Search
Search
Expanded No Fixed Address strategy houses half of those in danger of homelessness
At a community symposium on health care and homelessness attended by over 250 Londoners, a research team from Lawson Health Research Institute announced the results of a nine-month, federally funded project tackling the issue of homelessness from within hospital walls.
The No Fixed Address (NFA) strategy reaches and supports patients during the crucial transitional period when they are being discharged from the hospital and re-integrated into the community. The approach was initially tested with strong success for mental health patients across the city and the second ‘version’ of the project was extended to medical units at London Health Sciences Centre’s University Hospital and Victoria Hospital.

“Many of our patients with lived experience of homelessness were saying that their journey started with a hospital discharge,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and NFA project lead. “They were often experiencing major transitions in their lives and then experienced a hospital stay. Normally a relatively short visit, they aren’t able to gather the information and make a plan to be able to leave the hospital with somewhere to stay.”
Through partnerships between service providers and non-profit organizations, the NFA strategy helps prevent homelessness by providing timely and accessible supports to patients who would otherwise be discharged into homelessness. Staff from the Canadian Mental Health Association Middlesex, Salvation Army’s Housing Stability Bank, and Ontario Works in the City of London provided direct, on-site patient access to housing and income support databases
“Lawson’s No Fixed Address research project is the first evaluation anywhere of a strategy that aims to reduce the number of hospital patients being discharged into homelessness,” says Dr. Forchuk.
Over nine months, 74 people experiencing medical health issues accessed the NFA program. Of those, 54 per cent were also experiencing mental health challenges.
All of the study participants were in imminent danger of homelessness. Through the supports provided as part of this research study, half were able to arrange housing before being discharged.
“We were able to help a lot of people, with 50 per cent successfully securing housing,” shares Dr. Forchuk. “With the results and feedback we received, we learned a lot about how we can make the program even better.”
They found that there is a need for the supports to be extended as a transitional program in the community post-discharge, as the length of stay in the medical units tended to be short.
The project’s previous phase, involving acute and tertiary psychiatric care in the London region, prevented homelessness in 95 per cent of cases. “Going into the medical units, we found that people have highly complex needs that often involved mental health challenges.
By simply using the same approach that we did for those in psychiatric care, we helped half of the people find housing. To best serve the needs of everyone, we want to follow them after discharge.”
The team sees a solution in having a housing support worker provide transitional, wrap-around services that follow the person. They would continue to meet and work together after the hospital stay, helping to access community programs.
“This role would be embedded in both the health care system and the homeless serving system, supporting individuals who have complex physical and mental health issues as they are also navigating homeless resources.”
This project is funded by the Government of Canada's Homelessness Partnering Strategy’s (HPS) Innovative Solutions to Homelessness funding stream.
Overview and Numbers
Fast facts on homelessness and health care
- Stable housing after discharge is associated with higher quality of life, reduced substance abuse and fewer hospital admissions.
- Homeless clients are four times more likely to be readmitted to hospital within a month compared to low-income matched controls.
- Hospital care for homeless clients costs an average of $2,559 more per client.
- Finding appropriate housing or avoiding a potential eviction takes time – it is important to start as soon as possible during the discharge process.
Implementation of first phases of No Fixed Address
- Access on the unit to a housing advocate and income support staff.
- The initial intervention was accessed by 219 acute psychiatric clients, as well as 32 clients within a specialized tertiary care psychiatric hospital - only 3 became or remained homeless.
- Expanded to be an immediate wrap-around service with offices set up in the hospital mental health units.
- Staff from the Canadian Mental Health Association Middlesex (CMHA), Ontario Works (OW), and Salvation Army’s Housing Stability Bank (HSB) have on-site access to housing and income support databases.
- Clients can access service by drop-in or appointment.
- Services include assistance for finding housing, financial assistance, such as rent/utilities in arrears or first/last months’ rent for a new home, and access to high quality used furnishings, household supplies and a cleaning service.
Expanded second phase of No Fixed Address
- Program ran from July 2018 to March 2019 (9 months).
- 74 people accessed the program.
- Complex situations with both mental health and physical problems: 100% had medical issues and 54% had mental health issues.
- Lengths of stay were very short.
- People could not attend drop-in due to medical issues, so they relied on referral from staff.
- Although they were all in imminent danger of homelessness, 38 people (50%) were housed as a result of this program.
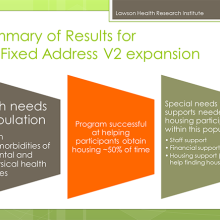
What were the main housing needs?
- Help finding a place to live
- Money for deposit
- Financial support
- Transportation support
- Help getting benefits
Recommendations and learnings for future models
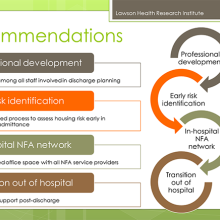
- Housing support worker needs to be a transitional support since work will be needed after discharge.
- Social work not the only key players (patient care facilitators, nursing staff, etc.).
- The transitional housing support role needs to be well embedded in the homeless serving system, as well as health care.
- People have physical and mental health issues and are also going to be navigating homeless resources.
- Despite the low success rate, many people were housed who would have otherwise been discharged to homelessness.
- We learned a lot about what was needed in an area where there was a knowledge vacuum.
- Future plans involve implementation with improvements to the model.
Family environment influences emotional well-being of children with epilepsy
LONDON, ON – Children with epilepsy have a higher risk of developing emotional and behavioural disorders, including depression, anxiety and poor self-esteem, yet it has been difficult for researchers to pinpoint why this occurs. In a new study, researchers at Children’s Health Research Institute (CHRI), a program of Lawson Health Research Institute, have found that family environment influences the relationship between clinical characteristics of epilepsy at diagnosis and children's emotional well-being two years later.
Emotional well-being is a broad measure of emotional functioning that includes multiple aspects of mental health, such as depression, anxiety, anger, happiness, or confidence. The researchers studied a group of children aged four to 12 with new-onset epilepsy, investigating factors at the time of diagnosis and their impact on the emotional well-being of the children two years later. The study focused on the role of the family environment, an area that has not been well-studied.
Results showed that clinical factors related directly to the children’s epilepsy, such as the type of epilepsy and frequency of seizures, were not associated with emotional well-being. Instead, several family characteristics, including family stresses, functioning and resources, were strongly associated with emotional well-being.
“This is important for how we think about patient care,” says Dr. Kathy Speechley, principal investigator on the study, Chair of the Children’s Health & Therapeutics Division at CHRI and a professor at Western University’s Schulich School of Medicine & Dentistry. “Treating the physical symptoms of chronic disease alone often does not result in significant improvements in quality of life. We need to examine other avenues for care.”
“From the time of diagnosis forward, it’s important for the health care team to take a broader, family-centred approach beyond controlling a child’s seizures. This means developing a better understanding of what day-to-day life is like for families living with childhood epilepsy, including their stressors, how well they are functioning and the resources they have to aid their adaptation to stressful life events,” says Dr. Shane Goodwin, first author on the study, which was conducted while he was a PhD candidate in the Department of Epidemiology & Biostatistics at Schulich Medicine & Dentistry and a trainee at CHRI. He is currently a postdoctoral fellow at the University of Waterloo.
One example of a family-centered approach to care the researchers point to is referring patients and their families to support programs, such as Clinic to Community in Southwestern Ontario. The Clinic to Community program is funded by the Ontario Brain Institute, and provides information about epilepsy and a network of support services.
The researchers completed the study using data from the Health-Related Quality of Life in Children with Epilepsy Study (HERQULES), a multicenter prospective cohort study based in Children’s Hospital at London Health Sciences Centre.
They will now continue to analyze data from the same group of patients as they progress toward adulthood and will develop intervention trials aimed at supporting families’ successful adaptation to life with epilepsy.
The study received funding from the Canadian Institutes of Health Research and the Children’s Health Foundation.
Drs. Kathy Speechley and Shane Goodwin will be available for interviews and photos on Wednesday, January 24 between 1:30 p.m. and 5:00 p.m.
-30-
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Senior Media Relations Consultant
Communications & Public Engagement
T: 519-685-8500 ext. 73502
Celine.zadorsky@lhsc.on.ca