Search
Search
Fecal transplants show promise in improving melanoma treatment
LONDON, ON – In a world-first clinical trial published in the journal Nature Medicine, a multi-centre study from Lawson Health Research Institute, the Centre hospitalier de l’Université de Montréal (CHUM) and the Jewish General Hospital (JGH) has found fecal microbiota transplants (FMT) from healthy donors are safe and show promise in improving response to immunotherapy in patients with advanced melanoma.
Immunotherapy drugs stimulate a person’s immune system to attack and destroy cancer. While they can significantly improve survival outcomes in those with melanoma, they are only effective in 40 to 50 per cent of patients. Preliminary research has suggested that the human microbiome – the diverse collection of microbes in our body – may play a role in whether or not a patient responds.
“In this study, we aimed to improve melanoma patients’ response to immunotherapy by improving the health of their microbiome through fecal transplants,” says Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Associate Scientist at Lawson and Associate Professor in the Department of Oncology at Western University’s Schulich School of Medicine & Dentistry.
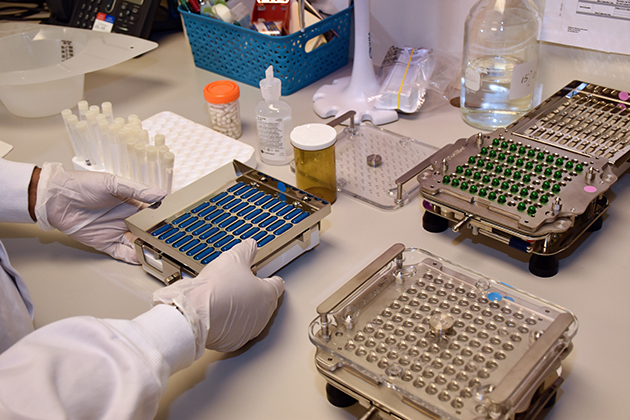
A fecal transplant involves collecting stool from a healthy donor, screening and preparing it in a lab, and transplanting it to the patient. The goal is to transplant the donor’s microbiome so that healthy bacteria will prosper in the patient’s gut.
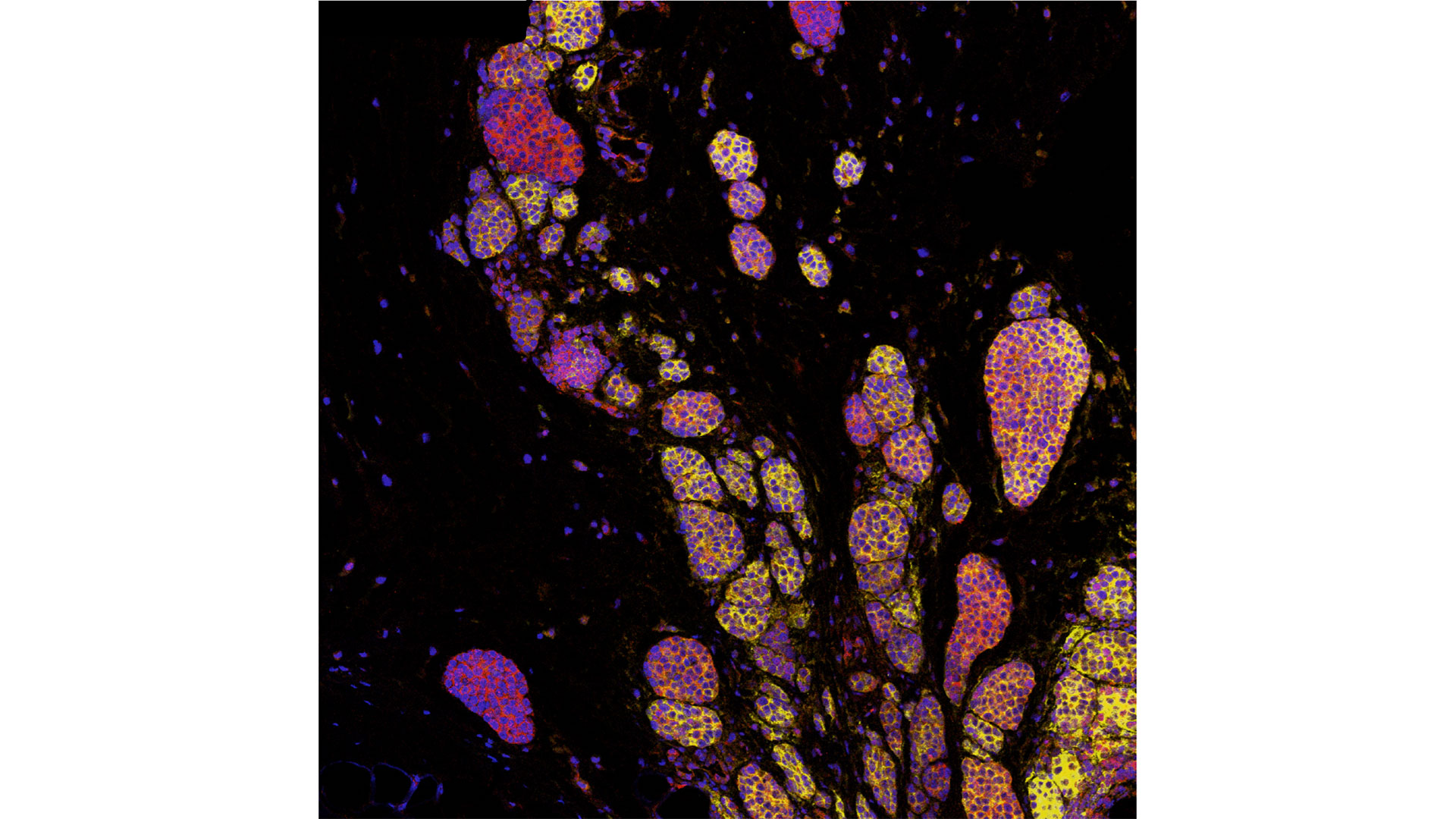
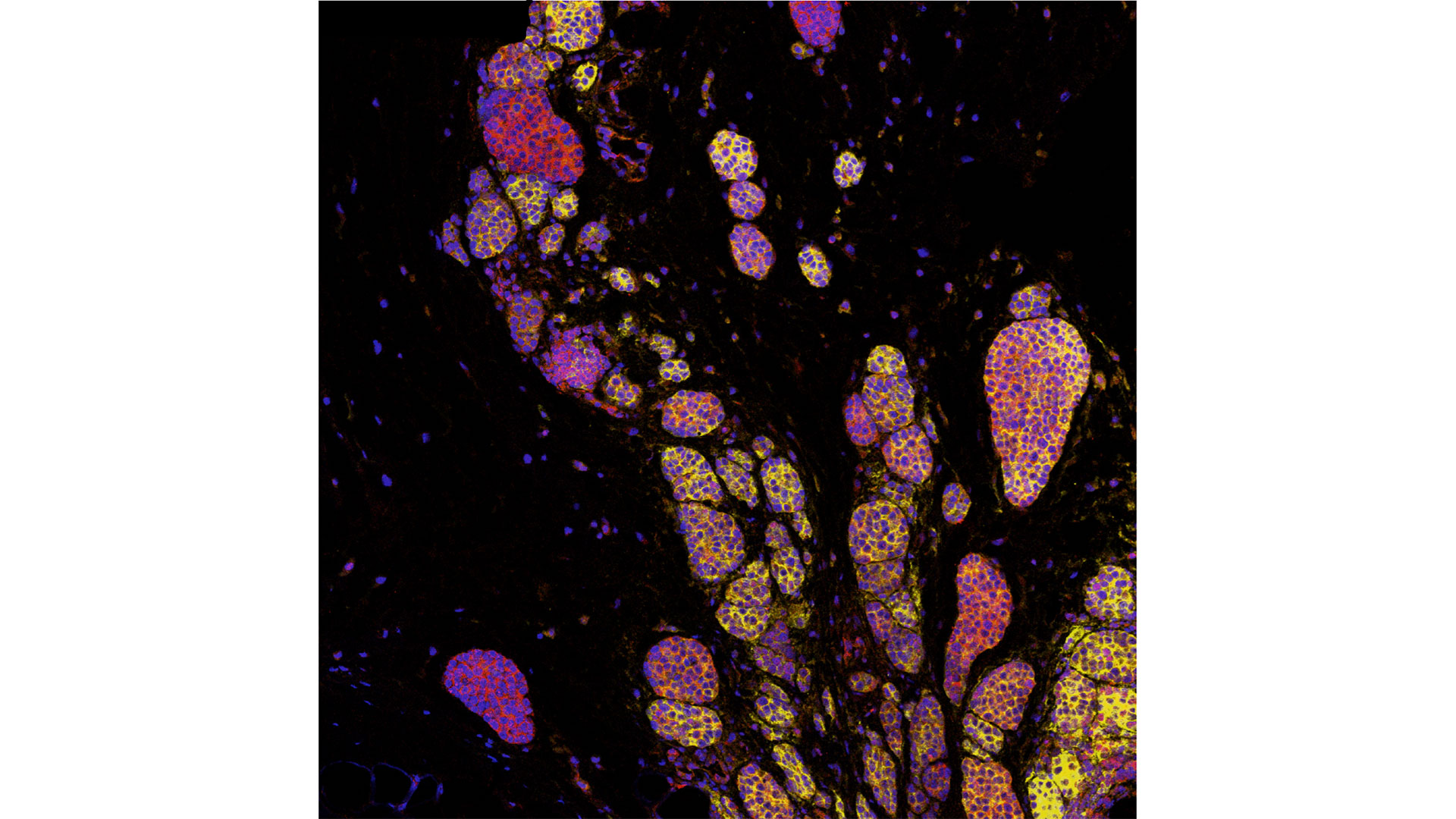
“The connection between the microbiome, the immune system and cancer treatment is a growing field in science,” explains Dr. Saman Maleki, Scientist at Lawson and LHSC’s LRCP, Assistant Professor in Schulich Medicine’s Departments of Oncology, Pathology and Laboratory Medicine, and Medical Biophysics, and senior investigator on the study. “This study aimed to harness microbes to improve outcomes for patients with melanoma.”
The phase I trial included 20 melanoma patients recruited from LHSC, CHUM and JGH. Patients were administered approximately 40 fecal transplant capsules orally during a single session, one week before they started immunotherapy treatment.
The study found that combining fecal transplants with immunotherapy is safe for patients – which is the primary objective of a phase I trial (also called ‘safety trials’). The study also found 65 per cent of patients who retained the donors’ microbiome had a clinical response to the combination treatment. Five patients experienced adverse events sometimes associated with immunotherapy and had their treatment discontinued.
“We have reached a plateau in treating melanoma with immunotherapy, but the microbiome has the potential to be a paradigm shift,” says Dr. Bertrand Routy, Oncologist and Director of CHUM’s Microbiome Center. “This study puts Canada at the forefront of microbiome research by showing we can safely improve patients’ response to immunotherapy through fecal transplants.”
“These exciting results add to a rapidly growing list of publications suggesting that targeting the microbiome may provide a major advance in the use of immunotherapy for our patients with cancer,” adds Dr. Wilson H. Miller Jr. of the JGH and Professor in the Departments of Medicine and Oncology at McGill University.
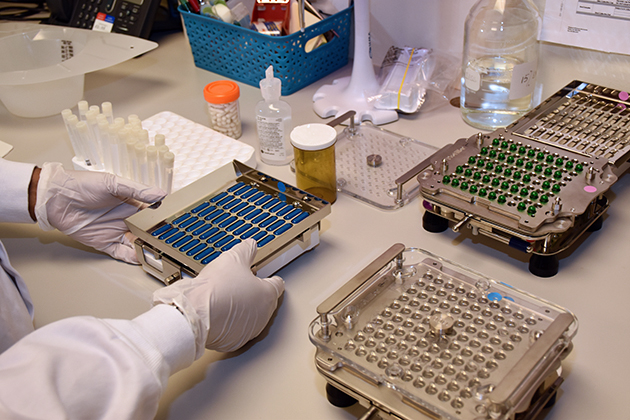
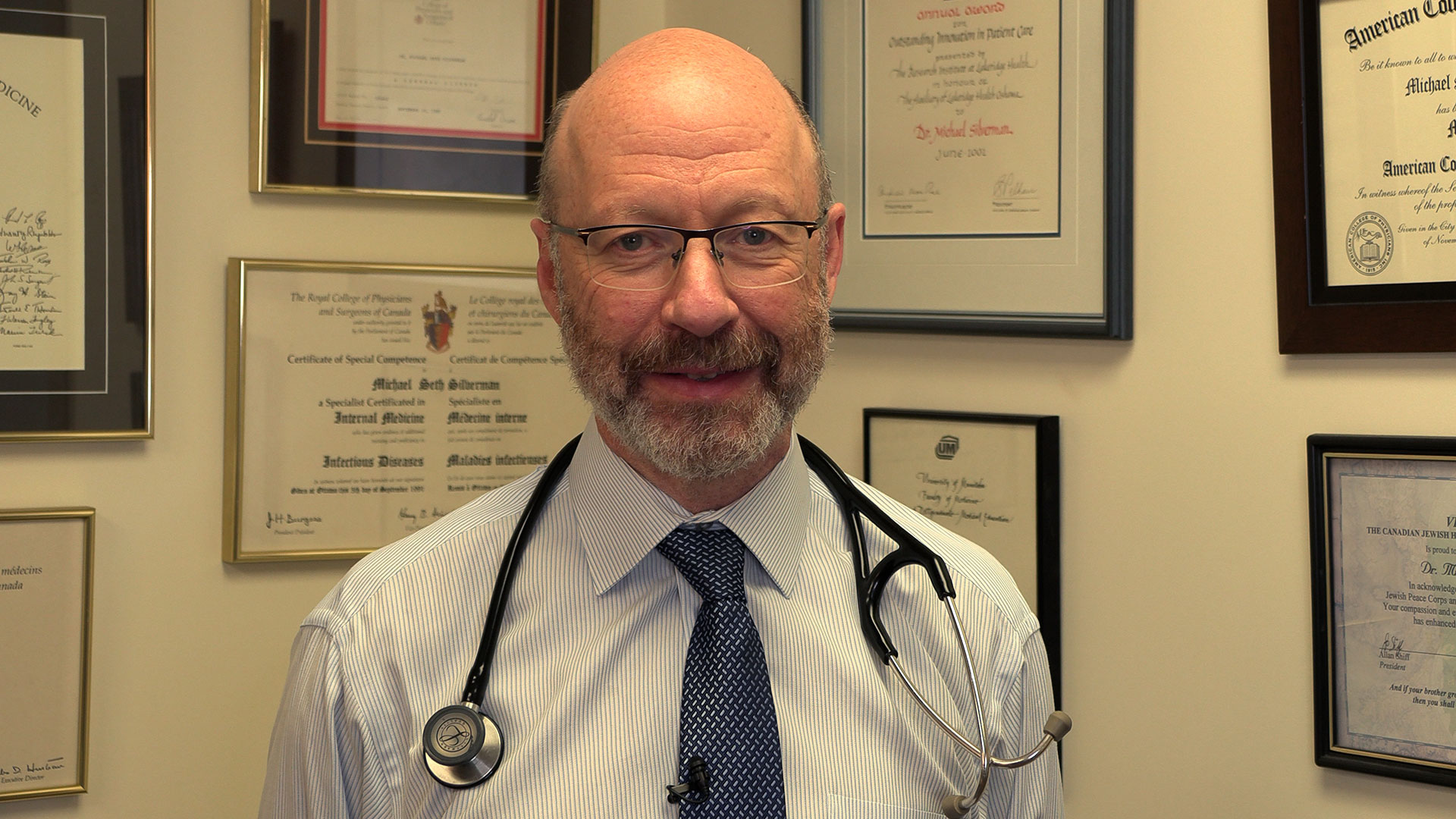
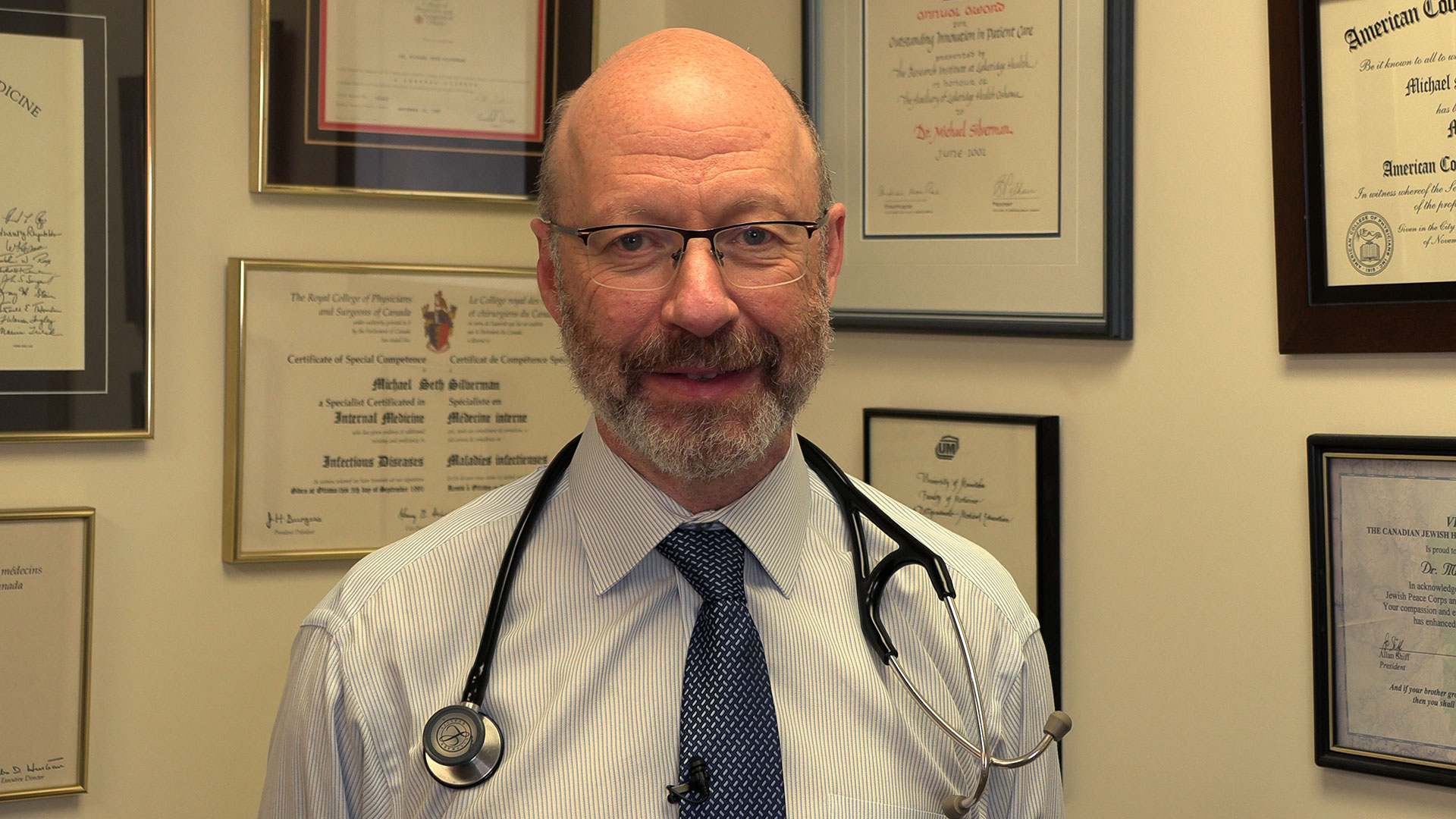
The study is unique due to its administration of fecal transplants (from healthy donors) in capsule form to cancer patients – a technique pioneered in London by Dr. Michael Silverman, Lawson Scientist, Chair of Infectious Diseases at Schulich Medicine and Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London.
“Our group has been doing fecal transplants for 20 years, initially finding success treating C. difficile infections. This has enabled us to refine our methods and provide an exceptionally high rate of the donor microbes surviving in the recipient’s gut with just a single dose,” says Dr. Silverman. “Our data suggests at least some of the success we are seeing in melanoma patients is related to the efficacy of the capsules."
The team has already started a larger phase II trial involving centres in Ontario and Quebec. Lawson researchers are also studying the potential of fecal transplants in the treatment of other cancers, including renal cell carcinoma, pancreatic cancer and lung cancer, as well as HIV and rheumatoid arthritis.
This research is supported in part through donor funding from London Health Sciences Foundation, Western University, the Lotte and John Hecht Memorial Foundation, the JGH Foundation, Canadian Cancer Society’s Impact Grant program and The Terry Fox Foundation.
-30-
ADDITIONAL DOWNLOADABLE MEDIA

About the CRCHUM
The CHUM Research Centre (CRCHUM) is one of North America’s leading hospital research centres. It strives to improve the health of adults through a continuum of research spanning disciplines such as basic science, clinical research and population health. More than 2,150 people work at the CRCHUM, including nearly 500 researchers and nearly 650 students and postdoctoral fellows. crchum.com
About the Jewish General Hospital
Part of the Integrated Health and Social Services University Network for West-Central Montreal (CIUSSS), the Jewish General Hospital has served patients from Montreal, elsewhere in Quebec, and beyond, since 1934. This McGill University teaching hospital, with approximately 600 beds, is one of the province's largest acute-care hospitals. It admits more than 22,000 patients per year, while handling approximately 578,000 outpatient visits, more than 84,000 emergency visits and more than 3,600 births. Treatment is provided by approximately 800 affiliated doctors, many of whom have teaching appointments at McGill University, as well as more than 300 medical residents per year, together with nursing and a wide range of allied health services.
Lawson Health Research Institute is one of Canada’s top hospital-based research institutes, tackling the most pressing challenges in health care. As the research institute of London Health Sciences Centre and St. Joseph’s Health Care London, our innovation happens where care is delivered. Lawson research teams are at the leading-edge of science with the goal of improving health and the delivery of care for patients. Working in partnership with Western University, our researchers are encouraged to pursue their curiosity, collaborate often and share their discoveries widely. Research conducted through Lawson makes a difference in the lives of patients, families and communities around the world. To learn more, visit www.lawsonresearch.ca.
Communications Consultant & External Relations
Lawson Health Research Institute
T: 519-685-8500 ext. ext. 64059
C: 226-919-4748
@email
Fecal transplants show promise in improving melanoma treatment
In a world-first clinical trial published in the journal Nature Medicine, a multi-centre study from Lawson Health Research Institute, the Centre hospitalier de l’Université de Montréal (CHUM) and the Jewish General Hospital (JGH) has found fecal microbiota transplants (FMT) from healthy donors are safe and show promise in improving response to immunotherapy in patients with advanced melanoma.
Immunotherapy drugs stimulate a person’s immune system to attack and destroy cancer. While they can significantly improve survival outcomes in those with melanoma, they are only effective in 40 to 50 per cent of patients. Preliminary research has suggested that the human microbiome – the diverse collection of microbes in our body – may play a role in whether or not a patient responds.
“In this study, we aimed to improve melanoma patients’ response to immunotherapy by improving the health of their microbiome through fecal transplants,” says Dr. John Lenehan, Medical Oncologist at London Health Sciences Centre’s (LHSC) London Regional Cancer Program (LRCP), Associate Scientist at Lawson and Associate Professor in the Department of Oncology at Western University’s Schulich School of Medicine & Dentistry.
A fecal transplant involves collecting stool from a healthy donor, screening and preparing it in a lab, and transplanting it to the patient. The goal is to transplant the donor’s microbiome so that healthy bacteria will prosper in the patient’s gut.
“The connection between the microbiome, the immune system and cancer treatment is a growing field in science,” explains Dr. Saman Maleki, Scientist at Lawson and LHSC’s LRCP, Assistant Professor in Schulich Medicine’s Departments of Oncology, Pathology and Laboratory Medicine, and Medical Biophysics, and senior investigator on the study. “This study aimed to harness microbes to improve outcomes for patients with melanoma.”
The phase I trial included 20 melanoma patients recruited from LHSC, CHUM and Jewish General Hospital. Patients were administered approximately 40 fecal transplant capsules orally during a single session, one week before they started immunotherapy treatment.
The study found that combining fecal transplants with immunotherapy is safe for patients – which is the primary objective of a phase I trial (also called ‘safety trials’). The study also found 65 per cent of patients who retained the donors’ microbiome had a clinical response to the combination treatment. Five patients experienced adverse events sometimes associated with immunotherapy and had their treatment discontinued.
“We have reached a plateau in treating melanoma with immunotherapy, but the microbiome has the potential to be a paradigm shift,” says Dr. Bertrand Routy, Oncologist and Director of CHUM’s Microbiome Center. “This study puts Canada at the forefront of microbiome research by showing we can safely improve patients’ response to immunotherapy through fecal transplants.”
“These exciting results add to a rapidly growing list of publications suggesting that targeting the microbiome may provide a major advance in the use of immunotherapy for our patients with cancer,” adds Dr. Wilson H. Miller Jr. of the JGH and Professor in the Departments of Medicine and Oncology at McGill University.
Previous studies looking at patients receiving immunotherapy who do not respond have found many had an unhealthy microbiome, explains Dr. Lenehan.
“There's a portion of people who don't respond or the treatment just doesn't work,” says Dr. Lenehan. “The hope with the fecal transplant is to make more people respond to treatment.”
These results have also led to a closer examination of the role of the microbiome in regulating how the body responds to disease and how the drugs themselves interact with the microbiome.

“The microbes on and in us - and there's actually a huge amount of those – play a critical role, including modulating some of our immune responses,” explains Dr. Jeremy Burton, Research Chair of Human Microbiome and Probiotics, Scientist at Lawson and St. Joseph’s Health Care London and Associate Professor in the Department of Microbiology and Immunology at Schulich Medicine.
The study is unique due to its administration of fecal transplants (from healthy donors) in capsule form to cancer patients – a technique pioneered in London by Dr. Michael Silverman, Lawson Scientist, Chair of Infectious Diseases at Schulich Medicine and Medical Director of the Infectious Disease Care Program at St. Joseph’s Health Care London.
“Our group has been doing fecal transplants for 20 years, initially finding success treating C. difficile infections. This has enabled us to refine our methods and provide an exceptionally high rate of the donor microbes surviving in the recipient’s gut with just a single dose,” says Dr. Silverman. “Our data suggests at least some of the success we are seeing in melanoma patients is related to the efficacy of the capsules."
The team has already started a larger phase II trial involving centres in Ontario and Quebec. Lawson researchers are also studying the potential of fecal transplants in the treatment of other cancers, including renal cell carcinoma, pancreatic cancer and lung cancer, as well as HIV and rheumatoid arthritis.
This work is not possible without poop donors, and there is a critical need for more. Donors must be between the ages of 18 to 50 and reside in the London, Ont. area. To learn more about eligibility and donating, call the 519 646-6100, ext. 61726 or email Dr. Seema Nair Parvathy, Research Scientist, at SeemaNair.Parvathy@sjhc.london.on.ca.
This research is supported in part through donor funding from London Health Sciences Foundation, Western University, the Lotte and John Hecht Memorial Foundation, the JGH Foundation, Canadian Cancer Society’s Impact Grant program and The Terry Fox Foundation.
Fifth annual Lawson Impact Awards honours research excellence
Over 300 guests attended the fifth annual Lawson Impact Awards on Wednesday, April 18 at the London Convention Centre to honour research making a difference and to recognize the accomplishments of our scientists, staff, trainees and partners.
“There are many individuals, groups and partners at Lawson who regularly go above and beyond to drive innovative new discoveries. For the past five years, the Lawson Impact Awards have given us the opportunity to step back and reflect on the importance of the work we do here and how these contributions ultimately improve patient care,” says Dr. David Hill, Scientific Director, Lawson Health Research Institute.
This year’s Lawson Impact Award winners include:
- Dr. Robert Teasell – Scientist of the Year Award
- Dr. Mandar Jog – Innovation Award
- Dr. Manuel Montero-Odasso – Dr. Joseph Gilbert Research Contribution of the Year Award
- London X-Ray Associates – Industry Partner of the Year Awards
- CAISA Fashion Show; London Run for Ovarian Cancer; and Kyle MacDonald and John Franklin – Community Partner of the Year Award
- Sarah Best – Staff Award of Excellence
- Sheila Fleming – Staff Award of Excellence
- Amanda McIntyre – Leadership Award for Fellows & Students
The recipients of Lawson’s 2018 Strategic Research Fund (SRF) were also revealed at the Lawson Impact Awards. The Lawson SRF is an annual competition that supports projects that will advance science in alignment with Lawson’s strategic research goals, as outlined in the Lawson Strategic Plan 2014-2018. This year’s competition was open to all areas of research. The following two projects were awarded $50,000 over a two-year period:
- “Mindfulness group intervention for newly diagnosed persons with Multiple Sclerosis: A pilot study” – Drs. Sarah A. Morrow and Arlene MacDougall
- “Extending routinely collected data research at Western: Does enhanced medical reconciliation improve care at London hospitals?” – Drs. Blayne Welk and Amit Garg
In addition to the Lawson Impact Award and SRF recipients, two Children’s Health Research Institute (CHRI) award recipients were recognized at the event. CHRI is a program of Lawson and awards a Scientist and Trainee of the Year annually. These awards are sponsored by the Children’s Health Foundation. CHRI’s 2017 award recipients were honoured at the Lawson Impact Awards: Dr. Lina Dagnino (CHRI Scientist of the Year) and Dr. Amer Youssef (CHRI Deb Comuzzi Trainee of the Year).
A highlight of the event was a keynote presentation from physician-scientist and 3D innovator, Dr. Julielynn Wong, titled “How Technology is Enhancing Our Future.” Dr. Wong delivered an engaging talk on how technology trends such as 3D printing and drones can improve health care accessibility. Her presentation included a 3D printing demonstration and guests were given the opportunity to examine samples of 3D printed medical supplies.
To view videos of each award winner, visit the Lawson YouTube page. To see more photos from the event, visit Lawson’s Facebook page.
First-in-North-America resource touts health benefit of fermented foods
New network helps consumers, researchers and food industry find and share trusted information about ‘ferment-ceuticals’
London (Ont.) – A one-stop network, the first of its kind in North America, has begun sharing easily digested research, recipes and other resources about the health benefits of fermented foods.
The new Canadian Fermented Foods Initiative (CFFI) launches officially on Nov. 17 with a gathering of research and industry experts from across the country and Europe.
The collaboration helps consumers, researchers, health professionals and food industry share trusted, science-based expertise and information about fermented foods.
Funded by the Weston Family Foundation, the initiative is led by Jeremy Burton, PhD, who heads of one of Canada’s largest microbiome research programs and is Interim Vice President Research at St. Joseph’s Health Care London and Lawson Research Institute. His research leadership is joined by Raylene Reimer, PhD, professor of nutrition at the University of Calgary; and University of Alberta professor Ben Willing, PhD, former Canada Research Chair in Microbiology of Nutrigenomics.
Fermented foods such as sourdough bread, sauerkraut, kimchi and kombucha offer more than just good taste and an economical way to preserve food, Burton says. Large, population-based studies show people who eat fermented foods are generally healthier, with fewer digestive issues and lower risk of chronic diseases.
“How exactly does that work – and why? Well, that’s the big question we’re trying to solve,” Burton says. “One day, I believe, ‘ferment-ceuticals’ will be engrained in our diets and our health vocabulary.”
St. Joseph's is a leader in the field. A paper authored by the team and published this week in Advances in Nutrition represents the most comprehensive synthesis to date of research on fermented foods and human health.
Connor Flynn, a London, Ont., chef, master food preserver and high school teacher whose video recipes are included in the CFFI website, adds, “Fermenting foods is an old practice that’s never fallen out of flavour, but has sometimes fallen out of favour to North Americans. Now it has become popular again.”
To learn more about the CFFI, including fermented food recipes and the chef behind them, head to fermentedfoods.ca.
- 30 -
To arrange interviews with CFFI project lead Jeremy Burton and chef Connor Flynn, who are available Friday Nov. 14 from 7 am – 8 am ET and Nov. 14 from 1 – 4 pm ET, contact:
Deb (Flaherty) Van Brenk, Communication Consultant
St. Joseph’s Health Care London
@email
About St. Joseph’s Health Care London
Renowned for compassionate care, St. Joseph’s Health Care London is a leading academic health care centre in Canada dedicated to helping people live to their fullest by minimizing the effects of injury, disease and disability through excellence in care, teaching and research. Through Lawson Research Institute, our innovation arm, and with collaborative engagement with other health and academic partners, St. Joseph’s has become an international leader in the areas of: chronic disease management; medical imaging; specialized mental health care; rehabilitation and specialized geriatrics; and surgery. St. Joseph’s operates through a wide range of hospital, clinic and long-term and community-based settings, including: St. Joseph’s Hospital; Parkwood Institute; Mount Hope Centre for Long Term Care; and the Southwest Centre for Forensic Mental Health Care.
Funding for unique strategy to prevent homelessness after hospital discharge
In Canada, about 235,000 people experience homelessness each year. The number of homeless people, and the length of time they spend homeless, continues to rise. Homelessness is not a choice and anyone can become homeless.
Although the root cause is poverty, some underlying issues are poor physical or mental health; violence or abuse in the home; lack of employment or income; and, a shortage of affordable housing.
A group of researchers at Lawson Health Research Institute (Lawson), working at both London Health Sciences (LHSC) and St. Joseph’s Health Care London (St. Joseph’s), are committed to tackling the issue of homelessness from within hospital walls, where some patients face the risk of being discharged into homelessness.
“Many of our patients with lived experience of homelessness were saying that their journey started with a hospital discharge,” says Lawson clinician researcher Dr. Cheryl Forchuk. “Often, they were experiencing major transitions in their lives and then experienced a hospital stay. Normally a relatively short visit, they aren’t able to gather the information and make a plan to be able to leave the hospital with somewhere to stay.”
On September 10, Adam Vaughan, Canadian MP and Parliamentary Secretary (Housing and Urban Affairs), on behalf of the Honourable Jean-Yves Duclos, Minister of Families, Children and Social Development, announced that Lawson will receive $223,572 from the Homelessness Partnering Strategy’s (HPS) Innovative Solutions to Homelessness funding stream to support the project “No Fixed Address Version 2 Expansion” research project.

“This is a brilliant approach. It supports an augmented duty of care where hospitals have the means to transfer people into stable settings where they can continue to heal and move towards self-sufficiency,” says Parliamentary Secretary Vaughan.
Taking place at London Health Sciences Centre, this research will further refine the No Fixed Address strategy for reaching and supporting patients during the crucial transitional period when they are being discharged from the hospital and re-integrated into the community.
“Lawson’s expanded No Fixed Address research project is the first evaluation anywhere of a strategy to reduce the number of patients being discharged into homelessness. There is almost no literature on any aspect of this troublesome issue,” explains Dr. Forchuk who is the study’s Principal Investigator. Dr. Forchuk is also the Beryl and Richard Ivey Research Chair in Aging, Mental Health, Rehabilitation and Recovery and Assistant Director at Lawson.

This project is an extension of three previous studies conducted by Dr. Forchuk’s research team, which developed and tested this novel approach. They demonstrated the efficacy, feasibility and cost-effectiveness of using the No Fixed Address strategy in acute and tertiary psychiatric care in the London region, at both LHSC and St. Joseph’s. In the first phase, they found that the interventions used prevented homelessness in 95 per cent of cases.
The researchers are now taking a solution proven to have worked in the mental health units and applying it in selected medical departments at LHSC. Through the study, the services will be available to all patients in those units who are at risk of homelessness. There have already been 17 patients who have accessed this support since the project got underway this summer.
Three community partners from London are supporting implementation of the strategy - Canadian Mental Health Association Middlesex, Ontario Works in the City of London and the Salvation Army’s Housing Stability Bank. They will provide assistance in areas like securing appropriate private-sector housing, provision of income and employment supports, and financial assistance.
“In many ways London, Ontario is the high water mark of solving and tackling homelessness. This community has a lot of be proud of given the way that the municipality is stepping up to the plate and how many different organizations are working together towards a common goal,” says Parliamentary Secretary Vaughan.
This kind of collaboration showcases the important partnership between the Canadian Government, research-intensive hospitals and community organizations to translate innovative solutions from the research stage to the front line of care.
“The hope is that the findings will be even more robust, leading to the development of a best-practice model of hospital discharge that can be adopted throughout Canada. This will reinforce the need for a systemic change in the way hospital discharges occur and ensuring the person is transitioning to a secure housing arrangement,” says Dr. Forchuk.
Learn more about the Government of Canada’s Homelessness Partnering Strategy.
News Coverage
- CBC London - Helping medical patients in London avoid homelessness when they leave hospital
- CTV London - Expanded research hopes to break the cycle of homelessness that psychiatric patients sometimes face when discharged
- Global News, AM 980 - Program that finds housing for homeless patients in hospital gets $223K in federal funding
- London Free Press - 'Brilliant approach' to homelessness gets federal grant