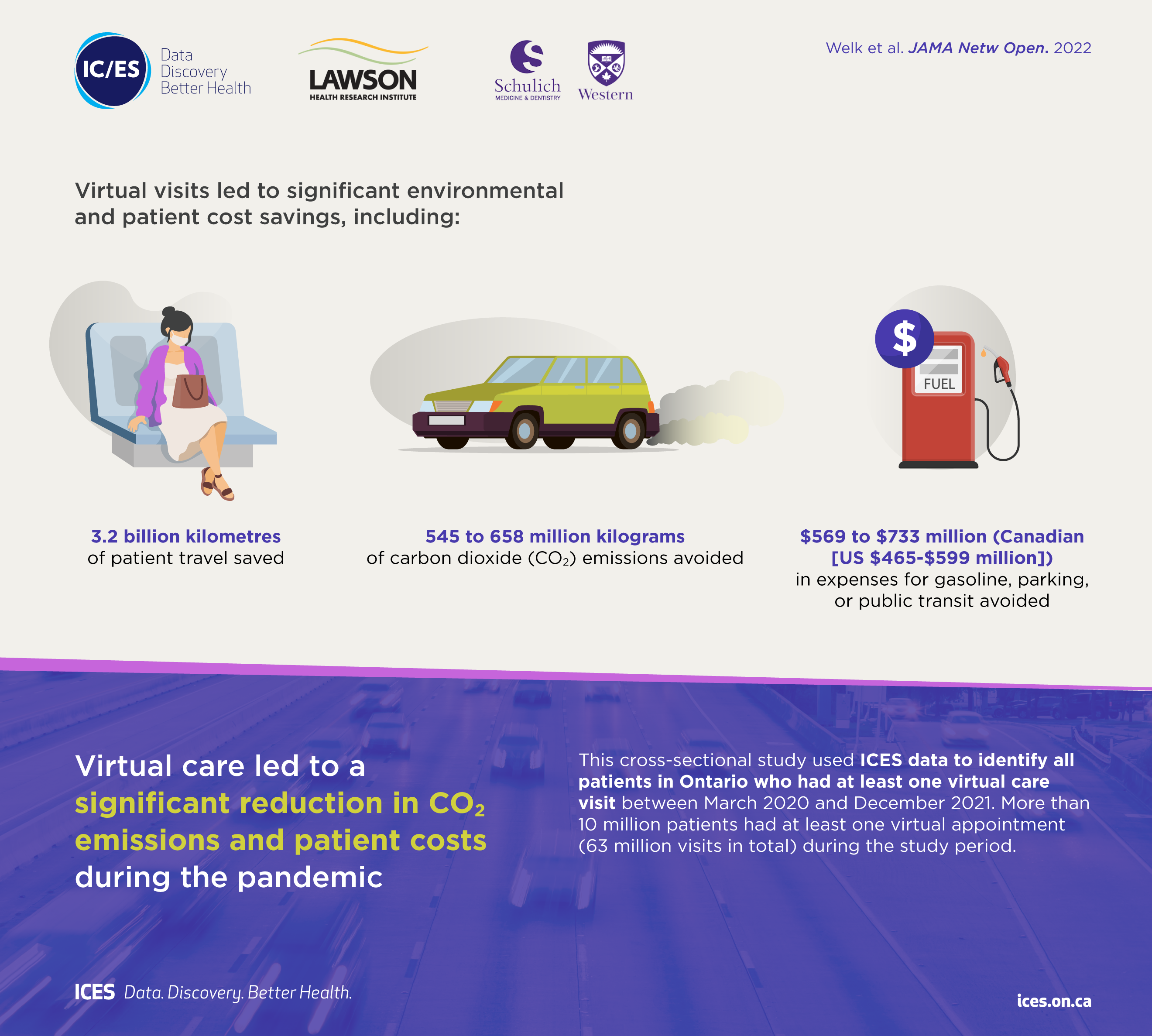
London, ON - A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can
be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Institute for Clinical Evaluative Sciences (ICES) is an independent, non-profit organization that uses population-based health information to produce knowledge on a broad range of health care issues. Our unbiased evidence provides measures of health system performance, a clearer understanding of the shifting health care needs of Ontarians, and a stimulus for discussion of practical solutions to optimize scarce resources. ICES knowledge is highly regarded in Canada and abroad, and is widely used by government, hospitals, planners, and practitioners to make decisions about care delivery and to develop policy. For the latest ICES news, follow us on Twitter: @ICESOntario
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Virtual care associated with significant environmental and patient cost savings
A new study by researchers at ICES, Lawson Health Research Institute and Western University finds that virtual care during the COVID-19 pandemic led to a significant reduction in carbon dioxide emissions and patient travel-related expenses, such as gasoline, parking or public transit costs.
Prior to the pandemic, less than two per cent of patient visits with physicians took place virtually. The beginning of the pandemic (April-June 2020) triggered a rapid transition to virtual visits, which soared to 70 to 80 per cent, and then stabilized at 50 to 60 per cent of all physician visits.
This cross-sectional study published in JAMA Network Open used healthcare administrative data from Ontario, Canada to identify all patients with at least one virtual care visit between March 2020 and December 2021.
“Virtual care has become an important part of the healthcare system in Ontario, and in addition to improved patient convenience, it results in significant environmental and financial benefits for patients,” says lead author Dr. Blayne Welk, associate professor of surgery at Western's Schulich School of Medicine & Dentistry, urologist at St. Joseph’s Health Care London, associate scientist at Lawson, and adjunct scientist at ICES Western. “The financial and environmental benefits of virtual care will likely continue beyond the pandemic and are particularly relevant for some patients who were frequent recipients of virtual care.”
Findings show that for more than 10 million patients with at least one appointment during the study period (63 million visits in total), virtual care was associated with estimated savings of:
• 3.2 billion kilometres of patient travel;
• 545 to 658 million kilograms of carbon dioxide (CO2) emissions; and
• $569 to $733 million (Canadian [US $465-$599 million]) in expenses for gasoline, parking, or public transit.
The avoidance of carbon dioxide emissions during the pandemic due to virtual visits represented approximately 0.2 per cent of the total annual carbon dioxide emissions (150 megatons) from Ontario.
The number of virtual care visits was greater for those aged 65 and older, individuals with multiple health conditions, and those living in urban areas. Due to distance travelled, virtual care may offer more potential environmental benefits and patient cost savings for rural residents. Other factors, such as decreased time off work (given that some virtual visits can be done during the day with little interruption to work) may have had additional benefits for some working adults and parents of young children.
“Virtual visits should not replace all in-person visits, but they are an important option that can enhance the care that physicians provide for patients,” says Dr. Alexandra Zorzi, a Paediatric Oncologist at Children’s Hospital at London Health Sciences Centre and Associate Scientist at Lawson. “Our findings suggest that physicians should continue to offer virtual care appointments when appropriate, especially for patients living in more remote areas and those that have barriers to accessing in-person health care.”
The study, “Association of virtual care expansion with environmental sustainability and reduced patient costs during the COVID-19 pandemic in Ontario, Canada” was published in JAMA Network Open.
Author block: Welk B, McArthur E, Zorzi AP.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca