Search
Search
Celebrating Clinical Trials Day
Clinical trials are the gold standard in medical research, used to test new treatments and medical devices to ensure they are safe and improve patient outcomes.
Each year on May 20, Clinical Trials Day aims to raise awareness about the importance of clinical trials. At Lawson Health Research Institute, our researchers, research staff and learners across London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London (St. Joseph’s) are working daily to advance clinical trials for some of the most pressing health challenges.
“If you look at many areas of medicine, like cancer and cardiovascular disease, part of why those conditions have had dramatic improvements in outcomes over the last several decades is because of clinical trials,” says Dr. Amit Garg, Scientist at Lawson, Lead for the Kidney, Dialysis & Transplantation Research Program at ICES Western, and a Nephrologist at LHSC.
Clinical trials can also provide patient participants with new treatment options and can demonstrate when existing treatments have applications for other diseases.
“We could not conduct clinical trials without patients participating in them,” adds Dr. David Palma, Associate Scientist at Lawson and Radiation Oncologist at LHSC. “A clinical trial is a very rigorous process where we carefully define a treatment and follow patients very closely with extra interventions and tests to see not only how the disease is responding to treatment, but also any effects on a patient’s quality of life.”
It also takes a team to make clinical trials a success, including the critical work of research coordinators, associates and assistants, adds Dr. Swati Mehta, Lawson Scientist based at St. Joseph’s Parkwood Institute.
Dr. Palma also notes that while clinical trials require investment to conduct them, they can ultimately lead to savings in the health system.
“While the primary goal of a clinical trial is to improve or save lives, they often lead to cost savings down the road. Improving cure rates means people don’t need as much treatment and that can save the initial investment many, many times over,” Palma says.
Looking ahead, work is ongoing to make clinical trials more efficient and equitable.
“Eliminating specialized infrastructure would help make trials more equitable, so they are available in smaller communities and at distant sites that otherwise would not have access. Making study materials available in multiple languages and to anyone with accessibility issues can also help,” Garg adds.
“Future clinical trials will need to follow more pragmatic, adaptive study designs that allow us to evaluate therapies or interventions in a more realistic setting,” Dr. Mehta says. “These would also allow us to follow-up with patients that were potentially underrepresented in past research.”
According to researchers at Lawson, the future of clinical trials is bright with hundreds of trials currently underway at LHSC and St. Joseph’s with the goal of improving patient outcomes.
Changing our MINDS
Local youth use art and storytelling to illustrate the personal and system challenges in mental health.
The words and images are both heartbreaking and hopeful.
“Nobody likes you if you are sad.”
you are enough. stay strong. let life surprise you.
“Please don’t leave like everyone else.”
1 year sober. 1 year of school. 1 year building a safe home. 1 year loving myself.
Zine-writing, a personal and introspective medium often used by people who have been marginalized, is an important part of local research that is finding solutions to complex mental health challenges among young adults. Its name derives from its magazine (“zine”) format.
“When we make the voices of people with lived experience central to our research, we can learn from each other and then change the system together,” says Dr. Arlene MacDougall, founder of MINDS of London-Middlesex.
The social innovation and research lab based at St. Joseph’s Health Care London (St. Joseph’s) is dedicated to designing, piloting and testing mental health innovations for teens and young adults. Its recent evolution into MINDS 2.0 adds insights by and for people up to age 35 who have complex, pervasive mental health and addiction issues.
Learning from experts
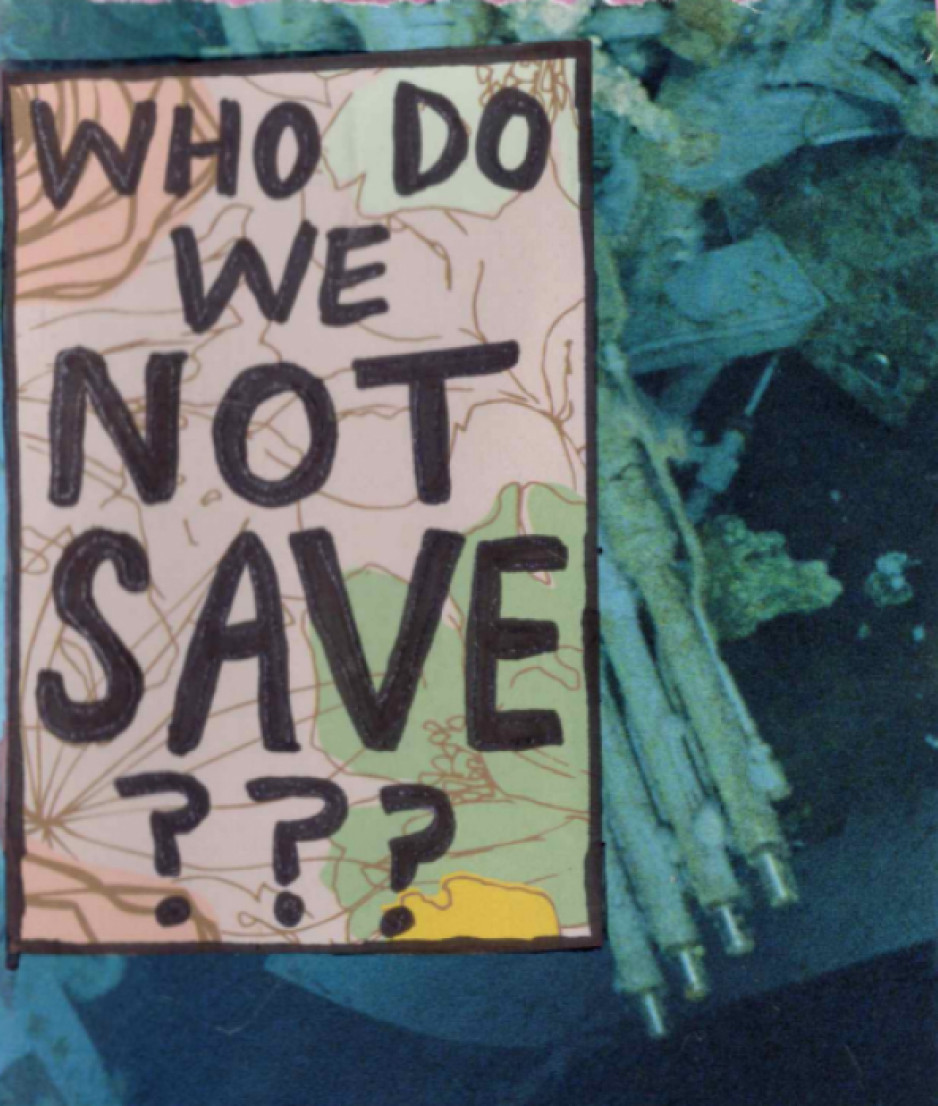
Rin, a London artist, who has published independent zines for a decade, created three for this project, including one that, with irony, asks the reader to ponder which vulnerable people aren’t worth saving.
“I believe making art can be very healing,” says Rin. “I wanted to share some of my story to help myself and help others. I want to play a part in shaping a mental health system that’s better than the one I encountered.”
The zines weave art, prose and poetry into story:
3 things I would change: affordability, stigma, waitlists.
“If I had a magic wand, I would use it to heal the waters, grow the trees, foster animal growth.”
Look in the mirror, see how far you’ve come.
They also raise and propose solutions to troubling issues among people with mental illness: housing and homelessness, sparse resources for people with addictions, lack of coordination among service providers, and dehumanizing attitudes in health and criminal justice systems.
“Participants experienced catharsis just in telling their stories,” says Renee Hunt PhD, Associate Director of Research and Operations at MINDS. “And because they’re the experts, they’re also playing an important part in changing systems that need an overhaul.”
Adds Rin, “It feels empowering knowing people are listening to us – people who care and are committed to making change to the system.”
MacDougall notes the pivotal role of St. Joseph’s Health Care Foundation – in particular, a groundbreaking $5-million donation towards mental health research from philanthropist Ryan Finch – in advancing mental health innovation through MINDS and MINDS 2.0.
“They’ve been our biggest supporters since day one. This wouldn’t have happened without support from Ryan and the foundation and all the many donors who believe in mental health research,” says MacDougall, who is also Director of Research and Innovation with St. Joseph’s Mental Health Care Program.
“MINDS has been a catalyst for system change,” MacDougall adds. “Research is always about finding answers and generating impact.”
Many findings from MINDS research have been put into practice, among them are the creation of guidebooks for peer support, free taxi service for rural youth needing urban mental health or addiction services, and educational resources to support 2SLGBTQI+ students.
MacDougall says MINDS 2.0 expands that work with new voices and the exploration of more in-depth solutions.
What’s next for MINDS 2.0
- Workshopping ideas and prototypes for mental health systems change. Sessions will be held where people with lived/living experience and service providers propose and develop potential solutions.
- Leadership-building. Twenty mental health practitioners will be trained to become “agents of change” who will collectively create, implement and evaluate mental health programs, technology, interventions and training.
- Imaginarium conference. In 2025, a first-of-its-kind national conference will take place to share system innovations in mental health and addiction.
CIHR funding for COVID-19 enables researchers to investigate virus transmission during surgery and pandemic planning
Researchers at Western University and Lawson Health Research Institute continue to make important contributions to help mitigate the spread of COVID-19 and its negative consequences. Two projects in London will address virus transmission during surgery and pandemic planning for COVID-19, thanks to new funding announced by the Government of Canada, through the Canadian Institutes of Health Research (CIHR), along with provincial partners.
Researchers in London received more than $400,000 in funding through this latest round.
“Accelerating high-quality research and real-time evidence is a priority for Canada in its fight against COVID-19. I congratulate the successful teams for their essential work aimed at better preventing, detecting and treating COVID-19 at the individual and population levels,” said Patty Hajdu, Minister of Health in a press release. “Our government believes that it’s through collaboration and data sharing that we will respond efficiently to this global health emergency.”
Virus transmission in surgical smoke
In an effort to perform surgery during the pandemic as effectively and safely as possible, Dr. Leigh Sowerby, Associate Professor at Schulich Medicine & Dentistry and Associate Scientist at Lawson, will be investigating whether or not the virus that causes COVID-19 can be transmitted in surgical smoke. Surgical smoke is the aerosol produced by an essential surgical tool called electrocautery.
“Electrocautery is a ubiquitous tool for surgery, and is known to generate aerosol and smoke. We do not know if the SARS-CoV-2 virus can be transmitted in this plume, and this is important to answer for all surgeons, but in particular, for surgeons working in the respiratory and aerodigestive tract,” said Dr. Sowerby, who is also a head and neck surgeon at London Health Sciences Centre and St. Joseph’s Health Care London. “CIHR funding will allow us to rapidly execute this project. Without this funding, the project would not be possible.”
Dr. Sowerby says the results from this study, whether positive or negative, will have important implications. If positive, it will have a critical and direct impact on ensuring the safety of health care workers performing procedures on patients. Procedures using cautery will continue to require high level protection if the COVID-19 status of the patient is unknown. If negative, it will allow these surgical procedures to continue safely and effectively while conserving critical protective equipment for cases that need it.
The family physician’s role in pandemic plans
Maria Mathews, PhD, Associate Professor at Schulich Medicine & Dentistry, is investigating how the role of family physicians can be better incorporated into pandemic plans. Family physicians play important roles during a pandemic, from detecting potential outbreaks and screening and testing patients to providing care to infected patients and contributing to surge capacity in hospitals.
“During the early stages of the COVID-19 pandemic, family physicians had concerns about roles they were asked to fill for a variety of reasons, including the lack of appropriate personal protective equipment, availability of tests, and concerns about infection risks to other patients and staff in a family practice clinic,” said Mathews.
Mathews will examine the experiences in four regions in Canada – Newfoundland and Labrador, Nova Scotia, Ontario and British Columbia – to identify key roles, supports and best practices. The results will provide government ministries, public health units, and other health organizations with evidence and tools in order to incorporate family physicians in the response to a potential second COVID-19 wave and plan for future pandemics.
Clinical use of EpiSign proven for diagnosing rare heritable disorders
LONDON, ON – A study led by researchers at Lawson Health Research Institute (Lawson) provides clinical validation of EpiSign, a molecular genomics test that diagnoses rare, heritable neurodevelopmental conditions.
Invented at Lawson by Dr. Bekim Sadikovic, the diagnostic test uses machine learning to analyze the EpiSign Knowledge Database. This database compiles information on rare genetic diseases using laboratory analyses of the epigenome from patients with suspected genetic abnormalities. The epigenome is a process that can change the expression of a gene without changing the gene sequence.
“Using 211 blood samples, we measured test performance and diagnostic yield in 207 subjects from two different cohorts,” explains Dr. Sadikovic, lead researcher at Lawson and Scientific and Clinical Director of the Verspeeten Clinical Genome Centre at London Health Sciences Centre (LHSC). The targeted cohort were subjects with previous genetic findings that were ambiguous or inconclusive. The screening cohort were those with clinical findings consistent with hereditary neurodevelopment syndromes but with no previous genetic findings.
“Of the 207 subjects tested, 57 were positive for a diagnostic episignature including 48 in the targeted cohort, and 8 in the screening cohort. Only four remained inconclusive after EpiSign analysis,” says Dr. Sadikovic. “This gives us strong evidence for the clinical use of EpiSign, as well as the ability to provide conclusive findings in the majority of subjects tested.”
While currently there are limited treatment options associated with many of these conditions,
providing a diagnosis can help physicians better predict the course of the disease, and allows for better planning and support for the patient. EpiSign is the only test in the world that has been clinically validated for testing these kinds of genetic disorders.
“Patients with rare diseases often wait years and undergo numerous exams and tests before receiving a correct diagnosis, if one is found at all,” says Matthew Tedder, PhD, staff scientist at the Greenwood Genetic Center, one of the EpiSign clinical testing laboratories. “EpiSign provides an additional high-yield diagnostic tool for clinicians to include in their evaluation of patients with undiagnosed diseases, providing better medical management for patients and hope for their families.”
The study, “Clinical epigenomics: genome-wide DNA methylation analysis for the diagnosis of Mendelian disorders", is published in February’s Genetics in Medicine and was completed in collaboration with the Greenwood Genetic Center and the University of Amsterdam.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca