Search
Search
Study testing benefit of antibodies from people recovered from COVID-19 on severe cases of infection
LONDON, ON – Researchers at Lawson Health Research Institute are taking part in a large, multi-centre study examining the use of convalescent plasma transfusions from people who have recovered from COVID-19 as a possible treatment for infected patients.
When a person is infected with a virus, their immune system produces protein antibodies, specific to that virus, that help the body fight the infection. These antibodies stay in the bloodstream after the person has recovered, and provide a degree of long-term immunity. Convalescent plasma is a term that describes plasma from a person who has recovered from illness. The hope is that naturally derived antibodies for COVID-19 will help fight serious infection in other individuals.
The CONCOR-1 Trial, led by Canadian researchers, will recruit 1,200 participants from Canada and New York. Researchers are collecting blood plasma from recovered COVID-19 patients and transfusing it into seriously ill patients. Measurable outcomes include the rate of intubation and mortality rate after 30 days of enrollment in the trial.
Convalescent plasma donation is being coordinated through Canadian Blood Services. For this study, they are currently collecting plasma from eligible donors under the age of 67 who have fully recovered from COVID-19 and have been symptom free for at least 28 days. Those who are interested in donating can find more information on the Canadian Blood Services website.
Dr. Ziad Solh, Lawson Associate Scientist, and Hematologist and Transfusion Medicine Specialist at London Health Sciences Centre explains, “this is an experiment; we don’t yet know if this treatment will show benefit, but it does show promise as similar treatments have had some success in studies of other viral infections such as SARS.”
Trial participants must be over 16 years of age, requiring oxygen, have been sick for less than 12 days, and their plasma must be compatible with donor plasma.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study to examine health impacts of the COVID-19 pandemic for mothers and their new babies
LONDON, ON - The COVID-19 pandemic has drastically altered many people’s lifestyles. Parents may be working from home, providing additional childcare or experiencing social isolation. Some are dealing with decreased work hours and loss of employment. With all these factors at hand, a team of researchers from Lawson Health Research Institute and Western University are investigating the possible health impacts on mothers and their babies who were born or will be born during the pandemic.
“This has been a stressful and pivotal time for everyone in the world, but we know the post-partum experience can greatly affect both the birthing person and their baby, in the short and long term,” says Dr. Genevieve Eastabrook, Associate Scientist at Lawson and Assistant Professor at Western’s Schulich School of Medicine & Dentistry. “We know perceived stress in the perinatal period may have a contribution to health later in life for the birthing person and their children in terms of overall cardiovascular and metabolic health, bonding experiences, and risk of mood disorders.” Dr. Eastabrook is also an obstetrician-gynecologist (OB-GYN) at London Health Sciences Centre (LHSC).
As part of the new study, the London research team is using an approach called ‘One Health’ which offers a holistic perspective to explore how various risk factors and social determinants of health interact to affect health. This is being studied through the Department of Pathology and Laboratory Medicine at Western. “It’s important for us to think of the environment as all of our surroundings, including the things around us like health care, grocery stores, education and employment,” says Mei Yuan, MSc research student at Schulich Medicine & Dentistry. “The purpose of this study is to look at the pandemic response rather than the pandemic itself. We know that even if women haven’t been infected with COVID-19, it doesn’t mean they haven’t been impacted.”
Study participants are asked to complete a 30-minute questionnaire at around 6-12 weeks after their delivery. The questionnaire focuses on perceived stress, postpartum depressive symptoms, perceived social support, the impact of COVID-19, health-care access and breastfeeding. Data from the questionnaire will be linked with participants’ medical records to look for associations between the various factors and pregnancy outcomes. “Even though the study is mainly focused on maternal health, studies have shown that once mental health is affected it really does impact the infant’s health, especially in the area of attachment between baby and caregivers,” explains Yuan.
Data from the study will be compared to the Maternity Experiences Survey, a national survey of Canadian women compiled in 2007 which looked at experience, perception, knowledge and practice during pregnancy, birth and the early months of parenthood. “The unique aspect here is that we have a comparative group using a historic cohort to see whether or not there are differences in markers that increase risk of depression, perceived stress and lack of social support,” adds Dr. Eastabrook. “We will also look at some unique things from the pandemic, such as how the use of virtual care for antenatal, postpartum and baby care impacted people’s experiences.”
The research team hopes to recruit 300 mothers for this study who have given birth at LHSC, specifically during the pandemic. Interested participants can email the Pregnancy Research Group at @email. Once all the data is collected the goal will be to use the findings to improve post-partum care for mothers and their babies within this population group.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Western delivers an academic experience second to none. Since 1878, The Western Experience has combined academic excellence with life-long opportunities for intellectual, social and cultural growth in order to better serve our communities. Our research excellence expands knowledge and drives discovery with real-world application. Western attracts individuals with a broad worldview, seeking to study, influence and lead in the international community.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study to examine inflammatory response in patients with COVID-19
LONDON, ON – Researchers at Lawson Health Research Institute and Western University have launched a new study to help us better understand how the body’s immune system responds to COVID-19.
Any time there is a threat to the body, the immune system is activated. Some early reports from scientists and physicians working with COVID-19 patients indicate that this virus may cause a cytokine storm, or a heightened immune response, in some patients.
“Some researchers are suggesting that mortality could be improved with immunosuppressive therapies, however, evidence to support this is severely lacking at this time,” explains Dr. Douglas Fraser, lead researcher and Paediatric Critical Care Physician at London Health Sciences Centre (LHSC).
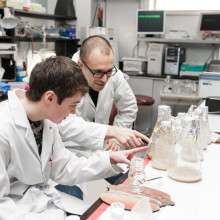
Daily blood samples are being taken from patients at LHSC who are presumed to have COVID-19. The samples are tested for inflammatory biomarkers and this information is recorded to track the changing immune response over time. The immune response in COVID-19 positive patients will also be compared to the immune response in patients with other infections, as well as in healthy controls. Clinical data of enrolled patients is also being recorded, and can be used in future studies.
Dr. Fraser, also a Lawson Scientist and Professor at Western’s Schulich School of Medicine & Dentistry, explains, “if a hyperinflammatory response is found to contribute to greater adverse outcomes from COVID-19, there are current therapies available to help these cases. This study could also inform why some people become critically ill and others do not, and help determine who will respond to certain therapies.”
This research will help provide an overall understanding of how the immune system reacts to COVID-19. As a hospital-based research institute, laboratories at Lawson are uniquely positioned to handle these types of studies, as close proximity to patients and sample collection is essential.
COVID-19, also referred to as the 2019 Novel Coronavirus, is a new respiratory virus first identified in Wuhan, China. On March 12, 2020, the World Health Organization declared COVID-19 a global pandemic. As of March 26, 2020, there are over 510,000 confirmed cases and over 22,000 recorded deaths world-wide.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
The Schulich School of Medicine & Dentistry at Western University is one of Canada’s preeminent medical and dental schools. Established in 1881, it was one of the founding schools of Western University and is known for being the birthplace of family medicine in Canada. For more than 130 years, the School has demonstrated a commitment to academic excellence and a passion for scientific discovery.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Study to examine inflammatory response in patients with COVID-19
Researchers at Lawson Health Research Institute and Western University have launched a new study to help us better understand how the body’s immune system responds to COVID-19.
Any time there is a threat to the body, the immune system is activated. Some early reports from scientists and physicians working with COVID-19 patients indicate that this virus may cause a cytokine storm, or a heightened immune response, in some patients.
A cytokine storm, or a heightened immune response results when excessive levels of cytokines, the activating compounds of immune cells, are released into the bloodstream to attack the virus. This can lead to lung inflammation and respiratory distress. The leading cause of death for patients with COVID-19 is respiratory failure with or without multiorgan dysfunction.
“Some researchers are suggesting that mortality could be improved with immunosuppressive therapies, however, evidence to support this is severely lacking at this time,” explains Dr. Douglas Fraser, lead researcher and Paediatric Critical Care Physician at London Health Sciences Centre (LHSC).
Daily blood samples are being taken from patients at LHSC who are presumed to have COVID-19. The samples are tested for inflammatory biomarkers and this information is recorded to track the changing immune response over time. The immune response in COVID-19 positive patients will also be compared to the immune response in patients with other infections, as well as in healthy controls. Clinical data of enrolled patients is also being recorded, and can be used in future studies.
Dr. Fraser, also a Lawson Scientist and Professor at Western’s Schulich School of Medicine & Dentistry, explains, “if a hyperinflammatory response is found to contribute to greater adverse outcomes from COVID-19, there are current therapies available to help these cases. This study could also inform why some people become critically ill and others do not, and help determine who will respond to certain therapies.”
This research will help provide an overall understanding of how the immune system reacts to COVID-19. With this understanding, targeted therapies can be developed to improve patient outcome and reduce Intensive Care Unit (ICU) demand. As a hospital-based research institute, laboratories at Lawson are uniquely positioned to handle these types of studies, as close proximity to patients and sample collection is essential.
COVID-19, also referred to as the 2019 Novel Coronavirus, is a new respiratory virus first identified in Wuhan, China. On March 12, 2020, the World Health Organization declared COVID-19 a global pandemic. As of March 26, 2020, there are over 510,000 confirmed cases and over 22,000 recorded deaths world-wide.
Study to improve geriatric care in Ontario receives CIHR funding
The Canadian Institutes of Health Research (CIHR) has awarded a $100,000 grant to a project that aims to examine and improve the delivery of care for older adults.
Dr. Jacobi Elliott, Associate Scientist at Lawson Health Research Institute and Coordinator (Geriatrics) at St. Joseph’s Health Care London, has received a Priority Announcement award for her study titled “Implementation, Equity and Impact: Examining specialized geriatric care programs in Ontario.”
“It is critical to provide older adults with timely and equitable access to specialized geriatric care,” says Dr. Elliott. “However, waitlists are growing with the current aging population and there is an increased demand for these services.”
Currently 1.6 million older Canadians are considered to be living with frailty, and that number is expected to double over the next decade. Without adequate geriatric services, older adults living with frailty are more likely to need hospital care. The goal of this research is to examine specialized geriatric care programs in Ontario.
“Across Ontario, there are more than twelve different geriatric outreach models of care, but we have no clear understanding of how these models were developed, implemented or evaluated,” says Dr. Elliott. “It is critical to understand whether the existing services are meeting the needs and goals of the diverse older adult population.”
Dr. Elliott hopes that the project’s findings can be used to inform the development of future specialized geriatric care programs.
Congratulations also goes out to the Lawson Scientists who are receiving CIHR funding totaling nearly $2.5 million through Western University’s Schulich School of Medicine & Dentistry:
Dr. Pingzhao Hu with Dr. Samuel Asfaha
A deep learning approach to identify inhibitors of adherent invasive Escherichia coli in the pathogenesis of inflammatory bowel disease
Dr. Steven Laviolette
Understanding the Effects of Adolescent Nicotine Exposure on Increased Risk for Mood and Anxiety Disorders: Bridging the Gap from Pre-Clinical to Clinical Investigations
Dr. Aaron Ward with Dr. Stephen Pautler
Histopathology image analysis for prostate cancer prognosis after radical prostatectomy
CIHR Priority Announcement recipients:
Dr. Xiao Zhen Zhou and Dr. Doug Fraser
Identification of Novel Disease Drivers, Therapeutic Targets, and Biomarkers of Sepsis
Study will use 3D bio-artificial tissue model to improve understanding of wound healing after glaucoma surgery
James Armstrong, an MD/PhD student at Western University’s Schulich School of Medicine & Dentistry conducting research at Lawson Health Research Institute, is creating a 3D bio-artificial tissue model to study wound healing following glaucoma surgery.
There are currently no curative treatments for glaucoma, the leading cause of irreversible blindness world-wide. The only therapy that can delay the progression of the disease is the reduction of intra-ocular pressure, which can be accomplished by taking drugs or undergoing surgery. Surgery is usually a last resort if pharmacological treatment is unsuccessful as many of these surgeries fail due to excessive healing of the surgical wound. A dense, scar-like tissue can develop at the surgical site, which blocks the pressure-lowering effect and leads to surgical failure, revision and even blindness.
Armstrong will identify risk factors for fibrotic glaucoma surgery failure through reviews of electronic patient records and literature. Using the constructed model of the ocular tissue involved in glaucoma surgery, he will simulate the surgical wound to study the physiology of how the tissue heals and test potential drugs designed to modulate the wound healing process.
The project has been awarded a Lawson Internal Research Fund (IRF) Studentship, and is supervised by Lawson scientist and St. Joseph’s Health Care London physician Dr. Cindy Hutnik.
“Right now there is a shift happening towards earlier surgical interventions for glaucoma so an understanding of the wound healing response is critical to ensure safe and successful outcomes for patients,” Armstrong says. “Future work in this area could include developing a diagnostic test to inform physicians of a patients’ likelihood of excessive healing before the patient even sets foot in the operating room. This will allow surgeons to ‘customize’ how they pre-treat each individual patient with wound healing modulating drugs.”
Although this study is focused on wound healing within the eye, the same processes are at work in many other diseases. Understanding and having the ability to manipulate wound healing mechanisms could have widespread applicability, not only for glaucoma, but also for other diseases such as atherosclerosis, interstitial pulmonary fibrosis, hepatic fibrosis, systemic sclerosis or muscular dystrophy, as well as heart, kidney or liver failure.
“The IRF has given me the opportunity to pursue research in an area where any progress could impact a significant portion of the population,” Armstrong says. “It’s a great way for researchers who are early in their career to get a foot in the door. It allows them to collect the amount of data necessary to receive funding from larger granting agencies.”
The IRF is designed to provide Lawson scientists and students the opportunity to obtain start-up funds for new projects with the potential to obtain larger funding, be published in a high-impact journal, or provide a clinical benefit to patients. Funding is provided by the clinical departments of London Health Sciences Centre and St. Joseph’s Health Care London, as well as the hospital foundations (London Health Sciences Foundation and St. Joseph's Health Care Foundation).

Supporting a rapid research response during the pandemic
LONDON, ON – Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca
Supporting a rapid research response during the pandemic
Hospital-based research is uniquely positioned to tackle the unprecedented COVID-19 challenge and quickly translate results into illness prevention and care for patients. Lawson Health Research Institute, the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London, has awarded more than $202,000 to its research teams to support critical discoveries during the pandemic.
Over 14 projects ranging from improved diagnostics to understanding the impact of the COVID-19 pandemic on frontline health-care workers have been funded through Lawson’s Internal Research Fund (IRF) COVID-19 Pandemic Response Competition.
“Lawson researchers are an intrinsic part of health care in London. Our research community has mobilized quickly to the COVID-19 pandemic and has come forth with innovative ideas to prevent infections, aid recovery and reduce the likelihood of mortality in those most seriously affected,” says Dr. David Hill, Scientific Director for Lawson. “Lawson has reallocated internal granting resources to enable some of the most exciting and credible ideas to be explored.”
Launched in March, this rapid response competition was focused on funding projects, such as two described below, that could impact the management of the pandemic and enhance our understanding of the novel coronavirus.
Using genetic therapy to block entry of the virus
Progression of COVID-19 depends on human proteins that the virus uses to escort itself into lung cells to cause disease. “There are three such ‘virus entry’ proteins that are particularly important for infection. We see them as potential targets for drugs to prevent and treat COVID-19,” explains Dr. James Koropatnick, Lawson Scientist and Principal Investigator for one of the funded studies.
There could be dangers in targeting these proteins, particularly for patients taking certain blood pressure-reducing drugs. The team is studying the safe use of a new type of drug – powerful “antisense” agents that block messenger RNAs which are the biological “blueprints” for the target virus entry proteins – to stop the virus from using those proteins to infect lung cells. They are testing two types of antisense molecules that reduce the amount of the virus entry proteins. “With our existing knowledge and infrastructure in place, this testing could rapidly lead to new, non-vaccine agents to prevent and treat COVID-19, as well as future coronaviruses with pandemic potential,” adds Dr. Koropatnick.
The impact of the pandemic response for those with disabilities
The COVID-19 pandemic has disrupted the daily lives of Canadians, with worsening mental health as people adapt to different stressors. “While many are struggling with this new normal, the degree of disruption resulting from the pandemic presents unique challenges for those with spinal cord injury and brain injury,” says Dr. Eldon Loh, Lawson Associate Scientist also leading one of the funded studies.
Relatively simple tasks such as frequent hand washing can be challenging for those with disability, and they may be more vulnerable to poor outcomes because of the decreased respiratory function many already face. The research team will document and evaluate the effect of the pandemic on the physical and mental health of those with spinal cord and brain injuries. “We plan to use our findings to provide guidance to those living with spinal cord and brain injury, and improve their quality of life during this challenging time. We expect that this study will not only help those with spinal cord and brain injuries, but also people living with other disabilities as well,” notes Dr. Loh. He is also a Physical Medicine and Rehabilitation Specialist at St. Joseph’s.
The IRF competition is supported with funding from clinical departments at LHSC and St. Joseph’s, and from London Health Sciences Foundation and St. Joseph’s Health Care Foundation.
Congratulations to all of the researchers and their teams who have been awarded funding:
- Dr. Ian Ball - Predictors of clinical deterioration in hospitalized patients with COVID-19: The CORAL study
- Dr. Doug Fraser - Translational Research Centre: Repository of biological specimens from patients
- Dr. Sean Gill - Rapid identification of therapeutic targets mediating pulmonary microvascular endothelial cell dysfunction in COVID-19 patients
- Dr. Marnin Heisel - Testing Online Meaning-Centered Men’s Groups to Promote Psychological Well-Being and Reduce Despair in the Face of the COVID-19 Pandemic
- Dr. Kimia Honarmand - The impact of the COVID-19 pandemic on frontline healthcare workers: A Southwest Ontario survey
- Dr. Michael Knauer - Improving diagnostic and epidemiologic detection of SARS-CoV-2
- Dr. Jim Koropatnick - Targeting the SARS-CoV-2 receptor with candidate antisense drugs to prevent infection and disease progression
- Dr. Eldon Loh - COVID-19 and Disability: The Impact of a Societal Lockdown on those with Spinal Cord and Brain Injuries
- Dr. Len Luyt - Stapled Peptides as SARS-CoV-2 Fusion Inhibitors
- Dr. Claudio Martin - COVIDOPATHY – An observational study of coagulation abnormalities in patients with COVID-19
- Dr. Tianqing Peng - Developing new ssDNA aptamers targeting S protein receptor binding domain of SARS-CoV-2 to disrupt virus infection cycle as a potential therapy
- Dr. Eva Turley - Hyaluronan signaling through the inflammasome is a target for blunting acute respiratory distress syndrome (ARDS) in COVID-19 patients
- Dr. Ruud Veldhuizen - Next generation exogenous surfactants for COVID-19 and future respiratory pandemics
- Dr. Blayne Welk - Characterizing the burden of surgical care in COVID-19 positive patients
Symposium features research on health through food and microbes
The past decade has featured rapid acceleration in the study of microbes and how they influence human and planetary health. This includes the study of probiotics and their diverse benefits.
On Friday, May 4, Lawson Health Research Institute (Lawson) and Western University hosted a free public symposium on health through food and microbes.
With more than 80 attendees, the symposium covered dynamic areas of research that are collectively impacting society and human wellbeing. These include the critical role of honey bees in pollination, bioremediation of toxic compounds, fermented food, maternal and infant nutrition and how microbes can confer a range of health benefits. The topics included a view of life in developing countries and efforts to help people overcome many challenges.
The event was opened by Dr. Bing Gan, Lawson scientist, plastic surgeon at St. Joseph's Health Care London and professor at Western’s Schulich School of Medicine & Dentistry, who described his harrowing experience working for Doctors Without Borders in the Congo.
“We live in a microbial world, and beneficial ones are essential to the future of our planet and for human wellness and longevity,” says Dr. Gregor Reid, a scientist at Lawson, professor at Western’s Schulich School of Medicine & Dentistry and lead organizer of this symposium. “The highly respected speakers at this event highlighted the potential for microbes to improve global health, and reminded us of the fragility of life on this planet.”
The event was made possible by a grant from the Gairdner Foundation for a lecture titled, “Food for 9.7 billion people,” by Dr. Rob Vos, Director Markets, Trade and Institutions, International Food Policy Research Institute, Washington, DC. The lecture was delivered by Dr. Reid as Dr. Vos unfortunately experienced travel delays.
The event also featured locally produced fermented foods provided by Booch and Nuts For Cheese.
Synthetic surfactant could ease breathing for patients with lung disease and injury
Human lungs are coated with a substance called surfactant which allows us to breathe easily. When lung surfactant is missing or depleted, which can happen with premature birth or lung injury, breathing becomes difficult. In a collaborative study between Lawson Health Research Institute and Stanford University, scientists have developed and tested a new synthetic surfactant that could lead to improved treatments for lung disease and injury.
Lung surfactant is made up of lipids and proteins which help lower tension on the lung’s surface, reducing the amount of effort needed to take a breath. The proteins, called surfactant-associated proteins, are very difficult to create in a laboratory and so the surfactant most commonly used in medicine is obtained from animal lungs.
London, Ontario has a rich legacy in surfactant research and innovation. Dr. Fred Possmayer, a scientist at Lawson and Western University, pioneered the technique used to purify and sterilize lung surfactant extracted from cows. Called bovine lipid extract surfactant (BLES), the therapeutic is made in London, Ontario and used by nearly all neonatal intensive care units in Canada to treat premature babies with respiratory distress.
“When we look at treating adults, surfactant therapy is more difficult. For example, their lungs are 20 times bigger than those of babies and so we need much higher doses of surfactant,” explains Dr. Ruud Veldhuizen, a scientist at Lawson and an associate professor at Western University’s Schulich School of Medicine & Dentistry. “We therefore need to find novel approaches to surfactant therapy for adult patients.”
In this collaborative study, the research team took a new approach to creating synthetic surfactant. Rather than trying to recreate surfactant-associated proteins in the lab, scientists at Stanford created protein mimics. Pioneered by Dr. Annelise Barron, associate professor at Stanford, these protein mimics look like surfactant-associated proteins and have similar properties but are easier to create and more stable. As a result, the team was able to create a new synthetic surfactant.
Collaborating with the Stanford team, Dr. Veldhuizen evaluated the synthetic surfactant in animal models in his research lab at St. Joseph’s Health Care London. The study showed that, unlike other synthetic surfactants currently on the market, the new surfactant equaled or outperformed the animal-derived surfactant in every outcome. This included outperforming animal-derived surfactant in oxygenating blood, which is the lungs’ main purpose.
“The unique ability of the Veldhuizen lab to perform these rigorous and sophisticated studies was a critical aspect of the success of this project,” says Dr. Barron.
“These are very promising results,” says Dr. Veldhuizen. “For the first time, a synthetic surfactant has been developed which appears to be just as effective, if not more so, as that taken from the lungs of animals.”
The team estimates that the synthetic surfactant could be produced at as low as one quarter of the cost of the animal-derived surfactant. With a lower cost the synthetic surfactant could be tested with more lung diseases and injuries in adults and made available in more developing countries.
The team hopes to continue their research with further testing of the synthetic surfactant, including its long term effects. The team also hopes to test its ability to be customized for specific diseases. “Since it is made in the lab, we could combine the surfactant with other drugs like antibacterial agents and deliver it to specific areas of the lung, such as those where an infection is located,” explains Dr. Veldhuizen.
One disease the scientists would like to further study is acute respiratory distress syndrome (ARDS). ARDS is characterized by a low amount of oxygen in the blood due to difficulty breathing. While current surfactants have been tested with ARDS patients, they have not been effective. Dr. Veldhuizen wants to combine this new synthetic surfactant with anti-inflammatory agents and antibacterial agents to test whether patient outcomes are improved.
The study, “Effective in vivo treatment of acute lung injury with helical, amphipathic peptoid mimics of pulmonary surfactant proteins,” is published in Scientific Reports.
Team players: FMT and microbiome research could have widespread impact
There is still much to learn about the human microbiome and its role in fighting disease, but ongoing studies at Lawson Health Research Institute, including a focus on fecal microbial transplants (FMT), are making strides in harnessing this complex system.
FMT is being studied in connection with conditions as varied as non-alcoholic fatty liver disease, rheumatoid arthritis, atherosclerosis, HIV, cancer and multiple sclerosis.
FMT is already in clinical use for the treatment of C. diff (Clostridium difficile), and in addition to showing promise in the treatment of other diseases, it is also being studied as a way to improve response to existing cancer treatments and ease treatment side effects.
Dr. Saman Maleki, a Scientist at Lawson Health Research Institute and the London Regional Cancer Program (LRCP) at London Health Sciences Centre (LHSC), says they’ve just begun to explore the possibilities.
"We are just starting to study FMT as an intervention outside its traditional use in patients with C. difficile infection, and we will be expanding to other areas, particularly in cancer.”
FMT can overhaul a patient’s microbiome, Dr. Maleki explains, and a healthy microbiome is beneficial especially when a treatment is trying to activate the body’s immune system.
Dr. Michael Silverman, Lawson Associate Scientist and Medical Director of St. Joseph’s Health Care London’s Infectious Diseases Care Program, is a pioneer in the field of FMT. He has been performing the procedure since 2003 with C. difficile patients and was one of the first in North America to do so. He sees a wide range of possible applications.
“FMT has enormous potential in being an important adjunctive therapy in many cancers. It may, for example, help cancer patients respond to immunotherapy,” says Dr. Silverman, who is also Chair/Chief of Infectious Disease at St. Joseph’s Health Care London, LHSC and Western University. “The potential to impact autoimmune and metabolic diseases is also quite exciting, but still in early development.”
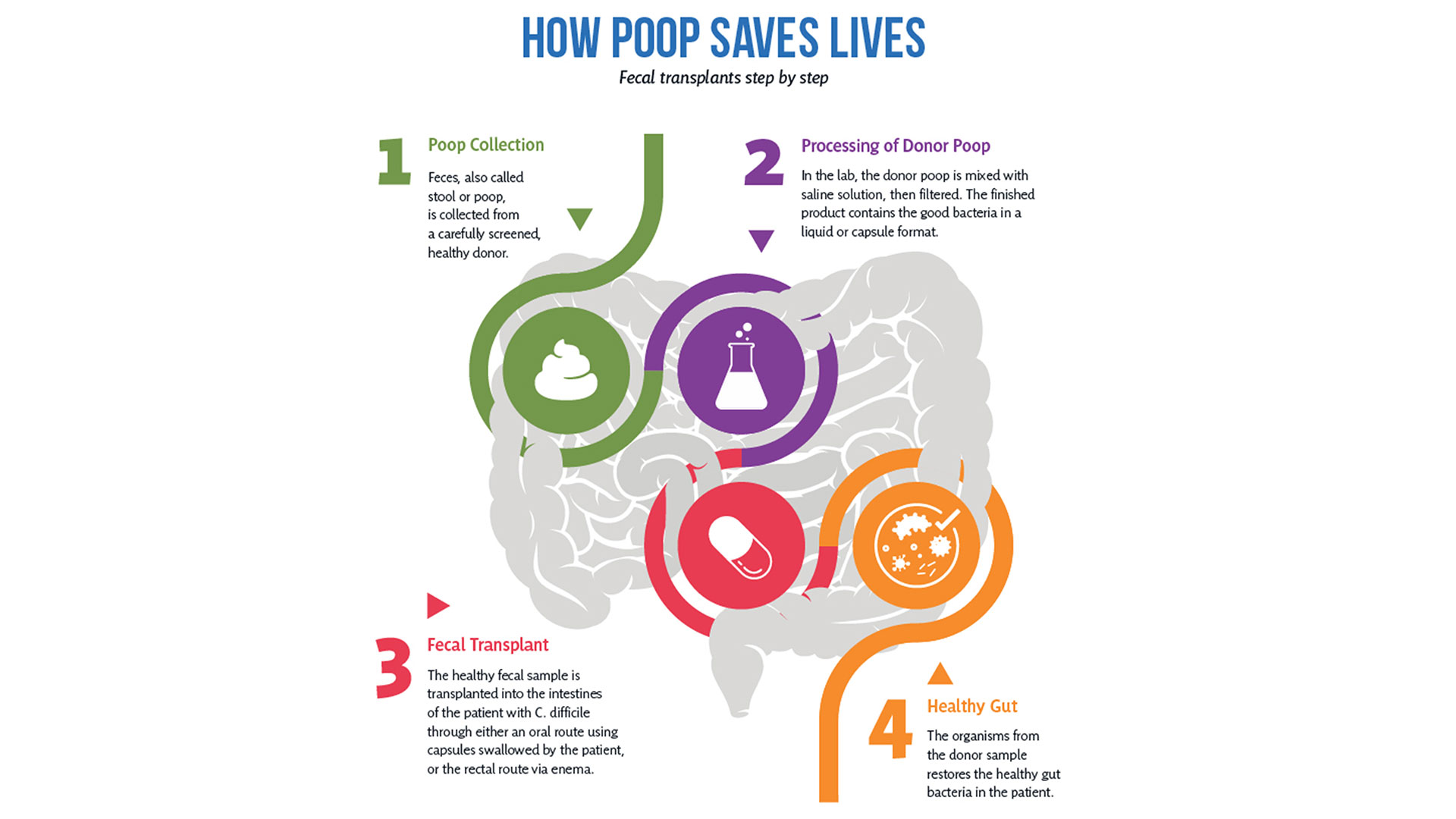
So how does it work?
After rigorous screening, stool from a healthy donor is collected and then processed in a lab into a liquid or capsule containing the good bacteria, which can then be administered to a patient’s gastrointestinal tract.
The Lawson team is also one of few delivering FMT using specially-prepared oral capsules. Introduced in 2018, they have been a game changer in patient acceptance and ease of administration, according to Research Coordinator Dr. SeemaNair Parvathy, who has been coordinating the program since 2015.
“There is a link between the fitness of the intestinal microbiome and the fitness of the immune system,” says Dr. John Lenehan, Associate Scientist at Lawson and Medical Oncologist at LHSC. “A ‘healthy’ microbiome leads to a more robust immune response when using immunotherapy. FMT from a healthy donor is expected to improve the fitness of the recipient’s intestinal microbiome and promote a better immune response.”
People with chronic disease can often experience what’s called a ‘leaky gut,’ allowing food, bacterial and microbial components to pass through the intestinal wall, negatively impacting the immune system.
“When people get FMTs their intestinal permeability improves – meaning it actually reduces,” says Dr. Jeremy Burton, Lawson Scientist and Research Chair of Human Microbiome and Probiotics at Lawson and St. Joseph’s. “What changes that intestinal permeability? The microbes at the site. They play a role in interacting with the host cells, providing nutrients and vitamins.”
With the immune system so closely tied to the health of the microbiome, it’s not surprising scientists are exploring how strengthening one can have a big impact on the other.
Boosting immunotherapy
Immunotherapy can be used to either stimulate or suppress the immune system to help the body fight disease, and FMT is showing promise in reducing resistance to the treatment.
While immunotherapy has been effective in treating a number of cancers – the number one cause of death in Canada – not all patients respond to the treatment.
But early work presented at a conference by the Lawson team for the Journal for ImmunoTherapy of Cancer has shown that using FMT to modify the microbiome could reduce resistance to immunotherapy. The study involved patients from LHSC with advanced melanoma, a type of skin cancer.
While in the very early stages, the combination of FMT and anti-PD1 immunotherapy has been found to be safe, and it appears that FMT could make tumours more responsive to the immunotherapy treatment.
“Microbiome-based treatment strategies, including FMT, have a high potential in oncology,” says Dr. Maleki. “Our team is also exploring its potential in treating pancreatic cancer.”
The research is so interesting that a recent Nature article listed the Phase I melanoma trial as “seminal” research. The study was also unique in that it used healthy donors, as opposed to donors who had previously responded to immunotherapy treatment.
A separate Lawson study with LHSC patients with metastatic renal cell carcinoma, a type of kidney cancer, published in the Journal of Clinical Oncology, also looked at combining immunotherapy and FMT to ease the adverse effects of the treatment.
The Phase I study, led by Dr. Maleki and Dr. Ricardo Fernandes, Medical Oncologist at LHSC, found adding FMT to doublet immunotherapy was safe, but further study is needed to determine whether it could bring about changes in the microbiome and immune system.
Dr. Lenehan says Lawson researchers are in a position to be leaders in this field in the near future for two reasons.
“One is that other academic researchers have not been able to assemble the expertise, and some who have, do not have the access to healthy donor stool. The second is that some biotechnology companies are interested in FMT, but almost exclusively for C. difficile infections.”
Autoimmune, metabolic and other illnesses
Two other areas that have seen recent advances include FMT for the treatment of non-alcoholic fatty liver disease (NAFLD) and multiple sclerosis.
“The gut microbiome is very important in the metabolism of foods and metabolic products. It can therefore have a major effect on obesity and atherosclerosis,” says Dr. Silverman. “It also is tightly involved in regulating the immune system and therefore moderating the microbiome may potentially impact autoimmune diseases.”
A study published in 2020 by the team in The American Journal of Gastroenterology showed that FMT appears to reduce intestinal permeability in patients with NAFLD.
The number of people with NAFLD is growing rapidly and studies show patients have different microbiota than healthy persons.
The trial included 21 NAFLD patients from LHSC and St. Joseph’s. While the researchers found no changes in percentage of liver fat or insulin resistance, they observed significant reduction in intestinal permeability in those patients who had elevated intestinal permeability at the study’s start (seven patients in total). They also observed changes to the gut microbiome in all patients who received a fecal transplant from a healthy donor.
“Metabolic syndromes including obesity and its complications of NAFLD and atherosclerosis are massive public health problems. Any impact on these would be of huge importance,” Dr. Silverman adds. “Autoimmune diseases also cause major morbidity and mortality. We have a lot of work to do before we can consider FMT as a routine therapy for any of these conditions, but the long-term promise is great.”
Research into the use of FMT for treatment of patients with multiple sclerosis is in the very early stages. But patients with MS show a difference in gut microbiota and higher small intestine permeability, which could contribute to the development of the disease.
A Phase I trial by the Lawson team published in the Multiple Sclerosis Journal – Experimental, Translational and Clinical, found FMT to be safe and tolerable.
While the study was very small, MS patients treated with FMT were found to have beneficial changes to gut microbiota and intestinal permeability, but further study is needed to determine if FMT could be used as a treatment.
Lawson scientists are also currently studying the use of FMT for patients with atherosclerosis, along with ongoing studies on melanoma and lung cancer. Funding for a study on pancreatic cancer has been secured and researchers are in the process of planning trials for a number of other applications.
Dr. Lenehan says, “The microbiome is connected to several diseases and their treatments. Evidence is growing that an individual’s health is related to their microbiome.”

The donor challenge
The challenge of finding fecal donors for FMT and the cost of that process remain an issue for research into this promising treatment, even as more potential applications are discovered.
There is currently no process in place to match donors and recipients – as with organ donation – but there is an extensive screening process for both infectious and non-infectious conditions, one that needs to be repeated if a donor experiences any lifestyle changes.
Dr. Burton says, “We still don't understand the full role of the microbiota. We have to ensure that we're not giving patients a microbiota that might cause them some other issue in the future, so the donors are screened very thoroughly for that.”
Screening also excludes donors with an increased risk of developing the diseases scientists are hoping to treat, such as metabolic syndrome related conditions.
A 2017 article published in Open Forum Infectious Diseases by Drs. Silverman and Burton found the cost of screening high numbers of potential donors could make establishing local programs extremely difficult, so having a central program such as the one in London could help patients in many regions.
In the study, only five of 46 potential donors passed the history, examination, blood, stool and urine tests, and of the five, four later travelled or had illnesses that made donation inadvisable.
The search continues in London for potential donors to help drive this research forward. You can read one donor’s story and learn how you can get involved here.
More on FMT and the microbiome:
Drugs vs. bugs: Harnessing the microbiome to improve treatments
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
The Best in Breast Care Conference
On Oct. 15, 2016, the Breast Care Program of St. Joseph’s Health Care London will be hosting the first annual Best in Breast Care Conference, which will feature leading experts in breast screening, diagnosis, treatment, reconstructive surgery, research, support, and survivorship.
Open to health professionals, students/trainees and the general public, this group learning program meets the certification criteria of the College of Family Physicians of Canada and has been certified by Continuing Professional Development, Schulich School of Medicine & Dentistry for up to 6.25 Mainpro+ credits.
When: Oct. 15, 2016, 8:00 am to 4:00 pm
Where: Best Western Lamplighter Inn, London, ON
Host: Presented by St. Joseph’s Health Care London, Supported by ONERUN
Keynote address: Surgical oncologist Dr. May Lynn Quan, University of Calgary, will present on improving outcomes for young women with breast cancer.
For the full agenda and to register, visit www.sjhc.london.on.ca/breast-care-conference.
The children of Masiphumelele Township
Written by Dr. Gregor Reid, scientist at Lawson and professor at the Schulich School of Medicine & Dentistry, Western University
Just off the main road from Cape Town, South Africa to Simon’s Town, sits Masiphumelele Township where challenges of poverty, malnutrition, HIV and the risk of violence face people every day.
It is also the location for the Desmond Tutu HIV Foundation Youth Centre, a safe haven that provides adolescent-friendly sexual and reproductive health services alongside educational and recreational activities for youth living in Masiphumelele and surrounding areas.
To understand some of the dangers that children face, in 2017 about 270,000 people in South Africa were newly infected with HIV, adding to one of the highest HIV prevalence rates in the world. The Tutu Youth Centre aims at helping educate youth to reduce their risk of becoming another HIV statistic.
I was invited there by University of Cape Town Professor Jo-Ann Passmore, a woman not only recognized for her research but whose passion for helping others is reflected in her warm smile (fourth from left in the below group photo). She asked if I would be interested in holding a workshop to illustrate to the youth how using sachets of probiotic bacteria could empower them. I jumped at the chance. On an afternoon break from the Keystone Symposium, thirty researchers joined me along with Jo-Ann and my wife Debbie, a teacher of children with learning disabilities.

After a tour of the areas where children learn on computers, play games in safety, or have personal discussions about sexual health, everyone filled the room with a stunning backdrop of the Nobel Laureate’s image. Having been privileged to meet the Archbishop when he was hosted by St. Joseph’s Health Care Foundation in 2008, it was a nerve-tingling experience.
Giving a lecture on beneficial microbes is hard enough to peers sitting in the back of the room, but to do so with young South Africans was somewhat more daunting. However, it proved to be a lot of fun especially when we had to identify kids who were good leaders (the boys all pointed to a girl), at making stuff and selling it to others (two boys stood out). By the end, we had picked the staff of a new company.
The next step was for four groups to go and decide on the company’s name, what products they’d make from the probiotic sachets (the options were many from yoghurt to cereals, juices and maize), what marketing tools they would use and who they would target to obtain a respectable income.

Interestingly, several of the conference participants seemed less engaged, as if they had never considered how microbiology research could affect real lives. In front of them were children facing huge challenges on a day-to-day basis. In one group, the kids were quiet until my wife brought out pens and paper, then they went to town designing products, names and labels. A lesson for me on how different people need different stimuli to become engaged. The faculty left early to beat the traffic back to Cape Town, so unfortunately, they did not hear the outcome of the children’s work.
When we re-assembled to present the results, I was impressed with what could be created in such a short time. My favourite was the Amazing Maize, a bottle shaped like a corn cob. It emphasized the importance of marketing and for products to taste and look good to be purchased.
It had been over ten years since Archbishop Tutu had applauded us for the Western Heads East project, and thanked us for empowering women and youth and contributing to nutrition in Africa. Since then, thanks to the huge efforts of Western University staff and students, and more recently IDRC funding and partnerships especially with Yoba-for-life, Heifer International and Jomo Kenyatta University of Agriculture and Technology, over 260,000 people in east Africa are now consuming probiotic yoghurt every week. The children of the South African townships were maybe too young to join in this new wave of microenterprises, but at least now they have heard about it and the importance of fermented food and beneficial bacteria.

In the background of the workshop several wonderful women committed to start up a new production unit. I left them some sachets to try out the process.
But it was me who left with the biggest lesson on how precious each life is, and how those of us with the knowledge need to provide the means for others to use their own talents to fulfill the purpose that their lives surely have.
No better way than to start with the children.
Gregor Reid PhD MBA FCAHS FRSC
Scientist, Lawson Health Research Institute, and Professor, Western University
London, Canada

The Dean's Gala - Schulich School of Medicine & Dentistry
London Convention Centre, 300 York Street, London, ON
Dr. Michael J. Strong, Dean, Schulich School of Medicine & Dentistry invites you to celebrate the excellence, innovation and leadership found within Schulich Medicine & Dentistry alumni.
Together, you will toast the recipients of the Schulich Medicine & Dentistry Alumni of Distinction Awards, recognizing alumni who have made outstanding contributions to the School, the community, and their profession. After dinner, dance the night away with friends, colleagues and former classmates to the music of Juno nominated singer Mac Graham and his band.
Tickets: $100 per person
Reunion Year Tickets: $75 per person (Alumni with graduating years ending in 1 or 6)
Table of 10: $1,000
Tickets include a complimentary cocktail, hors d'oeuvres, and a succulent three-course meal accompanied with wine. Black tie optional.
For more information, please visit the event website.
The invisible world inside us
The human microbiome is a wonder of nature.
Trillions of microbes call our body home. They live in our gut and many other places throughout our body. They are involved in virtually every aspect of how we function and we are learning that they are essential to staying healthy. An unhealthy microbiome has been linked to many diseases from allergies to cancer and even mental health.
Most people out there have heard about probiotics and fermented foods, and chances are you’re trying to get more of them in your diet.
Drinking kombucha or eating yogurt, anyone?
Join Lawson Health Research Institute for our next Café Scientifique event, "The invisible world inside us: Exploring the human microbiome."
Hear from a panel of researchers who are unraveling the mysteries about the microbiome and using that knowledge to improve health and health care. They will also bust some myths and share the important facts when it comes to probiotics, prebiotics and the microbiome.
Image

SPEAKERS
- Dr. Gregor Reid, Lawson Scientist and Professor of Microbiology & Immunology and Surgery at Western University.
Presenting: Probiotics and Prebiotics - Look beyond the fake news - Dr. Michael Silverman, Lawson Associate Scientist, Chair of Infectious Diseases, Schulich School of Medicine & Dentistry at Western University and Chief of Infectious Diseases for St. Joseph’s Health Care London and London Health Sciences Centre.
Presenting: Fecal Transplants: What does this crap have to do with me? - Dr. Jeremy Burton, Lawson Scientist and Assistant Professor of Surgery (Urology) and Microbiology & Immunology at Western University.
EVENT DETAILS
Date: Wednesday, November 27, 2019
Time: 7-9 pm (doors open at 6:30 pm)
Location: Best Western Plus Lamplighter Inn & Conference Centre (Regency Room), 591 Wellington Rd, London, ON N6C 4R3
Map and directions.
Parking: Free on-site parking
This is a free event and online registration is REQUIRED.
Registration for this evengt is now FULL.
Please fill out the form here to be added to the waitlist.
You will be notified should a spot open up.
Therapeutic seizure for depression: The positive and not so positive effects
You are invited to the second in a series of Research Bites. These informative and interactive talks focus on specific illnesses, their prevention and related research being conducted by researchers in London, Ontario.
Topic: Therapeutic seizure for depression: The positive and not so positive effects

The talk will include an overview of convulsive therapy, the benefits and risks, and new research to overcome some of the cognitive side effect of the treatment. It will also include a dialogue between Dr. Burhan and a family that went through the experience of electroconvulsive therapy to elicit the experience from the consumer perspective.
Date: Thursday, June 6, 2019
Time: 4 - 5 pm
Location: Parkwood Institute, Mental Health Building, Auditorium (F2-235)
550 Wellington Road South
London, Ontario N6C 0A7
Maps and Directions for Parkwood Institute.
Parking: The lot rate is $4.00 when you enter. $1 and $2 coins and credit card accepted (press the start button then insert payment)
Registration is required and spots will fill up quickly.
Click here to register.
These talks are hosted by Parkwood Institute Research, a program of Lawson Health Research Institute.
Third clinical trial launched to study whether type 2 diabetes can go into remission
Since launching two years ago, an innovative study that aims to induce remission of type 2 diabetes has captured the attention of hundreds of Londoners. For those with type 2 diabetes like Greg Ackland and Jocelyne Chauvin, the idea of stopping all medications has translated from a dream to a reality through participation in the REMIT study at Lawson Health Research Institute (Lawson).
With a family history of type 2 diabetes, Greg Ackland was first diagnosed over six years ago when he underwent an operation for a hernia. He developed a mild infection and, while being treated, his care team discovered his blood sugar levels were high.
Ackland started treatment and was eventually taking four pills per day. “I watched the progression of my medications and thought ‘I’m losing this battle,’” says 51 year-old Ackland.

Above: Greg Ackland, research participant in the REMIT study
He saw information about the REMIT study on the local news and after meeting the criteria he was enrolled. The outcomes have been incredible. Ackland has now stopped all medications and his blood sugar levels are good. He has recommitted to exercise which has resulted in weight loss and muscle gain.
“I’m glad I jumped at the opportunity to participate in this trial,” says Ackland. “I’ve reset myself.”
Lawson is one of seven Canadian sites taking part in the REMIT study, which is considered a significant departure in strategy in the care of people with type 2 diabetes. The study consists of a series of clinical trials that tests an aggressive approach in recently diagnosed patients. The first two trials in London saw significant interest in participation from those with type 2 diabetes. A third REMIT trial is now being launched providing another opportunity for individuals with type 2 diabetes to take part.
“The goal of the REMIT study is to take a proactive approach to help people early in the disease, normalize their blood sugars for a period of 12 weeks and then slow the progression of the disease and the need for additional medications,” says Dr. Irene Hramiak, Lawson researcher, endocrinologist, and Chief of the Centre for Diabetes, Endocrinology and Metabolism at St. Joseph’s Health Care London. “We want to know if we can induce remission, for how long and whether it matters what combination of medications we use.”
The standard treatment for people with type 2 diabetes is to start on a single medication, which is then followed by the addition of more drugs and insulin as the disease progresses. In the REMIT study, patients receive intensive treatment early in their care journey that consists of two diabetes medications plus insulin at bedtime for three months to see if remission can be induced. In addition, patients are supported to make lifestyle changes with a diet and 30 minutes of exercise each day.
“When I saw a gentleman on the news talking about the REMIT study and how it allowed him to stop taking all medications, I thought ‘cool!’” says Jocelyne Chauvin. The 62 year-old Londoner was first diagnosed with type 2 diabetes three years ago after a regular checkup. While it was difficult news, she had a family history of the disease and health issues before her diagnosis.

Above: Jocelyne Chauvin, research participant in the REMIT study
“I started taking one pill a day and was told I’d be up to four pills a day within six months,” says Chauvin. “But with good nutrition and exercise I worked hard to stay on one pill a day for three years.”
After hearing about the study, she contacted the research team and, after meeting the criteria, was enrolled in April 2017. Chauvin has now stopped all medications and says she feels much better. She exercises more and her blood sugar levels are close to normal.
“This is my first time participating in a clinical trial and I’m very excited about my experience,” says Chauvin.
REMIT is being led by the Population Health Research Institute (PIHR), a joint institute of McMaster University and Hamilton Health Sciences. The study follows a PHRI pilot study of early aggressive treatment that resulted in up to 40 per cent of intervention group participants with type 2 diabetes going into remission and not needing any diabetes treatment for at least three months.
“The idea of putting type 2 diabetes into remission is changing the way we think about the disease. It has a strong appeal to both those with type 2 diabetes and clinicians,” says Dr. Hramiak. “It’s changing the paradigm of when and how to use medication for type 2 diabetes.”
Those who would like more information about the trial can call 519-646-6100 ext. 65373.